Pressure alopecia (PA) is an infrequent entity presented by patients undergoing extensive surgery.
ObjectiveTo report the case of a patient under 14 years of age undergoing orthopedic surgery of the pelvis and femur. Also, we present a review of the literature.
ResultsPA has been related to prolonged surgical time and possibly to the continuous pressure generated by head position during the intervention. It is considered a self-limiting adverse effect derived from anesthesia, which is clinically evidenced during the early postoperative period.
ConclusionEnsuring continuous repositioning of the patient's head during the procedure is the main recommendation for its prevention.
la Alopecia por Presión (AP) es una entidad de aparición poco frecuente, observada en pacientes sometidos a cirugías extensas.
Objetivopresentamos el caso de un paciente de 14 años con AP, sometido a cirugía ortopédica de pelvis y fémur, y adicionalmente, una revisión de la literatura existente.
Resultadosla AP se ha visto relacionada con el tiempo prolongado de los procedimientos quirúrgicos y posiblemente a la presión generada de forma continua por la posición de la cabeza durante la intervención. Se considera un evento adverso del acto anestésico, de manifestación clínica en el período posoperatorio temprano en la mayoría de los casos autolimitada.
Conclusiónla recomendación principal para la prevención de la AP es el cambio de posición de la cabeza durante el procedimiento.
Postoperative or Pressure Alopecia (PA) is the term used to describe a set of scars and alopecia that occur after ischemic changes in the scalp. It has a physiopathology similar to that of bedsores. The condition was first described by Lewis, who presented a series of eight cases in the annual meeting of the American Society of Dermatology in 19591. PA usually presents as a discrete area of alopecia, generally in the occiput, within a few weeks after surgery or prolonged stays in the Intensive Care Unit (ICU). Here, we present the case of a pediatric patient after an orthopedic surgical procedure.
Case descriptionMale patient, 14 years of age, secondary student with a history of bilateral hip dysplasia, left acetabular dysplasia, and bilateral coax valga. There were no reports of comorbidities or diseases of the scalp. Weight: 55kg, BMI: 20.5kg/m2. Performed triple osteotomy of the pelvis and left femoral varisation osteotomy. The procedure was performed under combined anesthesia (general and regional with peridural catheter) with the patient in the supine position. The anesthesia for the surgery lasted 5h, with no sign of hypotension or hypothermia. Bleeding was estimated at 300ml. There was no specific mention of the position of the head or its support in the anesthetic record.
During hospitalization, the patient did not present related symptoms such as headache or hair loss. No changes were observed in the physical examination. He was discharged in the second day of the postoperative period.
In follow-up, on the second check-up visit at 4 weeks after surgery, the patient reported symptoms that initiated 8 days after the procedure consisting of a 5×3 zone of alopecia in the central right parietal region (Fig. 1) with no other related symptoms. He was referred to dermatology, where expectant management was suggested.
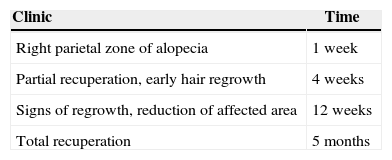
The patient reported signs of partial recuperation at 12 weeks (Fig. 2) and progressive recuperation in following check-ups. In the 5-month check-up, complete recuperation from the symptoms can be observed (Fig. 3), and in following check-ups, there was no new alteration. The patient's progress is summarized in Table 1.
Although there is no definitive histopathological aspect for PA, a variety of findings have been described. Fibrosis with loss of hair follicles has been observed in patients with cicatricial alopecia. Others report chronic inflammation and granulomatous reactions to foreign bodies. Hanly et al2. found multiple follicles and hair with apoptotic bodies without inflammation. Since Abel's first papers1,3, more than 100 cases of PA have been recorded.
Reports are more common after heart surgery. Lawson et al.4 conducted searches for cases of PA after coronary bypass surgery in a reference center, finding an incidence of 7% in the retrospective study. In the prospective phase from the following year, an incidence of 14% was found in the patients. In the third year of the study, an incidence of 4% was found.
Lawson et al.4 were the first to report PA after surgery, and the duration of the procedure directly correlated with the probability of alopecia. In the study by Lee et al.5, the average time was 5.9h. When the head was turned every 30min during the procedure and after the operation, no cases of PA were reported4.
Boyer and Vidmar identified PA in a 79 year-old man who underwent surgery of the coronary arteries6. The biopsy of the scalp 4 weeks later showed fibrosis and inflammation of the superficial reticular dermis associated with follicles in the catagen stage. There was no necrosis of the cells of the pilous bulb in contrast with the findings of Abel and Lewis. There were also no reports of vasculitis.
In 1996, Steinmetz and Langemo7 measured occipital capillary perfusion pressures of 25 volunteers that had undergone coronary bypass surgery. They found it to be greater than the maximum normal capillary perfusion pressure, putting the patients at a risk of developing a bedsore in the occiput during surgery. They recommended regular repositioning during surgery, reiterating the recommendations of Lawson et al.4 twenty years before.
Abel and Lewis described 8 patients with hair loss in the vertex 28 days after gynecological surgery1. All patients had undergone surgery in the Trendelenburg position over a period of 3 or more hours. 5 patients experienced the formation of scabs and sensitivity on the scalp before hair loss. The authors conducted biopsies of the scalp and found vasculitis with atrophic hair follicles in areas of alopecia1. They posited that the force that the weight of patient's head exerts on the same area of the scalp during anesthesia produces the temporary occlusion of small blood vessels, which leads to hypoxia in this site. The temporary cessation of the activity of the hair follicles resulted in reversible alopecia of the affected zones. The hypothesis was demonstrated in animal models1.
In 1979, Poma published a new case of temporary PA after gynecological surgery8. The patient developed a seroma in the first day post-surgery in a zone that was later affected by alopecia.
Khalaf et al. reported PA in four patients that had been donators or recipients of liver transplants and four patients that underwent heart surgery9. Hanly et al. reported a case of temporary PA in a 21 year-old woman who underwent exploratory gallbladder surgery with a total time of 19h under anesthesia. The biopsy of the scalp found hair follicles in the catagen phase with apoptotic bodies in the follicular epithelium with no evidence of inflammation. They concluded that hypoxia secondary to pressure had caused all the hair follicles to enter into programmed cell death2.
Cases after trauma include a 23 year-old man that was unconscious in the ICU for 9 days after a motorcycle accident. The biopsy of the scalp, destroyed hair follicles, rich neutrophil infiltration, and a granulomatous reaction to foreign bodies10.
Ferran and Dharmarajah11 report on a case of PA after a direct closed trauma. A 27 year-old man who was trapped between a truck and a trailer for 10min with direct pressure to the head suffered hair loss shortly after his accident. 5 weeks later, he still had a zone of alopecia but recuperated over the following 5 months. It was concluded that the cutting and friction forces may have provoked the hair loss.
The phenomenon of PA is not exclusive to adults. It has been described in children and newborns after surgery and stays in the ICU. In 1977, Eldred reported two cases of alopecia after thoracic wall surgery12. Ben-Amitial and Garty13 described 3 cases of children between 10 months and 2 years of age that underwent heart surgery with intubation times of between 24h and 10 days. They developed scabs in the occipital scalp within a few days after the operation. Two had permanent alopecia.
The first descriptions of PA in the neonatal ICU appeared in 199314. 5 newborns with normal deliveries developed occipital bedsores that progressed to cicatricial alopecia. All had severe heart problems and had suffered episodes of hypoxemia/hypoperfusion. Physicians proposed the hypothesis that the hypoxia, acidosis, and the prolonged immobilization of the head had contributed to the development of the bedsores and the increase in the risk of PA. Poor nutrition may have been a contributing factor. The authors highlighted that alopecia can have lasting psychological effects on the children and their parents.
Lee et al.5 reported a series of 3 cases of adolescents, between 13 and 16 years of age, that were subjected to orthopedic surgery. They had a history of non-morbid obesity and underwent long proximal femoral osteotomies, which had an average duration of 6h. Hair loss presented 3 weeks after with recuperation between 8 and 12 months later.
Although it is rarely occurring pathological profile, PA is considered to be an adverse event that can be prevented with several methods, including repositioning the head during the procedure.
The therapeutic team is responsible for attentively following up with the patient if PA does occur since it can have serious effects on the patient and their family.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
FundingNone.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Galván-Villamarín F, Mahecha-Toro MT. Alopecia posoperatoria (por presión): reporte de un caso después de una cirugía ortopédica pediátrica y revisión de la literatura. Rev Colomb Anestesiol. 2015;43:241–244.