Valproic acid is one of the most widely used drugs for the treatment of epilepsy in children and adults since early 1967 to the present, and it is also useful for the treatment of refractory epilepsy and multiple conditions.1 However, the use of this drug has been associated with blood disorders, including bone marrow suppression, alteration of the coagulation cascade and reduction of factor VIII and Von Willebrand factor, in addition to changes in the platelet numbers and function. In terms of the major surgery patient, all of these issues result in an increased risk of perioperative bleeding and a higher requirement of perioperative blood transfusion. A topic for discussion should then be whether the presence of these disorders is relevant for the morbidity and mortality of the patients and whether there is any clinical evidence of benefits for the patient when the drug is interrupted prior to surgery. Many hospital centers recommend stopping the use of valproic acid one to two weeks prior to surgery, though this recommendation is based on controversial evidence. It is our intent to submit a report of an abnormal uterine hemorrhage in the immediate postoperative period of curettage due to incomplete abortion with a history of chronic intake of valproic acid.
El ácido valproico es uno de los medicamentos más usados para el tratamiento de la epilepsia en niños y adultos desde inicios de 1967 hasta la actualidad, y es útil también para el tratamiento de epilepsia refractaria y múltiples enfermedades.1 Sin embargo, el uso de este medicamento se ha asociado con alteraciones hematológicas que incluyen supresión medular, alteración de la cascada de la coagulación, disminución del factor VIII y factor de Von Willebrand, y alteración del número y función de las plaquetas, que en el contexto del paciente llevado a cirugía mayor representa un aumento del riesgo de sangrado perioperatorio y mayor requerimiento de transfusión en el posoperatorio. Es entonces aún tema de discusión, si la presencia de estas alteraciones establece una relevancia en la morbimortalidad de los pacientes, y si existe evidencia clínica que la suspensión de este previo al procedimiento representa un beneficio para el paciente. Muchos centros hospitalarios recomiendan la suspensión del ácido valproico una a dos semanas previo al procedimiento quirúrgico, a pesar de que esta recomendación está basada en una evidencia controvertida. Es de nuestro interés presentar un reporte de caso de hemorragia uterina anormal en el postoperatorio inmediato de un legrado obstétrico por aborto incompleto con antecedente de ingesta crónica de ácido valproico.
This is a 29-year-old patient admitted to the ER of the University Hospital San Ignacio, Bogotá, because of a 12-h course of transvaginal bleeding associated with the hypogastrium and amenorrhea in a patient who underwent diagnostic ultrasound that evidenced incomplete 10-week abortion. The patient came to us for a uterine curettage. The underlying pathology of the patient – convulsive syndrome – had been treated with valproic acid 250mg every 12h for one year. The patient did not exhibit any hemorrhagic diathesis or menstrual disorders. She was admitted to the OR with normal blood pressure and tachycardia (heart rate 110bpm); the physical examination produced no relevant findings except for hypochromic conjunctivae. The procedure was performed under intravenous induction with fentanyl and propofol, and anesthesia was maintained with Sevoflurane administered through a facemask. The procedure was short and free from complications; the patient was transferred to the post-anesthesia ICU. After 10min the patient presented with abundant transvaginal bleeding and was therefore evaluated by the treating doctors who started crystalloid treatment and a bolus of 10 units of oxytocin in continuous infusion; however, the patient continued to bleed and an I.M. dose of methylergonovine was administered, with no favorable response. During this time the patient remained stable but tachycardia persisted as well as evident bleeding; so, considering a history of chronic valproic acid intake and the potential risk of diminishing clotting factors, a dose of 0.3mcg/kg of desmopressin was administered resulting in a considerable reduction of bleeding after 20min. No blood by-products transfusion was needed. Then a blood workup was requested with 8g/dL hemoglobin and 150,000 platelet count. Plasma valproic acid levels were not measured.
DiscussionValproic acid is a branched short chain fatty acid from valeric acid, extracted from valerian plant.1 It is an anticonvulsant used for treating a broad spectrum of focal and generalized epilepsies. It has further proven to be beneficial in multiple neurological pathologies, in the management of addictions to psychoactive drugs, in psychiatric diseases, cancer, and asthma, inter alia.2–4 Its mechanism of action consists in potentiating the inhibitory activity of the gamma-aminobutyric acid, attenuating the N-methyl d-aspartate mediated excitation and blocking the voltage dependent sodium, calcium and potassium channels.1 Therapeutic levels are achieved within a 50–100-mcg/ml range. Chronic use of this drug has been associated with hematologic, hepatic, and endocrine disorders, in addition to morphological changes in the capillaries of the brain and glial cells, recorded at values above 100mcg/ml.
Valproic acid causes bone marrow suppression, compromising the production of red blood cells and platelets and reducing platelet aggregation, prolonging the bleeding times, because of its toxic effect on the hematopoietic stem cells, exhibiting values over 120mcg/ml.5 Thrombocytopenia is one of the most frequent findings, with an incidence of 5–60%, secondary to a drop in platelet production or enhanced platelet consumption because of the presence of IgM type antibodies induced by the particular anticonvulsive agent.5–7 Szupera showed that the platelet aggregation decrease is due to the involvement of cyclooxygenases and arachidonic acid, in a similar action to that of NSAIDs, with a thromboxane A2 reduction.8 However, several studies indicate that the thrombocytopenia is not clinically significant since thrombopathic thrombocytopenia occurs with a platelet count below 50,000.5,6 There are case reports of patients with severe bleeding and valproic acid. Tetzlaff in 1991 published a case of a 12-year-old child with cerebral palsy and refractory epilepsy managed with valproic acid, phenitoine and phenobarbital, and who was surgically managed for muscle contractures of the lower limbs, a platelet count of 150,000 and normal clotting times. During the operation the patient lost 600ml of blood, which for a minor surgery with no bone involvement, suggests potential platelet pathology attributable to valproic acid.9 Likewise, in 2000 Sleiman published a case of a 30-year-old female patient with mental retardation and fatal pulmonary bleeding induced by thrombocytopenia secondary to valproic acid monotherapy, with a platelet count of 15,000 and valproic acid serum levels of 124mcg/ml.10
Other alterations in the coagulation cascade include decreased fibrinogen levels due to hepatic synthesis disorders, decreased vitamin K-dependent factors due to inhibition of the gamma-carboxylation of glutamic acid residues and of epoxy reductase, decreased factor XIII and reduction of Von Willebrand factor.1,2,5,6,11 Existing recommendations suggest treating with plasma-derived factor VIII concentrate, because the use of desmopressin has been associated with increased frequency of seizures and hyponatremia.6,12,13
Retrospective studies showed that the use of valproic acid causes more bleeding in orthopedic and neurological surgical procedures. In 2011, Manohar C evaluated 84 children who were managed with valproic acid and required surgery for refractory epilepsy. During the postoperative period, 28% of these patients exhibited abnormal blood measurements and 4.7% showed activates prothrombin and thromboplastin times within a range over 1.5 fold the range of reference, showing that there is a potential risk of bleeding.3 Likewise, Carney BT in 2005, revised the clinical records of 29 children with cerebral paralysis treated with valproic acid and undergoing bilateral femur osteotomy. 6 of them (21%) presented a decreased platelet count below 200,000, increased need for transfusion, and higher blood losses (>30cc/kg).14
The controversy of this discussion in based on two studies published in 1996 and 1997, showing that blood disorders are not clinically relevant. Anderson in 1997 published a trial with 313 patients who were subject to cortical surgery for treatment of refractory epilepsy, with no blood complications in the patients treated with valproic acid, even when there was a drop in red cells, hematocrit and hemoglobin, fibrinogen and platelet count.15 Similarly, Ward MM in 1996 presented a trial in 87 patients undergoing surgery for epilepsy, showing no significant differences in the estimated blood losses, the red cells count or the incidence of transfusion.16
With the evidence described and within the context of our patient, the chronic use of valproic acid could have been responsible for the outcome and the favorable response to treatment with desmopressin because of the increased factor VIII plasma levels and Von Willebrand factor that in turn reduced bleeding. It should be kept in mind that desmopressin does not affect platelet count but may enhance platelet adhesion to the vessel wall; however, it is difficult to determine a direct cause responsible for the perioperative bleeding in this patient.17
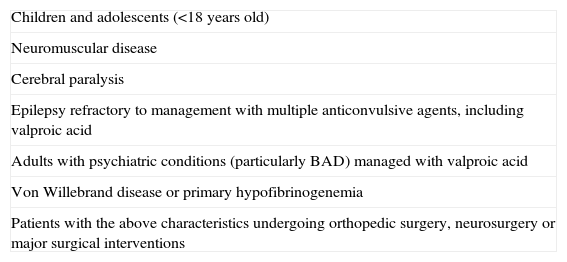
ConclusionThere are currently no studies establishing a direct relationship between valproic acid and the risk of perioperative bleeding. Keeping in mind that there is a potential association with increased bleeding in a particular group of patients (Table 1), they may continue receiving valproic acid, unless there is evidence of an abnormal preoperative hematology tests.
Patients at high risk of bleeding with chronic use of valproic acid.
| Children and adolescents (<18 years old) |
| Neuromuscular disease |
| Cerebral paralysis |
| Epilepsy refractory to management with multiple anticonvulsive agents, including valproic acid |
| Adults with psychiatric conditions (particularly BAD) managed with valproic acid |
| Von Willebrand disease or primary hypofibrinogenemia |
| Patients with the above characteristics undergoing orthopedic surgery, neurosurgery or major surgical interventions |
Source: Authors.
Authors’ own resources.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Fajardo A, et al. Ácido Valproico y riesgo de sangrado perioperatorio. Reporte de caso y revisión de la literatura. Rev Colomb Anestesiol. 2013;41:61–4.