The purpose of the study was to determine the prevalence and characteristics of patients with persistent delirium (PD) at three months after hospital discharge.
MethodologyLongitudinal descriptive study to assess the prevalence and characteristics of in-patients aged 65 years and older in the Clinica Universitaria Bolivariana who met DSM-5 criteria for delirium at admission, at discharge, and at a 3-month follow up assessment. Socio-demographic features were determined, and CGI-S and DRS-R98 scales used.
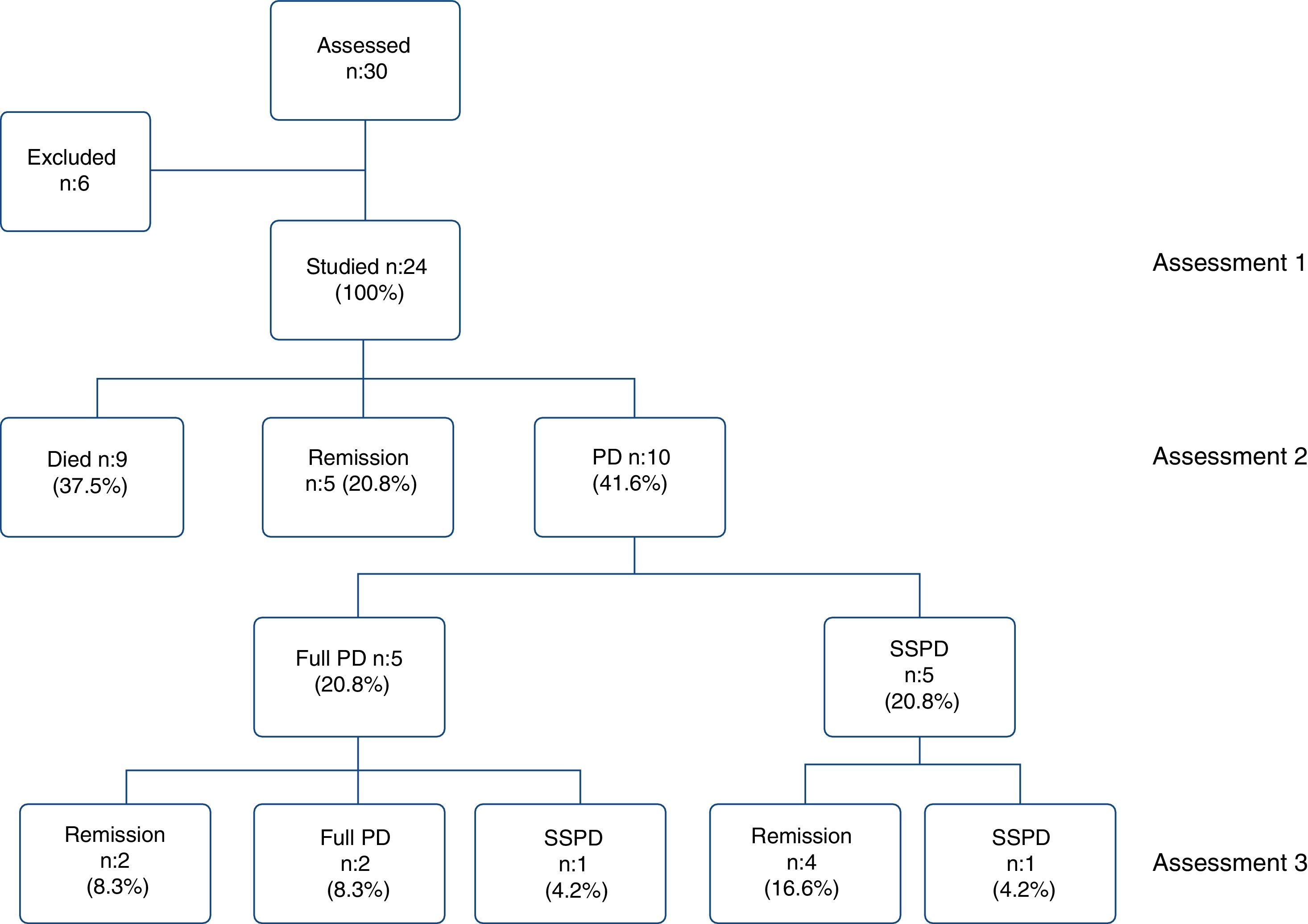
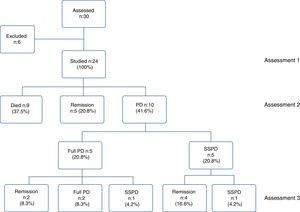
ResultsA total of 30 patients were evaluated between April and October 2013, but 6 did not fulfil the inclusion criteria. The study included 24 patients, with 9 (37.5%) dying during hospitalisation. Of the 15 surviving patients, five (20.8% of the total sample) had their delirium resolved at discharge, and ten (41.6% of the sample) continued with symptoms. These established the PD group, of whom five of them (20.8%) had full PD, and the other five (20.8%) sub-syndromal PD (SSPD). At the final assessment, only two patients (8.3%) continued with full PD, and another two (8.3%) with SSPD. Among the PD group, 30% had a full delirium at admission (prevalence), and 70% developed full delirium during hospitalisation (incidence).
ConclusionsA significant number of patients did not recover from delirium at leaving hospital, and remained symptomatic three months after discharge. The study findings suggest a course of gradual improvement of delirium, with a persistence of symptoms over time in 40% of the patients, which would have implications for the clinical practice.
El delirium es muy prevalente entre los pacientes ancianos con enfermedad general. Si no se revierte en el momento del alta hospitalaria, se lo considera «delirium persistente» (DP). El propósito del estudio es describir la prevalencia y las características de los pacientes con DP 3 meses después del egreso hospitalario de la Clínica Universitaria Bolivariana (CUB).
MétodosSe realizó un estudio descriptivo longitudinal para evaluar la prevalencia y las características de los pacientes de 65 o más años del servicio de hospitalización de la CUB que cumplieran criterios de delirium del DSM-5 al ingreso, el egreso y 3 meses después. Se determinaron las variables sociodemográficas y se aplicaron las escalas CGI-S y DRS-R98.
ResultadosSe evaluó a 30 pacientes con diagnóstico de delirium con interconsulta por psiquiatría de enlace entre abril y octubre de 2013, y se excluyó a 6 por no cumplir los criterios de inclusión. Se incluyó en el estudio a 24 pacientes, de los que 9 fallecieron durante la hospitalización (37,5%). De los 15 sobrevivientes, 5 (el 20,8% de la muestra) presentaron remisión del delirium al egreso y 10 (41,6%) continuaron con síntomas y conformaron el grupo de DP. Del grupo de DP, 5 (20,8%) presentaron DP completo y los otros 5 (20,8%), DP subsindrómico (DPSS). A los 3 meses del egreso, solo 2 pacientes (8,3%) continuaron con DP completo y otros 2 (8,3%), con DPSS. En el grupo de pacientes con DP, la prevalencia fue del 30% (diagnóstico de delirium al ingreso) y una incidencia del 70% (aparición del delirium durante la hospitalización).
ConclusionesUn grupo importante de pacientes con delirium continúan sintomáticos 3 meses después del alta. El 40% de los pacientes con síntomas persistentes en el seguimiento a 3 meses indica una trayectoria de mejoría gradual del delirium, lo cual tiene implicaciones en la práctica clínica.
Delirium is an acute neuropsychiatric disorder that alters consciousness and affects a number of higher cortical functions. When the symptoms persist beyond hospital discharge, it is known as persistent delirium (PD). The interest in studying the characteristics of patients with PD stems from the impact PD has on prognosis when compared to the prognosis of patients whose delirium fully resolves. The geriatric population is considered to be the most vulnerable, with roughly half of all elderly patients having PD one month after discharge. This is accompanied by high associated mortality and disability rates.
The prevalence of delirium is 1–2% in the community, but increases to 14–24% among admissions in a general hospital. The incidence during a hospital stay fluctuates from 6% to 56%, although this can be higher in specific population groups such as intensive care, postoperative and palliative care; post-surgical delirium occurs in 15–53% of people over 65 and in 70–87% of elderly patients admitted to intensive care units.1
In general, delirium is associated with high mortality and morbidity rates, long hospital stay, complications and functional impairment. Elderly patients are very vulnerable; 22–76% die during the hospital stay and 25% die within six months after discharge.2 Patients with Alzheimer's disease suffering from delirium are known to have a worse prognosis than those without dementia and are more prone to cognitive impairment, institutionalisation and death.3 Patients with limited social support are at risk of delirium after orthopaedic surgery.4
Delirium can have many different causes,2 but little is known about the brain mechanisms involved in this disorder. Neuroimaging studies indicate involvement of neuronal connectivity in the dorsolateral prefrontal and posterior cingulate cortex, with cortical hypofunction and increased integration in posterior, medial structures.5
Delirium can begin with a prodromal phase before the specific signs and symptoms develop over the course of 1–3 days. With treatment, symptoms may be resolved within hours or days or persist for weeks or months, particularly in elderly people and patients with associated dementia. Complete recovery from delirium is less likely in elderly people, as only 4–40% of patients have recovered by the time they are discharged from hospital and symptoms can persist for three to six months afterwards.2
In the past it was believed that delirium was reversible in most cases, but studies published over the last ten years suggest that persistence of the condition may be more common than previously thought; in the first place, full recovery is understood to be the return of mental functioning at a level equal to the state prior to the delirium, and sustained for more than 48h.6 When the episode is not reversed and the delirium criteria are still met at discharge and beyond, it is referred to as PD.7
In community support services, Kiely et al.8 found that 51% of their adult patients had PD one month after discharge. In a second article, they reported that one third of patients aged over 65 continued to have PD after six months, that cumulative mortality at one year was 39% regardless of age, gender, comorbidities, level of functioning and the presence of dementia, and that the probability of dying was 2.9% greater than in patients with resolved delirium.9
In their first review of this subject, Cole et al.7 concluded that elderly patients with PD can remain symptomatic for several months and have a worse prognosis than those who make a full recovery. They also reported PD in 44.7% at discharge, 32.8% at one month after discharge, 25.6% at three months and 21% at six months. In a more recent review, Cole highlights that delirium in any form (hypoactive, hyperactive or mixed) can occur in up to 50% of hospitalised geriatric patients and that PD can occur in patients with or without dementia.6
Meagher et al.10 found that patients with PD had greater impairment in the domains of attention, vigilance and orientation than those with sub-syndromal delirium (SSD), and that this was related to the administration of large doses of benzodiazepines. The use of opioids and haloperidol in the geriatric population has been associated with PD,4 and delirium in elderly patients with a history of hypertension (HTN) and alcohol use disorder, a high APACHE II score and analgesics and sedatives used to induce coma.11
SSD is an intermediate state in severity between full delirium and no delirium.12 It has an unfavourable prognosis compared to non-delirium control patients and can occur without progression to full delirium, in the prodromal period or during resolution, but can also persist for a long time.13 It is vital that it be detected by the clinician if the patient is to receive the proper care.12
There are no statistics on PD in our setting and the diagnosis is not reported. Our search found no Colombian publications on PD.
The objective of the study was to describe the prevalence of PD and the characteristics of patients aged 65 or over with PD three months after hospital discharge. We also aimed to estimate the proportion that developed PD, determine the severity of delirium symptoms on admission, at discharge and three months later, explore the relationship between PD and the results of DRS-R98 and CGI-S over time, and identify aetiological factors and pharmacological treatments.
Material and methodsParticipantsThis was a longitudinal descriptive study. The study population was all patients admitted by internal medicine, medical–surgical sub-specialities and the Intensive Care Unit of the Clínica Universitaria Bolivariana (CUB) in Medellín with a diagnosis of delirium or who developed delirium during their hospital stay and were referred to Liaison Psychiatry for assessment. We did not select a sample because we made every effort to study all patients who met the inclusion criteria and had referrals over a period of eight consecutive months (April to November 2013).
The inclusion criteria were males and females aged ≥65 years who: lived in the metropolitan area of Valle de Aburrá; had a relative or responsible caregiver; met the delirium criteria of the Diagnostic and Statistical Manual of Mental Disorders-Fifth Edition (DSM-5)14; had no history of recurrent delirium or alcohol/substance abuse/use; were not in a coma or stupor or under excessive sedation and did not have severe hearing impairment that prevented verbal communication; were not terminally ill; did not have structural brain damage, severe dementia or severe mental retardation; and agreed (or a relative, the legal representative or responsible caregiver agreed) to take part by signing the informed consent form. Patients who refused or were unable to provide information for any reason, those who did not complete the three assessments and those who failed to complete more than 10% of the information requested on the forms were excluded.
InstrumentsWe used forms to record the following patient information: age; gender; marital status; level of education; work activity/status; social security; type of residence; address and telephone number; diagnosis of general underlying disease; medical and psychiatric history; and a contact or caregiver (name, address, telephone and type of relationship with the patient).
To assess the presence and severity of delirium symptoms, we used the Delirium Rating Scale-Revised-98 (DRS-R98), translated and validated for Colombia,15 which consists of 16 items, 13 of which assess severity and the other three (optional) assess diagnostic aspects. We also used the DEC-S (Delirium Aetiology Checklist), adapted to Spanish by Franco et al.,15 consisting of a list of aetiological factors for delirium grouped into 13 categories rated as definite, probable or possible cause, apparently unrelated or definitely unrelated. The criterion to define recovery from delirium was a DRS-R-98 score <8 points; for SSD, it was a score of 8–13 points and for full delirium, ≥14 points.12 We applied the Clinical Global Impression-Severity scale (CGI-S) to assess the severity of the delirium and changes over the course of the study,16 and the functional Global Deterioration Scale (GDS) for dementia, which measures severity as mild cognitive deficit or mild dementia, moderate dementia or severe dementia. The GDS was validated by Aguirre-Acevedo et al.17 and is widely used by the Grupo de Neurociencias de Antioquia [Neurosciences Group of Antioquia] and the Memory Clinic at Hospital Universitario San Ignacio in Bogotá. For the diagnosis of delirium, we used the DSM-514 criteria, and psychiatric comorbidity was confirmed using the respective items of the Mini-International Neuropsychiatric Interview (MINI).18
ProceduresAll the patients referred to Liaison Psychiatry with a diagnosis of delirium were assessed. After informed consent had been obtained, socio-demographic information and information on previous medical history and current illness with the underlying medical diagnosis were collected from an interview with the patient, relative or caregiver and the hospital medical notes. One of the psychiatrist investigators or psychiatry residents performed the first (baseline) assessment to check that the inclusion criteria were met and to confirm the diagnosis of delirium and psychiatric comorbidity with the MINI; the 16-item DRS-R-98, the DEC-S and the CGI-S scales were applied. When the patient was being discharged from hospital, one of the investigators performed the second assessment with application of the severity items of the DRS-R-98 and the CGI-S. A third assessment was carried out three months after discharge with application of the severity items of the DRS-R-98 and the CGI-S. The type of pharmacological treatment was recorded at all three assessments (medical, psychiatric drugs, sedatives, anaesthetics, etc.). At the third assessment it was determined whether the patient had survived or had in fact died, and whether there had been any change in caregiver or if the patient had gone into residential care for the elderly or a nursing home. The third assessment was arranged with the family member or caregiver.
The type of delirium (hypoactive, hyperactive or mixed) was determined clinically according to the DSM-514 criteria. The GDS was applied, as per protocol, when the patient had a history of dementia or cognitive deficit to confirm the diagnosis and determine the severity of the deficit, along with information from the medical records and additionally from a relative or caregiver.
Before beginning the study, the psychiatrist investigators and participating psychiatric residents carried out a check and standardisation of the instruments. The study and informed consent form were approved by the Health Research Ethics Committee of the Universidad Pontificia Bolivariana.
A pilot test was conducted on four patients in the Intensive Care Unit who met the eligibility criteria in order to fine-tune the protocol procedures and they were included as study participants; 50% of the records were selected at random and the data were collated with the respective survey to check for typing errors and, as a paired analysis was being carried out, only patients with complete information in the three assessments were taken into account (patients with incomplete assessments were excluded). This helped maximise the control of biases.
Statistical analysisA database was created in SPSS 19.0 in which the information was processed. The analysis was planned with non-parametric measures because we expected fewer than 30 patients to finish the study at three months with the three assessments. The high mortality rate among this group of patients and the possible loss to follow-up because of change of address affected the estimations. We estimated proportions for the socio-demographic variables, except for age, for which the median [interquartile range] was estimated. We also estimated the proportion of patients who ended up in PD and the proportion of patients with each of the DEC-S aetiological factors on entering the study, at hospital discharge and at three months. Averages of the DRS-R-98 scores were calculated on entering the study, at hospital discharge and at three months, and proportions estimated for the delirium severity category according to CGI-S in the three assessments.
The Friedman test was performed to explore the relationship between the dependent variable PD and the independent variables, which were the three repeated measurements of the DRS-R-98 and the CGI-S (on entering the study, at hospital discharge and at three months). Statistically significant differences were assumed if the p-value was <0.05.
ResultsThirty patients were assessed, six of whom were excluded for not meeting the inclusion criteria: two with severe dementia; two because of incomplete information for the scales; one for permanently residing outside the metropolitan area; and one because of brain cancer. A total of 24 patients were included for the analysis. The baseline assessment was performed when responding to the referral, the second when the patient was discharged from hospital and the third, a mean of 92.8 days after discharge. Nine patients (37.5%) died while in hospital but none died during follow-up; of the 15 who survived, five (20.8% of the total sample) had fully recovered from the delirium by the time of discharge from hospital, while the other ten (41.6%) continued to have symptoms and became the PD group. The PD group was subdivided into five patients (20.8% of the total) with full PD and another five (20.8%) with SSPD; at the third assessment, only two patients (8.3% of the total) still had full PD and two (8.3%) SSPD (Fig. 1).
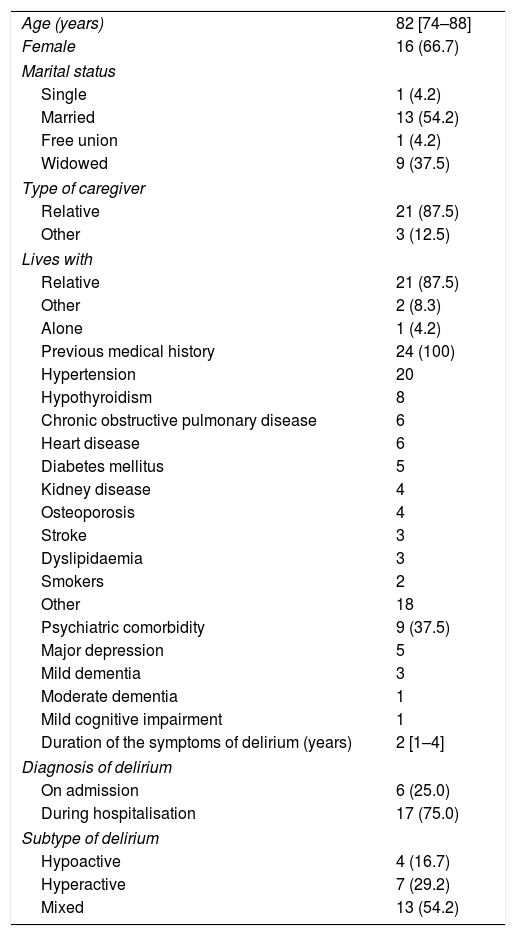
In the overall sample, females represented 66.7%. The median age was 82, slightly more than half (54.2%) were married, 37.5% were widowed, one patient was cohabiting and one was single. The vast majority (87.5%) lived with one of their relatives, who acted as their caregiver; two patients did not live with relatives (one in geriatric residential care and one with an outside caregiver), and one widowed patient lived alone. The most common types of previous medical history involved: hypertension (20 patients); hypothyroidism (8 patients); COPD (6 patients); heart disease (6 patients); diabetes (5 patients); kidney disease (4 patients); osteoporosis (4 patients); dyslipidaemia (3 patients); and stroke (3 patients). Two were active long-term smokers. Most had more than one organic disease. There were nine patients (37.5%) with psychiatric comorbidity: four with major depression as sole comorbidity and five (20.8%) with different degrees of neurocognitive impairment: three with mild dementia (one with associated major depression), one with moderate dementia and one with mild cognitive impairment. Six of the patients (25%) had a diagnosis of delirium on admission to hospital (prevalence) and 17 (75%) developed delirium while in hospital (incidence). By subtypes of delirium, mixed predominated (54.2%), followed by hyperactive (29.2%) and hypoactive (16.7%). The median duration of delirium symptoms before the baseline assessment was two days (Table 1).
General characteristics of the 24 patients included in the study.
| Age (years) | 82 [74–88] |
| Female | 16 (66.7) |
| Marital status | |
| Single | 1 (4.2) |
| Married | 13 (54.2) |
| Free union | 1 (4.2) |
| Widowed | 9 (37.5) |
| Type of caregiver | |
| Relative | 21 (87.5) |
| Other | 3 (12.5) |
| Lives with | |
| Relative | 21 (87.5) |
| Other | 2 (8.3) |
| Alone | 1 (4.2) |
| Previous medical history | 24 (100) |
| Hypertension | 20 |
| Hypothyroidism | 8 |
| Chronic obstructive pulmonary disease | 6 |
| Heart disease | 6 |
| Diabetes mellitus | 5 |
| Kidney disease | 4 |
| Osteoporosis | 4 |
| Stroke | 3 |
| Dyslipidaemia | 3 |
| Smokers | 2 |
| Other | 18 |
| Psychiatric comorbidity | 9 (37.5) |
| Major depression | 5 |
| Mild dementia | 3 |
| Moderate dementia | 1 |
| Mild cognitive impairment | 1 |
| Duration of the symptoms of delirium (years) | 2 [1–4] |
| Diagnosis of delirium | |
| On admission | 6 (25.0) |
| During hospitalisation | 17 (75.0) |
| Subtype of delirium | |
| Hypoactive | 4 (16.7) |
| Hyperactive | 7 (29.2) |
| Mixed | 13 (54.2) |
The values are expressed as n, n (%) or median [interquartile range].
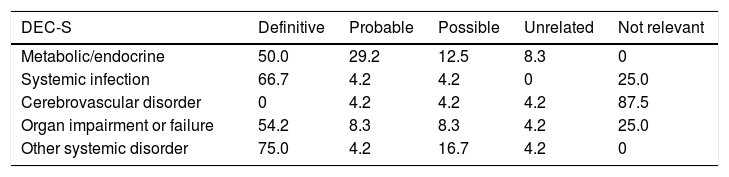
Table 2 shows the aetiological factors for delirium for the 24 patients assessed. Definite causes identified were: systemic infections (66.7%); single-organ or multiple-organ failure (54.2%); metabolic or endocrine disorders (50%); and some other systemic disorder (75%), such as postoperative peritonitis (2 patients), or after hip-fracture surgery (4 patients).
Distribution (%) of the causes or aetiological factors of the delirium for the 24 patients in the study.
| DEC-S | Definitive | Probable | Possible | Unrelated | Not relevant |
|---|---|---|---|---|---|
| Metabolic/endocrine | 50.0 | 29.2 | 12.5 | 8.3 | 0 |
| Systemic infection | 66.7 | 4.2 | 4.2 | 0 | 25.0 |
| Cerebrovascular disorder | 0 | 4.2 | 4.2 | 4.2 | 87.5 |
| Organ impairment or failure | 54.2 | 8.3 | 8.3 | 4.2 | 25.0 |
| Other systemic disorder | 75.0 | 4.2 | 16.7 | 4.2 | 0 |
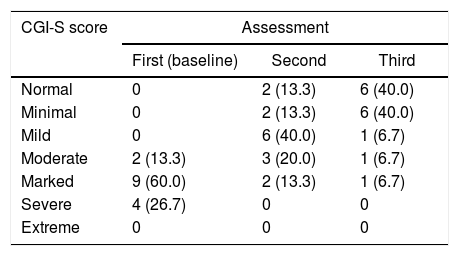
Table 3 shows the CGI-S scale scores decreasing over time and the severity of the delirium with each assessment; we can see that at the time of the first assessment 86.7% of the 15 surviving patients were markedly or severely ill.
Delirium severity scores according to CGI-S in the 3 assessments of the 15 surviving patients.
| CGI-S score | Assessment | ||
|---|---|---|---|
| First (baseline) | Second | Third | |
| Normal | 0 | 2 (13.3) | 6 (40.0) |
| Minimal | 0 | 2 (13.3) | 6 (40.0) |
| Mild | 0 | 6 (40.0) | 1 (6.7) |
| Moderate | 2 (13.3) | 3 (20.0) | 1 (6.7) |
| Marked | 9 (60.0) | 2 (13.3) | 1 (6.7) |
| Severe | 4 (26.7) | 0 | 0 |
| Extreme | 0 | 0 | 0 |
Friedman test=25.10 (p<0.001).
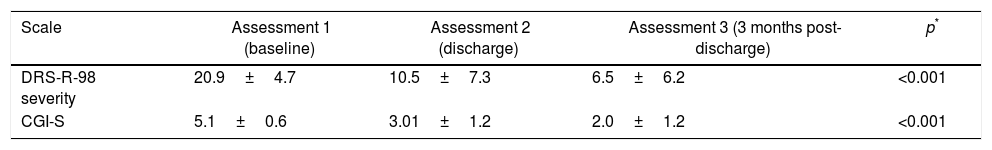
The total DRS-R-98 score for the survivor group was 26.9±4.7 (21–38) points, and the total severity subscale score was 20.9±4.7 points. As can be seen in Table 4, the scores for this subscale decreased over time in the same way as the CGI-S, with the results being statistically significant.
Mean scores for the scales used in the 15 surviving patients.
| Scale | Assessment 1 (baseline) | Assessment 2 (discharge) | Assessment 3 (3 months post-discharge) | p* |
|---|---|---|---|---|
| DRS-R-98 severity | 20.9±4.7 | 10.5±7.3 | 6.5±6.2 | <0.001 |
| CGI-S | 5.1±0.6 | 3.01±1.2 | 2.0±1.2 | <0.001 |
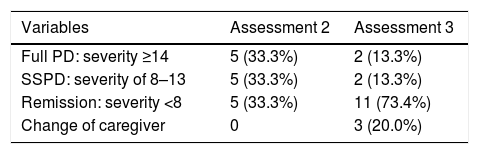
Table 5 shows the course of the delirium in the patients who survived and were discharged from hospital. At the end of the study, 11 of the 15 patients (73.4%) were in remission, two (13.3%) had full PD and two (13.3%) had SSPD.
Course of the delirium for the 15 patients surviving at discharge and at 3 months.
| Variables | Assessment 2 | Assessment 3 |
|---|---|---|
| Full PD: severity ≥14 | 5 (33.3%) | 2 (13.3%) |
| SSPD: severity of 8–13 | 5 (33.3%) | 2 (13.3%) |
| Remission: severity <8 | 5 (33.3%) | 11 (73.4%) |
| Change of caregiver | 0 | 3 (20.0%) |
PD: persistent delirium; SSPD: sub-syndromal persistent delirium.
In terms of caregivers, three patients (two with delirium in remission and one with full PD; 20%) changed caregiver and the rest remained under the care of the same people as before hospitalisation. Two of the above three patients moved to residential care for older adults and in the third case, their care was taken over by a different family member.
Of the patients whose delirium had resolved before discharge from hospital, two had been admitted with delirium and three had developed it while in hospital. For the total group of patients with PD, the prevalence was 30% and the incidence was 70%. Of the subgroup of patients with full PD, three already had the symptoms on admission (prevalence of 60%) and in two the symptoms started once in hospital (incidence of 40%); in the subgroup of patients with SSPD, all five developed delirium in hospital (incidence of 100%). The in-remission and full-PD subgroups both had one hypoactive, one hyperactive and three mixed subtypes of delirium each, while the SSPD subgroup had two hypoactive, two hyperactive and one mixed. During follow-up, one patient with SSPD and mild dementia associated with discharge suffered a further episode of full delirium requiring readmission two months after discharge.
The average length of hospital stay for the patients who survived and were discharged from hospital was 15.3±14.4 (4–55) days and for those who died, it was 26.9±4.7 (21–38) days. By subgroup, the average length of hospital stay was 17.2 days for patients in remission, 10.8 days for patients with full PD, and 18 days for those with SSPD. The median duration of the delirium symptoms before the baseline assessment for the patients who survived and were discharged from hospital was three days for patients in remission, 6.8 days for patients with full PD and one day for those with SSPD.
With regard to psychiatric comorbidity, two of the survivors in total remission at discharge had a history of major depression. In the subgroup of five patients with full PD, one suffered from moderate dementia, one from mild dementia and one from mild cognitive impairment. In the subgroup of five patients with SSPD, one had mild dementia, one had mild dementia with a history of major depression and one had a history of major depression.
The main medical diagnoses leading to the admission of the five patients with full PD were: urinary infection; hip fracture; pneumonia; stroke; and COPD with pneumonia associated with stroke. The main medical diagnoses in the SSPD subgroup were: pneumonia; pneumonia plus heart disease; heart and kidney failure; sepsis plus adrenal insufficiency; and sepsis, hip fracture and anaemia.
For patients with full PD at discharge, the definitive aetiological causes were distributed as follows: 40% had metabolic/endocrine disorders; 40% had systemic infections; 10% had failure of one or more organs; and 10% had other (postoperative) systemic disorders. For patients with SSPD, the distribution was: 40% with metabolic or endocrine disorders; 30% with systemic infections; and 30% with failure of one or more organs.
Analysis of the psychiatric and non-psychiatric drugs administered to the surviving patients while in hospital, at discharge and at three months post-discharge showed a tendency for the number to decrease over time, with statistically significant differences. Non-psychiatric drugs were found to number 9.4±3.9, 6.6±2.8 and 6.9±2.7 in the three respective assessments (p=0.01). Psychiatric drugs numbered 1.6±0.8, 0.9±0.7 and 1.0±0.8 (p=0.03). Three patients received benzodiazepines while still in remission during follow-up, two (one in remission and another with full PD) received opioids continuously up to visit 3, and seven in remission and one with full PD received corticosteroids at the end of the study. At the third assessment, one patient with full PD had no prescribed psychiatric drug treatment.
DiscussionThe results of the study show that not all patients recover from delirium before being discharged from hospital and a significant number remain symptomatic three months after discharge. The prevalence of delirium we found, at 25% of the entire group studied, is in line with the Fong et al.1 estimate of 14–24% in general hospitals, but higher than the 11.7% found by Franco et al.19 in the Internal Medicine Department at CUB. The reason for the differences in prevalence reported in many publications is the heterogeneity of the population groups studied. The same can be said about the incidence of delirium. Our figure of 75% is higher than the 6.9% found by Restrepo et al.20 in adults admitted to Hospital San Vicente de Paul in Medellín, but it is consistent with the figure reported by Fong et al.1 in their review of delirium in the elderly, where they state that the incidence may be over 56% in intensive care, postoperative and palliative care populations. There have been incidences of 70–87% in elderly patients admitted to intensive care.14 Our sample is made up of patients from the Intensive Care Unit and the internal medicine and medical–surgical admission departments at CUB, which may partially explain our findings.
Our group was predominantly female (66.7%) with a median age of 82. The mortality rate was 37.5%, which is within the 22–76% range for elderly people who die during hospitalisation; these data appear in the APA (American Psychiatric Association) guide for the treatment of delirium.2 Our case studies had similar characteristics and results to the study on PD by Kiely et al.,9 whose sample was 65% female, with an average age of 84 and a cumulative mortality rate at one year of 39%. None of our survivors died during the three-month follow-up period. Other characteristics of the group related to predisposing factors, such as history of hypertension, COPD and cigarette smoking, have been described in several studies.21,22
The prevalence of dementia and mild cognitive deficit of 20.8% in our sample is higher than the 13% reported by Saxena et al.,23 but lower than the prevalence of delirium superimposed on dementia found by Fick et al.24 (from 22% to 89% in patients over 65) and by Laurila et al.25 (26.4% of patients admitted to a general medicine department in Helsinki). The differences in results with respect to dementia associated with delirium can be explained by the heterogeneity of the groups studied, the inconsistency in the diagnostic or measurement criteria and the lack of information on cognitive status prior to hospitalisation.26 An important finding was the rate of 25% for associated depressive illness, as it is considered a risk factor for delirium.27 This is in line with the 28.7% found by Laurila et al.,25 but lower than the 33.2% reported by Pisani et al.28
Aetiological factors reported for delirium include infections, intercurrent medical diseases, surgery, metabolic imbalance, primary neurological conditions, uncontrolled pain, medications and environmental factors,23 some of which occurred in our study.
Those of our patients who survived to be discharged from hospital were severely or moderately ill at the baseline assessment, but their severity scale scores gradually decreased over the course of the study. In 20.8% of patients, the delirium had resolved by the time they were discharged, and none died during follow-up. Only four out of ten patients with PD (40%) remained symptomatic after three months. These findings indicate that the delirium followed a course of gradual improvement, and are consistent with the hypotheses proposed by a number of different researchers: that delirium manifests as a spectrum or ordinal continuum.13,29–32 The review by Cole et al.7 reported that half of the patients with PD at discharge were in remission at three months; the remission rate for PD in our study at three months was 60%. It is established that patients with PD have a worse prognosis than those who recover. Marcantonio et al.33 believe that discharging the patient with delirium home with family members can be of great benefit, particularly if the patient has comorbidity in addition to dementia. In our study, the vast majority of patients returned to live with a member of the family group, and this represented a protective factor.
The fact that 20.8% at discharge and 8.4% at the end of the study had SSD is consistent with the findings reported by Cole6: partial recovery rates of 20–42% at the time of discharge and the possibility that it would persist for longer. The negative effect of SSPD in elderly patients is well documented; they have high rates of hospital stay, re-admission, medical complications, mortality after discharge and cognitive and functional impairment with a higher risk of institutionalisation. The prognosis is halfway between that of patients with full delirium and those without delirium.11,13,34,35 Recurrence of delirium, as occurred in one of our patients with SSD, has been documented in recent studies.36,37
The list of medications that can induce delirium in elderly people is very long.38 In fact, Catic39 specifically mentioned some of the medications that patients received during the study (analgesics, benzodiazepines, anticholinergics and antidepressants) as risk factors. Meagher et al.40 included other drug groups in their list (antipsychotics, benzodiazepines, opioids, psychostimulants and corticosteroids). Ouimet et al.,11 however, found no relationship with indomethacin and corticosteroids. What can be extracted from our study with respect to pharmacological treatments is evidence of a general reduction in their use over time. Our research was not focused on the therapeutic aspects and nor did we determine the impact that the use of certain medications might have had on the results.
Our results should be interpreted with caution as the study has certain limitations. The first is the small number of patients with PD, which prevents extrapolation of the results. There is also the fact that the state of delirium can change between assessments because of the fluctuating nature of the condition. Further limitations are the heterogeneity of the group in terms of the origin of the cases, the lack of cognitive assessment prior to the delirium, the fact that the diagnosis of dementia was made from information on the history of cognitive deficit in the medical records and confirmed by interviewing relatives, and the fact that we do not know the primary cause of the dementia. One of the study's strengths is the fact that it is the first on PD to be conducted in Colombia with standardised instruments.
ConclusionsFrom the results of the study, we can conclude that not all patients have recovered from delirium by the time they are discharged from hospital and a significant number remain symptomatic three months after discharge. The prevalence of PD in our study was 30% and the incidence was 70%. The study findings suggest a process of gradual improvement, with symptoms persisting at the three-month follow-up in 40% of patients. This obviously has implications for clinical practice.
FundingCentro de Investigación para el Desarrollo y la Innovación (CIDI) [Research Centre for Development and Innovation], Universidad Pontificia Bolivariana.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work centre on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Constaín GA, Ocampo Saldarriaga MV, Velásquez Tirado JD, de los Ángeles Rodríguez-Gázquez M, Betancur Morales LM, Rico Escobar JJ, et al. La persistencia de delirium a los 3 meses del egreso de los pacientes ancianos hospitalizados en una clínica universitaria. Rev Colomb Psiquiat. 2018;47:37–45.
Article based on the 2015 academic thesis “Prevalence and characteristics of persistent delirium at three months post-discharge in patients admitted to the hospital Clínica Universitaria Bolivariana”, Faculty of Medicine, Universidad Pontificia Bolivariana (UPB), Medellín, Colombia. Preliminary findings presented at the 3rd Research Symposium, School of Health Sciences and Clínica Universitaria Bolivariana, UPB, Medellín, Colombia, on 18 November 2015.