Perinatal depression is a major depression episode that starts during pregnancy and the postpartum period; and is an important cause of health risks in women and infants. A cross-sectional observational study was conducted with information from the records of 112 pregnant women or in the immediate postpartum period who were surveyed to determine the possible association between perinatal depressive symptoms and psychosocial factors occurring in the last year. The prevalence of clinically significant perinatal depressive symptoms using the Edinburgh scale was of 22.36%. The logistic regression model found association between clinically significant perinatal depressive symptoms (score on the Edinburgh scale≥12 and the following psychosocial factors: end of the couple's relationship (OR=6.26; 95% CI, 1.91–20.49), severe economic problems (OR=6.61; 95% CI, 1.86–23.45), and the death of a family member (OR=3.79; 95% CI, 1.12–12.74). In this study, one in four women had broken up with their partner and had severe economic problems during pregnancy, also one of ten had suffered the death of a loved one in the past year. These psychosocial factors were strongly associated with the presence of depressive symptoms with clinical importance. These finding offer the opportunity to consider psychosocial factors as a source of maternal stress that could be easily identified in the prenatal controls that pregnant women receive to identify women at risk of experiencing depressive symptoms in the perinatal period, which will enable appropriate treatment to be given to those who need it.
La depresión perinatal es el episodio depresivo mayor que se inicia durante el embarazo o en las primeras 4 semanas posparto y genera importantes riesgos de salud para la madre y para el bebé. Se realiza un estudio descriptivo transversal a partir de 112 registros de mujeres embarazadas o en el posparto inmediato, a quienes se aplicó la escala de Edimburgo para depresión perinatal y se exploró la posible asociación con factores de riesgo psicosocial ocurridos en el último año. La prevalencia de síntomas depresivos perinatales de importancia clínica usando la escala de Edimburgo fue del 22,36%. El modelo de regresión logística encontró asociación entre síntomas depresivos perinatales clínicamente significativos (escala de Edimburgo ≥ 12) y los siguientes factores psicosociales: finalización de la relación de pareja (OR=6,26; IC95%, 1,91-20,49), dificultades económicas graves (OR=6,61; IC95%, 1,86-23,45) y muerte de un familiar (OR=3,79; IC95%, 1,12-12,74). En este estudio, 1 de cada 4 mujeres había roto con la pareja y tenía problemas económicos graves durante la gestación; además, 1 de cada 10 había sufrido la muerte de un ser querido en el último año. Estos hallazgos ofrecen la oportunidad de identificar precozmente algunos eventos psicosociales negativos como factores de riesgo de depresión perinatal, lo que permitiría dar acompañamiento y tratamiento oportuno a quienes lo requieran.
According to the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), perinatal depression is a major depressive episode that starts in the perinatal period (during pregnancy or in the first four weeks after childbirth).
According to a recent meta-analysis, the prevalence of perinatal depression is 11.9% (95% confidence interval [95% CI] 11.4–12.5).1 It is widely known that women present with mood disorders more frequently. The prevalence is two-fold compared to that in males, with a prevalence of 14–21%.1 What is still not as clear for some is that, contrary to what was believed previously, pregnancy does not protect from, but rather makes a woman vulnerable to, the risk of suffering depression symptoms and perinatal depression.2 The prevalence of perinatal depression has been reported to range from 14 to 23%3 and it increases as the pregnancy progresses.4
Perinatal depression can have devastating consequences not only for the mother, but also for the newborn and the family.5 When it occurs in the first half of pregnancy, it increases the risk of preterm birth, pre-eclampsia,6,7 small for gestational age, low birth weight,8 low Apgar score and a smaller head circumference. In a meta-analysis, Grigoriadis et al.9 found that maternal depression was associated significantly with preterm birth, low birth weight and poor sucking.
Another study demonstrated foetal alterations to vibroacoustic stimulation, in the variability of the foetal heart rate, in the motor activity and in the behavioural development when the mother was depressed.10
Deterioration in the self-care of these mothers was also observed, which can be associated with greater consumption of nicotine, alcohol and psychoactive substances, little physical activity and not taking prenatal vitamins.10
In addition to all of this, perinatal depression is underdiagnosed and poorly treated.11 Furthermore, women with a history of depression frequently discontinue treatments with psychotropic drugs, worsening the risk for them and their babies.12 Between 50 and 62% of women with a history of postpartum depression and 33% with a history of perinatal depression will suffer from depression in their next pregnancy.13
Recently, attention has been paid to the impact that adverse psychosocial factors could have on the pregnant women and the association with prenatal depression.14 Among the numerous factors that have been associated with this condition are low income,15 low educational level,16 sexual abuse in childhood,17 limited social support18 and major life events.19
Robertson et al.20 identified predictive factors of perinatal depression and classified them as strong, moderate or weak. The strong predictors include anxiety, stressful life events, limited social support during pregnancy and a history of depression. The moderate predictors are low self-esteem and maternal anxiety, and the weak predictors are not having a partner or having a difficult relationship with the partner, low economic level and obstetric complications.
The objective of this research was to investigate the possible association between perinatal depression symptoms and negative psychosocial events occurring in the past year.
MethodsA descriptive cross-sectional study based on a secondary information source. The primary study was carried out in the Hospital General de Medellín, the main public hospital of the city of Medellín, which provides third-level complexity services to the general population of the department of Antioquia.
The sample size for the primary study was by convenience sampling from women who were hospitalised between 1 November and 15 December 2014 and who fulfilled the following criteria: literate, hospitalised and pregnant or in the first 72h post-partum, having Spanish as their mother tongue and a clinical condition that did not prevent the patient from participating in the study according to the criteria of the treating physician.
The survey used to collect information for the study was designed by investigators, one of them (SG) with extensive experience in the field of perinatal psychiatry. It was self-applied. The language of the questions was simple, and the patients took between 15 and 30min to respond to them. One of the investigators (JV) was responsible for motivating the patients to participate in the research and was present to clarify doubts and guarantee the correct service.
The survey included the Edinburgh Perinatal Depression Scale,21,22 validated by Jadresic et al.23 This scale has been translated and has been used in numerous studies to identify women who could experience depression in pregnancy and/or the post-partum period.24–28 The scale consists of 10 items and is self-applied. Completing it takes 5min. The questions are Likert scale questions with scores from 0 (“No, never”) to 3 (“Yes, most of the time”). The maximum score is 30. When the cut-off point is taken to be between 12 and 13, greater general efficiency is obtained (correct classification of cases and non-cases in 87.4%), with a good combination of positive (85.3%) and negative predictive values (88.3%), in addition to a sensitivity of 76.3% and a specificity of 93.2%. The score obtained for each patient on the Edinburgh scale allowed two comparison groups to be created: (a) patients with ≥12 points and (b) patients with <12 points.
The dependent variable for this study was depression symptoms according to the Edinburgh scale. The cut-off point chosen for the scale was ≥12, which was taken to determine which patients were at high risk of depression. Other variables included were age, marital status, education, place of residence, employment and ability to support themselves financially. From the psychosocial risk factors characterised in the primary study, the following were taken: death of a family member or a loved one, end of a significant loving relationship, serious problems, financial difficulties, theft or loss of valuable objects, diagnosis of a serious disease, unemployment, change of job, legal problems, suffering an accident, being a victim of physical violence, change of religion and circumstances surrounding the pregnancy from the point of view of the relationship, family relationships, financial situation, physical health and emotional state. The questions which evaluated these aspects were Likert-type questions, with five possible responses: excellent, good, average, poor and terrible.
Statistical analysisQualitative variables were described with absolute and relative frequencies, while the median [interquartile range] was used for age due to the fact that the sample did not present normal distribution.
Normality tests were performed and summary measures were calculated of the quantitative variables and absolute and relative frequency tables of the qualitative variables. The association was sought between having an Edinburgh scale ≥12 points and the other variables included in the study.
As a measure of association, the odds ratio (OR) was used with its respective 95% CI. To establish the relationship between qualitative variables, the χ2 test of independence was used. The binary logistic regression model was used, in which the variables which met the Hosmer–Lemeshow criterion (p<0.25) in the bivariate analysis were included. The variables age, education, marital status and employment were re-categorised into two categories for the multivariate model, according to the clinical criteria of the investigating psychiatrists.
In order to minimise possible biases, the management of the databases was the responsibility of personnel with training in this field, which guaranteed the reliability of the information obtained. It was controlled with logistic regression due to possible confounding variables. For the analysis of the information, the software SPSS® version 21.0 (SPSS Inc.; Chicago, Illinois, United States), covered by a licence, was used.
This research was classified as without risk according to Colombian legislation (resolution 8430 of 1993) and was approved by the university Ethics Committee and by the Hospital Research Committee. Informed consent was requested from the women participating who were older than 18, and assent was requested from minors and the informed consent was given by the family or the responsible legal guardian. Confidentiality of the information analysed was guaranteed at all times.
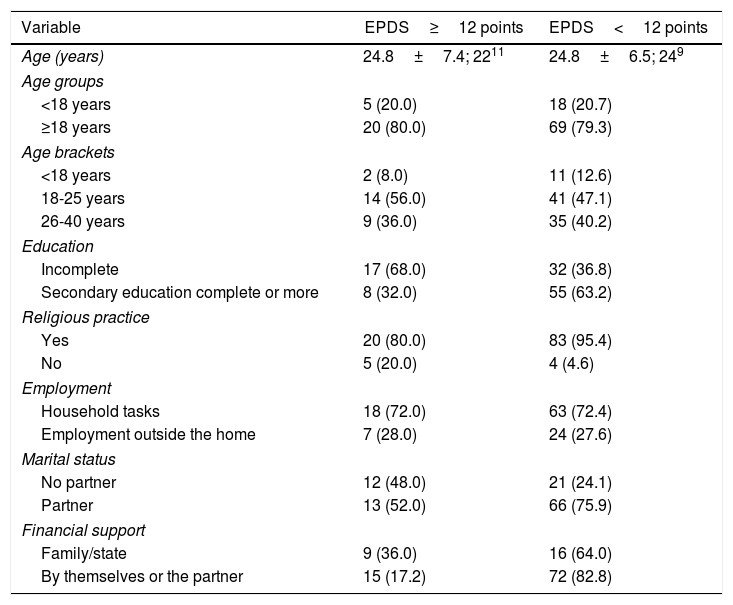
ResultsInformation was analysed from 112 women who were pregnant or in the immediate post-partum period. The minimum age was 13, and the maximum 45. A total of 44.6% of the women had completed intermediate secondary studies, and 29.4% had not. In terms of marital status, the majority lived in a common-law marriage (58.9%), and 29.4% were single. Only 16.1% of the patients were employed and 15.1% supported themselves financially. All the patients received social security benefits (Table 1).
Sociodemographic characteristics of the study population, by scores on the Edinburgh Perinatal Depression Scale.
| Variable | EPDS≥12 points | EPDS<12 points |
|---|---|---|
| Age (years) | 24.8±7.4; 2211 | 24.8±6.5; 249 |
| Age groups | ||
| <18 years | 5 (20.0) | 18 (20.7) |
| ≥18 years | 20 (80.0) | 69 (79.3) |
| Age brackets | ||
| <18 years | 2 (8.0) | 11 (12.6) |
| 18-25 years | 14 (56.0) | 41 (47.1) |
| 26-40 years | 9 (36.0) | 35 (40.2) |
| Education | ||
| Incomplete | 17 (68.0) | 32 (36.8) |
| Secondary education complete or more | 8 (32.0) | 55 (63.2) |
| Religious practice | ||
| Yes | 20 (80.0) | 83 (95.4) |
| No | 5 (20.0) | 4 (4.6) |
| Employment | ||
| Household tasks | 18 (72.0) | 63 (72.4) |
| Employment outside the home | 7 (28.0) | 24 (27.6) |
| Marital status | ||
| No partner | 12 (48.0) | 21 (24.1) |
| Partner | 13 (52.0) | 66 (75.9) |
| Financial support | ||
| Family/state | 9 (36.0) | 16 (64.0) |
| By themselves or the partner | 15 (17.2) | 72 (82.8) |
EPDS: Edinburgh Perinatal Depression Scale.
Values are expressed as the n (%), mean±standard deviation or median [interquartile range].
A total of 22.36% of women assessed obtained an Edinburgh scale ≥12 points, which represents a risk of perinatal depression.
At the time of the survey, 39.3% of the women studied were pregnant, and 60.7% were in the immediate post-partum period, i.e. the first 72h after childbirth. Due to this, it was considered that depression symptoms that were detected in this evaluation were present during pregnancy, and did not correspond to baby blues, given that it is considered that symptoms of this condition are manifested after the third day following the birth.29,30
Two out of every three pregnant women had a gestational age>28 weeks, 34.1% were between 13 and 28 weeks and only one was <13 weeks. The main reasons for hospitalisation for these women were the risk of preterm birth (40.0%) and labour (23.2%).
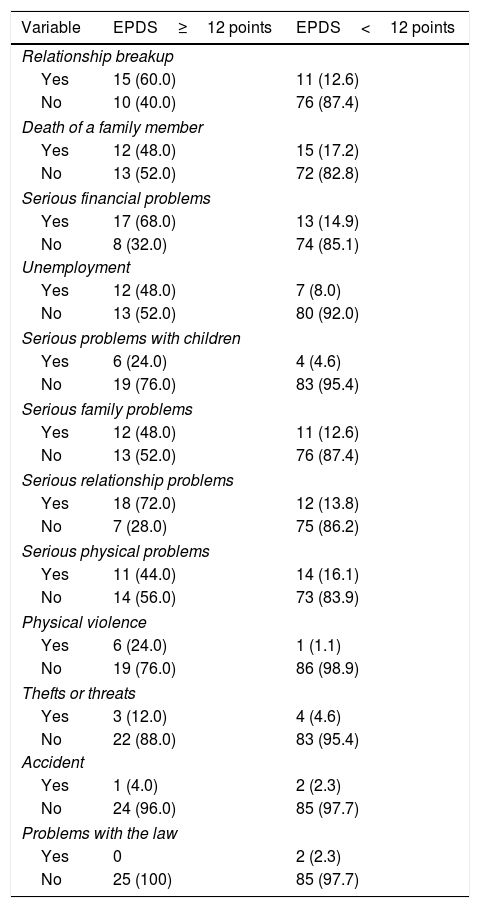
Life events and stressful psychosocial events in the past yearNegative life events which had occurred in the last 12 months were compared for women with and without relevant depression symptoms according to the Edinburgh depression scale (Table 2).
Prevalence of negative life events experienced by the study population in the past 12 months.
| Variable | EPDS≥12 points | EPDS<12 points |
|---|---|---|
| Relationship breakup | ||
| Yes | 15 (60.0) | 11 (12.6) |
| No | 10 (40.0) | 76 (87.4) |
| Death of a family member | ||
| Yes | 12 (48.0) | 15 (17.2) |
| No | 13 (52.0) | 72 (82.8) |
| Serious financial problems | ||
| Yes | 17 (68.0) | 13 (14.9) |
| No | 8 (32.0) | 74 (85.1) |
| Unemployment | ||
| Yes | 12 (48.0) | 7 (8.0) |
| No | 13 (52.0) | 80 (92.0) |
| Serious problems with children | ||
| Yes | 6 (24.0) | 4 (4.6) |
| No | 19 (76.0) | 83 (95.4) |
| Serious family problems | ||
| Yes | 12 (48.0) | 11 (12.6) |
| No | 13 (52.0) | 76 (87.4) |
| Serious relationship problems | ||
| Yes | 18 (72.0) | 12 (13.8) |
| No | 7 (28.0) | 75 (86.2) |
| Serious physical problems | ||
| Yes | 11 (44.0) | 14 (16.1) |
| No | 14 (56.0) | 73 (83.9) |
| Physical violence | ||
| Yes | 6 (24.0) | 1 (1.1) |
| No | 19 (76.0) | 86 (98.9) |
| Thefts or threats | ||
| Yes | 3 (12.0) | 4 (4.6) |
| No | 22 (88.0) | 83 (95.4) |
| Accident | ||
| Yes | 1 (4.0) | 2 (2.3) |
| No | 24 (96.0) | 85 (97.7) |
| Problems with the law | ||
| Yes | 0 | 2 (2.3) |
| No | 25 (100) | 85 (97.7) |
EPDS: Edinburgh Perinatal Depression Scale.
The values are expressed as n (%).
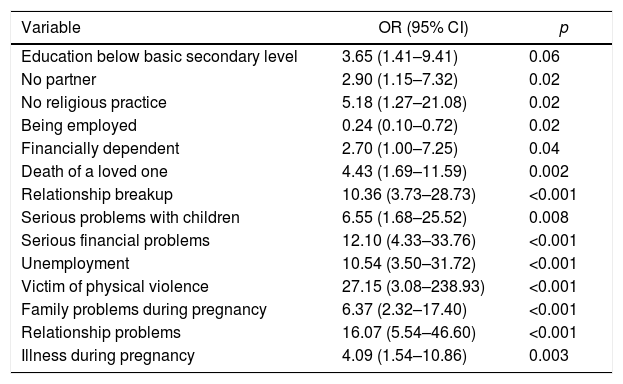
Multiple associations between perinatal depression symptoms and psychosocial and some sociodemographic variables were found in the bivariate analysis. The following risk factors were found: not having a partner, serious emotional problems, death of a loved one, serious financial problems in the past year, suffering physical violence, family problems during pregnancy and moderate or poor partner situation during the pregnancy. The only protective factor was having a job (Table 3).
Significant associations between perinatal depression symptoms and other study variables.
| Variable | OR (95% CI) | p |
|---|---|---|
| Education below basic secondary level | 3.65 (1.41–9.41) | 0.06 |
| No partner | 2.90 (1.15–7.32) | 0.02 |
| No religious practice | 5.18 (1.27–21.08) | 0.02 |
| Being employed | 0.24 (0.10–0.72) | 0.02 |
| Financially dependent | 2.70 (1.00–7.25) | 0.04 |
| Death of a loved one | 4.43 (1.69–11.59) | 0.002 |
| Relationship breakup | 10.36 (3.73–28.73) | <0.001 |
| Serious problems with children | 6.55 (1.68–25.52) | 0.008 |
| Serious financial problems | 12.10 (4.33–33.76) | <0.001 |
| Unemployment | 10.54 (3.50–31.72) | <0.001 |
| Victim of physical violence | 27.15 (3.08–238.93) | <0.001 |
| Family problems during pregnancy | 6.37 (2.32–17.40) | <0.001 |
| Relationship problems | 16.07 (5.54–46.60) | <0.001 |
| Illness during pregnancy | 4.09 (1.54–10.86) | 0.003 |
95% CI: 95% confidence interval; OR: odds ratio.
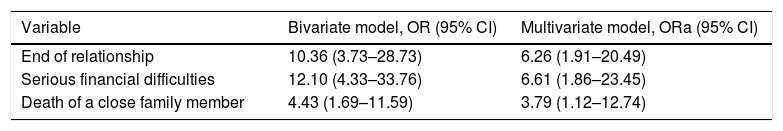
An explanatory binary logistic regression model, which made it possible to control the confounding variables and demonstrate the real associations of perinatal depression symptoms and candidate variables, which were selected for having a p value <0.25 in the bivariate analysis according to the Hosmer–Lemeshow criterion. The independent variables which had more than two categories were analysed as dummy variables. Subsequently, the Enter method was used for the input of the variables and to obtain the adjusted measure.
The variables which remained in the model and the adjusted OR can be observed in Table 4. The model constructed with the three variables included makes it possible to explain the perinatal depression symptoms (χ2=44.150; p<0.001), is significant, explains between 0.326 and 0.498 of the dependent variable and classifies correctly 84.8% of cases, which makes it possible to accept the model.
Factors associated with perinatal depression symptoms: bivariate model versus logistic regression model.
| Variable | Bivariate model, OR (95% CI) | Multivariate model, ORa (95% CI) |
|---|---|---|
| End of relationship | 10.36 (3.73–28.73) | 6.26 (1.91–20.49) |
| Serious financial difficulties | 12.10 (4.33–33.76) | 6.61 (1.86–23.45) |
| Death of a close family member | 4.43 (1.69–11.59) | 3.79 (1.12–12.74) |
95% CI: 95% confidence interval; OR: odds ratio; ORa: adjusted odds ratio.
Psychosocial factors and negative life events associated with perinatal depression were determined in 112 women in pregnancy and the immediate post-partum period (<3 days). The most significant finding of this study was the high prevalence of perinatal depression (22.3%), compared with prevalences described in other studies, which range between 10 and 15%: Switzerland, 13.7%31,32; United Kingdom 13.5%33; Australia, 16.9%,19 and the United States, 15.6%.30,34,35 This high prevalence found and the statistical association with psychosocial adversity factors may be the reflection of the type of obstetric population attending the hospital where the sample was taken.
Locally, a wide range of prevalences of perinatal depression has been reported, which could be in relation to the instruments used to measure the depression symptoms. In a study conducted with 189 pregnant women in Medellín using the Beck Depression Inventory version II (BDI-II), they found a prevalence of depression symptoms of 61.4%, and they also found an association with the history of depression (OR=7.1; 95% CI, 2.6–19.2), psychological abuse (OR=8.7; 95% CI, 2.0–38.5) and dysfunctional relationship (OR=5.1; 95% CI 1.9–13.8).36 Another local study included 125 pregnant adolescents and compared them with 125 non-pregnant adolescents using the Zung Self-Rating Depression Scale. The prevalence of depression symptoms in pregnant adolescents was 32.8% and, in non-pregnant adolescents, it was 16.8%.37 One study conducted in Cali (Colombia)38 included 149 women in the immediate post-partum period and, using the Edinburgh scale, a prevalence of depression symptoms of 46.3% was found. This is the only study which could be directly compared with ours, although the cut-off point used by the investigators to determine the risk of depression was ≥10, and we used as the cut-off point ≥12, according to what was recommended in the literature.
Another important finding is the significant association between perinatal depression symptoms and negative psychosocial factors in the past year. A relationship breakup was associated with a five-fold risk of suffering from perinatal symptoms (OR=6.26); serious financial problems, a five-fold risk (OR=6.61), and death of a family member, a two-fold risk (OR=3.79), which coincides with a systematic review carried out by Lancaster et al.,27 who found that stressful events, limited social support, domestic violence, low economic income, low educational level and poor interpersonal relationships were associated with a greater risk of prenatal depression symptoms.
Yelland et al.39 found that more than 60% of women experienced at least one stressful life event in the 12 months preceding the birth, and at least 18% experienced three or more social adversity events. There are numerous investigations which have associated stressful life events during pregnancy with prenatal depression,20,32,39–43 which coincides with our findings. Most of the studies which take into account stressful life events overlook classifying them by type of event, which is useful for defining interventions.
Unlike in other studies, no association was found with previous abortions,44,45 education level46–48 or having a dysfunctional relationship.30 Despite these findings, few studies have focussed on the role of the family and social support network in the preventive intervention of the psychosocial risk associated with pregnancy.49,50
Kingston et al.51 found in a sample of 6,421 women that 10.5% reported abuse close to the time of the childbirth and 4.3% in the previous two years. It was found in our study that having suffered violence during pregnancy is a risk factor for prenatal depression. Several research studies have shown that women are victims of different types of violence during pregnancy, with sexual and domestic violence being much more prevalent.52–55
The findings of this study should be interpreted in view of the following limitations: (a) the results are based on a self-assessment which can be affected by recall bias; (b) the study sample was carried out by convenience sampling and it was made up mainly of women with low income and means; in addition, the hospital where the study was performed is a tertiary care centre to which pregnant women with a high obstetric risk are referred, which could detract external validity from the results; (c) the questionnaire with which the psychosocial information was obtained was designed by the investigators and has not been validated; (d) most of the women at the time of being surveyed were in the immediate post-partum period and in the third trimester of pregnancy, which means that women in the first and second trimester of pregnancy are not represented; (e) given the sensitive content of the questions, it is possible that patients felt embarrassed when answering them, which could represent an information bias; (f) when situations of violence were investigated, the type of violence was not specified, meaning that no conclusions can be reached on this aspect, and (g) cases of depression should be taken as prevalent and not as incidents, which is why it cannot be guaranteed that some of the women were not depressed at the time of becoming pregnant. Nevertheless, despite these limitations, this study provides valuable information related to prenatal depression and psychosocial risks in women with a high obstetric risk.
ConclusionsThe symptoms of perinatal depression in this group of women with a high obstetric risk are associated significantly with the presence of concrete situations of psychosocial risk, such as a dysfunctional relationship, financial problems and grief due to the death of a family member. All these psychosocial aspects can be identified in the prenatal check-ups and are susceptible to clinical observation in order to intervene promptly in women who require it. This could have a positive impact on the well-being of both these mothers and their babies.
A joint social effort is required which is based on the promotion of healthy lifestyles, the psychoeducation of the risk population, in this case women of reproductive age, but also of healthcare service providers, doctors, nurses and health promoters, who should identify women who go through these psychosocial situations and, in turn, classify them by risk factors for the mother and the foetus.
Lastly, a problem of such magnitude as perinatal depression requires comprehensive interventions that include resources, policies and public health actions.
Conflicts of interestThe authors have no conflicts of interest to declare.
We would like to give special thanks to the women who helped us with this research.
Please cite this article as: Gaviria SL, Duque M, Vergel J, Restrepo D. Síntomas depresivos perinatales: prevalencia y factores psicosociales asociados. Rev Colomb Psiquiat. 2019;48:166–173.