We report the case of a 60-year-old female patient with a history of hypertension and dyslipidemia, who suddenly presented with a clinical picture of emotional lability, disorientation, complex visual hallucinations and persecutory delusions. There were no associated neurological findings in her initial physical examination. At a local hospital she was initially diagnosed with late-onset bipolar disorder and a manic episode with psychotic features, then referred to the mental health unit, where nuclear magnetic resonance (NMR) imaging of the brain revealed an acute ischemic stroke in the territory of the left posterior cerebral artery (PCA) with haemorrhagic reperfusion to the occipital cortex. Complete and spontaneous resolution of her clinical condition was achieved after approximately 15 days.
Se presenta el reporte de caso de una mujer de 60años de edad con antecedente de hipertensión arterial y dislipidemia, quien presenta cuadro clínico de inicio súbito consistente en labilidad emocional, desorientación alopsíquica global, alucinaciones visuales complejas e ideación delirante de tipo persecutorio, sin hallazgos neurológicos asociados en el examen físico inicial. Se enfocó en hospital local como un trastorno bipolar de inicio tardío con episodio actual maníaco con características psicóticas y es remitida a unidad de salud mental. Posteriormente hallazgos de resonancia magnética nuclear (RMN) cerebral revelaron una lesión correspondiente a ataque cerebrovascular (ACV) isquémico agudo en territorio de la arteria cerebral posterior (ACP) izquierda con reperfusión hemorrágica a nivel de corteza occipital. Se alcanzó una resolución espontánea completa de su cuadro clínico en un curso aproximado de 15días.
Although a “mimics” chart is that presented with the typical clinical features of a diagnosis, it actually corresponds to another aetiology. Stroke's more frequent mimics include seizures, migraine headaches, fainting, and metabolic disorders. By contrast, a chameleon clinical chart consists of those charts in which demonstrations are not typically expected, generally leading to diagnostic errors.1 Stroke is among the clinical conditions most frequently diagnosed as another; up to 20% of these errors occur in emergency rooms (ER), where the pressure of time windows for appropriate intervention represents great stress on the physician.2 This error rate can range between 4%3 and 64%,4 depending on the clinical population studied. Approximately 9% of the strokes are sub-diagnosed during their initial stages, especially when there are mild, non-specific, or transitory neurological manifestations (ranging from 24% to 60%5). This characteristically occurs with motor or sensory disorders, aphasia, and hemianopia.6 However, other less common clinical manifestations which lead to misdiagnosis in the ER have been described.5 One study found that altered mental state was the most common chameleon,7 including manifestations such as psychosis, memory alterations, behavioral changes, mood alterations, and confusion.7,8 This type of presentation often guides the physician toward a non-neurological (psychiatric) cause for the clinical chart.9 These findings are consistent with another study, which found that up to a 6% of patients attended for alteration in their mental status in fact had an ischemic stroke.10
In this panorama of mimics and chameleons, lesion location is important. A stroke in the posterior cerebral artery (PCA) represents 20-25% of ischemic strokes.11 In its clinical profile, visual field defects are more frequent, while speech and limb weakness disorders are less frequent.12 Pure alexia (alexia without dysgraphia) is probably the most characteristic sign of unilateral stroke of the left PCA.13 Other manifestations include unilateral, bilateral, or cross sensory weakness or loss, instability or ataxia, dysarthria, and dysphagia.14 It has been found that stroke chameleons are more likely to occur when the PCA is compromised.15,16 This situation can generate atypical symptoms such as vertigo, nausea, vomiting, headache, or dizziness.4,7,14 In addition, the National Institute of Health Stroke Scale (NIHSS), often used to detect signs of stroke in the ER, is focused on dominant and neurological deficits of the above-mentioned circulation.8 All of these factors make the stroke in the PCA being the most commonly sub-diagnosed variety of these conditions.4,17
Acute neuropsychiatric manifestations as initial presentations of stroke have been poorly reported in the literature. There is frequent reference to their mediate and late consequences on behavior and mood. These manifestations have mainly been described when the right cerebral hemisphere is involved,18,19 with depression being the most common symptom, with a prevalence of 9% to 37%,20,21 followed by generalized anxiety disorder, with 24%. Emotional lability is among the least prevalent manifestations, while pathological laughter and crying, constitute the most commonly described clinical chart.19 Its prevalence in different studies varies between 8-32% in the 3 to 12 months following a stroke, with symptoms subsiding in a maximum of 6 months.22 Secondary mania presents a prevalence of less than 2%. Nearly the half of the patients tend to present this chart in the early days of the stroke, and the other 50% between 1 and 24 months later.22 It has been found that most lesions causing mania involve, directly or indirectly, the limbic system, as practically all of these lesions are located in the right hemisphere, mainly on the right orbit frontal cortex and thalamus.18 Psychotic symptoms are reported with an approximate incidence of 0.4% to 3.1%, with a higher prevalence at the right temporo-parieto-occipital union.18 Finally, global alterations in behavior and mood (non psychiatric disorders of personality), due to scarce reports thereof, have an unknown prevalence.22
It is worth highlighting that, among the causes of the misdiagnosis in the ER, it has also been found that the sensitivity of diagnostic images is overestimated. One study reported that almost one third of patients diagnosed with non-disabling stroke lacked proof of acute ischemic lesions in their initial image (computed tomography [CT] or magnetic resonance imaging [MRI]), which were later encountered on their MRIs.23
Clinical CaseThis involves a 60-year-old woman who is a widow, housekeeper, and has basic primary schooling. As important background information, she reported only hypertension and dyslipidemia. She presents a clinical chart with sudden onset, consisting of overall allopsychic disorientation (with time, people, places, and spaces), emotional lability, uncontrollable crying followed by unrestrained laughter, persecutory delusions, complex visual hallucinations, and hetero-aggressive behavior. She then presented attention problems and occasionally incoherent speech, and finally she was taken to the emergency room of the local hospital 5 days after the onset of said manifestations. There, management began with 5 drops of haloperidol every 12 hours, with little effect in recovery and a presumptive diagnosis of late onset bipolar disorder with manic episodes and psychotic features. She was referred to the San Juan de Dios Psychiatric Clinic in the city of Manizales on February 25th, 2017.
When she was admitted to the mental health unit, she was alert, with global disorientation, a neglected appearance, extremely friendly attitude, presence of motor symptoms of anxiety, and a mixed anxious and elevated mood. Speech characterized by circumstantiality and tangential pararesponses, with increased time for latency question-answering, without delusional ideation verbalization, or indicators of hallucinations. Higher mental functions were clinically assessed and found that they were compromised with poor judgment and marked distractibility, without immediate memory alterations, but with failures in recent memory, and with apparent amnesia of the events reason of consultation, and poor insight. Neuropsychology standardized tests were not used during the initial assessment or follow up. Physical examination did not find any significant alteration, especially regarding the neurological aspect: no conscious state alteration, Glasgow 15/15, normal muscle tone, preserved sensitivity. No neck stiffness and without meningeal signs, symmetric osteotendinous reflexes++/++++, preserved and symmetric strength, without pathological reflexes, negative Babinski, negative Oppenheimer, negative Gordon, negative frontal release reflexes (glabellar, snout, sucking, grasping, palmomentonian). This findings staid negative for the remain of the hospitalization.
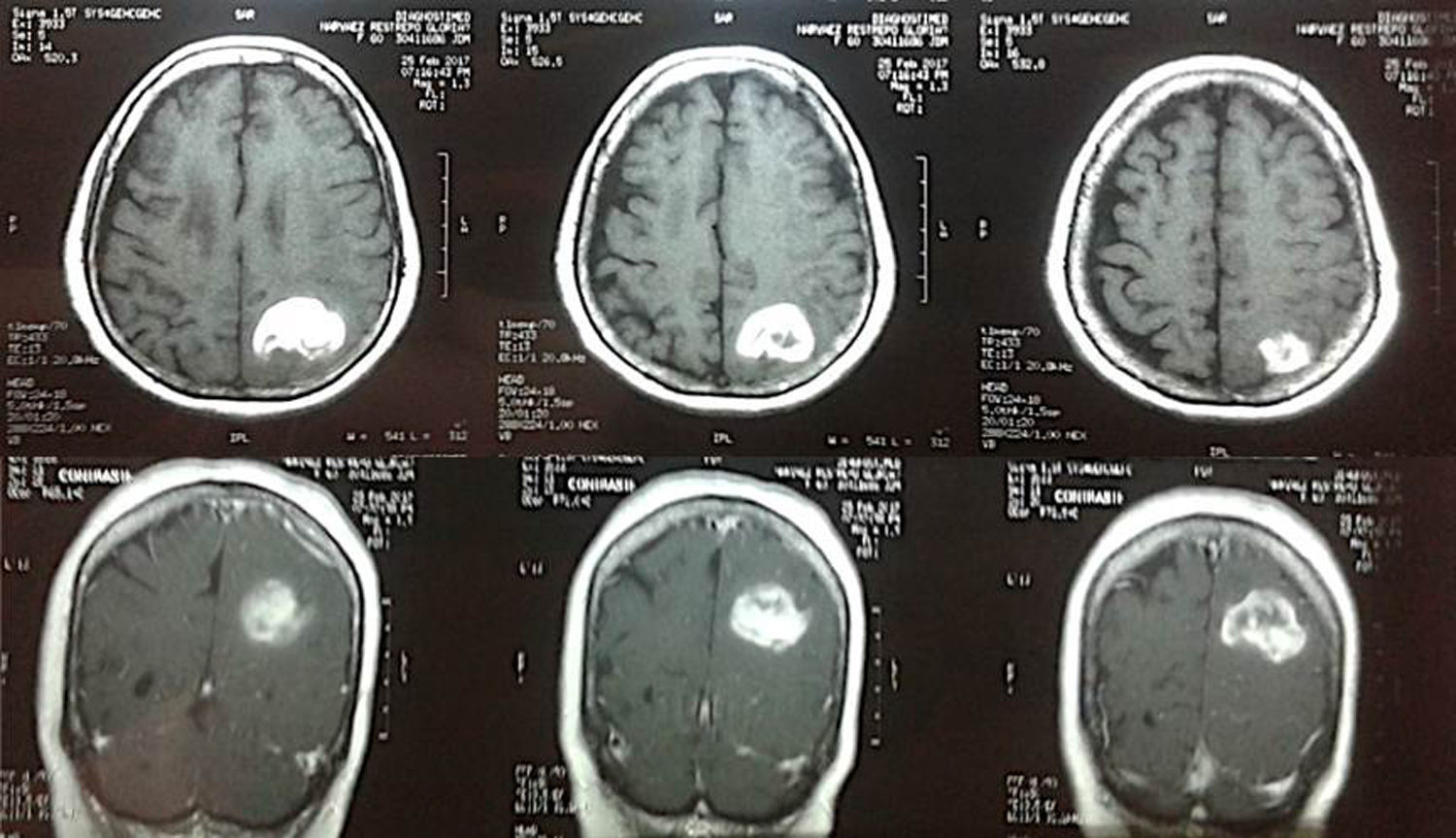
A contrast MRI of brain was requested, due to atypical manifestations on the clinical chart, especially the age of presentation without a previous history of mental health problems (Figure). It showed microangiopathic leukoencephalopathy, and an image suggestive of ischemic stroke in the area of the left PCA, with hemorrhagic reperfusion in the occipital cortex measuring 31×38 mm (lateral and anteroposterior diameter) and a possible old ischemic region in the territory of the Middle Cerebral Artery (MCA). In addition, lab tests were requested for vitamin B12 levels, HIV 1 and 2 antibodies, glucose, creatinine serum, ureic nitrogen, potassium, sodium, AST liver enzymes, ALT, folic acid, VDRL, test for prothrombin time (PT) or international normalized ratio (INR), partial thromboplastin time (PTT). All results were within the normal laboratory range. An altered lipid profile was found, with cholesterol levels at 244mg/dl, triglycerides at 229mg/dl, low density lipoproteins (LDL) at 140.1mg/dl, and high density lipoproteins (HDL) at 58.1mg/dl.
In consequence, the case was considered to be a clinical chart of acute neuropsychiatry symptomatology secondary to stroke, an urgent neurology consultation was requested, but was not authorized by her insurer (EPS) during hospitalization. Followed treatment only with haloperidol 10 mg/day (5 drops of VO every 12 h) and psychotherapeutic interventions of reinsurance and psycho-education. During her time in the mental health unit, her neuropsychiatric chart manifestations evolved favorably. Two days after her admission, on February 27th, there was an increase in the support base as a single abnormality on the neurological exam, and persistence of time disorientation as the only alteration, on mental examination. Resolution of her clinical chart is progressively achieved, without the need for additional pharmacological interventions, up to its full resolution in about 15 days, with a gradual decrease in haloperidol followed by its complete removal, she was therefore discharged from the hospital with an order for a neurology and psychiatric outpatient consultation. At the time of the drafting of this case report, the patient was in general, appropriate conditions, without psychiatric consequences or evident neurological focalization.
DiscussionThe clinical diagnosis of stroke is complex, especially when its manifestations are atypical. In this case, the patient only presented, late in the course of her symptoms, instability denoted by the increase in the support base as a single neurological phenomenon, which favored an initial misdiagnosis of bipolar disorder, given pathological laughter and crying, psychotic symptoms, elevated mood and motor restlessness.
There is a high frequency of psychiatric symptoms in almost all diseases affecting the central nervous system. Psychiatric symptoms typically occur parallel to classical neurological symptoms, and they can deteriorate one's quality of life even more drastically.24 However, psychiatric symptoms may also be the only acute manifestation of stroke, as occurred in this case. In few existing reports, it has been found that the above mentioned manifestations are mainly present when the right hemisphere is affected.18,19 This patient's left hemisphere was affected. This may be a clinical presentation yet undescribed, which would be especially important, as neuropsychiatric manifestations have been more scantly reported and studied, probably as they go unnoticed in clinical practice,22 thus compromising patients’ diagnosis, early treatment, and prognosis.
It is worth highlighting that patients with a stroke only affecting the PCA have significantly less risk of long-term disability and mortality, in comparison to those who have a stroke in PCA together with another outside that territory.25 In this case, it is clear that, despite the late diagnosis and management, the patient had an appropriate clinical recovery, which is consistent with the aforementioned findings.
ConclusionsWe agree with other authors that there is a need to recognize the difficulties implied in stroke diagnosis, and to carry out studies about misdiagnosis, so as to identify related factors which lead to this errors and thus to contribute to the improvement of clinical reasoning when facing similar situations.4,8,15 This especially applies to delays in treatment that they may represent, which may worsen patient prognosis and possibility for long-term improvement. It is possible that some indicators of atypical presentations should be included on scales which focus on stroke in emergency rooms. It is fundamental to keep in mind that mental pathologies which occur with sudden onsets and at infrequent ages should guide us to non-psychiatric pathologies, even in the absence of neurological phenomenology.
Ethical responsibilitiesThe authors declare that they do not have conflicts of interests, that experiments were not carried out on human beings or animals, that in this article, there is not any patient or family data present, and that, through the respective consultation, informed consent was obtained for the composition of this case report, a document that is in the power of the main author.
Conflicts of interestsThe authors declare that they do not have conflicts of interests, that experiments were not carried out on human beings or animals, that in this article, there is not any patient or family data present, and that, through the respective consultation, informed consent was obtained for the composition of this case report, a document that is in the power of the main author.