The axillary block of the brachial plexus is widely used as an anaesthesia and analgesia technique in upper limb surgery, specifically for hand, wrist and forearm procedures. The use of nerve stimulation and ultrasound guidance has increased the rate of success with this block.
ObjectiveThis article presents a non-systematic review of the most recent literature on axillary block of the brachial plexus using ultrasound and peripheral nerve stimulation.
Materials and methodsA search for a non-systematic review was conducted in the Cochrane, Pubmed/Medline, Embase and OVID databases.
ConclusionThe axillary block of the brachial plexus is an anaesthetic and analgesic technique for upper limb surgery that has a high percentage of success, with a low degree of difficulty for the procedure.
El bloqueo axilar del plexo braquial es un bloqueo anestésico ampliamente utilizado como técnica anestésica y analgésica en cirugía de miembro superior, específicamente para mano, muñeca y antebrazo. El uso de neuroestimulador y ultrasonido ha aumentado la tasa de éxito de éste bloqueo.
ObjetivoEl presente artículo hace una revisión no sistemática de la literatura más reciente relacionada con el bloqueo axilar del plexo braquial utilizando ultrasonido y estimulación de nervio periférico.
Métodos y MaterialesSe hizo una búsqueda en las bases de datos de Cochrane, Pubmed/Medline, Embase y OVID para la realización de una revisión no sistemática.
ConclusiónEl bloqueo del plexo braquial a nivel axilar es una técnica anestésica y analgésica para cirugía de miembro superior con alto porcentaje de éxito y bajo grado de dificultad en cuanto a realización del procedimiento.
The axillary block is a regional anaesthesia technique, involving blockade of the brachial plexus at the axillary level. It is widely used as an anaesthetic and analgesic technique in upper limb surgery, specifically for hand, wrist and forearm procedures. In the axillary block, the terminal branches of the brachial plexus are blocked. The use of nerve stimulation and ultrasound has increased the rate of success with this block1 and has reduced the incidence of complications. Unlike the inter-scalene and supra and infraclavicular blocks, the risk of injury to the stellate ganglion, pneumothorax or phrenic nerve palsy is practically non-existent with this block because of the site where the puncture is performed.2,3
MethodsA search was conducted in the Cochrane, Medline/Pubmed, OVID and EMBASE databases using the words axillary block, ultrasound, nerve stimulator, regional anaesthesia. Included in the search were meta-analyses, systematic reviews, clinical trials and non-systematic reviews, and articles in English, Spanish and French.
ResultsHistoryThe first percutaneous axillary block was described by Hirschel in 1911.4 In 1958, Burnham described how the axillary neurovascular bundle was enveloped by a fascia that could be “filled” with local anaesthetic.5 In 1961, De Jong referred to the axillary space as a pyramid of 42ml in volume, and described that the nerves and blood vessels were surrounded individually by septae.6 In 1979, Eriksson and Skarby used a tourniquet distal to the axillary injection site and, in 1984, Thompson and Rorie identified the brachial plexus septae in the axillary space as preventing the homogenous spread of the anaesthetic.7 More recently, cadaver studies using nuclear magnetic resonance have concluded that the terminal branches are lined by connective tissue and fascial sheaths that prevent the anaesthetic from flowing homogenously after a single injection and covering the entire plexus.8,9 The nerve stimulator was introduced in the 1990s, and ultrasound has been introduced in recent years10; their use has increased the rate of success with the axillary block. The use of nerve stimulation and ultrasound has also reduced the number of complications because of the smaller volume of local anaesthetic required to achieve blockade,11–13 although there are reports in which the use of ultrasound does not reduce the occurrence of complications when compared to the nerve stimulator.14 Complications associated with the axillary block include toxicity from the local anaesthetics15 and neurological and vascular injury,16,17 although there is a paucity of reports in the literature on these occurrences, supporting the theory that this block provides a high safety margin. Obesity increases the risk of vascular puncture and failure rates with this type of block.18
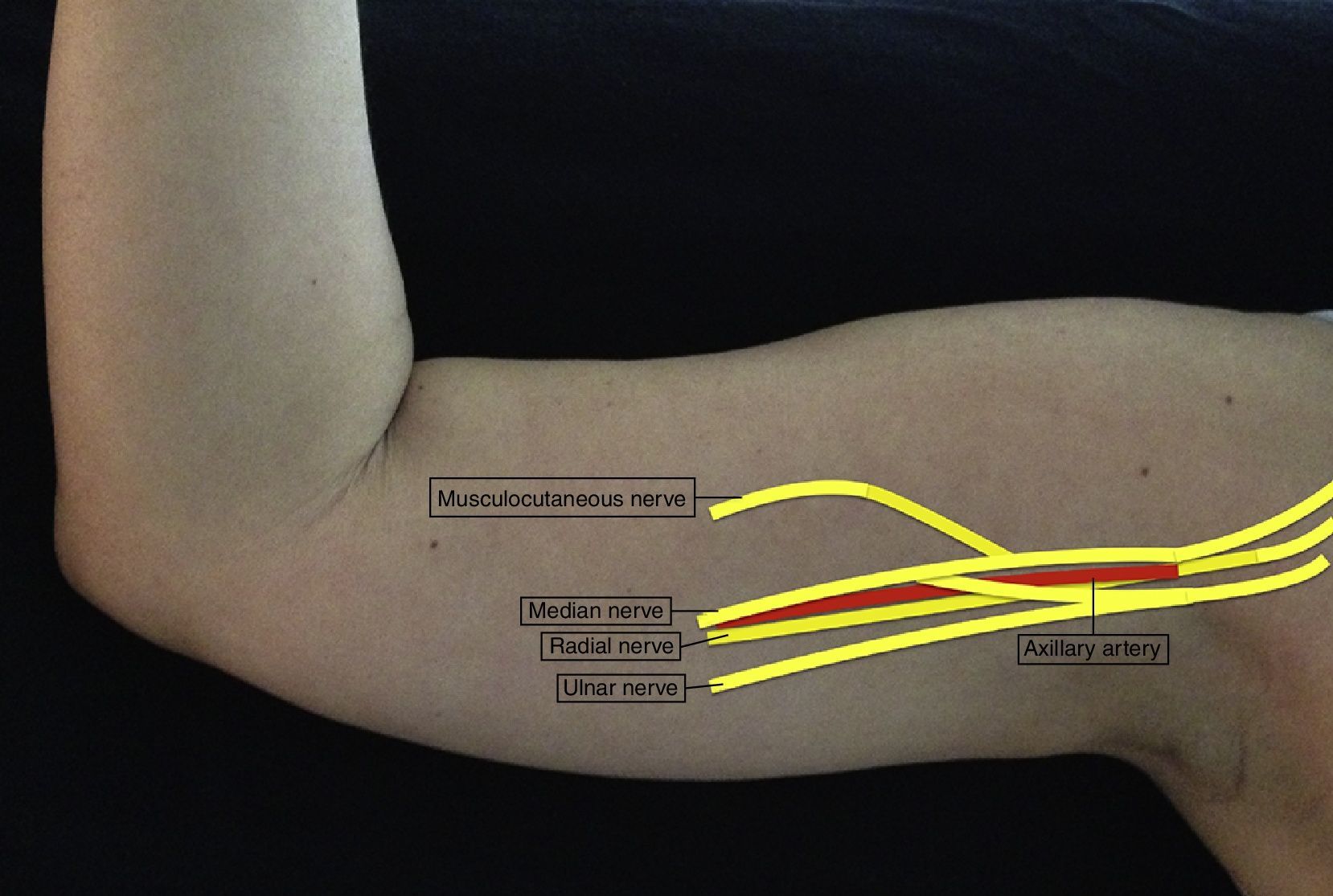
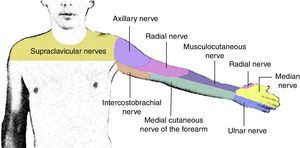
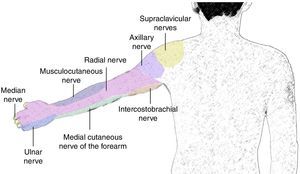
AnatomyThe brachial plexus arises from the ventral branches of C5 to C8. At the level of the scalene muscles, these branches regroup to form the superior, middle and inferior trunks, and when they leave the inter-scalene space, they form anterior and posterior divisions at the supraclavicular level. The divisions regroup again at an infraclavicular level to form the three lateral, posterior and medial cords which finally give rise to the five terminal branches at the axillary level: radial, axillary, musculocutaneous, median and ulnar nerves (Fig. 1).19
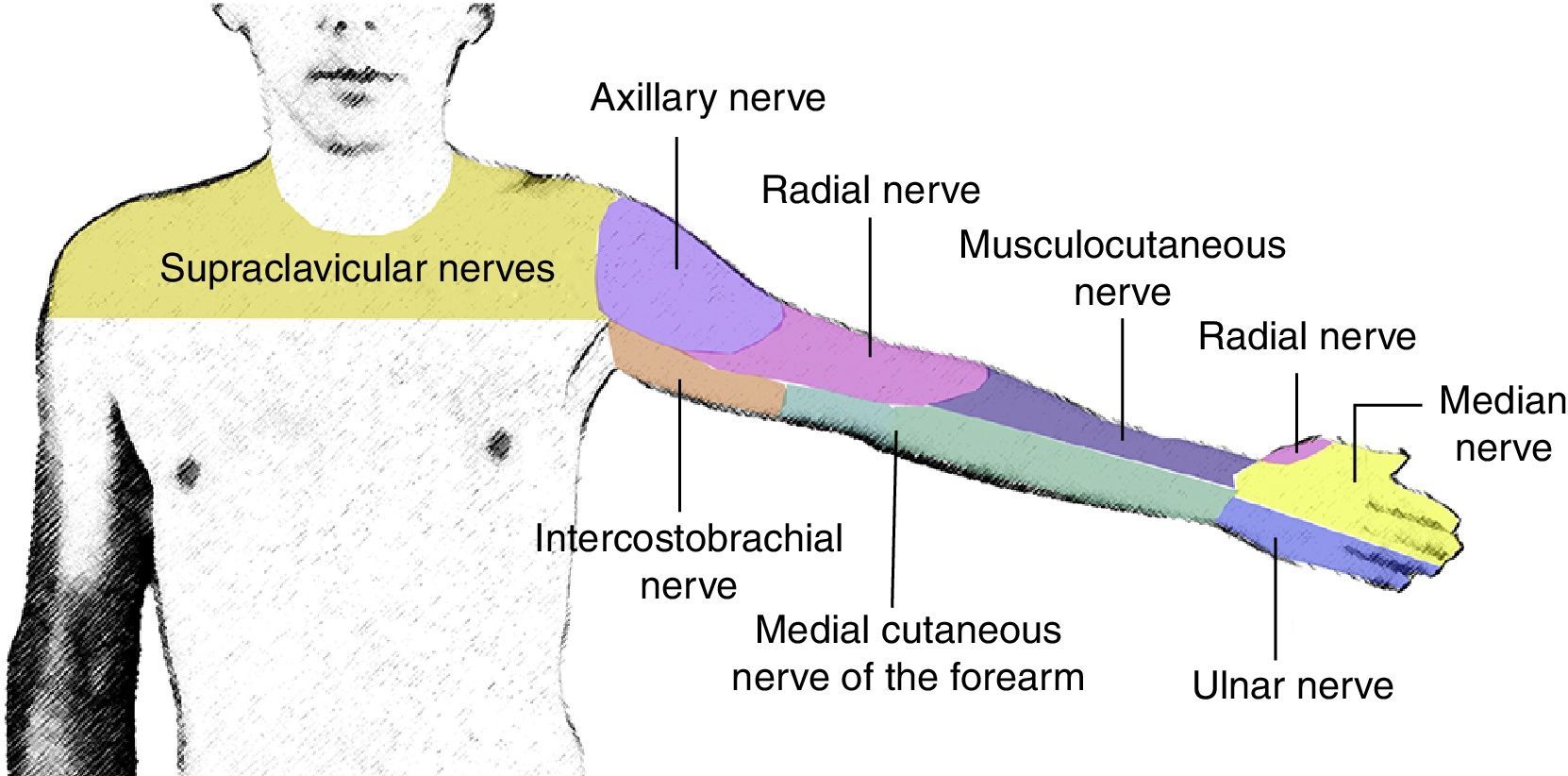
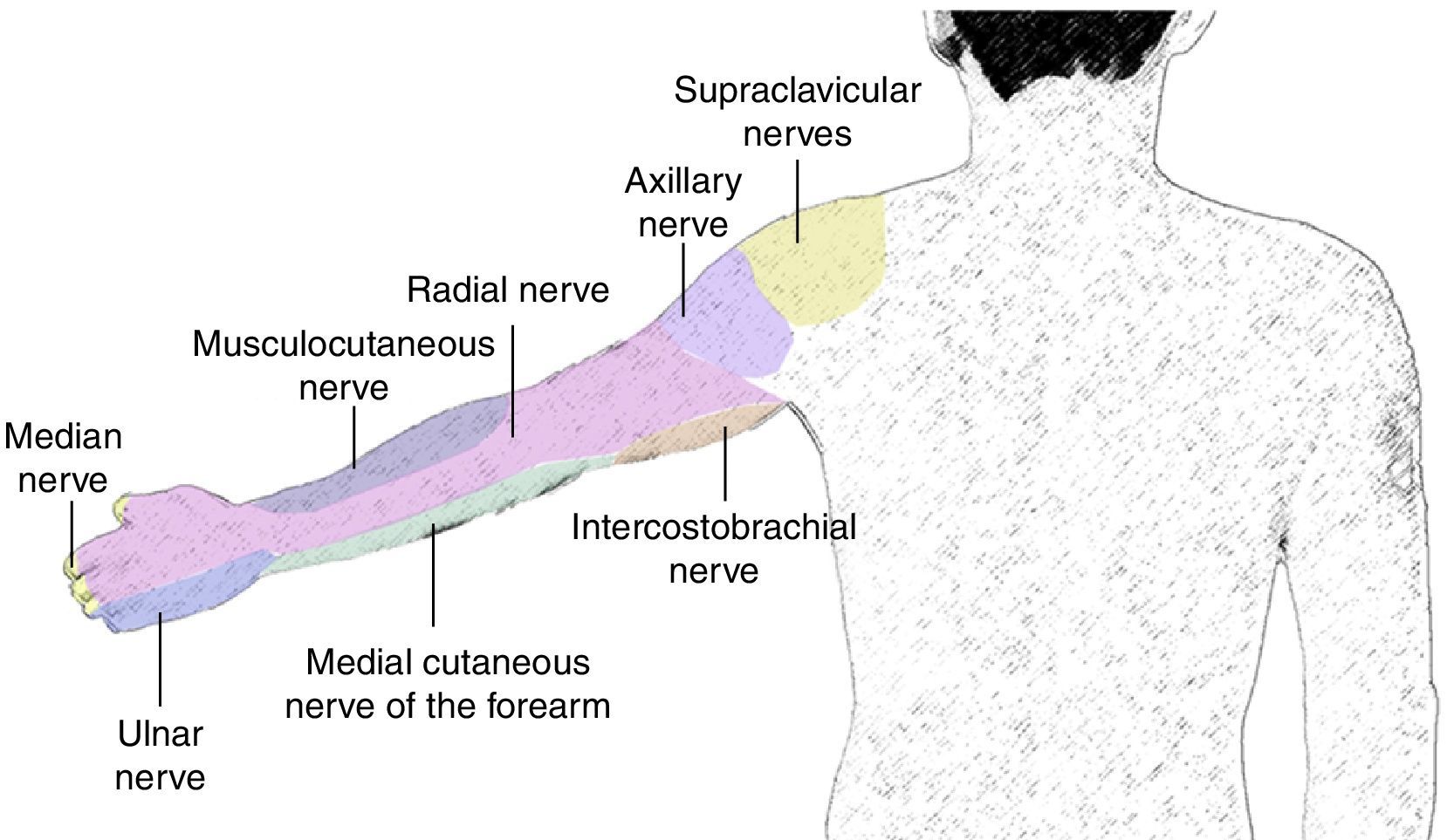
The radial nerve arises from the posterior cord. It runs together with the radial artery along its posterior aspect and breaks away from the neurovascular bundle at the axillary level in order to continue along the spiral humeral groove. It provides sensation to the posterior and lateral aspects of the arm and forearm down to the wrist, the lateral aspect of the dorsum down to the hand, the dorsal surface of the first three digits and half of the fourth digit. It provides motor innervation to the triceps and brachioradialis muscles and to the extensors of the posterior compartment of the forearm.
The axillary nerve arises from the posterior cord at the level of the coracoid process, forming an angle towards the deltoid muscle, which it innervates (Fig. 2).
The median nerve traverses most of the time superior to the axillary artery, while the ulnar and axillary nerves are found inferior to the axillary artery. The median nerve does not have cutaneous or motor branches in the arm, but in the forearm it provides motor innervation to the anterior compartment, except for the flexor carpi ulnaris and half of the flexor digitorum profundus. In the hand, it innervates the thenar eminence and the first two lumbrical muscles. It provides sensation to the lateral half of the hand and the dorsum of the first three digits, and half of the fourth finger down to the nail bed.
The ulnar nerve arises from the medial cord and it does not provide branches to the arm. It provides motor innervation to the flexor carpi ulnaris and the medial half of the flexor digitorum profundus. In the hand, it innervates all the small muscles except for the thenar eminence and the first two lumbricals. It provides sensitive innervation to the middle third of the palm, the dorsum of the fifth finger, and the medial aspect of the fourth finger.
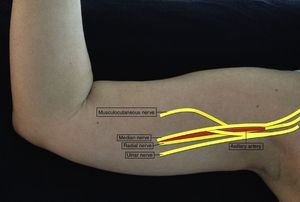
The musculocutaneous nerve arises from the lateral cord, perforates the coracobrachialis muscle and leaves the neurovascular sheath usually at the level of the lateral edge of the pectoralis major. It may be found outside the coracobrachialis muscle and joining the median nerve in 1 out of 5 individuals.20 It provides motor innervation to the coracobrachialis, biceps and brachialis muscles. At the elbow, it becomes a purely sensory nerve, innervating the anterior portion of the forearm down to the wrist (Fig. 3).
TechniqueThe axillary block is used in hand, wrist and forearm surgery. It is not as effective as other brachial plexus blocks in elbow surgery.21
The axillary block may be performed using a nerve stimulator, ultrasound or a combination of the two. With the use of the nerve stimulator, the failure rate is 5–30%, while the two techniques combined increase the success rate by up to 97%.22 As for the time required for performing the block, no significant difference has been found with the two techniques; ultrasound has allowed the use of a smaller local anaesthetic volume, although this affects the duration of the effect. One of the advantages of ultrasound is the ability to visualize the nerves – making blockade easier in patients with anatomic variants23 – and the spread of the local anaesthetic as it is injected.24 Complications associated with the axillary block appear to be less when ultrasound is used.25
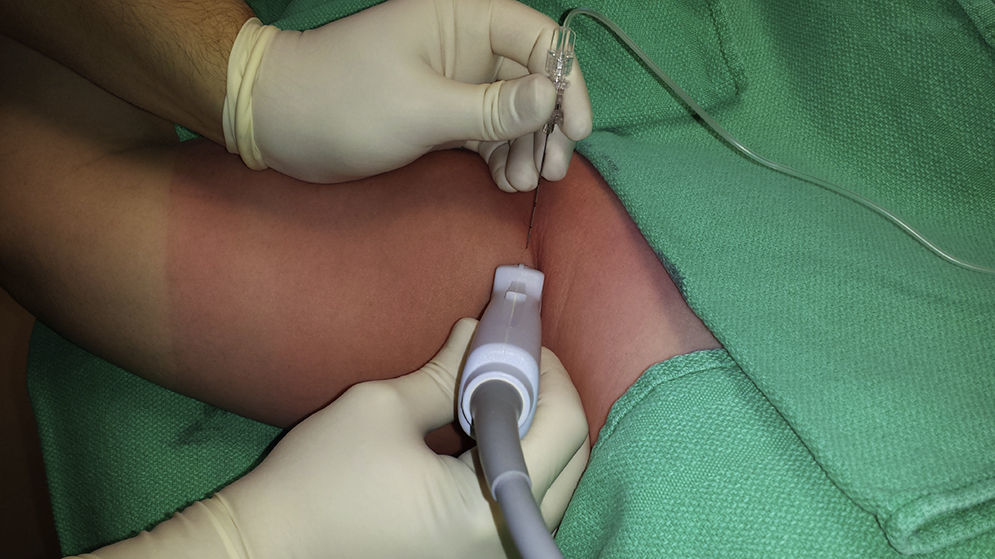
The patient is positioned in supine decubitus, with the arm in 90° of abduction and the forearm in flexion (Fig. 4). Asepsis must be performed up to the distal portion of the arm. A high frequency linear probe is placed on the transverse axis, over the axillary fold. The neurovascular bundle is localized 1–2cm underneath the skin.
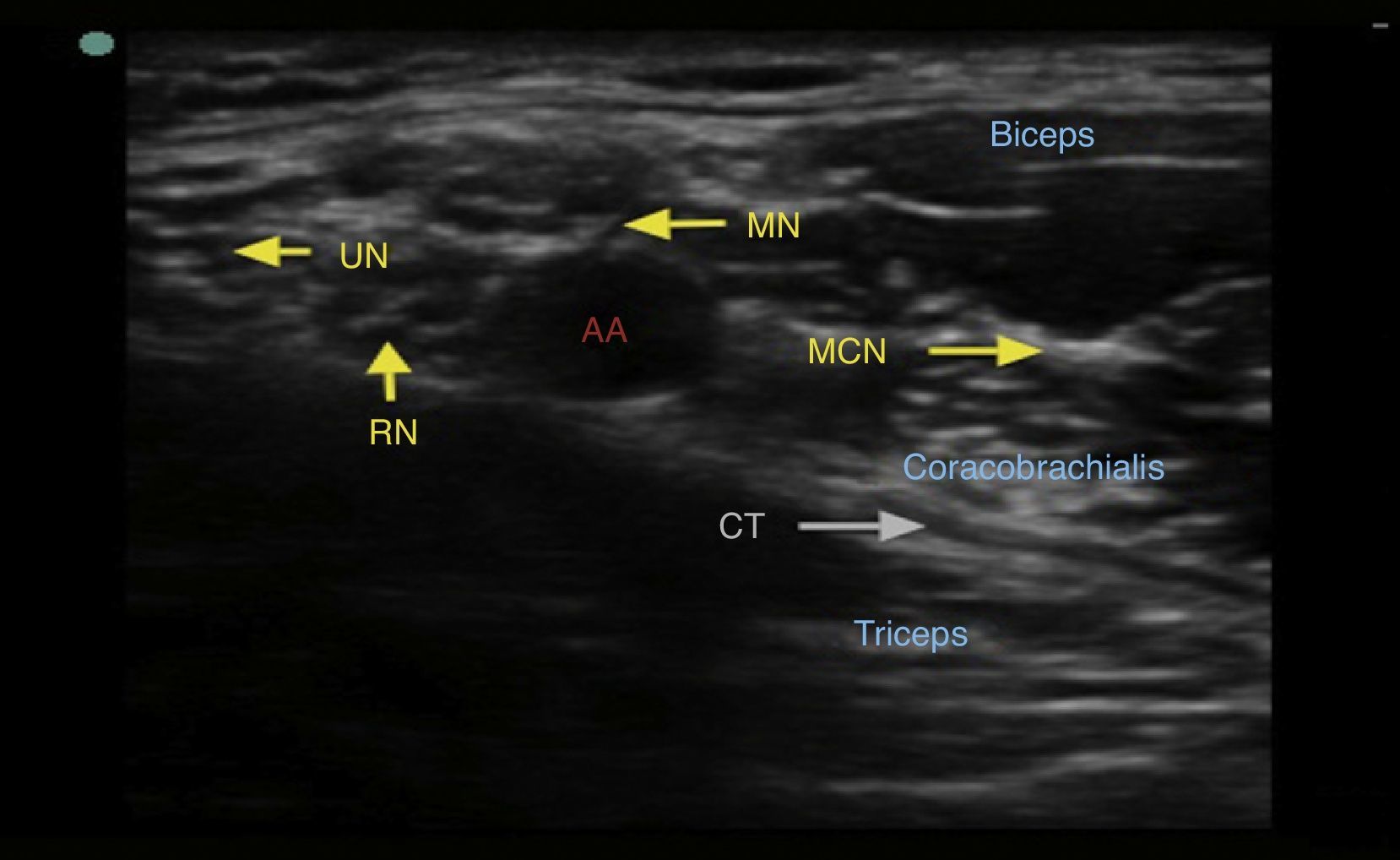
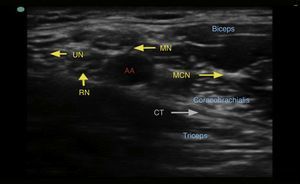
The axillary artery must be localized first. It provides a spherical, pulsatile hypoechoic image and it is not readily compressible. It is found over the conjoined tendon, formed by the junction of the latissimus dorsi and teres major tendons. It is important to identify the axillary vein, because it also provides a spherical and hypoechoic image, although it is not pulsating and is readily compressible. The median, ulnar and radial nerves are arranged around the artery. They appear as spherical or oval-shaped, hyperechogenic, hypoechogenic or beehive-like structures. Their position around the artery is not constant. The position of the radial and the median nerves in relation to the artery is usually constant.26 The radial nerve is located between 4 and 6 o’clock in 83% of cases, the median nerve is found between 9 and 12 o’clock in 88% of cases, and the ulnar nerve is between 12 and 3 o’clock in 85% of cases.27 The musculocutaneous nerve is usually separated laterally from the artery, between the short head of the biceps and the coracobrachialis muscle (Fig. 5).
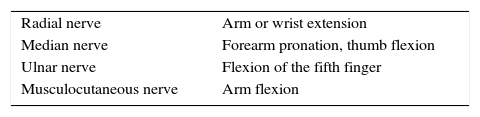
Once the structures have been identified under ultrasound, the skin is infiltrated with local anaesthetic and then, using a 50mm 22G nerve stimulator needle on an in-plane approach, the nerves are localized with the nerve stimulator (Table 1). There is no significant difference in terms of success using the echogenic or non-echogenic needle in this type of block.28 It is recommended to use a 0.5–1.0mA current in order to reduce the risk of dysfunction or nerve injury. Stimulation with a current of 0.3–0.5mA increases the success of the block and shortens the onset time, but increases the risk of nerve injury.29 When muscle stimulation is obtained with a 0.2mA current or less, an intraneural injection must be suspected to be likely.30 Once the corresponding muscle contraction is obtained, syringe aspiration is done in order to rule out intravascular injection, and then the local anaesthetic is injected, always under ultrasound guidance in order to visualize the deposition of the anaesthetic around the nerve.
Three ways of injecting the local anaesthetic at the axillary level have been described: a single injection, dual injection, and multiple injections to deliver the full volume of the anaesthetic. When a single injection is used, the anaesthetic is delivered under the axillary artery. In the dual injection, part of the dose is delivered under the artery and the other part is delivered around the musculocutaneous nerve.31 The most effective technique with less associated complications but the most time consuming is the multiple injections.22 The time to onset of the axillary block varies depending on the injection technique. In the study conducted by Lopez-Morales et al. comparing the axillary block with the inflaclavicular block, time to onset was significantly longer for the axillary block, at a mean of 10.2min.32 Blockade rate for the axillary, intercostobrachial and medial cutaneous nerves of the arm is lower through the axillary approach.33
The choice of the local anaesthetic depends on the duration of the block and the availability in the Anaesthesia service. Reducing the local anaesthetic concentration and increasing the volume prolongs the duration of the block.34,35 Levobupivacaine and ropivacaine have been used in concentrations of 0.375–0.75% and 0.25–0.5%, respectively. Compared to levobupivacaine, ropivacaine has a faster onset of action (9min vs. 12min) but blockade duration is shorter (9.2h vs. 11.3h).36 The total volume used ranges between 30 and 40ml when delivered in a single injection, and between 5 and 8ml when each nerve is anaesthetized individually. González et al. found that the MAC-90 of 1.5% lidocaine with epinephrine 5mcg/ml is 5.5ml and 23.5ml in the dual injection technique.37 The minimum effective volume (MEV90) of 0.5% bupivacaine is 1.56ml per nerve.38 The use of other additives to prolong the block, like using dexamethasone with the local anaesthetic, has shown to be an effective way to increase motor and sensory blockade.39,40 The use of clonidine as adjunct to the local anaesthetic has not been shown to increase block duration,41 different from dexmedetomidine which does appear to prolong axillary block duration.42,43 Magnesium sulphate has also been used as additive in axillary blocks, but has not been shown to improve block duration or efficacy.44 Other adjuncts such as ketamine and tramadol have also been used, and some studies have shown evidence that they prolong the action of the axillary block.45 There is recent evidence about the effect of hyaluronidase in shortening the time to onset of the axillary block in upper limb surgery.46
Continuous infusion of the local anaesthetic using catheters is not well documented in the literature.47,48 The axillary region is prone to catheter displacement and does not allow adequate fixation. The continuous infusion technique for the local anaesthetic has been used, but it is the surgeon who places the catheter under direct vision.49
It is recommended to add the intercostobrachial nerve block to the axillary block in order to increase tolerance of the tourniquet during the surgical procedure.50 This nerve is the cutaneous branch of the second intercostal nerve and provides sensory innervation to the upper portion of the medial and posterior aspects of the arm.
ConclusionThe brachial plexus block at the axillary level is an anaesthetic and analgesic technique used with a high degree of success in upper limb surgery, creating little difficulty for the procedure. The use of nerve stimulation and ultrasound has increased the rate of effectiveness of this block and reduced the rate of complications.
FundingNone.
Conflict of interestThe authors declare having no conflicts of interest.
Please cite this article as: Lopera-Velásquez LM, Restrepo-Garcés C. Bloqueo axilar guiado por ultrasonido y neuroestimulador. Rev Colomb Anestesiol. 2016;44:30–35.