Neurosyphilis is a chronic infectious disease caused by Treponema pallidum that can cause a great variety of neuropsychiatric signs and symptoms, which complicates its diagnosis.
Case descriptionThis case occurred in a 40-year-old man who consulted the Emergency Department because of a convulsion (de novo) which was related to a chronic condition of cognitive impairment and psychosis. The appropriate studies were performed for the diagnosis of neurosyphilis and the recommended treatment was initiated. The patient presented clinical improvement and was discharged.
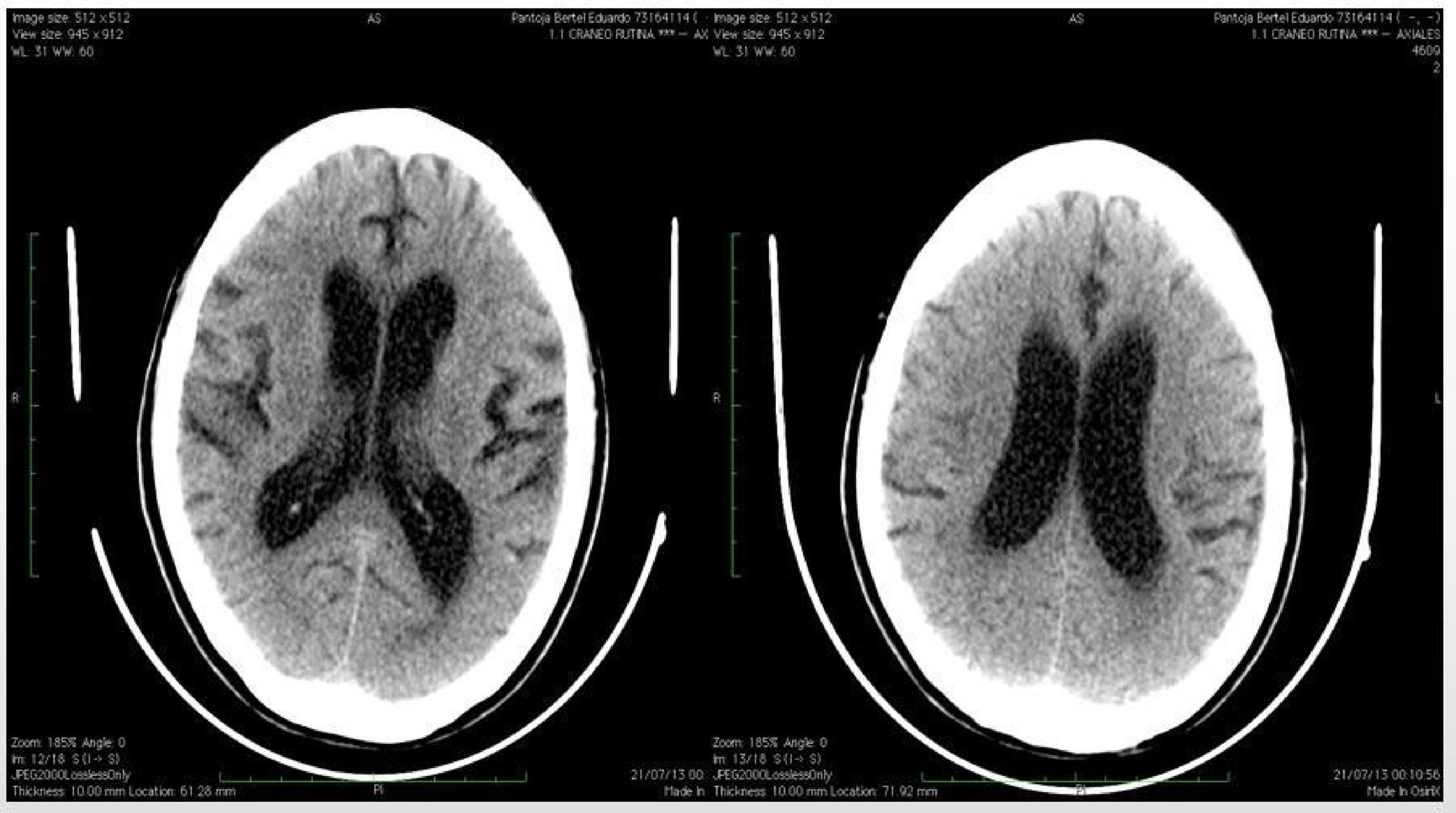
DiscussionPositive VDRL serology results and imaging findings of marked cortical atrophy conducted to consider a late-stage parenchymatous neurosyphilis with serious cognitive impairment and associated psychosis. Treatment with crystalline penicillin was formulated, which reduced the intensity of the patient's symptoms; however, the patient's lack of interest to attend the check-ups significantly reduces his chances of an adequate recovery.
ConclusionsNeurosyphilis must be suspected in patients with clinically evident neurological or psychiatric symptoms. Analysis of VDRL serology and neuroimaging studies are important as an initial evaluation of the patient and must be complemented with cognitive tests or mental examination to determine the state of cognitive impairment.
La neurosífilis es una enfermedad infecciosa crónica ocasionada por Treponema pallidum y puede producir una gran variedad de signos y síntomas neuropsiquiátricos, lo que complica su diagnóstico.
Descripción del casoSe presenta el caso de un paciente de 40 años que consultó al servicio de urgencias por una convulsión de novo, junto con un cuadro crónico de deterioro cognitivo y psicosis. Se le realizaron los estudios pertinentes para el diagnóstico de neurosífilis y se inició el tratamiento recomendado. El paciente presentó mejoría clínica y fue dado de alta.
DiscusiónCon resultados de serología VDRL positivos y hallazgos imagenológicos de atrofia cortical marcada, se consideró una neurosífilis parenquimatosa de tipo tardío, junto con franco deterioro cognoscitivo y psicosis. Se le dejó tratamiento con penicilina cristalina, que disminuyó la intensidad de los síntomas del paciente; sin embargo, el poco interés de este en asistir a sus controles disminuye sus probabilidades de una recuperación adecuada.
ConclusionesLa neurosífilis se debe sospechar en pacientes con síntomas neurológicos o psiquiátricos clínicamente evidentes. El análisis de la serología de VDRL y los estudios de neuroimagen son importantes como evaluación inicial del paciente, que debe complementarse con pruebas cognitivas o examen mental para determinar el estado de deterioro cognitivo.
Syphilis is a chronic infectious disease caused by the spirochaete Treponema pallidum.1 It is known as the “great imitator” because its signs and symptoms are not pathognomonic and it is not readily distinguished from other conditions.2 The discovery of penicillin brought about a significant reduction in the number of cases of syphilis and therefore of its late forms. Neurosyphilis is a late form of syphilis characterised by diffuse or focal nervous system decline.3
Until the early 1990s, syphilis was considered a rare disease in Europe and the United States, as its prevalence had significantly decreased.4 However, since the mid-1990s, there has been a marked increase in the prevalence of syphilis and neurosyphilis, both in the United States and in Europe.5,6 Central nervous system impairment due to T. pallidum occurs in 5%–10% of cases of infection,7 and neurosyphilis develops in one-third of cases that progress to advanced stages.8 The classic forms of late neurosyphilis (tabes dorsalis and progressive general paralysis) are uncommon, and there is a predominance of atypical clinical manifestations.9 Cerebral parenchymatous neurosyphilis, classically known as progressive general paralysis (PGP), leads to dementia characterised by cognitive decline and personality and behavioural disorders,10 which appear 10–20 years after the start of the initial untreated infection and may have a poor prognosis.11
At present, this disease, which used to be so common, is a rare cause of dementia in both low-income and high-income countries, meaning that diagnostic suspicion is low.12
With the changes that have occurred in disease classification for cognitive disorders, according to the DSM-5, dementia is now called neurocognitive decline, meaning that cases once termed syphilitic dementia13 are now referred to as neurocognitive disorders due to another medical condition (neurosyphilis).14
We report a case of neurosyphilis characterised by neurocognitive decline and psychotic symptoms.
Case reportA 40-year-old man had presented signs and symptoms for the past four years. They started with slowness in his movements, a hunched posture and perseveration. A few weeks later, forgetting of recent information, thought blocking, bradypsychia, terminal insomnia and daytime somnolence were added. Two years after these signs and symptoms developed, the patient presented further behavioural abnormalities (hiding household objects with no clear purpose), occupational functional decline due to accentuated voluntary movements, sexual indiscretions, theft of minor objects, isolation and decreased social contact. After three years, the patient's signs and symptoms worsened as he also started to suffer from distractibility, apathy, incoherent language, neglect of personal hygiene and clothing, and sexually maladaptive behaviours such as zoophilia. Two months after the patient was admitted to hospital, he became irritable and hostile and directed verbal aggression at family members. His judgement and behaviour declined further, and he developed incontinence. Subsequently, he had a tonic-clonic seizure of indeterminate duration, with sialorrhoea and deviated gaze, whereupon he was admitted to the emergency department at his city's hospital. The patient had no known history of mental illness or sexually transmitted disease, but he reportedly occasionally engaged in heterosexual intercourse without a stable sexual partner; no family history of neurological or psychiatric diseases was cited.
Physical examination on admission to the emergency department showed that the patient's vital signs were within normal limits, but he was seen to be in a stupor, with a Glasgow Coma Scale score of 12 out of 15 points. He also had sluggishly reactive isochoric pupils, with no sensory deficit, and a muscle strength grade of 4 out of 5 in his right upper limb. No other physical abnormalities were found.
Midazolam 5 mg was administered and it was decided to hospitalise the patient with IV phenytoin 125 mg every 8 h and IV ranitidine 50 mg every 8 h. Laboratory results (for complete blood count, prothrombin time [PT], partial thromboplastin time [PTT], urinalysis, blood glucose, serum electrolytes and PCR) were within normal limits. A single computed tomography (CT) scan of the brain showed dilation of the ventricular system on the axial slices from the base to the vertex of the skull, consistent with communicating hydrocephalus but with no evidence of obstruction as a compensatory mechanism for cortical atrophy (Fig. 1).
On the second day after admission, the patient was seen to have spatial and temporal disorientation associated with incoherent language, excessive wandering and a tendency towards physical and verbal aggression; consequently, oral haloperidol in 5 mg tablets every 12 h was started. On the third day, it was learned that the patient's venereal disease research laboratory (VDRL) test was reactive at a 1:32 dilution and that his serum fluorescent treponemal antibody absorption (FTA-ABS) test was positive. Hence, it was decided to perform a lumbar puncture. In addition, serum levels of thyrotropin and vitamin B12 were determined and reported to be normal, and HIV-1, HIV-2, Herpes simplex type 1 IgM, Herpes simplex type 2 IgM, Herpes simplex type 1 IgG and Herpes simplex type 2 IgG antibodies were all measured and found to be negative.
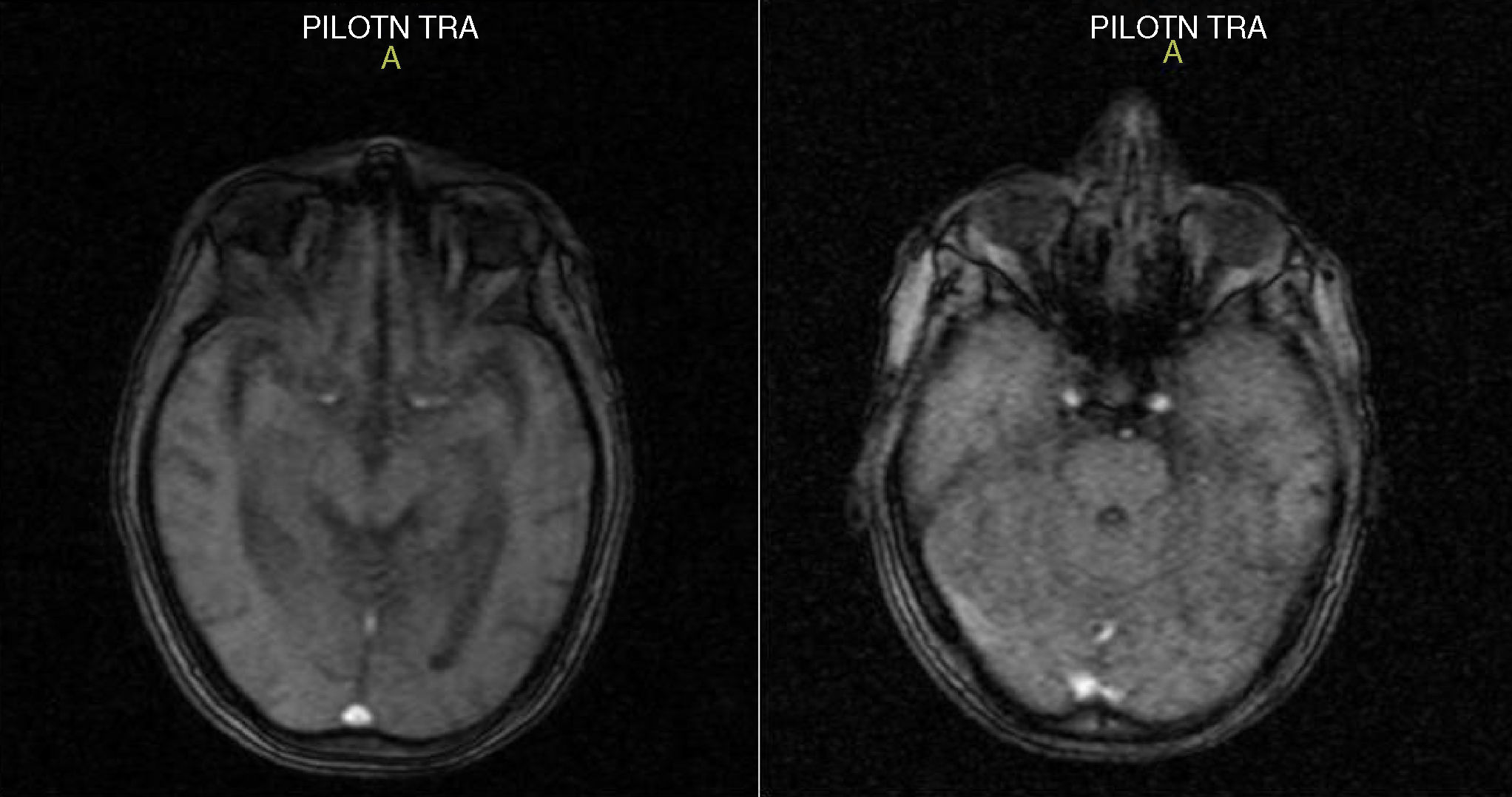
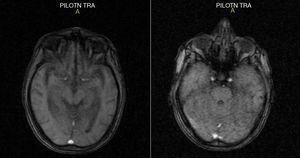
Four days following admission, the patient's magnetic resonance imaging (MRI) report was received. The report found significant supratentorial cortical subcortical atrophy, with an increase in the width of the ventricular cavities and the sulci of the brain surface due to atrophic changes; no other structures were found to show any abnormalities (Fig. 2). The patient also continued to experience spatial and temporal disorientation, and memory tests showed evidence of memory decline in addition to disorganised behaviour. A lumbar puncture was performed without complications at the L4-L5 level and a clear, crystalline fluid was obtained.
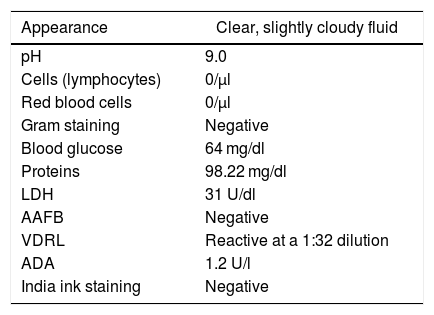
On the sixth day of admission, the cerebrospinal fluid laboratory report was received (Table 1; notably, the VDRL test was reactive at a 1:32 dilution). The diagnosis of neurosyphilis was confirmed and intravenous treatment was started with crystalline penicillin 4 MIU every 4 h for 14 days.
Characteristics of the results of the cerebrospinal fluid examinations.
| Appearance | Clear, slightly cloudy fluid |
|---|---|
| pH | 9.0 |
| Cells (lymphocytes) | 0/μl |
| Red blood cells | 0/μl |
| Gram staining | Negative |
| Blood glucose | 64 mg/dl |
| Proteins | 98.22 mg/dl |
| LDH | 31 U/dl |
| AAFB | Negative |
| VDRL | Reactive at a 1:32 dilution |
| ADA | 1.2 U/l |
| India ink staining | Negative |
AAFB: acid-alcohol-fast bacilli; ADA: adenosine deaminase; LDH: lactate dehydrogenase.
That day, the patient was evaluated by the neurology and psychiatry department, which found clear cognitive decline according to a Mini-Mental State Examination of 18 points, with no evidence of tabes dorsalis, and pupils sluggishly reactive to light (direct and consensual reactions) but reactive to accommodation. Mental examination determined that the patient was partially disoriented in the allopsychic sphere, with judgement deviated from reality, affected reasoning, restricted and inappropriate affect with unmotivated laughter, episodes of psychomotor agitation, hetero-directed physical and verbal aggression and disorganised behaviour. Given the clinical presentation, the patient was believed to have late parenchymatous neurosyphilis, with frank cognitive decline and associated psychosis. Therefore, it was decided to continue with crystalline penicillin and to readjust the patient's psychiatric drug treatment with haloperidol, levomepromazine and biperiden due to extrapyramidal symptoms.
On the eighth day of admission, another CSF culture came back negative, but the patient remained disoriented and logorrhoeic with disorganised behaviour despite antipsychotic treatment. At that time, the patient's results for transaminases, gamma-glutamyltransferase, ionic calcium and phosphorus were also received; these values were within normal limits.
The patient's psychotic symptoms and cognitive decline were seen to improve. After a month, his penicillin treatment ended, and a more significant improvement in psychotic, cognitive and behavioural symptoms was observed. Therefore, it was decided to discharge him with outpatient follow-up by neurology, psychiatry and infectious disease, with general recommendations. After he was discharged (in 2013), the patient did not go to his psychiatry or neurology follow-up visits, though he did continue his psychiatric drug treatment with haloperidol and levomepromazine for one month.
After an active search, the patient attended a follow-up appointment with a family member in March 2015. The family member reported that, three months after discharge, the patient showed notable short-term memory loss, increased response latency, confabulation, perseveration in the behaviour of accumulating useless objects, non sequiturs, terminal insomnia, erratic behaviour, disorganised behaviour (“stripping wires in the early morning for no reason”), neglect of personal hygiene, irritability, verbal aggression towards family members and physical and verbal aggression towards people on the street. This pattern of symptoms was maintained up to three months before the follow-up appointment in 2015, when the patient showed better personal hygiene, decreased aggression and improved interpersonal relationships and started working as a construction worker. Physical examination was normal, with no neurological deficits. Mental examination showed no psychotic or manic symptoms, but the patient did exhibit striking deficits in higher cognitive processes and memory. His Mini-Mental State Examination was 21 points. The need to perform a neuropsychological evaluation to determine the patient's exact degree of decline and start a cognitive rehabilitation programme was raised, but the patient chose not to attend his appointments.
DiscussionAccording to the criteria of the DSM-5, our patient had a major neurocognitive disorder due to another medical condition (neurosyphilis) with abnormal behaviour.14
In general, common causes of neurocognitive disorders include neurodegenerative diseases such as Alzheimer's disease, frontotemporal degeneration, vascular dementia and Lewy body dementia,15,16 which are difficult to treat. There are also many treatable conditions that cause symptoms of neurocognitive disorders (potentially reversible dementia). These conditions include disorders of metabolic origin, drug-induced disorders, structural abnormalities and infections such as neurosyphilis.17,18
The incidence of neurosyphilis dramatically declined with the use of penicillin, but recent years have witnessed an increase in the incidence of this problem.3 Since AIDS was first reported in 1981, the occurrence of neurosyphilis in HIV infection has been the reason for the increase in new cases in developed countries.19 Despite major advances in public health, neurosyphilis is a disease that is still seen in developing countries (regardless of HIV infection and AIDS),20 and due to its clinical polymorphism, it should be considered as a differential diagnosis for several neurological and psychiatric diseases.21 That is why a high degree of suspicion and an active search for this condition are important.
The US Preventive Service Task Force recommends screening all high-risk individuals, given the resurgence in syphilis rates and the constellation of possible clinical manifestations.22 Systematic screening for syphilis in psychiatric patients should enable them to undergo early identification and staging so that they may start treatment on an emergency basis.23 In the case of our patient, neurosyphilis was not suspected and specific tests were not performed until he arrived at the hospital due to a seizure.
Neurosyphilis may present with a wide variety of neuropsychiatric symptoms, from abnormal pupil reflexes to a constellation of cognitive and psychotic signs and mood abnormalities.22 Clinical manifestations are classified as latent forms and late forms. The latter include asymptomatic and symptomatic neurosyphilis. Symptomatic forms cause meningeal irritation with cranial neuropathies such as ocular syphilis, otosyphilis and meningovascular syphilis.20 Late forms of neurosyphilis, which primarily cause general paralysis and tabes dorsalis, occurs a few years to 20 years after the initial infection.3 Our patient experienced abnormal cognitive functioning for four years; this was consistent with late syphilis. He exhibited clear cognitive decline, as indicated by a Mini-Mental State Examination of 18 points, with no evidence of tabes dorsalis, pupils sluggishly reactive to light (direct and consensual reactions) but reactive to accommodation, abnormalities in affectivity and judgement, episodes of psychomotor agitation, hetero-directed physical and verbal aggression and disorganised behaviour, positive serological tests for neurosyphilis and significant cerebral atrophy seen on MRI of the brain.
Neurosyphilis abnormalities on MRI include generalised atrophy, focal lesions, non-specific changes in white matter and extra-axial enhancement indicative of meningitis.24 In this case, the most characteristic finding was generalised atrophy, which, in the absence of specialised neuropsychological tests, serves as a marker for diagnosing major neurocognitive disorder.14 This patient did not undergo any specialised cognitive tests during his hospitalisation, as his psychotic state at the time compromised their use and reliability.25
The patient's clinical presentation and complementary tests revealed that the cause of his neurocognitive disorder was a late parenchymatous form of neurosyphilis, previously called PGP,26 with frank cognitive decline and associated psychosis.
Recent treatment guidelines established that the diagnosis of neurosyphilis is a process that should include careful selection of a combination of treponemal and non-treponemal tests in serum and CSF, cell count in CSF and protein concentration.27 The most significant finding in the examination of the patient's CSF was that his VDRL test was reactive at a 1:32 dilution. This established a diagnosis of neurosyphilis.28 However, a negative result would not have ruled out this diagnosis; Hooshmand et al.29 found that 43% of the cases with neurosyphilis that they evaluated had non-reactive VDRL test results in CSF. Cases have been reported of delirium and psychosis secondary to viral encephalitis due to the Herpes simplex type 1 or type 2 virus in the acute stage of neuroinfection and neurocognitive sequelae during the postencephalitic stage30; therefore, it was important to rule out infection with herpes as the aetiology of our patient's clinical condition.
Treatment for neurosyphilis is based on crystalline penicillin G 18–24 MIU/day, administered intravenously at a rate of 3–4 MIU every 4 h or as a continuous infusion for 14 days according to the Centers for Disease Control and Prevention (CDC).28 Our patient was administered intravenous crystalline penicillin 4 MIU every 4 h for 14 days in accordance with the above-mentioned regimen. Although there is no specific antipsychotic drug recommended for the treatment of psychosis in neurosyphilis, Sánchez et al.31 demonstrated that the antipsychotic drugs that appear to decrease psychotic symptoms in patients with neurosyphilis are haloperidol, risperidone and quetiapine. The patient was administered haloperidol to treat his aggressive and disorganised behaviour and levomepromazine due to its hypnotic effect as it acts on dopamine, thus preventing the patient's cerebral overstimulation.32 This patient showed improvements in his psychotic symptoms and cognitive decline. After a month, his treatment with penicillin ended, and a more significant improvement was seen in his psychotic, cognitive and behavioural symptoms, whereupon it was decided to discharge him.
Follow-up of neurosyphilis is based on re-evaluation of CSF every six months. The cell count should decrease within six months, and the VDRL test and protein concentration should decrease within two years. Otherwise, the patient must be re-treated with intravenous penicillin.28,33 This follow-up could not be strict because the patient did not attend follow-up visits after he was discharged, and even after he was located, he did not attend several appointments for laboratory follow-up and neuropsychological evaluations.
In parenchymatous forms of neurosyphilis, recovery may be incomplete and patients have long-term sequelae, necessitating follow-up for neuropsychological evaluation and neurocognitive rehabilitation.26 After 20 months, our patient was seen to exhibit persistent deficits in higher cognitive processes and memory, with a Mini-Mental State Examination of 21 points.
This case further serves as an illustrative example of tolerance by the family and the patient of cognitive and behavioural symptoms for several years causing a substantial delay in diagnosis and enabling the onset of frank dementia in a young patient, resulting in permanent sequelae.
Improvement in physical health care in the psychiatric population has been focused on cardiovascular and metabolic risk factors, but the prevalence of blood-borne infections in the population with serious mental diseases is estimated to be higher than in the general population.34 The prevalence of syphilis in psychiatric patients has varied a great deal over the years, but has generally stayed above the prevalence in the general population.35 The above highlights the importance of screening for syphilis and other organic and infectious aetiologies of psychiatric symptoms in any patient with psychiatric findings, to start suitable treatment and ensure improvement in symptoms before referring the patient to the psychiatry department for re-evaluation and treatment changes.36
ConclusionsSyphilis is still a real concern. Therefore, neurosyphilis should be considered as a possible aetiology of progressive dementia, especially in non-elderly patients.
VDRL serology and neuroimaging studies are important in an initial evaluation of the patient and should be supplemented with cognitive tests or a mental examination to determine the patient's state of cognitive decline.
This case shows the need to consider this serious but treatable condition in patients with cognitive decline. Neurosyphilis should also be part of the differential diagnosis in all patients with cognitive decline and behavioural abnormalities.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Cassiani-Miranda CA, Chen X. Trastorno neurocognitivo debido a neurosífilis: informe de un caso. Rev Colomb Psiquiat. 2020;49:202–207.