The phantom limb pain has been described as a condition in which patients experience a feeling of itching, spasm or pain in a limb or body part that has been previously amputated. Such pain can be induced by a conflict between the representation of the visual and proprioceptive feedback of the previously healthy limb. The phantom limb pain occurs in at least 42–90% of amputees. Regular drug treatment of phantom limb pain is almost never effective.
MethodsA systematic review of the literature was conducted in Medline and Cochrane using the MESH terms “phantom limb pain” and “psychotherapy”, published in the last 10 years, in English and Spanish, finding 49 items. After reviewing the abstracts, 25 articles were excluded for not being related to the objective of the research. Additionally cross references of included articles and literature were reviewed.
ObjectivesTo describe the psychotherapies used in the management of phantom limb pain, their effectiveness and clinical application reported in the literature.
AimsThe mechanisms underlying phantom limb pain were initially explained, as were the published studies on the usefulness of some psychotherapies such as mirror visual feedback and immersive virtual reality, visual imagery, desensitisation and reprocessing eye movements and hypnosis.
ConclusionsThe phantom limb pain is a complex syndrome that requires pharmacological and psychotherapeutic intervention. The psychotherapies that have been used the most as adjuvants in the treatment of phantom limb pain are mirror visual feedback, desensitisation and reprocessing eye movements, imagery and hypnosis. Studies with more representative samples, specifically randomised trials are required.
El dolor de miembro fantasma ha sido descrito como una condición en la que los pacientes experimentan una sensación de prurito, espasmo o dolor en un miembro o parte del cuerpo previamente amputado. Dicho dolor puede ser inducido por un conflicto entre la representación de la retroalimentación visual y propioceptiva del miembro previamente sano. El dolor de miembro fantasma ocurre en al menos 42 al 90% de los amputados. El tratamiento farmacológico regular del dolor del miembro fantasma casi nunca es efectivo.
MétodoSe realizó una revisión sistemática en las bases de datos Medline y Cochrane usando palabras MESH “phantom limb pain” y “psychotherapy”, publicados en los últimos 10 años, en español e inglés, encontrando 49 artículos. Al revisar los resúmenes, se excluyeron 25 artículos por no ser afines con el objetivo de la investigación. Adicionalmente se revisaron referencias cruzadas de los artículos incluidos y literatura médica.
ObjetivosDescribir las psicoterapias usadas en el manejo del dolor de miembro fantasma, su efectividad y aplicación clínica reportada en la literatura.
DesarrolloSe explican inicialmente los mecanismos subyacentes al dolor de miembro fantasma y se describen los estudios publicados sobre la utilidad del uso de algunas psicoterapias como la retroalimentación visual con espejo y con realidad virtual inmersiva, imaginería visual, reprocesamiento y desensibilización por movimientos oculares e hipnoterapia.
ConclusionesEl dolor de miembro fantasma es un síndrome complejo que requiere intervención farmacológica y psicoterapéutica. Las psicoterapias que más se han usado como coadyuvantes en el tratamiento del dolor de miembro fantasma son la retroalimentación visual con espejo, la desensibilización y reprocesamiento por movimientos oculares, la imaginería y la hipnosis. Se requieren estudios con muestras más significativas, específicamente estudios clínicos aleatorizados.
The concept of phantom limb pain, understood to mean pain perceived in a region of the body that no longer exists, was first described by Ambrose Pare, a 16th century military surgeon,1 but it was Silas Weir Mitchell, a famous 19th century surgeon, who coined the term “phantom limb pain”. More recently, phantom limb pain has been described as a condition in which patients experience a sensation of itching, spasm or pain in a previously healthy limb or body part.2 Such pain may be induced by a conflict between the representation of visual and proprioceptive feedback of the amputated limb.3 A 2008 study on amputees with a traumatic cause estimated that there were at least 1.6 million people who had lost limbs in the United States in 2005 and this number was projected to rise to 3.6 million by 2050.6 Phantom limb pain occurs in at least 42–90% of amputees,2,4,5,7,8 usually begins during the first week after amputation and is described as a “knifelike, burning, squeezing, and throbbing” pain.9
Among the causes that lead to the amputation of a limb are vascular problems, trauma, cancer and congenital abnormalities. In the United States, the number of traumatic amputations has increased since the beginning of the conflicts in Iraq and Afghanistan.10 In Colombia, the armed conflict has left millions of citizens with disabilities. In 2008, Colombia was ranked as the fourth country with the most victims of anti-personnel mines, after Chechnya, Afghanistan and Angola, and the only country that, in the midst of an armed confrontation, destroys the arsenal of these mines.11 There are WHO reports stating that between 15,000 and 25,000 people are killed or maimed by anti-personnel mines in developing countries; 80% of these victims are civilians, most of them children, and one-third of survivors require the amputation of a limb.12
In acquired amputations, the evidence focuses on three classes of neuropathic pain: phantom pain of the amputated limb, stump pain and mixed pain (stump pain and phantom pain), with a prevalence ranging from 51 to 80% for phantom limb pain.8,13 This pain often becomes incapacitating in the contralateral non-amputated limb, in the neck and/or in the back, which causes people who suffer it to report a lower quality of life in relation to their physical and mental health, to demonstrate poorer adaptation to the limitations of amputation and to present maladaptive coping strategies. It is also associated with an increase in depressive and anxious symptoms in the first three years after surgery, particularly in women.14,15
Mechanisms underlying phantom limb painThe convergence of neuroanatomical, neurophysiological and clinical evidence suggests that amputation is associated with neuroplastic changes in the sensory and motor cortex. A brain region disconnected from its original afferent input will not remain inactive for long. The nerve cells of the inactive part of the brain rapidly become involved in the activity occurring in the neighbouring areas of the somatosensory and motor maps to deafferented cortical representations. Clinical manifestations of this change include phantom limb sensation and phantom limb pain. It is not well understood why the absence of afferent inputs and the subsequent expansion of the cortical representation of the face to that of the hand causes pain, rather than an abnormal sensation. One hypothesis is that it is due to the lack of inhibition of cortical motor activity by cortical sensory activation proving that the required movement has taken place.8,16
In the case of upper limb amputation, two changes can be observed: (1) the area of the brain that is responsible for the intact arm will be used more frequently and will process more information than usual, thus improving the abilities of this limb and subsequently increasing the size of this area or (2) brain structures that had processed information from the now amputated arm can be reorganised to begin processing information from the lips or face,17 in some cases, a tactile stimulus in the face occasionally causes this sensation to spread to the phantom hand. These somatotopic changes have been shown to correlate with the incidence and severity of phantom pain.18
Treatment for phantom limb painSome reviews have concluded that regular treatment of phantom limb pain is almost never effective.8 In a 2011 Cochrane review that included 13 studies with 255 participants, six groups of drugs were reviewed, concluding that the effectiveness of opioids, NMDA receptor antagonists, anticonvulsants, antidepressants, calcitonin and anaesthetics for clinically relevant outcomes such as pain, function, mood, sleep, quality of life, satisfaction and adverse effects remains unclear.19
Morphine, gabapentin and ketamine demonstrate short-term analgesic efficacy. Memantine and amitriptyline were ineffective for treating phantom limb pain. The results, however, should be interpreted with caution, since they are mostly based on a small number of studies with limited sample sizes that vary considerably. The direction of efficacy of calcitonin, anaesthetics and dextromethorphan need clarification. Larger and more rigorous randomised controlled trials should be conducted to make strong recommendations about which drugs are useful in clinical practice.19
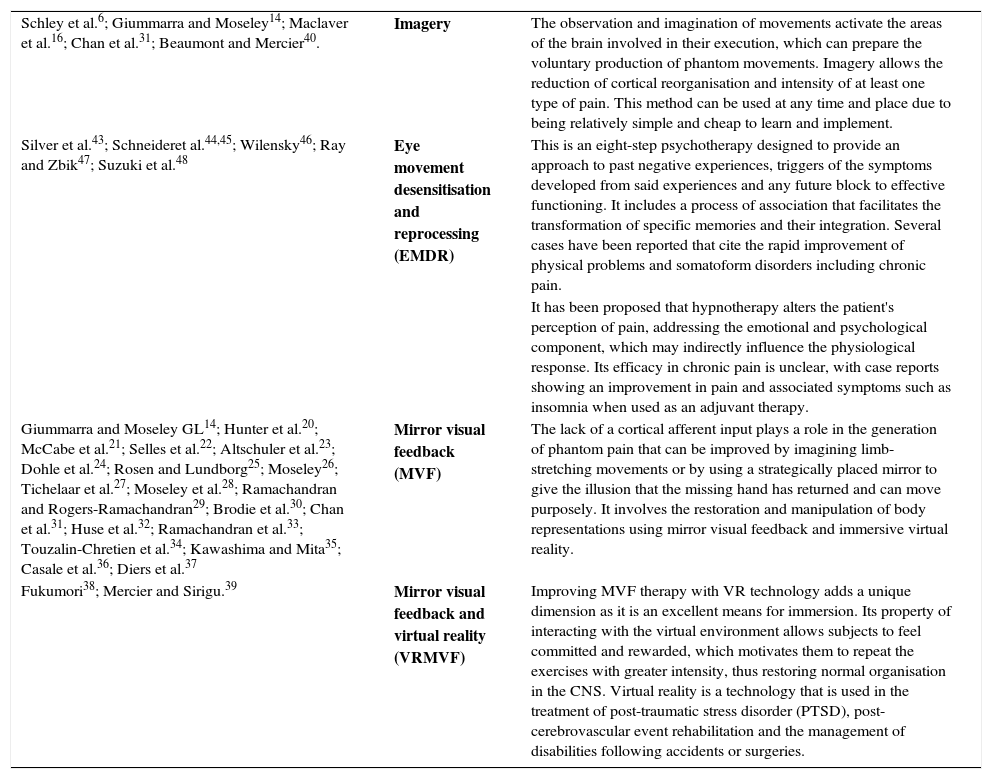
Given the few satisfactory results that have been found with pharmacotherapy as the sole treatment and, taking into account the incidence, frequency and degree of suffering caused by this condition, the development of effective treatments is of great importance. In this context, a literature search was conducted on the psychotherapies used in the management of phantom limb pain, as well as their effectiveness and clinical application, in order to have more therapeutic options and even combine them if necessary. Table 1 summarises the publications found with respect to each psychotherapy proposed as a treatment for phantom limb syndrome.
Publications on the use of psychotherapies in phantom limb syndrome.
| Schley et al.6; Giummarra and Moseley14; Maclaver et al.16; Chan et al.31; Beaumont and Mercier40. | Imagery | The observation and imagination of movements activate the areas of the brain involved in their execution, which can prepare the voluntary production of phantom movements. Imagery allows the reduction of cortical reorganisation and intensity of at least one type of pain. This method can be used at any time and place due to being relatively simple and cheap to learn and implement. |
| Silver et al.43; Schneideret al.44,45; Wilensky46; Ray and Zbik47; Suzuki et al.48 | Eye movement desensitisation and reprocessing (EMDR) | This is an eight-step psychotherapy designed to provide an approach to past negative experiences, triggers of the symptoms developed from said experiences and any future block to effective functioning. It includes a process of association that facilitates the transformation of specific memories and their integration. Several cases have been reported that cite the rapid improvement of physical problems and somatoform disorders including chronic pain. |
| It has been proposed that hypnotherapy alters the patient's perception of pain, addressing the emotional and psychological component, which may indirectly influence the physiological response. Its efficacy in chronic pain is unclear, with case reports showing an improvement in pain and associated symptoms such as insomnia when used as an adjuvant therapy. | ||
| Giummarra and Moseley GL14; Hunter et al.20; McCabe et al.21; Selles et al.22; Altschuler et al.23; Dohle et al.24; Rosen and Lundborg25; Moseley26; Tichelaar et al.27; Moseley et al.28; Ramachandran and Rogers-Ramachandran29; Brodie et al.30; Chan et al.31; Huse et al.32; Ramachandran et al.33; Touzalin-Chretien et al.34; Kawashima and Mita35; Casale et al.36; Diers et al.37 | Mirror visual feedback (MVF) | The lack of a cortical afferent input plays a role in the generation of phantom pain that can be improved by imagining limb-stretching movements or by using a strategically placed mirror to give the illusion that the missing hand has returned and can move purposely. It involves the restoration and manipulation of body representations using mirror visual feedback and immersive virtual reality. |
| Fukumori38; Mercier and Sirigu.39 | Mirror visual feedback and virtual reality (VRMVF) | Improving MVF therapy with VR technology adds a unique dimension as it is an excellent means for immersion. Its property of interacting with the virtual environment allows subjects to feel committed and rewarded, which motivates them to repeat the exercises with greater intensity, thus restoring normal organisation in the CNS. Virtual reality is a technology that is used in the treatment of post-traumatic stress disorder (PTSD), post-cerebrovascular event rehabilitation and the management of disabilities following accidents or surgeries. |
One of the most innovative techniques to be used in the management of phantom pain involves the restoration and manipulation of body representations using mirror visual feedback and immersive virtual reality.14
Mirror visual feedback is used in phantom limb pain,20 complex regional pain syndrome,21,22 cerebrovascular event sequelae23,24 and pain following hand fractures and surgery.25 It has also been incorporated into therapy programmes designed to improve motor planning26 and as an adjuvant in more established rehabilitation approaches.27
Clinical evidence that the lack of a cortical afferent input plays a role in the generation of phantom pain comes from observations that show how phantom pain can be improved by imagining hand-stretching movements or by using a strategically placed mirror to give the illusion that the missing hand has returned and can move purposely.2
In this therapy, a limb is placed behind a mirror positioned in the observer's medial line. The observer, who is looking at the surface of the mirror, will perceive the limb that is reflected as the limb that is behind the mirror. People subjectively report the experience as “looking through a glass,” as if the surface of the mirror were actually transparent.28 They are then asked to perform symmetrical movements with both limbs; when the patient moves the limb that is contralateral to the amputated limb, this causes the phantom limb to feel as if it is moving, reducing phantom pain in some cases.29–31
The importance of having access to visual and kinaesthetic feedback is supported by the observation that visual feedback helps to produce kinaesthetic feedback and thus both can restore voluntary control over phantom movements.32
Ramachandran, Brang and McGeoch noted that observing one's own hand through a reducing lens made it feel smaller and caused a curious alienation of the hand, especially if wiggled. They determined that in the contest between vision and proprioception, vision frequently dominates and overrides its opponent, although not invariably so. In 2009, they reported the case of a 42-year-old man whose left arm had been amputated after being in a traffic accident; he was treated with standard mirror visual feedback but using a reducing lens. Not only did the patient see the reflection of his shrunken hand, but he felt it as well, reporting a reduction in pain at that time. However, as soon as he closed his eyes or when the mirror was removed, the pain immediately returned to its previous intensity. When attempted with a magnifying lens, no changes in pain were observed. Further studies should be undertaken if prolonged use of the reducing mirror could have more stable results.33 Nevertheless, some studies suggest that the behaviour of the organisation of the visuomotor conduct depends on the corporal representation established prior to the traumatic event.34
The clinical limitations and adverse effects have never been defined and there have only been occasional reports of discomfort, restlessness and foreign sensations. Some disadvantages of this therapy have been reported as a possible counterproductive effect during early pain rehabilitation or reactivation once the visual stimulus with the mirror has stopped.35 Casale et al. retrospectively reviewed the existence of adverse effects or adverse reactions in a group of 33 patients with phantom limb pain, finding that 19 of them reported confusion and dizziness, six reported unspecified irritation, and four did not continue the treatment. Only 4 of the 33 patients had no complaints. They clarify, however, that the reasons for this large number of adverse effects may be the lack of selection of patients and that mirror therapy was performed simultaneously with conventional rehabilitation for the use of a prosthesis.36
Dier et al. conducted a study using functional magnetic resonance imaging to investigate the neural correlates of mirror therapy. It involved 14 participants with upper limb amputation, 7 with phantom limb pain, 7 without pain and 9 healthy control subjects. They found a lack of activation in the sensory or motor cortex in amputated patients with phantom limb pain corresponding to the amputated limb during visual mirror therapy, in comparison to the pain-free patient group. They propose conducting a larger study to determine if combining interventions such as imaging therapy and mirror feedback could affect brain activation in amputated patients with phantom limb pain.37
Mirror visual feedback and virtual reality (VRMVF)Virtual reality is a technology used in a wide range of fields and its possible medical application makes it even more interesting. The potential benefits reported have been in the treatment of post-traumatic stress disorder (PTSD), post-cerebrovascular event rehabilitation and the management of disabilities following accidents or surgeries. Improving MVF therapy with VR technology adds a unique dimension as it is an excellent means for immersion. Its property of interacting with the virtual environment allows subjects to feel committed and rewarded, which motivates them to repeat the exercises with greater intensity, thus restoring normal organisation in the CNS.38
The VRMVF system not only mediates the inconsistency between motor intention and proprioceptive feedback, as with the original MVF system, but can also address different brain regions. This system consists of performing objective-oriented motor tasks that require movement planning and coordination, thus activating the parietal, premotor and primary motor cortex. Distraction and reduced anxiety are potential candidates as the underlying mechanism of analgesia provided with this system.38
In 2009, Mercier and Sirigu39 recruited eight participants with phantom limb pain after a traumatic upper limb amputation or brachial plexus avulsion, trained them twice a week for eight weeks using a virtual image of the missing limb performing different movements that the participant had to follow with their phantom limb. On average, participants reported a 38% decrease in pain on the visual analogue scale, with 5 of 8 patients reporting a reduction greater than 30%. Pain reduction lasted for up to four weeks after the initial intervention in 4 of 5 participants. This supports the use of this therapy to relieve phantom limb pain. The authors propose that differences in outcomes may be to do with the difference in susceptibility of virtual visual feedback to factors related to injury or the duration of deafferentation.
In 2010, Sato et al. reported the results obtained by applying the VRMVF system as a treatment for patients with various types of pain in the upper limbs and hand, such as phantom limb pain, brachial plexus avulsion injury and complex regional pain. They found that this therapy improved pain in 80% of patients, demonstrating a pain intensity reduction of over 50% after 3–8 consecutive treatment sessions. It should be noted, however, that only five patients were operated on, all had a chronic state of regional pain, none reported related adverse effects and two continued to experience an analgesic effect even after the therapy was stopped. VRMVF therapy may be considered a promising alternative for patients with this type of pain. Although the realism of the hand represented in the VRMVF system is obviously inferior to that of mirror reflection, it is capable of providing analgesic efficacy which does not seem to depend on whether subjects recognise the virtual arm as their own.38
ImagerySome authors have proposed that the observation and imagination of movements activate the areas of the brain involved in their execution,6,14 which can potentially prepare the voluntary production of phantom movements. This is called imagery and its use has been shown to allow the reduction of cortical reorganisation and the intensity or discomfort of at least one type of pain.16,40
The demonstration that visual feedback modulates central pain set in motion a wave of new experiments involving both neuroimaging and clinical trials. These not only confirm the initial findings of cortical reorganisation but also explore other types of visual modulation such as virtual reality and “guided visual imagery”.41 In fact the standard placebo for mirror visual feedback has been a covered mirror or visual imagery.
The study by Chan et al.31 showed a pain reduction of around 30–50 on the visual analogue scale (0–100) in the mirror group, compared to an pain increase from 35 to 40 in the covered mirror group and 40 to 60 in the visual imagery group. When patients were switched from the control group to the mirror group, the pain decreased by only 10–15 points. Since visual imagery activates the same pathways as real sensory afferent inputs, one would expect it to at least be as useful as MVF; it would not, however, be expected to be more effective, as in spite of presenting an activation of this same mechanism, this is partial.
Another example of the power of visual modulation in phantom limb pain from visual afferent inputs can be shown by simply asking the patient to observe a volunteer's hand being caressed or rubbed. The patient literally begins to experience the tactile sensations of the volunteer,42 presumably due to a loss of tonic inhibition of mirror neurons by tactile receptors.
Maclver et al. chose a mindfulness-based body scan meditation technique as a relaxation method, and used it in patients with unilateral amputation of the upper limb above the wrist, with a phantom limb sensation of about one year's duration. The simple and remarkable technique of imagining movement and sensation in the missing limb resulted in a significant improvement in pain among these patients. Additionally, they wanted to evaluate the relationship between cortical reorganisation, various forms of pain in patients with phantom limb pain syndrome and the analgesic effects of imagery. Patients were asked to tightly purse their lips together while they measured cortical activation by means of functional magnetic resonance imaging (fMRI), finding extensive, concomitant and consistent activation of the hand representation area, which was not found in healthy participants and thus could explain the phantom limb phenomenon generated by a change in excitability of cortical neurons that previously only responded to functions of the hand or arm. They also found that during the second body scan session, in addition to presenting a significant reduction in pain, they failed to show abnormal cortical activation in the fMRI.16
They also record having seen an activation of the hand representation area contralateral to the phantom limb, irrespective of the requested task (purse lips, imagine a movement of the phantom or intact limb, etc.) and conclude that cortical reorganisation after amputation involves intrahemispheric reorganisation from the adjacent area on the homunculus as well as interhemispheric reorganisation from the recruitment of horizontal connections of the intact limb representation to the deafferented cortex.16
Moseley successfully used a similar method, in this case based on the observation of images of movement to decrease phantom limb pain, presenting a reduction in pain even after six months of follow-up. However, because only 11 of the 51 patients in the sample had phantom limb pain, it is difficult to draw a conclusion regarding its effectiveness for this population.41
In 2011, Beaumont et al. conducted a study that included seven people with phantom limb pain following a traumatic unilateral amputation of upper or lower limbs. An intervention was performed which consisted of repeatedly imagining movements of the phantom limb which they had previously seen in a video. Group statistics show that this intervention significantly decreased pain intensity, with individual analyses showing pain reductions of up to 43% after eight weeks. Although the group's effect was not significant between the two intervention phases, individual analyses showed that most participants had a more significant decrease in pain level after eight weeks than after four weeks, suggesting that this type of intervention needs time to be assimilated, and requires the patient's active participation in order to maintain the analgesic effect. The fact that this method can be used at almost any time and place due to being relatively simple and cheap to learn and implement makes it a potentially applicable adjuvant therapy.40
Eye movement desensitisation and reprocessing (EMDR)EMDR is an eight-step psychotherapy designed to provide an approach to past negative experiences, triggers of the symptoms developed from said experiences and any future block to effective functioning.43 It was created by Dr Francine Shapiro for use in individuals who had experienced severe traumatic stress; however, it has become a widely accepted treatment for psychological trauma. The primary goal of the treatment is to access and process recorded memories through a series of standardised procedures, including repetitive eye movements, auditory cues and tactile stimulation. In controlled studies, eye movements have been shown to reduce impact, increase attentional flexibility and recover episodic memory. EMDR includes a process of association that can also serve to facilitate the transformation of specific memories and their integration within the relevant context of the memory network.43–46
Given that in several combat traumas individuals were found to have wounds and injuries that generated pain of considerable intensity, EMDR began to be used for the management of chronic pain in war veterans. Recent reports have found EMDR to be an effective therapy in relieving chronic pain, including phantom limb pain.43 Ray and Zbick believe that although Cognitive Behavioural Therapy (CBT) is effective in reducing pain, EMDR is superior. CBT specifically introduces techniques that allow patients to modify thoughts or physical reactions to pain sensations, while EMDR not only works through cognitions, but also appears to have a direct effect on the desensitisation of the increased limbic portion in the experience of pain. In this way, EMDR provides an additional dimension to pain management that differs from cognitive and/or behavioural interventions, including hypnosis.47
The difference between the EMDR and CBT results can potentially be explained by new neurobiological theories on the differences between memory reconsolidation and extinction.48 According to these theories, treatments that rely on extinction (such as exposure therapies) result in the formation of competing memories rather than a transformation of the old memories as such. The effect of EMDR is based on a different known process with reconsolidation that may involve a modification and re-storage of certain specific memories. It has been proposed that longer exposures result in extinction, while shorter exposures result in reconsolidation.48 More research is needed on these possibilities.
EMDR is based on the Adaptive Information Processing (AIP) model, which proposes that when traumatic memories are registered in isolation and processed inadequately, the dysfunctional emotions, perspectives and sensations of the initial event remain unchanged. In other words, the model proposes that chronic pain involves not only the automatic emotional response to the sensation of pain, but also the somatic component of registered memories. Thus, EMDR treatment of chronic pain, including phantom limb pain, encompasses the processing of both disturbing affective responses and memories of pain associated with causal events. This model may help to explain why phantom limb pain can sometimes be prevented by the epidural administration of agents prior to amputation and other times not. If the pain is directly related to the experience of surgical amputation, such a procedure can effectively reduce subsequent phantom limb pain. However, if the pain is also related to a traumatic injury, prior to the amputation, the epidural procedure will not be as preventive since the patient will have registered the somatic memory of the painful injury. Consequently, traumatic lesions and amputation could be seen as potential independent contributors to this type of pain.45
The first published case of phantom pain eliminated through EMDR concerns a Colombian child treated in 1996 for limb amputation secondary to a cancer diagnosis. The processing of the pain sensations, coupled with the associated feeling of fear and abandonment at having been left in a agency's care by her family, and the horror of never being able to “run and jump with children again” resulted in a complete elimination of the phantom leg pain, and was maintained for two years of follow-up. Subsequent cases of EMDR application and its association with the decrease or remission of phantom pain have been reported in several cases that cite a rapid improvement of physical problems and somatoform disorders including chronic pain.45
HypnotherapyHypnotherapy (and self-hypnosis) alter the patient's perception of pain, addressing the emotional and psychological component, which may indirectly influence the physiological response. It is safe and can reduce the costs of medical treatment in chronic pain49,50 but it remains unused in clinical medicine. Its efficacy on the chronic pain of a traumatically amputated limb is unclear, with three case reports in the literature.51–53 Hypnotherapy was attempted in a case reported in 1996.51 It involved a 58-year-old male patient who met the criteria for post-traumatic stress disorder and for phantom limb pain in his left leg. His left leg was amputated after being severely injured in a collision with a train. Twelve years later he was admitted to hospital for severe burning pain, for which analgesics were prescribed. The patient began taking analgesics 10–20 times a day, and pain relief was only obtained while he was working or after he took the medication. After being treated for his abuse of analgesics, he was pharmacologically treated with carbamazepine, amitriptyline, chlorpromazine and clonazepam, with no effect. Pentobarbital, clomipramine and acetaminophen were also used. 27 years after the amputation, he started his first hypnosis session. Superficial hypnosis was induced where the patient could think and speak, and consciousness was focused on the image of his phantom limb, initially imagined as shorter, and later as the same length as the healthy limb. After three months, severe pain occurred only intermittently and oral analgesics decreased to 2–5 times per day. His insomnia also improved.
Another case reported in July 201352 highlights the experience of the authors who conclude that hypnosis should be considered in the multimodal management of chronic post-amputation upper limb pain. It concerns a 49-year-old woman whose second and third fingers were amputated after being crushed by a sugar cane juicer. She then developed severe phantom limb pain that did not respond to drug management, including a cocktail of tramadol, etoricoxib, pregabalin and amitriptyline. A medical hypnotherapist was consulted and after four sessions of hypnotherapy the pain was resolved. Five months later, the patient developed a different type of pain (causalgia and dysesthesia) in the stump. Over the next six months she received treatment for multidisciplinary pain, including physical desensitisation, a cocktail of oral analgesics, 5% lidocaine patches and two nerve blocks with bupivacaine. Only the latter managed to temporarily control the pain. Later, she was surgically explored where two neuromas were extracted. Subjectively, her pain did not improve, but the patient used her hand more comfortably and her hypersensitivity even disappeared almost immediately with the application of placebo (saline solution), suggesting a significant psychological component. Hypnotherapy was then reattempted. Nine sessions were held over a period of two weeks. A combination of several therapeutic approaches were included, such as “healing garden”, “tension and stress”, “switches for pain”, “releasing negative emotions” and “float-away stress”. Under hypnosis, the patient revealed that her burning pain originated from her inability to accept her appearance after the amputation. This was exacerbated due to being the caregiver of a father with dementia. Her pain decreased to unnoticeable levels after the ninth session and eight months later it remained well controlled without regular analgesia and using self-hypnosis with a CD or recorded hypnotherapy sessions.
A third case53 refers to a male patient who lost his left arm at 5 years of age. It was his dominant arm. As soon as he awoke from the surgery where his arm was amputated, he reported phantom limb pain, which he continued to suffer intermittently until adulthood. As part of the introductory Psychology group at Midwestern University, at age 31, he was administered the Harvard Group Scale of Hypnotic Susceptibility (HGSHS) via tape recording, with it being noted that he responded to right hand and arm movement items, despite missing a large part of his right arm. After the group experience, he agreed to participate in a post-experimental interview, reporting the following “It felt like I had my right hand and it was getting heavier. I was able to lift it a little, but it was very heavy”, “It actually felt like I felt my fingers”, “I felt like I was clapping my hands” and “I could touch both hands.”
ConclusionsPhantom limb pain is a complex syndrome that requires joint pharmacological and psychotherapeutic intervention. Medications used to treat this type of chronic pain continue to be ineffective for total pain control, interfering with the patient's quality of life, sleep, functionality and mood. The psychotherapies that have been most widely used as adjuvants in the treatment of phantom limb pain are mirror visual feedback, eye movement desensitisation and reprocessing, imagery and hypnosis. These therapies have yielded satisfactory results regarding pain management, but most of the studies have been case reports and case series, so studies with more representative samples, specifically randomised clinical trials, are required.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Cárdenas K, Aranda M. Uso de psicoterapias como tratamiento del dolor de miembro fantasma. Rev Colomb Psiquiat. 2017;46:178–186.