Up to 80% of hemophilia patients present acute and chronic pain, mostly secondary to joint involvement. In Colombia there are no studies on the topic.
ObjectiveTo show the epidemiological profile, assessment and management of these patients in a referral hospital for the treatment of hemophilia.
MethodologyObservational descriptive study, based on case series. Patients older than 18 years with diagnosis of hemophilia who were evaluated between January 1st, 2013 and March 31st, 2016 were included. The qualitative variables were described with absolute frequencies and the quantitative variables with means.
Results196 hemophilia patients were registered in the trial; 87%, males and 13% females; the average age was 39 years. Hemophilia A 79%, hemophilia B 18%, carriers 3%. The causes for admission were 45% surgical, 37% medical and 17% trauma. The average hospital stay was 8 days (range 1–58) and 2 hospital admission per year (range 1–5). No pain evaluation scales were used in 71% of the cases and 29% were administered the Visual Analogue Scale. Opioids were prescribed in 58% of cases, acetaminophen in 67%, and pregabalin in 5.6%. Only 33 patients were treated by the pain clinic.
ConclusionsNotwithstanding the presence of pain and the frequency of functional sequelae among hemophilia patients, most of them were not assessed by the pain clinic and no pain evaluation scales were used. The pharmacological management was based on the prescription of opioids and acetaminophen.
Los pacientes con hemofilia presentan dolor agudo y crónico hasta en un 80% de los casos, secundario principalmente a compromiso articular. En Colombia no existen estudios referentes al tema.
ObjetivoMostrar el perfil epidemiológico, evaluación y manejo en un centro hospitalario de referencia para manejo de hemofilia.
MetodologíaEstudio observacional descriptivo tipo serie de casos. Se incluyeron pacientes mayores de 18 años con diagnóstico de hemofilia valorados entre el 1 de enero de 2013 y el 31 de marzo de 2016. Las variables cualitativas fueron descritas con frecuencias absolutas y relativas y las cuantitativas con medias.
ResultadosSe registraron 196 pacientes con hemofilia; género masculino 87%, femenino 13%; edad promedio 39 años; hemofilia A 79%, hemofilia B 18%, portadoras 3%. Las causas de ingreso fueron: quirúrgicas 45%, medicas 37% y traumáticas en 17%; estancia promedio de 8 días (rango 1-58) y 2 hospitalizaciones por año (rango 1-5). En el 71% no se utilizó ninguna escala de valoración del dolor, en el 29% se utilizó la Escala Visual Análoga. Se prescribieron opioides en el 58%, acetaminofén en el 67% y pregabalina en el 5,6%. Solo 33 pacientes fueron manejados por la clínica de dolor.
ConclusionesA pesar de que la presencia de dolor y sus secuelas funcionales son frecuentes en pacientes con hemofilia, en su mayoría no fueron valorados por clínica de dolor, ni tampoco se utilizaron escalas para valoración del mismo. El manejo farmacológico se basó en la prescripción de opioides y acetaminofén.
In 1979, the International Association for the Study of Pain (IASP) defined pain as an “unpleasant sensory and emotional experience, associated with real or potential tissue damage, or described in terms of such damage”.1 Pain may be classified in terms of time as acute or chronic and it is considered a factor that impairs the quality of life of patients and may be potentially disabling. So currently, and in accordance with the World Health Organization (WHO), pain is considered the fifth vital sign and pain treatment and relief is a fundamental right of people who are in pain.2
Patients diagnosed with hemophilia present clinically with acute and chronic pain in up to 80%3 of the cases, usually associated with repeated episodes of hemarthrosis,4–6 with significant impact on quality of life; therefore, pain should be assessed and timely treated by a multidisciplinary team.3 Most of the trials focusing on this issue are descriptive in nature and the clinical trials that assess pain in this group of patients are really few as compared to other chronic arthropathies such as rheumatoid arthritis7,8 and specifically refer to non-pharmacological interventions such as acupuncture and hydrotherapy, although drug therapies have also been evaluated, including COX-2 inhibitors (celecoxib)9,10 and opioids.3,11
In Colombia we have no studies describing or assessing pain management in hemophilia patients, thus we feel it is important to learn about the epidemiological profile of this group of patients, the way pain is assessed, the treatment administered, and the clinical response to treatment at a national referral center specialized in the diagnosis and treatment of hemophilia.
MethodologyDesignA case series type of observational descriptive trial was performed.
PopulationPatients older than 18 years of age with a diagnosis of hemophilia, evaluated in-hospital or as outpatients at a fourth level hospital in Bogotá, from January 1st, 2013 through March 31st, 2016.
ProcedureWith the collaboration of the systems and statistics department, the charts of patients with a diagnosis of hemophilia and admitted to the hospital were obtained. The medical records were reviewed and the socio-demographic variables were established; age, sex, level of education, profession, social level, health care provider institution, and place of origin. Clinical variables were also considered including type of hemophilia, level of factors and inhibitors, condition of carrier, reason for consultation, diagnosis at admission and comorbidities; date of admission and discharge, hospital length of stay, and number of hospital admissions per year. The type and severity of pain was also recorded based on the VAS; pharmacological management: opioids (equivalent morphine dose per day – DEMO), non-steroidal anti-inflammatory drugs (NSAIDs), and neuromodulators; non-pharmacological management; side effects and complications of the treatment received; opioid addiction and associated psychiatric conditions.
The study was approved by the institutional ethics committee.
Statistical analysisThe qualitative variables were described in terms of absolute and relative frequencies. The quantitative variables sere described as means. The Stata 13 statistical package was used.
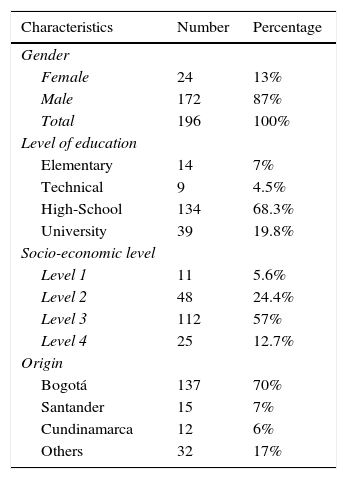
ResultsDemographic variables196 patients were included in the trial; the average age was 39 years old (range: 18–82 years), males 87% (172) and females 13% (24), mostly original from Bogotá (70%) and Santander (8%) (Table 1).
Socio-demographic characteristics.
| Characteristics | Number | Percentage |
|---|---|---|
| Gender | ||
| Female | 24 | 13% |
| Male | 172 | 87% |
| Total | 196 | 100% |
| Level of education | ||
| Elementary | 14 | 7% |
| Technical | 9 | 4.5% |
| High-School | 134 | 68.3% |
| University | 39 | 19.8% |
| Socio-economic level | ||
| Level 1 | 11 | 5.6% |
| Level 2 | 48 | 24.4% |
| Level 3 | 112 | 57% |
| Level 4 | 25 | 12.7% |
| Origin | ||
| Bogotá | 137 | 70% |
| Santander | 15 | 7% |
| Cundinamarca | 12 | 6% |
| Others | 32 | 17% |
Source: Authors.
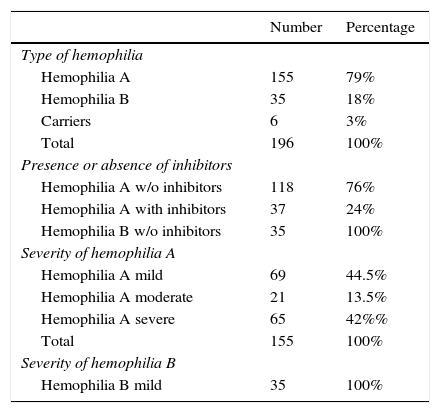
Of the 196 patients diagnosed with hemophilia, 79% (155) were classified as hemophilia A, 18% (35) hemophilia B, and 3% (6) as carriers. Patients with hemophilia A were classified as mild: 44.5% (69), moderate: 13.5% (21) and severe: 42% (65); hemophilia A were classified as without inhibitors 76% (118) and with inhibitors 24% (37) (Table 2).
Type and level of severity of patients with hemophilia.
| Number | Percentage | |
|---|---|---|
| Type of hemophilia | ||
| Hemophilia A | 155 | 79% |
| Hemophilia B | 35 | 18% |
| Carriers | 6 | 3% |
| Total | 196 | 100% |
| Presence or absence of inhibitors | ||
| Hemophilia A w/o inhibitors | 118 | 76% |
| Hemophilia A with inhibitors | 37 | 24% |
| Hemophilia B w/o inhibitors | 35 | 100% |
| Severity of hemophilia A | ||
| Hemophilia A mild | 69 | 44.5% |
| Hemophilia A moderate | 21 | 13.5% |
| Hemophilia A severe | 65 | 42%% |
| Total | 155 | 100% |
| Severity of hemophilia B | ||
| Hemophilia B mild | 35 | 100% |
Source: Authors.
In terms of comorbidities, 76% had no associated comorbidities, whilst 9% (17) were documented with C and 3% (6) were HIV+.
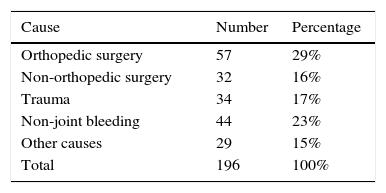
Based on the reason for consultation, the primary cause of admission was due to surgical pathology (45%), followed by medical pathology (37%) and trauma in 17% of cases. The average hospital stay was 8 days (range 1–58) with an average of 2 hospital admissions per year (range 1–5) (Table 3).
Pain assessment and managementOf the 196 patients, 86% (169) described somatic pain and 72% (143) were assessed by acute postsurgical pain. Pain severity was not assessed using a validated scale in 71% (140) of the cases and when one scale was administered, the visual analogue scale (VAS: 0–10) was used in 56 patients, of which more than 66% classified pain as severe (VAS 8–10) in the first evaluation.
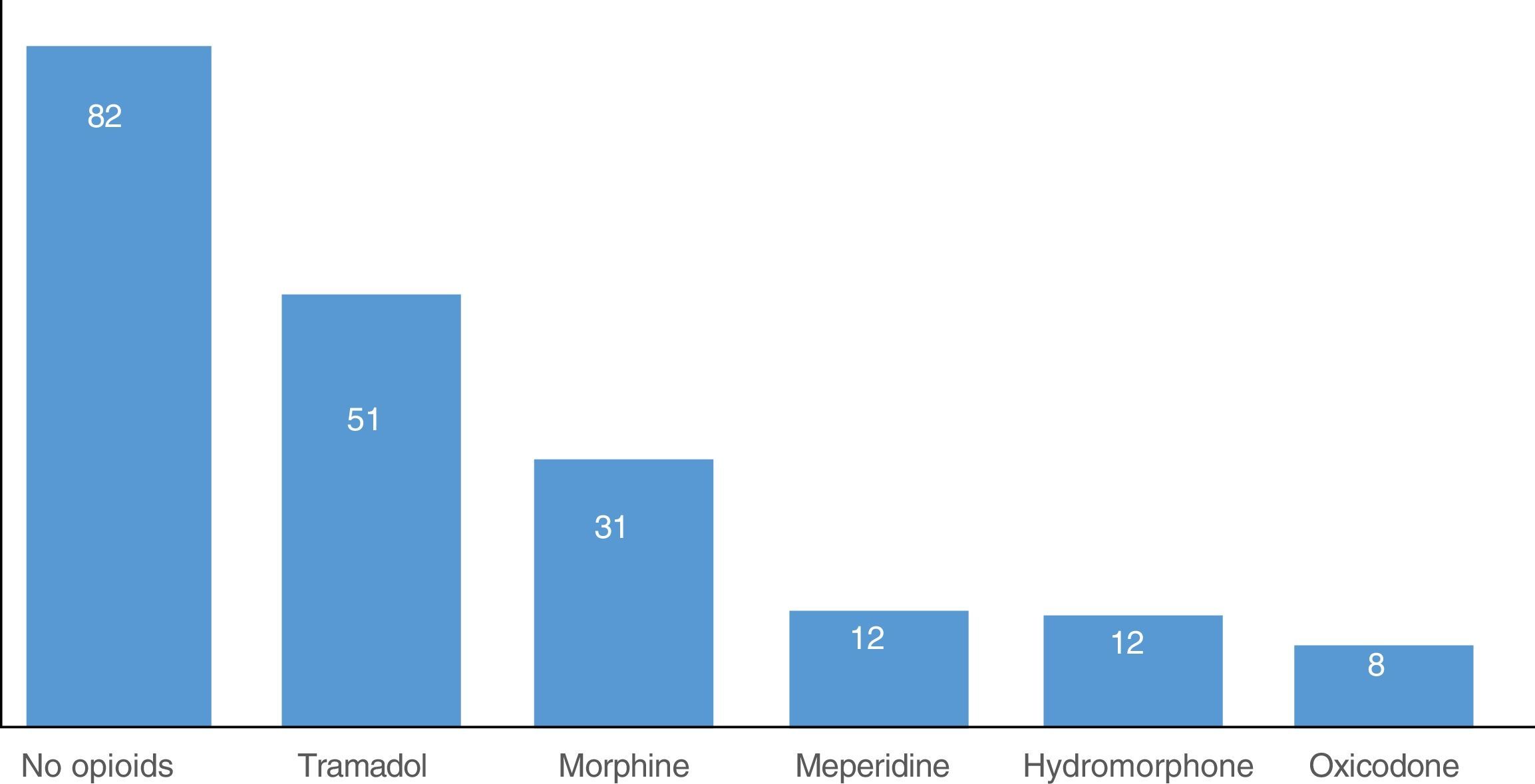
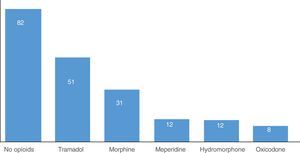
With regards to pain management, 58% (114) of the patients used opioids, tramadol being the most prescribed (50mg IV every 8h), followed by morphine (3mg every 6h for up to 30 days; DEMO mean dose 51mg/day, interquartile range 23–216mg/day).
Other drug groups such as NSAIDs were also used. The medication most widely used was acetaminophen in 67% of the cases; to a lesser extent dipyrone and diclofenac were also used (each in three cases, respectively). Pregabalin was the most frequently prescribed neuromodulator in 5.6%(11) of the cases (Fig. 1).
31.6% (62) of patients were evaluated by the rehabilitation service and physical respiratory and hydro-therapy were prescribed.
During the postop period, only 33 patients (17%) were evaluated by the Pain and Palliative Care Clinic. They all rated their pain as severe (VAS 8–10) and were treated with potent opioids: 45% (15) received morphine, 36% (12) hydromorphone, and 18% (6) oxycodone. Additionally, all patients received acetaminophen and 45% (15) of the cases also received neuromodulators: pregabalin in 27% (9), gabapentin and amitriptyline (3 cases respectively). All patients in this group were followed with the VAS scale, reporting a significant improvement (mild pain, VAS: 1–3) in up to 82% (27) of the cases. Almost all patients (32) were treated with physical therapy (sedatives, transcutaneous electrical nerve stimulation – TENS) and hydrotherapy. Opioids (72%) and acetaminophen (21%) were prescribed as ambulatory therapy. There were no adverse events reported secondary to treatment, but there was one case of opioid addiction (tramadol). Other diagnoses reported by psychiatry in these patients were: anxiety disorder 2% (5) and sleep disorder 1% (3).
DiscussionThe prevalence of hemophilia around the world is estimated at around 400,000 patients, 85% of which are hemophilia A, equivalent to one case per 10,000 births and hemophilia B, one case per every 100,000 births.12 According to the report: “The situation of Hemophilia in Colombia 2015”, of the Colombian fund of high-cost diseases, 3500 cases of patients with hemophilia and other coagulopathies have been reported in Colombia, of which 1525 are hemophilia A, 307 hemophilia B and 385 are carriers.13
A frequent reasons for consultation of these patients is the presence of hemarthrosis and/or muscle bleeding in up to 80% of the cases, in addition to bleeding at other sites (central nervous system, oropharynx, GI tract, etc.). Hinge joints, such as elbows and knees, are the most frequently affected; the former are the most compromised, with multiple bleeding episodes that result in severe and disabling pain, with major functional sequelae.6
In our patients, hemarthrosis and chronic arthropathy were the primary cause for consultation, with the knees being more frequently compromised (71% of the cases), giving rise to a significant number of surgical procedures (average 2 per year per patient) and an extended hospital stay (8 days in average).
Notwithstanding the functional involvement and disability as a result of poor pain control, a validated pain scale was not used in most of our patients, and no clear guidelines were documented for their management. Unfortunately this is not too different from the world situation: Holstein et al.14 administered a survey among 1687 patients younger than 18 years of age and 5103 adults in 22 hemophilia centers in various European countries. Among the adults, 1490 had arthropathy and 840 had chronic pain, but only 8 of the 12 centers administered a specific scale for pain evaluation and had pain management protocols. In another study, Witkop et al.15 reported inappropriate pain control (VAS 6/10) in up to 39% of a group of patients with hemophilia.
Despite the fact that VAS is not an adequate tool to assess pain in hemophilic patients, it is the scale most frequently used. However, there are studies published in the literature about specific scales for hemophilia patients11,16,17 such as “Hemophilia Joint Health Score” (HJHS),18 that should be implemented and used in every patient, since adequate pain evaluation is the foundation for optimal treatment of these patients.19
With regards to pharmacological pain management, opioids were the most frequently prescribed medicines in our population, in association with acetaminophen and in some cases with neuromodulators. Although there are no clear guidelines in the literature regarding pharmacological management for pain in patients with hemophilia, it is still considered appropriate to follow the recommendations of WHO analgesic ladder: for the first step for pain classified as mild, non-opioids analgesics shall be used, such as paracetamol or NSAIDs. If the response is not adequate, then escalate to mild opioids, and in there is no improvement, the next step shall be strong opioids.20 According to the trial by Holstein et al.14 first line therapy for managing acute pain was paracetamol and for chronic pain, the COX-2 inhibitors. The latter are recommended because of their anti-inflammatory activity but their use during acute bleeding is controversial.21 Acetaminophen is then a good option to control mild to moderate pain in patients with hemophilic atrophy, since it does not extend the bleeding times or inhibit the platelet function in vitro, but the liver function shall be monitored and the doses adjusted if the liver function is altered.16,22,23 Opioids to control chronic severe, non-cancer pain, are an excellent tool, but in the long term may result in side effects, as well as tolerance, dependence, and even abuse. The clinical data guiding the use of opioids for treating pain in patients with hemophilia are practically non-existent; therefore, the recommendation of the World Federation of Hemophilia with regards to their use – only when acetaminophen is ineffective and always assessing the risk–benefit ratio24–27 may be adopted.
Moreover, just one fifth of our patients were treated by the Pain Clinic, receiving a multimodal therapy associating strong opioids, acetaminophen, and in some cases neuromodulators. Additionally, non-pharmacological management was offered with physical therapy, TENS, sedative techniques and hydrotherapy, similar to the report by Witkop et al. (2012), who included the administration of coagulation factor and non-pharmacological measures such as rest, ice, compression, and elevation.15 It should be highlighted that 82% of the patients managed with a multidisciplinary approach, reported pain improvement down to a mild level (VAS 1–3).
Strengths and weaknesses of the studyOur study is the first study in Colombia that describes pain management in patients with a diagnosis of hemophilia. Since our hospital is a national referral center for hematology, our population is proportionally significant.
However, being an observational trial, it is impossible to arrive at any conclusions about pain evaluation and management in this type of patients and their final evolution. Moreover, there may be information biases because we relied on the information recorded in the medical records reviewed.
ConclusionsPatients with hemophilia frequently present with joint bleeding and secondary chronic arthropathy, reporting severe and debilitating pain, with serious functional sequelae. It is then necessary to implement specific pain assessment scales, as well as guidelines including pharmacological and non-pharmacological measures that are effective for the treatment of pain in patients with hemophilia. Pharmacological therapy is mainly based on multimodal analgesia with the association of opioids and other drugs such as acetaminophen. COX-2 inhibitors are a good option in chronic, less severe pain.
In view of the significant sequelae that may derive from poor pain control, it is essential to set up interdisciplinary teams for the evaluation, treatment, and rehabilitation of these patients.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study
Confidentiality of dataThe authors declare that no patient data appear in this article
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
FundingNo institutional funding was provided for this research study.
Conflicts of interestThe authors have no conflicts of interest to disclose.
Dr. Alejandra Ceballos and Dr. María Helena Solano: Instructors at the service for Pain and Palliative Care and Hematology of the Fundación Universitaria de Ciencias de la Salud – Hospital de San José, Bogotá, Colombia.
Please cite this article as: Pérez-Moreno DP, Buitrago CL. Dolor en pacientes con hemofilia: evaluación y manejo en un centro hospitalario de cuarto nivel. Serie de casos. Rev Colomb Anestesiol. 2017;45:24–29.