The “Curriculum for the administration of sedation outside the OR in patients over 12 years of age” was developed by the Universidad Nacional de Colombia, by invitation of the Colombian Society of Anesthesiology and Resuscitation – S.C.A.R.E.
ObjectiveIdentify the essential knowledge and the skills required by practitioners for the safe and effective administration of sedation to develop of a curriculum for the administration of sedation outside the operating room in patients over 12 years of age.
Materials and methodsThe curriculum was developed based on the methodological guiding principles of the Clinical Practice Guidelines for the administration of sedation outside the OR, using the PICO approach, in addition to the recommendations according to levels of evidence under the GRADE methodology.
ResultsThe Curriculum was designed with ten (10) recommendations about the competencies that the professional administering sedation to patients older than 12 years of age must have, for diagnostic or therapeutic procedures outside the OR.
ConclusionsThe Curriculum collects the best available evidence with a view to determine the competencies that the professional administering sedation to patients older than 12 years old shall develop, for diagnostic or therapeutic procedures outside the OR, and hence to contribute to improved quality, reducing the variability and morbidity of patients requiring sedation outside the OR.
El “Currículo para la administración de sedación fuera del quirófano en pacientes mayores de 12 años” fue desarrollado por la Universidad Nacional de Colombia, por convocatoria de la Sociedad Colombiana de Anestesia y Reanimación - S.C.A.R.E.
ObjetivoIdentificar los conocimientos indispensables y las competencias necesarias en los profesionales proveedores para que administren sedacion de manera segura y efectiva para el desarrollo de un curriculo para la administración de sedación fuera del quirófano en pacientes mayores de 12 años.
Materiales y métodosLa construcción del Currículo se basó en los lineamientos metodológicos de la Guía Práctica Clínica para la administración de sedación fuera del quirófano en pacientes mayores de 12 años, en los resultados de la búsqueda sistemática de la literatura orientada por la pregunta PICO, y en la formulación de recomendaciones según niveles de evidencia graduados bajo la metodología GRADE.
ResultadosSe desarrolló el Currículo con diez (10) recomendaciones de las competencias que debe tener el profesional que administra sedación a los pacientes mayores de 12 años para procedimientos diagnósticos o terapéuticos fuera del quirófano.
ConclusionesEl Currículo recoge la mejor evidencia disponible, con el propósito de determinar las competencias que debe desarrollar el profesional que administra sedación a los pacientes mayores de 12 años, sometidos a procedimientos diagnósticos o terapéuticos fuera del quirófano, y así contribuir a mejorar la calidad, disminuir la variabilidad y la morbilidad de los pacientes que requieran sedación fuera del quirófano.
Sedation is a frequently used practice to perform invasive and non-invasive medical and dental procedures, both diagnostic and therapeutic, for imaging, invasive radiology, emergencies, cardiac catheterization, and endoscopies, among others.1 These are out-patient procedures performed in places other that the operating room, and hence require adequate cooperation to unify processes and ensure a complete training of the staff involved, in order to avoid sedation-associated complications that are mostly preventable.1 Sedation training has traditionally been defined on the basis of expert consensus, educational tradition, self-learning and extrapolation of other scenarios.2 Acquiring skills to manage sedation requires that the provider be trained to provide an integrated response of knowledge, skills and attitudes.3 Most competences essential to sedation are established under the so-called parachute principle, the evaluation of interventions with great validity of appearance through randomized controlled trials may not be relevant, considering the common sense surrounding the favorable impact of its application.4
MethodologyA set of de Novo Clinical Practice Guidelines (CPG) on the administration of sedation outside the OR for patients over 12 years old was developed, upon identifying all the CPGs available in the literature, through a systematic literature search done by the Cochrane STI Group, then they were evaluated with a screening tool to measure their quality; these were all finally dismissed because none of them were adaptable.
The Guidelines Developer Team (GDT) designed 5 clinical PICO questions, prioritizing the safety and effectivenes of the clinical outcomes. The full version of the Clincal Practice Guideline is published as a web-appendix. A short version is published in other paper in this issue. The fifth question was: What competencies should the professionals administering sedation to patients over 12 years of age, undergoing diagnostic or therapeutic procedures outside the OR have? The question will be further elaborated with particular recommendations. The systematic reviews (SR) were evaluated using the AMSTAR checklist and the levels of evidence with GRADE. The results were analyzed by a working team formed by experts in sedation from 7 scientific societies and patients representative, in order to establish the strength and direction of the recommendations.
Independently, two pairs of experts – one in methodology and the other in content – were invited to review and comment on the extent and accuracy of the interpretation of the evidence supporting the recommendations in this guide.
Search of clinical evidenceThe systematic literature search identified four trials that evaluated the competencies and necessary training that healthcare professionals administering sedation outside the OR should have. The first is a controlled clinical trial and the remaining three are observational studies following an epidemiological design of the “before” and “after” type.
The controlled clinical trial5 compared the effectiveness of formal training in sedation versus self-learning in 48 emergency practitioners at a University Hospital with a high level of complexity. The self-learning phase included studying educational materials weeks prior training in person. The second phase was a four-hour in person training, with the guidance of expert instructors in pediatric critical care, anesthesiology and pharmacology.
The outcomes evaluated in this controlled trial were: the performance of the professionals in the cognitive evaluation about sedation, the perception of the participants about the training as a valuable clinical practice tool, and the perception of the participants about the need to learn more about sedation management.
The comparison between the in person training and self-learning indicates that the students assigned to the in person experience scored higher in the cognitive evaluation (p<0.0001 for means difference, with a 0.6 effect size calculated using “Cohen D” of 1.52, pointing to an overlap between the two groups of 38.2%). Furthermore, 79.2% of the participants taking the course and 100% of those that did not, agreed that the sedation course is a useful clinical practice tool. When evaluating the perception of the participants about the relevance of acquiring further knowledge on the management of sedation, only 54.2% of the course participants expressed the need for additional training, versus 79.2% of the self-learning group. The quality of the evidence was too low due to limitations in the risk of biases, applicability and accuracy.
The second trial is a before and after type observational design6 that assessed the impact of sedation training outside the OR, for non-anesthesiologists. The educational intervention was addressed to 19 participants from the emergency department, ICU, trauma, gastroenterology, radiology, oral surgery, pediatric cardiology, and pneumology. The educational program comprised virtual workshops on twelve topics: sedation objectives, professional requirements of the practitioners administering sedation, cardiopulmonary considerations, pharmacology, patient monitoring, equipment and devices, preparation for the procedure, development of a sedation plan, transfer, and recovery, timely identification and initial treatment of sedation-associated complications, “The Joint Commission” requirements, and finally, quality assessment. Then the participants attended presentations by one or two expert anesthesiologists who addressed topics regarding airway management, mask-reservoir device, use of the laryngeal mask, adequate tidal volume and respiratory rate, maneuvers to clear the airway, use of nasopharyngeal and oral devices, recognizing the call for assistance and mask ventilation by two providers, all using high fidelity simulators. The simulation was done under supervision and direct feedback of the facilitators (1 instructor per every 4 participants in each section).
Finally, and after the simulation, workshops were organized on the pharmacological considerations about the use of opioids and benzodiazepines (fentanyl, morphine, meperidine, hydromorfone, midazolam, and diazepam), how to reverse the use of these agents (naloxone and flumazenil) as well as different patient responses to sedation (normal, resistant, sensitive and extremely sensitive).
The outcomes evaluated in this trial were the level of knowledge of the theoretical concepts related to the used of sedation, performance in the basic airway management, airway management with different devices (laryngeal mask, bag-mask ventilation) and sedation reversie in the various clinical scenarios. The written test given before and after the course documented a higher performance of the practitioners after the training (p<0.0001), as well as in the management of mask-reservoir ventilation device in difficult airway patients (p<0.05), in patients without a difficult airway (p<0.05), management of the airway using the laryngeal mask (p<0.05) and the basic airway management (p<0.05). The quality of the evidence was extremely low due to limitations in the risk of biases, applicability and accuracy.
The third trial is a before and after design7 assessing the results of high fidelity simulation-based training for the use of sedation in the Emergency Department. 10 practitioners from the ED were invited to participate in this trial, half of which were trainees, while the other half were graduated professionals. During the high fidelity simulation, four scenarios were developed: airway management and difficult sedation administration (patient with asthma and patient allergic to opioids), use of airway salvage devices and/or drugs to reverse sedation, device failure (reservoir mask or defective pulse oximeter), and finally, basic and advanced airway management (mask-reservoir and orotracheal intubation).
The trial failed to indicate who provided the training and the outcomes evaluated were the frequency of participants who administer supplemental oxygen administration, those who use of expired CO2 monitoring, and those who review of paraclinical tests prior to the intervention, and the proportion of correct checklist completion before (patient and equipment evaluations) and after sedation. This study documented that after training all the participants administered supplemental oxygen (50% versus 100% before and after, respectively, p: 0.008), used the expired CO2 monitoring devices (before vs after training, non-informed proportions p: 0.004), and reviewed the laboratory results and images (20% versus 100% before and after, respectively, p: 0.024) prior to the procedure. Moreover, after the training, the percentage of practitioners that completed the checklist correctly increased both before (patient evaluation 56% DM 9 versus 80% DM 8, p=0.006), and after the procedure (32% DM 18 vs. 57% DM 20, p=0.048), except for the equipment checklist (25% DM 18 versus 35% DM 22, p=0.34). The quality of the evidence was very low because of limitations with the risk of biases, applicability, and accuracy.
Finally, the last trial included also with before and after type epidemiological design8 evaluated the acceptance and compliance with the clinical practice guidelines for the use of sedation and analgesia by non-anesthesiologists, developed by the American Society of Anesthesiology and the Japanese Medical Society. This study included 84 participants, specialists in emergency medicine, dentists, internists, surgeons, pediatricians, gynecologists and obstetricians.
The educational strategy included reading the clinical practice guidelines and a simulation component with four practical aspects:
- 1.
Clinical practice guidelines: pre-sedation evaluation, informed consent, proper fasting times, pulse oximetry during sedation, use of electrocardiography in cardiac patients, appointment of one assistant to monitor the patient, availability of a trained ACPR person during sedation, availability of emergency equipment and medicines, availability of oxygen, differentiation between analgesics and sedatives, administration of medicines, taper the dose when combining sedatives and analgesics, keep an IV line during the procedure, use of capnography if opioids are used, availability of antagonists, keep the patient under close observation until the risk of cardiopulmonary depression is no longer present, and consultation with an anesthesiologist in case of patients with especial circumstances.
- 2.
Use of sedatives and analgesics.
- 3.
Basic and advanced airway management.
- 4.
Cardiopulmonary revival.
The conclusion from this study was that the participants that properly follow the management guidelines increased considerably after the training, particularly with regards to informed consent (71.4% before versus 91.7% after, p<0.05), clinical evaluation of patients prior to sedation (71.4% vs 91.7%, p<0.05), the need to have a basic and advanced cardiopulmonary resuscitation expert available during sedation (56% vs 91.7%, p<0.05), proper knowledge to differentiate between sedatives and analgesics (65.5% vs 85.7%, p<0.05), availability of antagonist drugs (83.3% vs 100%, p<0.05), consult anesthesiologist in case of patients with especial circumstances (67.9% vs 95.2%, p<0.05), patient observation until the risk of cardiovascular depression clears (75% vs 81%, p<0.05), and finally, appoint someone to monitor the patient (50% versus 65%, p<0.05). The quality of the evidence was too low because of limitations in the risk of biases, applicability, and accuracy.
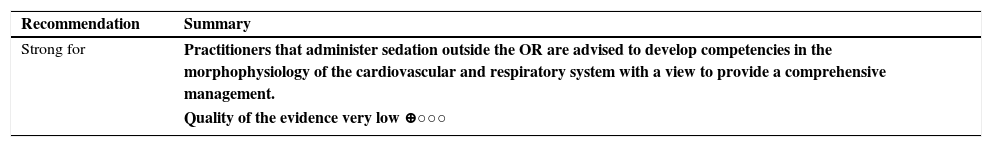
Recommendations and competenciesMorphophysiology of the cardiovascular and respiratory systemDuring sedation, changes in the anatomy and physiology of the airway take place, with a tendency to develop obstruction and collapse,9,10 in addition to hemodynamic variability secondary to drugs such as hypotension and bradycardia that increase the complications and the morbidity and mortality of patients under anesthesia.5,7,9,10 The review of training programs identified that the teaching of the basic principles of physiology and anatomy of the airway and the cardiovascular system improves the outcomes, the quality and safety during sedation.5–8
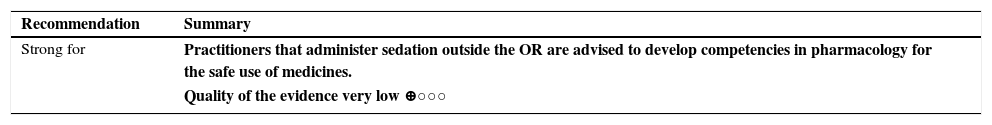
Pharmacology of sedationSedation is a balance between the patient's wellbeing, the effects of medicines used, and safety; hence, the practitioner who administers the sedation shall be knowledgeable about the medicines, any side effects thereof,9–11 the variables related to the type of patient and the procedure that modify the dosing. In this regard, during the sedation training, it is mandatory to include a theoretical module of sedation pharmacology.5–7
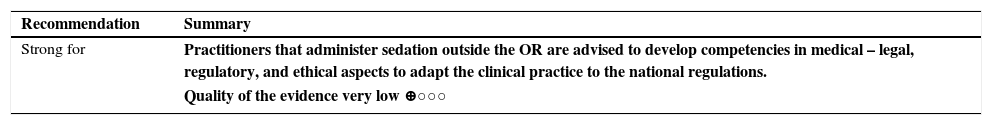
Legal, normative and ethical considerations of sedation outside the ORThe practice of administering sedation outside the OR has both medical and legal implications requiring the implementation of, and compliance with, sedation protocols, patient selection, and completion of the informed consent by the staff providing the sedation, in order to avoid and reduce any complications and medical-legal implications thereof.11 Consequently, all training programs should include a module on medical-legal aspects. 5–8
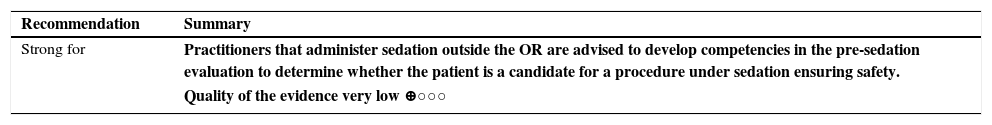
Pre-sedation evaluation and preparationThe patient evaluation prior to sedation is essential to making decisions about the management provided, and to administer safe and quality sedation.11,12 Therefore, a careful history must be obtained, including: patient comorbidities, prior use of medicines, addictions, allergies and family history of anesthesia-related complications, physical examination focusing on the cardio-respiratory system, neurological status, and airway. 5–8,12
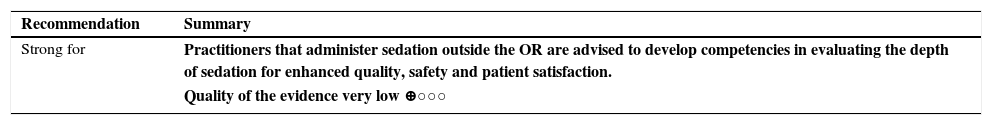
Evaluation of the depth of sedationThe ability to recognize and manage the various levels of sedation as a continuum is a management standard in the different training programs on sedation administered by non-anesthesiologists, in order to avoid safety conflicts,13,14 ensuring quality and patient satisfaction.6–8
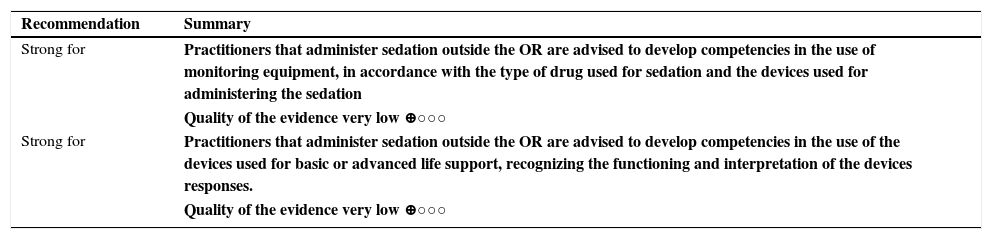
Interpretation and management of the basic monitoring equipment and devices for administering sedation outside the ORKnowledge of the correct functioning, use and interpretation of the devices during sedation are the basis for the proper administration and safety of sedation, as shown by the various training programs including a module for learning about the technology used for patient monitoring and management.13,14
| Recommendation | Summary |
| Strong for | Practitioners that administer sedation outside the OR are advised to develop competencies in the use of monitoring equipment, in accordance with the type of drug used for sedation and the devices used for administering the sedation |
| Quality of the evidence very low ⊕○○○ | |
| Strong for | Practitioners that administer sedation outside the OR are advised to develop competencies in the use of the devices used for basic or advanced life support, recognizing the functioning and interpretation of the devices responses. |
| Quality of the evidence very low ⊕○○○ |
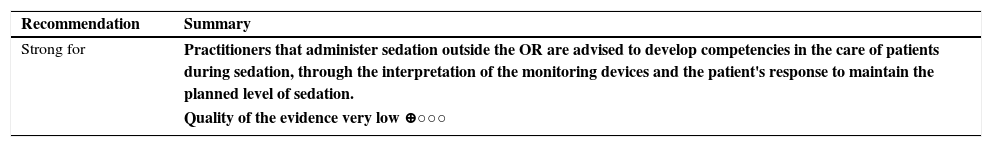
Interpreting the physical findings of the patients as reported by the monitoring devices during the administration of medicines used for sedation, allows an adequate sedation process. Sedation training programs should include the evaluation of these skills during supervised practice, using high fidelity simulators.6–8,12–14
| Recommendation | Summary |
| Strong for | Practitioners that administer sedation outside the OR are advised to develop competencies in the care of patients during sedation, through the interpretation of the monitoring devices and the patient's response to maintain the planned level of sedation. |
| Quality of the evidence very low ⊕○○○ |
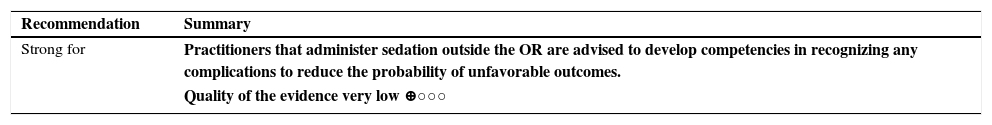
Diagnostic and therapeutic procedures performed under sedation outside the OR may give rise to both low impact complications (post-sedation nausea and vomiting) and high impact complications (cardiac arrest, severe respiratory depression, airway obstruction), and practitioners administering sedation outside the OR must be skilled to manage those complications.
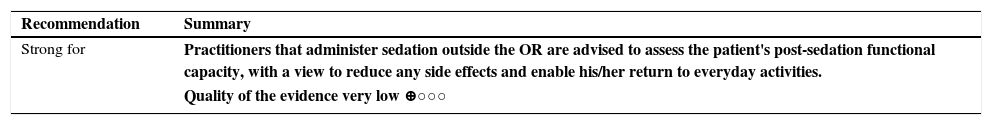
Post-sedation care and patient dischargeDischarge following sedation must be subject to returning to the prior physiological variables with minimal side effects or patient malaise so that the patient may be able to return to his/her usual activities; consequently, every training program shall include this last step in any patient intervention.5–8
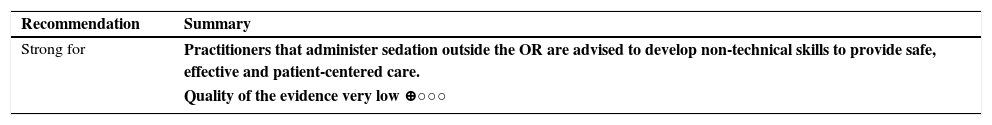
Non-technical skills in sedation outside the ORHealthcare workers should have a high level of medical knowledge, technical and non-technical skills for safe, effective and patient-centered care, including communication skills, team work and professionalism.15,16
Curricular contentsObjectiveTo suggest the necessary ingredients for structuring a training program for the development of the necessary competencies for the ethical and skillful practice of administering sedation outside the OR. The suggested curriculum is intended to develop clinical judgment and, technical and non-technical skills.6
Target populationIn accordance with the systematic literature review, the proposed curriculum focuses on the training of physicians and dentists5–8,17–21 with prior certification of basic and advances cardiovascular support (BLS and ACLS),14 and for those trained as exclusive Nitrous Oxide providers in BLS.
Healthcare environmentThe setting for practice of the above-mentioned practitioners is outside the OR, in areas where diagnostic or therapeutic procedures are performed in patients over 12 years old, such as21:
- •
Dental, dermatology or gynecology offices.
- •
Laboratories of electrophysiology or vascular ultrasound.
- •
Endoscopy, cardiac catheterization, dialysis, diagnostic imaging, and interventionist radiology units.
- •
Emergency departments and other services where sedation outside the OR is provided.
A training program should be “semi” in person with a variable duration in accordance with the drug to be administered.22–24 It should include a theory module that can be in person and autodidactic. The in person sessions shall include a review of the theory of the guidelines with instructors and workshops for discussing cases related with the clinical practice guidelines.8
The theory module must be 80% in person (Decree 4904 year 2009 of Education Ministry), lasting 22h for exclusive suppliers of nitrous oxide and for other drugs, including Propofol, 96h. The participant shall study the Clinical Practice Guidelines for the Administration of Sedation Outside the OR in patients over 12 years old25 and some supplement material reviewing the basics such as6,8,22:
- •
Introduction (sedation as a continuum).
- •
Anatomy and cardiopulmonary physiology.
- •
Pharmacological foundations in sedation (pharmacokinetics and pharmacodynamics).
- •
Physical examination and medical record.
- •
Ethical and legal considerations in sedation (informed consent).
- •
Contraindications for the use of sedation outside the OR (risk classification).
- •
Technical requirements for the provision of sedation services.
- •
Non-technical skills in sedation outside the OR.
- •
Management and preparation of devices for the procedure.
- •
Monitoring (clinical and basic) of patients.
- •
Sedation scales.
- •
Recognition and initial management of sedation-associated complications.
- •
Choice and dosing of agents used for sedation.
- •
Post-sedation care and patient discharge.
- •
General recommendations for the post-sedation patient.
The practice module of the program shall be under the supervised training modality. First with the support of high fidelity simulators, with a maximum of 4 students per instructor6 in settings including preparation for sedation, proper management of drug-related hemodynamic and respiratory complications and management of effective communication with the patient and the healthcare team.20 Second, practice in the basic and advanced airway management in the OR.20,22,24 And third, the program shall include the administration of sedation in groups of 2 students under the supervision of the instructor.6,23,24
In accordance with the type of drug to be administered, the period of time of practical training may vary24:
- •
Suppliers of exclusive nitrous oxide sedation: 18h of supervised practice and 8h of BLS. Adding the theory and the practical modules, both account one academic credit (48hours) equivalent to a semester 3-h per week subject.
- •
Suppliers of other sedatives: 96h of practical work (56 in high fidelity simulator and 40h in the OR, with supervised practice of observation and airway management in groups of two students under the guidance of one anesthesiologist). The theory and practical modules are equivalent to four academic credits.
- •
Suppliers of sedation with propofol: in addition to the above requirements, a 96-h supervised practice or 70 cases of sedation with propofol per student are mandatory. The theory and practical modules are equivalent to six academic credits.
The team of program instructors includes: anesthesiologists, a specialist in the type of intervention to be performed, and one specialist in medical law.
Competencies evaluationThe process of evaluation of the training program will include acknowledgment of the development of competencies and meeting the performance criteria at the various stages of the course. Therefore, learning progress is evaluated throughout the course, and at the end of the process a comprehensive evaluation shall determine the level of comprehension and skills developed by the participant versus the expected standard.
The following techniques are recommended for evaluating the learning process:
- •
Initial test pre and post completion of each module or topic of the guidelines taught via the internet platform or any other means, during the theory phase.6,21,22
- •
Solution of clinical cases addressing different diagnostic and therapeutic procedures under sedation, in addition to a review of the planning, implementation, documentation processes and patient discharge.
- •
Completion of the checklists by the participants in cases of simulation. During supervised practice with actual patients, evaluation of the skills to recognize and manage the various events that may arise during sedation.
The comprehensive evaluation may comprise a written examination at the end of the course to evaluate knowledge, with a minimum passing grade of 80/100 points, in addition to complying with the number of hours or number of patients established.
It is also important for the participants to evaluate the contents, the teaching strategy, and other aspects regarding the course organization.
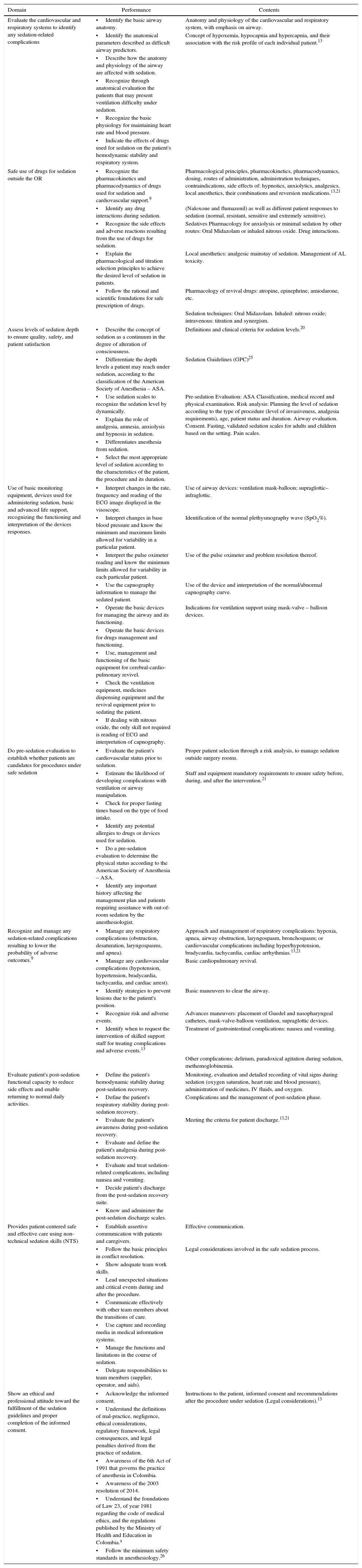
Competencies and program contentsUpon completion of training and education, participants are expected to master the knowledge, skills, attitudes and responsibilities regarding the administration of sedation. The training program shall focus on the following domains, level of performance and contents: (Table 1)
Curriculum for sedation outside the operating room.
| Domain | Performance | Contents |
|---|---|---|
| Evaluate the cardiovascular and respiratory systems to identify any sedation-related complications | •Identify the basic airway anatomy. | Anatomy and physiology of the cardiovascular and respiratory system, with emphasis on airway. |
| •Identify the anatomical parameters described as difficult airway predictors. | Concept of hypoxemia, hypocapnia and hypercapnia, and their association with the risk profile of each individual patient.13 | |
| •Describe how the anatomy and physiology of the airway are affected with sedation. | ||
| •Recognize through anatomical evaluation the patients that may present ventilation difficulty under sedation. | ||
| •Recognize the basic physiology for maintaining heart rate and blood pressure. | ||
| •Indicate the effects of drugs used for sedation on the patient's hemodynamic stability and respiratory system. | ||
| Safe use of drugs for sedation outside the OR | •Recognize the pharmacokinetics and pharmacodynamics of drugs used for sedation and cardiovascular support.9 | Pharmacological principles, pharmacokinetics, pharmacodynamics, dosing, routes of administration, administration techniques, contraindications, side effects of: hypnotics, anxiolytics, analgesics, local anesthetics, their combinations and reversion medications.13,21 |
| •Identify any drug interactions during sedation. | (Naloxone and flumazenil) as well as different patient responses to sedation (normal, resistant, sensitive and extremely sensitive). | |
| •Recognize the side effects and adverse reactions resulting from the use of drugs for sedation. | Sedatives Pharmacology for anxiolysis or minimal sedation by other routes: Oral Midazolam or inhaled nitrous oxide. Drug interactions. | |
| •Explain the pharmacological and titration selection principles to achieve the desired level of sedation in patients. | Local anesthetics: analgesic mainstay of sedation. Management of AL toxicity. | |
| •Follow the rational and scientific foundations for safe prescription of drugs. | Pharmacology of revival drugs: atropine, epinephrine, amiodarone, etc. | |
| Sedation techniques: Oral Midazolam. Inhaled: nitrous oxide; intravenous: titration and synergism. | ||
| Assess levels of sedation depth to ensure quality, safety, and patient satisfaction | •Describe the concept of sedation as a continuum in the degree of alteration of consciousness. | Definitions and clinical criteria for sedation levels.20 |
| •Differentiate the depth levels a patient may reach under sedation, according to the classification of the American Society of Anesthesia – ASA. | Sedation Guidelines (GPC)25 | |
| •Use sedation scales to recognize the sedation level by dynamically. | Pre-sedation Evaluation: ASA Classification, medical record and physical examination. Risk analysis: Planning the level of sedation according to the type of procedure (level of invasiveness, analgesia requirements), age, patient status and duration. Airway evaluation. Consent. Fasting, validated sedation scales for adults and children based on the setting. Pain scales. | |
| •Explain the role of analgesia, amnesia, anxiolysis and hypnosis in sedation. | ||
| •Differentiates anesthesia from sedation. | ||
| •Select the most appropriate level of sedation according to the characteristics of the patient, the procedure and its duration. | ||
| Use of basic monitoring equipment, devices used for administering sedation, basic and advanced life support, recognizing the functioning and interpretation of the devices responses. | •Interpret changes in the rate, frequency and reading of the ECG image displayed in the visoscope. | Use of airway devices: ventilation mask-balloon; supraglottic–infraglottic. |
| •Interpret changes in base blood pressure and know the minimum and maximum limits allowed for variability in a particular patient. | Identification of the normal plethysmography wave (SpO2%). | |
| •Interpret the pulse oximeter reading and know the minimum limits allowed for variability in each particular patient. | Use of the pulse oximeter and problem resolution thereof. | |
| •Use the capnography information to manage the sedated patient. | Use of the device and interpretation of the normal/abnormal capnography curve. | |
| •Operate the basic devices for managing the airway and its functioning. | Indications for ventilation support using mask-valve – balloon devices. | |
| •Operate the basic devices for drugs management and functioning. | ||
| •Use, management and functioning of the basic equipment for cerebral-cardio-pulmonary revivel. | ||
| •Check the ventilation equipment, medicines dispensing equipment and the revival equipment prior to sedating the patient. | ||
| •If dealing with nitrous oxide, the only skill not required is reading of ECG and interpretation of capnography. | ||
| Do pre-sedation evaluation to establish whether patients are candidates for procedures under safe sedation | •Evaluate the patient's cardiovascular status prior to sedation. | Proper patient selection through a risk analysis, to manage sedation outside surgery rooms. |
| •Estimate the likelihood of developing complications with ventilation or airway manipulation. | Staff and equipment mandatory requirements to ensure safety before, during, and after the intervention.21 | |
| •Check for proper fasting times based on the type of food intake. | ||
| •Identify any potential allergies to drugs or devices used for sedation. | ||
| •Do a pre-sedation evaluation to determine the physical status according to the American Society of Anesthesia – ASA. | ||
| •Identify any important history affecting the management plan and patients requiring assistance with out-of-room sedation by the anesthesiologist. | ||
| Recognize and manage any sedation-related complications resulting to lower the probability of adverse outcomes.9 | •Manage any respiratory complications (obstruction, desaturation, laryngospasms, and apnea). | Approach and management of respiratory complications: hypoxia, apnea, airway obstruction, laryngospasm, bronchospasm; or cardiovascular complications including hyper/hypotension, bradycardia, tachycardia, cardiac arrhythmias.13,21 |
| •Manage any cardiovascular complications (hypotension, hypertension, bradycardia, tachycardia, and cardiac arrest). | Basic cardiopulmonary revival. | |
| •Identify strategies to prevent lesions due to the patient's position. | Basic maneuvers to clear the airway. | |
| •Recognize risk and adverse events. | Advances maneuvers: placement of Guedel and nasopharyngeal catheters, mask-valve-balloon ventilation, supraglottic devices. | |
| •Identify when to request the intervention of skilled support staff for treating complications and adverse events.13 | Treatment of gastrointestinal complications: nausea and vomiting. | |
| Other complications: delirium, paradoxical agitation during sedation, methemoglobinemia. | ||
| Evaluate patient's post-sedation functional capacity to reduce side effects and enable returning to normal daily activities. | •Define the patient's hemodynamic stability during post-sedation recovery. | Monitoring, evaluation and detailed recording of vital signs during sedation (oxygen saturation, heart rate and blood pressure), administration of medicines, IV fluids, and oxygen. |
| •Define the patient's respiratory stability during post-sedation recovery. | Complications and the management of post-sedation phase. | |
| •Evaluate the patient's awareness during post-sedation recovery. | Meeting the criteria for patient discharge.13,21 | |
| •Evaluate and define the patient's analgesia during post-sedation recovery. | ||
| •Evaluate and treat sedation-related complications, including nausea and vomiting. | ||
| •Decide patient's discharge from the post-sedation recovery suite. | ||
| •Know and administer the post-sedation discharge scales. | ||
| Provides patient-centered safe and effective care using non-technical sedation skills (NTS) | •Establish assertive communication with patients and caregivers. | Effective communication. |
| •Follow the basic principles in conflict resolution. | Legal considerations involved in the safe sedation process. | |
| •Show adequate team work skills. | ||
| •Lead unexpected situations and critical events during and after the procedure. | ||
| •Communicate effectively with other team members about the transitions of care. | ||
| •Use capture and recording media in medical information systems. | ||
| •Manage the functions and limitations in the course of sedation. | ||
| •Delegate responsibilities to team members (supplier, operator, and aids). | ||
| Show an ethical and professional attitude toward the fulfillment of the sedation guidelines and proper completion of the informed consent. | •Acknowledge the informed consent. | Instructions to the patient, informed consent and recommendations after the procedure under sedation (Legal considerations).13 |
| •Understand the definitions of mal-practice, negligence, ethical considerations, regulatory framework, legal consequences, and legal penalties derived from the practice of sedation. | ||
| •Awareness of the 6th Act of 1991 that governs the practice of anesthesia in Colombia. | ||
| •Awareness of the 2003 resolution of 2014. | ||
| •Understand the foundations of Law 23, of year 1981 regarding the code of medical ethics, and the regulations published by the Ministry of Health and Education in Colombia.a | ||
| •Follow the minimum safety standards in anesthesiology.26 | ||
Resolution 1478 of 2006 of the Ministry of Social Protection, Resolution 2564 of 2008 of the Ministry of Social Protection, Resolution 1995 of 1999 on the management of the Medical Record. Health Statutory Act 1751 of 2015, Resolution 2003 of 2014, Law 1438 of 2011 on Education for Work of the Ministry of Education, Law 1164 of 2007 on Healthcare Human Resources, Decree 4909 of 2009 of the Ministry of Education.
Source: The authors.
This study was funded by the Colombian Society of Anesthesiology and Resuscitation (S.C.A.R.E.), and carried out by the Institute of Clinical Research, in collaboration with the Reviewer Team STI Cochrane of the Universidad Nacional de Colombia. Recommendations and opinions given on this paper are those of the authors and they do not necessarily reflect the S.C.A.R.E.’s opinon.
Conflicts of interestPrior to preparing this document, the authors completed a form to identify any conflicts of interest. The authors have no disclosures to make.
Please cite this article as: Rubiano-Pinzón AM, Burbano-Paredes CC, Hernández-Caicedo ÁC, Rincón-Valenzuela DA, Benavides-Caro CA, Restrepo-Palacio S, et al. Currículo para la administración de sedación fuera del quirófano en pacientes mayores de 12 años. Rev Colomb Anestesiol. 2017;45:239–250.
This paper comes from the complete version of “Clinical Practice Guideline with recommendations for the administration of sedation as part of diagnostic or therapeutic procedures outside the operating room in patients over the age of 12” which is available on the web-appendix.