To evaluate the associations between relapse and admissions (voluntary and involuntary) in a sample of patients with substance dependence.
MethodsThis is a cross-sectional study undertaken at a private medical therapeutic community specialised in treating addiction, located in a rural area of São Paulo, Brazil. Sociodemographic characteristics, the University of Rhode Island Change Assessment Scale (URICA), Stages Readiness and Treatment Eagerness Scale (SOCRATES), Beck Anxiety Inventory (BAI) and Beck Depression Inventory (BDI) and Structured Clinical Interview for DSM-IV-SCID were used.
ResultsRelapse was associated with low family income (P=.006) and contemplation motivational stage (P<0.05). Nevertheless, no significant differences between individuals who were admitted involuntarily (64%) and voluntarily (54%) were observed (P=0.683) in terms of relapses.
ConclusionsIn this sample, the relapse outcome in involuntary admissions was no different from the voluntary ones.
Evaluar las asociaciones entre recaída y admisiones (voluntarias e involuntarias) en una muestra de dependientes de sustancias.
MétodosEste es un estudio transversal realizado en una comunidad médica terapéutica privada, especializada en el tratamiento de la adicción, ubicada en una zona rural de São Paulo, Brasil. Se utilizaron las características sociodemográficas, la Escala de Evaluación de Cambios de la Universidad de Rhode Island (URICA), la Escala de Evaluación de la Etapa de Preparación y Tratamiento (SOCRATES), el Inventario de Ansiedad de Beck (BAI), el Inventario de Depresión de Beck (BDI) y la Entrevista Clínica Estructurada para DSM-IV-SCID.
ResultadosLa recaída se asoció con bajos ingresos familiares (p=0,006) y contemplación de la etapa motivacional (p <0,05). Sin embargo, no se observaron diferencias significativas entre los individuos que ingresaron involuntariamente (64%) y los voluntarios (54%) (p=0,683) en términos de recaídas.
ConclusionesEn esta muestra, el resultado de la recaída en admisiones involuntarias no fue diferente que en los voluntarios.
The use of involuntary admission in substance dependence treatment may be necessary to enable treatment and prevent harm, such as violence, suicide, delirium tremens, liver failure, heart disease, and central nervous effects.1–3
In a review of the literature about legal coercion in the treatment of substance abusers, note that research into the effectiveness of compulsory treatment have yielded a mixed, inconsistent, and inconclusive pattern of outcomes, calling into question the evidence-based statements made by researchers that compulsory and involuntary treatment is effective in the recovery of substance users.4
Researcher's recommendation points out for the needy to expand eligibility criteria for involuntary admission with clinical research and forensic interface for involuntary admissions for substance dependents individuals.4 In addition, some supplementary professional guidelines are required to avoid the outdated deliberative-oriented ideal of reasoning about legal criteria for involuntary admission lapses into “paternalism” in clinical decision-making.5
In Brazil, the current mental health policies stem from mobilizations and struggles of patients, families and health professionals, aimed at changing the exclusion scenario, long stay in facilities and imprisonment of people with mental disorders and drug problems.6 It highlighted that psychiatric hospitalization is only recommended when treatment in outpatient's services may be insufficient. One of the main features for achieving change in care was restricting the increase of beds in psychiatric hospitals, directing the public investment to the implementation of community and outpatient services in the municipality. However, the hospitalization appears to keep being used as one of the main tools for promoting abstinence of substance users in initial periods of treatment, like showed an example in a state of Santa Catarina.7
Such claims process and popular participation gains strength in the 80's and results in the Brazilian Psychiatric Reform (PR) that, to base state policies – such as Law No. 10216, April 2001. According to this law, psychiatric hospitalizations were classified as voluntary (with patient's consent), involuntary (without patient's consent), or compulsory (required by Court).8 It represents a major advance in the treatment people with mental disorders towards the community, ensuring human rights and enhancing citizenship. The attention for drug users has emerged more intensely on the national public policies schedule from 2010, when the regulation of these policies intensified, resulting in the establishment by the Federal Government, the “Integrated Plan to Combat Crack and other Drugs”. The emergence of this agenda has been accompanied by the diversification of the services available. A diffuse philanthropic network, focusing on Therapeutic Communities (TC) has spread,15 including the modality of involuntary hospitalization since the most recent Brazilian normative (ANVISA Resolution RDC No. 29/11) provide accreditations for that.9
The term “Therapeutic Community” refers to a terminology widely used internationally to describe an efficient, inpatient (or boarding) approach to the treatment of alcohol and drug users. The TC includes not only a “set of people living in common”, but also the notion of “communion” and “participation in common”, that is, an approach of self- and inter-help. This approach is preferably applied outside the traditional psychiatric, psychological and medical intervention institutions and modalities.9 They are nowadays presenting a wide and diverse set of human services and support that try to respond to a set of needs and gaps felt and lived by the residents. In Brazil, the involuntary treatment, provided for by law No. 10.216 of April 6, 2001, and in accordance with the Resolution of the Collegiate Board of Directors DRC number-101 of Agência de Vigilância Sanitária (ANVISA), Brazil, Annex 1, second item 4 treatment services procedures 4.1 fourth paragraph, which would assist persons in need of treatment, but are not in a position to decide on their own account endangering their life and the lives of others.10
The aims of this study are to evaluate relapse and other associated conditions for involuntary admissions of substance dependent individuals in a therapeutic community with three months of follow up after discharge.
MethodsThis is a cross-sectional study design, conducted with male substance dependents, and an interview with 3 months of follow up after the discharge. It was undertaken at a “natural medical private TC” (the terminology we use in this paper is TC, but the readers need to take in mind that we are referring to a “natural medical private TC”), specialised in addiction treatment, located in Sao Paulo State, Brazil. Data collection was conducted from July to November 2013.
Data collection and follow up were conducted by one psychologist not blind for involuntary and voluntary admissions, with addiction knowledge background who was previously trained to apply the questionnaire used in this study. The patients were interviewed up to 1 week after admission. Each interview takes about 40minutes. The group 1 was comprised by involuntary patients undergoing to treatment for the first time in TC, and the group 2 was comprised by voluntarily patients undergoing treatment for drug addiction for the first time in TC.
The inclusion criteria was a dependence diagnosis according to the Diagnostic and Statistical Manual of Mental Disorders, 4th edition, text revised (DSM-IV-TR) diagnosis criteria. The exclusion criteria were: a) evidence of severe communication problems by organic disease such as deafness or muteness, and b) comorbidities related to brain damage or severe cognitive impairment assessed through clinical observation that compromise the understanding of the responses during the interview. No refusals were recorded.
The following instruments were applied:
University of Rhode Island Change Assessment Scale (URICA)This is a scale consisting of 32 items, divided into 4 subscales: pre-contemplation (8 items), contemplation (8 items), action (8 items) and maintenance (8 items). The objective is to auxiliary treatment for the identification of motivational stages in which the patient lies. It was developed by McConnaughy, Prochaska and Velicer,11 adapted in Brazil by Szupszynski and Oliveira,12 and validated by Figlie.13
The Stages and Treatment Readiness Scale Eagerness (SOCRATES)It investigates the degree of alertness/motivation for the accomplishment of the treatment, through the stages of recognition, ambivalence and action. In Brazil, it was validated by Figlie,14 with reliability from 0.84 to 0.89. Initially it was delineated by Miller15 in a version with 32 items, modified later for a version with 19 items.
Beck Anxiety Inventory (BAI)It was developed by Beck et al. in 1988, and validated in Brazil by Cunha. It presents 21 items related to anxiety symptoms, each composed of 4 statements that evolve in a degree of intensity from 0 to 3. More than 1 statement can be chosen, but the computed score is always the most intense. The sum of the scores obtained on each item results in a total score ranging from 0 to 63.16
Beck Depression Inventory (BDI)This instrument was developed by Beck et al.17 to assess the intensity of depression. The inventory items refer to sadness, pessimism, sense of failure, lack of satisfaction, feelings of guilt, feelings of punishment, self-deprecation, self-accusation, suicidal ideas, crying spells, irritability, social withdrawal, indecisiveness, distortion body image, inability to work, sleep disturbance, fatigue, loss of appetite, weight loss, somatic concern, and decreased libido.
Diagnostic and Statistical Manual of Mental Disorders (APA, 2000)It consists of eight modules that evaluate the following disorders: psychotic, moody, anxious, somatoform, substance use, adjustment, eating and personality. For this study, it was used only the module of substance use, which characterizes the diagnosis of alcohol dependence in the presence of 3 or more symptoms evaluated, in a period of 12 months.18
Ethical IssuesThis study was approved by the Federal University of Sao Paulo (UNIFESP) Ethics Committee (Number 332.443/2013). All the participants signed an informed consent form. The patients did not receive any refunds or compensation for participating in this study.
Statistical AnalysesThe data were analyzed descriptively. For categorical variables were presented absolute and relative frequencies and numerical variables, mean, minimum, maximum and standard deviation (SD). For statistical analysis, the hospitalization variable was categorized according to the type: voluntary and involuntary, being therefore the dependent variable.
The χ2 and Fisher's exact tests were used to assess associations between variables such as relapse, sociodemographic, URICA, anxiety (BAI) and depression (BDI). For a comparison of the mean age, scores SOCRATES (recognition ambivalence and action) by the occurrence of relapse were performed using Student's t test for independent samples.
To assess simultaneously the effects of sociodemographic characteristics, URICA, SOCRATES, levels of anxiety, depression level and group (voluntary or involuntary) —explanatory variables— in relapse at 3 months after discharge (dependent variable), a logistic regression model was adjusted. Initially, all explanatory variables were included in the model. In the final model of regression analysis were analyzed areas URICA (pre-installation/contemplation and preparation/share) and SOCRATES (recognition, ambivalence, and action) individually. Thus, all categorical variables related to socio-demographic information, relapse after 3 months of follow-up, type of admission (voluntary or involuntary group) level of anxiety (BAI) and level of depression (BDI) were controlled by fields of URICA AND SOCRATES scales. Then, the non-significant variables at 5% were excluded one by one in order of significance (backward method). In addition, the suitability configuration of the final model was evaluated through the Hosmer and Lemeshow test. The level of statistical significance for the study was established in 95% confidence interval (95%CI), P<.005.
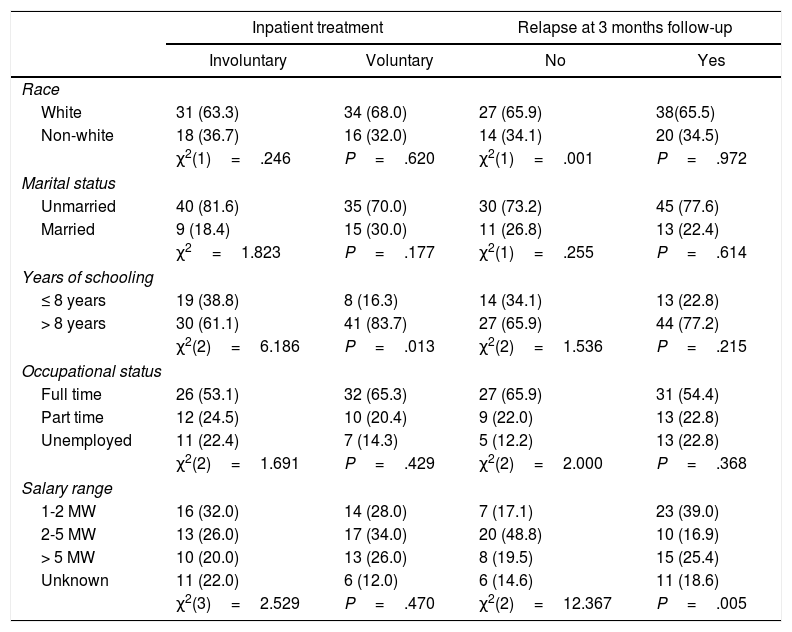
ResultsSocio-demographic DataThe sample was comprised by 100 drug dependent patients (mean age, 30.1±8.8 years old; range, 18-58). Socio-demographic profile for both groups (Table 1) presents homogeneity on the majority of variables. The sample was composed predominantly by Caucasians (63.3%), unmarried (81.6%), with more than 8 years of schooling (83.7%), full time job (53.1%), and receiving among 2-5 Minimum Wage (MW) (1 MW=788 Reais; 1 USD=∼3.30 Reais) (26%). The groups have differed only in relation to years of schooling. Table 2
Sociodemographic data and type of inpatient treatment.
| Inpatient treatment | Relapse at 3 months follow-up | |||
|---|---|---|---|---|
| Involuntary | Voluntary | No | Yes | |
| Race | ||||
| White | 31 (63.3) | 34 (68.0) | 27 (65.9) | 38(65.5) |
| Non-white | 18 (36.7) | 16 (32.0) | 14 (34.1) | 20 (34.5) |
| χ2(1)=.246 | P=.620 | χ2(1)=.001 | P=.972 | |
| Marital status | ||||
| Unmarried | 40 (81.6) | 35 (70.0) | 30 (73.2) | 45 (77.6) |
| Married | 9 (18.4) | 15 (30.0) | 11 (26.8) | 13 (22.4) |
| χ2=1.823 | P=.177 | χ2(1)=.255 | P=.614 | |
| Years of schooling | ||||
| ≤ 8 years | 19 (38.8) | 8 (16.3) | 14 (34.1) | 13 (22.8) |
| > 8 years | 30 (61.1) | 41 (83.7) | 27 (65.9) | 44 (77.2) |
| χ2(2)=6.186 | P=.013 | χ2(2)=1.536 | P=.215 | |
| Occupational status | ||||
| Full time | 26 (53.1) | 32 (65.3) | 27 (65.9) | 31 (54.4) |
| Part time | 12 (24.5) | 10 (20.4) | 9 (22.0) | 13 (22.8) |
| Unemployed | 11 (22.4) | 7 (14.3) | 5 (12.2) | 13 (22.8) |
| χ2(2)=1.691 | P=.429 | χ2(2)=2.000 | P=.368 | |
| Salary range | ||||
| 1-2 MW | 16 (32.0) | 14 (28.0) | 7 (17.1) | 23 (39.0) |
| 2-5 MW | 13 (26.0) | 17 (34.0) | 20 (48.8) | 10 (16.9) |
| > 5 MW | 10 (20.0) | 13 (26.0) | 8 (19.5) | 15 (25.4) |
| Unknown | 11 (22.0) | 6 (12.0) | 6 (14.6) | 11 (18.6) |
| χ2(3)=2.529 | P=.470 | χ2(2)=12.367 | P=.005 | |
MW: minimum wage.
Descriptive level of the chi-squared test [χ2, (df)]. N=50 (P≤.05).
Data are expressed as n (%).
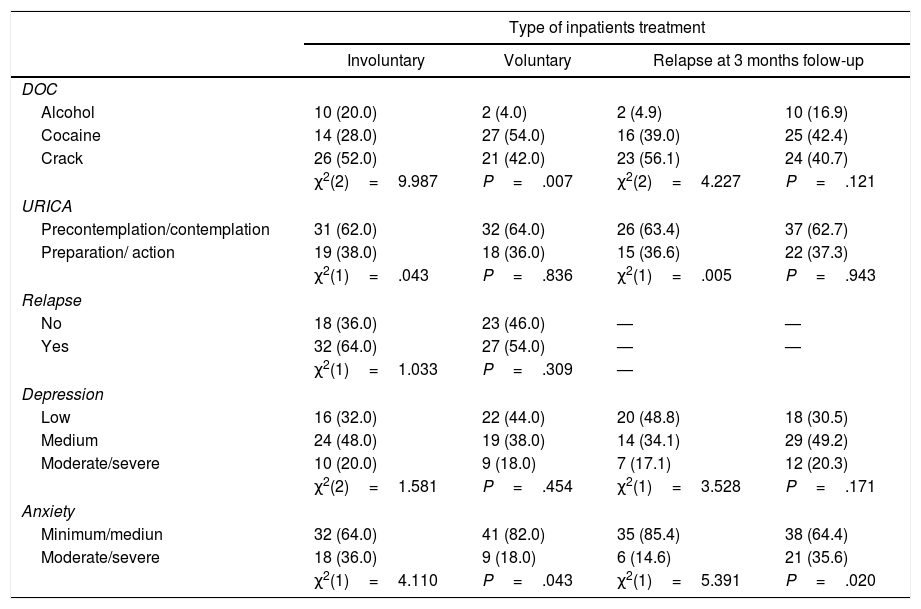
Drug of Choice (DOC), motivational stages, relapse, anxiety, depression and type of inpatient treatment.
| Type of inpatients treatment | ||||
|---|---|---|---|---|
| Involuntary | Voluntary | Relapse at 3 months folow-up | ||
| DOC | ||||
| Alcohol | 10 (20.0) | 2 (4.0) | 2 (4.9) | 10 (16.9) |
| Cocaine | 14 (28.0) | 27 (54.0) | 16 (39.0) | 25 (42.4) |
| Crack | 26 (52.0) | 21 (42.0) | 23 (56.1) | 24 (40.7) |
| χ2(2)=9.987 | P=.007 | χ2(2)=4.227 | P=.121 | |
| URICA | ||||
| Precontemplation/contemplation | 31 (62.0) | 32 (64.0) | 26 (63.4) | 37 (62.7) |
| Preparation/ action | 19 (38.0) | 18 (36.0) | 15 (36.6) | 22 (37.3) |
| χ2(1)=.043 | P=.836 | χ2(1)=.005 | P=.943 | |
| Relapse | ||||
| No | 18 (36.0) | 23 (46.0) | — | — |
| Yes | 32 (64.0) | 27 (54.0) | — | — |
| χ2(1)=1.033 | P=.309 | — | ||
| Depression | ||||
| Low | 16 (32.0) | 22 (44.0) | 20 (48.8) | 18 (30.5) |
| Medium | 24 (48.0) | 19 (38.0) | 14 (34.1) | 29 (49.2) |
| Moderate/severe | 10 (20.0) | 9 (18.0) | 7 (17.1) | 12 (20.3) |
| χ2(2)=1.581 | P=.454 | χ2(1)=3.528 | P=.171 | |
| Anxiety | ||||
| Minimum/mediun | 32 (64.0) | 41 (82.0) | 35 (85.4) | 38 (64.4) |
| Moderate/severe | 18 (36.0) | 9 (18.0) | 6 (14.6) | 21 (35.6) |
| χ2(1)=4.110 | P=.043 | χ2(1)=5.391 | P=.020 | |
Descriptive level of the chi-squared test [χ2, (df)]. N=50 (P≤.05).
Data are expressed as n (%).
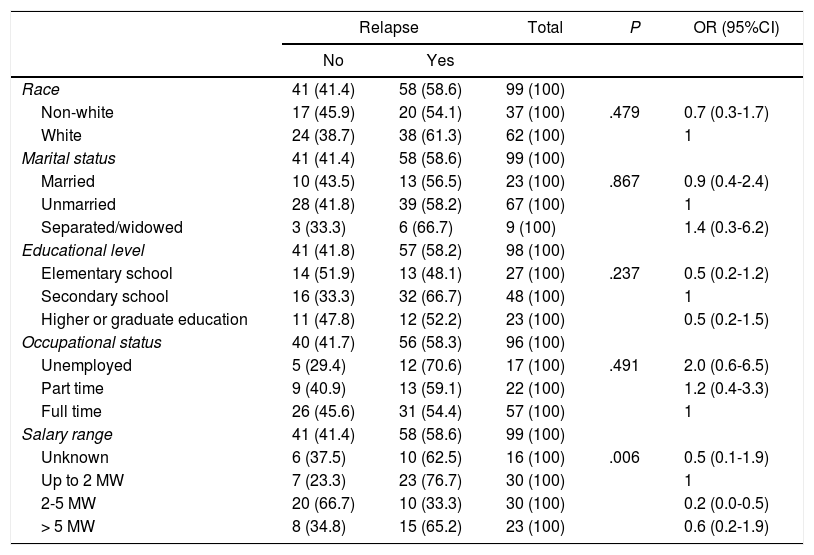
In the final model of regression analysis, controlled by treatment admission group (involuntary), variables such as civil status (single) and low educational level (< 8 years) remained significant. The chances to be admitted involuntarily was 4-fold more among single people (odds ratio [OR]=4; 95%CI, 1.274-8.553; P=.018), and in patients with low level of education (OR=3.7; 95%CI, 1.393-6.167; P=.020). Table 3
Final model of logistic regression analysis—Distribution of patients by relapse, according to socio-demographic characteristics.
| Relapse | Total | P | OR (95%CI) | ||
|---|---|---|---|---|---|
| No | Yes | ||||
| Race | 41 (41.4) | 58 (58.6) | 99 (100) | ||
| Non-white | 17 (45.9) | 20 (54.1) | 37 (100) | .479 | 0.7 (0.3-1.7) |
| White | 24 (38.7) | 38 (61.3) | 62 (100) | 1 | |
| Marital status | 41 (41.4) | 58 (58.6) | 99 (100) | ||
| Married | 10 (43.5) | 13 (56.5) | 23 (100) | .867 | 0.9 (0.4-2.4) |
| Unmarried | 28 (41.8) | 39 (58.2) | 67 (100) | 1 | |
| Separated/widowed | 3 (33.3) | 6 (66.7) | 9 (100) | 1.4 (0.3-6.2) | |
| Educational level | 41 (41.8) | 57 (58.2) | 98 (100) | ||
| Elementary school | 14 (51.9) | 13 (48.1) | 27 (100) | .237 | 0.5 (0.2-1.2) |
| Secondary school | 16 (33.3) | 32 (66.7) | 48 (100) | 1 | |
| Higher or graduate education | 11 (47.8) | 12 (52.2) | 23 (100) | 0.5 (0.2-1.5) | |
| Occupational status | 40 (41.7) | 56 (58.3) | 96 (100) | ||
| Unemployed | 5 (29.4) | 12 (70.6) | 17 (100) | .491 | 2.0 (0.6-6.5) |
| Part time | 9 (40.9) | 13 (59.1) | 22 (100) | 1.2 (0.4-3.3) | |
| Full time | 26 (45.6) | 31 (54.4) | 57 (100) | 1 | |
| Salary range | 41 (41.4) | 58 (58.6) | 99 (100) | ||
| Unknown | 6 (37.5) | 10 (62.5) | 16 (100) | .006 | 0.5 (0.1-1.9) |
| Up to 2 MW | 7 (23.3) | 23 (76.7) | 30 (100) | 1 | |
| 2-5 MW | 20 (66.7) | 10 (33.3) | 30 (100) | 0.2 (0.0-0.5) | |
| > 5 MW | 8 (34.8) | 15 (65.2) | 23 (100) | 0.6 (0.2-1.9) | |
95%CI: 95% confidence interval; MW: minimum wage; OR: odds ratio.
Descriptive level of the chi-squared test. N=50 (P≤.05).
Regarding the drug of choice (DOC), 87% of patients were crack cocaine users (41% inhaled and 47% smoked), 63% were in pre-contemplation stage/contemplation (URICA). The sample differed in relation to the DOC, type of inpatients treatment (χ2=9.987; P=.007), and anxiety level (P=.043). There were predominate voluntary impatient admissions among cocaine users and involuntary admissions among crack users with statistically significant differences (P=.007). Cocaine use reduces the chances in 91.2% (OR=0.088; 95%CI, 014-571; P=.014) of being involuntary admitted.
Depression and AnxietyIn the sample, 43% were medium depression and 73% minimum level/medium anxiety.
Motivational StagesIn the independent t-test, to compare the motivational stages, it is noted that the participants admitted in volunteered group in the contemplation stage (URICA) higher mean values (10.3±0.573; t=–3.237; 95%CI, –0.965-0.226), compared with those admitted at involuntarily group (9.7±0.821; t=–3.275; 95%CI, –0.959-0.231), with statistically significant differences (P=.002). While involuntarily admission group had higher average values in action stage (URICA) (12.2±0.688; t=3.045; 95%CI, 0.209-1.043), and voluntarily admissions group (11.6±0.550; t=3.064; 95%CI, 0.211-1.041), with statistically significant differences (P=.004). When evaluating motivational stages of SOCRATES, there were no differences in the type of admissions groups. The URICA was not significant in the evaluation (P≥.05).
The variables “occupational status, relapse and type of admission group” were a predictor that significantly influence the user's motivation in the contemplation stage (P≤.05). All other variables were controlled in this assessment, however, there were not statistically significant. The variables “occupational status, anxiety, alcohol and type of admission group” were significant predictors, which has a significant effect on action preparation stage (P≤.05). In SOCRATES scale, only the variables “anxiety and alcohol” were predictors that influence the recognition motivational stage. Anxiety interferes with ambivalence (SOCRATES). The subscale action (SOCRATES) was compared, but no significant statistical values (P≥.05) were observed.
RelapseIn the sample, 59% relapsed in three months at follow up. No significant differences between replaces between patients who were admitted at involuntarily group (64%) and at voluntary group (54%). There was an association between relapse and family income (P=.006). Thus, it is noted that patients with up to 2 MW showed a higher percentage of relapse (76.7%) compared to the others. In contrast, patients with a family income between 2 and 5 MW had the highest percentage of cases without relapse (66.7%). In bivariate and multivariate analysis, there were no association between relapse and type admission group (voluntary or involuntary); however, as seen, this variable is influenced by the motivation stage. The variable relapse was significant at final model binary logistic regression analysis (P<.05).
DiscussionThe findings of this study indicate that relapse after 3 months of follow-up are high in voluntary and involuntary admissions and associated with low family income. Nevertheless, no significant differences between patients who were admitted involuntarily (64%) and voluntary (54%). The results corroborate to caution into the evidence-based claims made by previous researchers and clinicians that compulsory and involuntary treatment is effective in the rehabilitation of substance users. Many evidences show us that effectiveness seen not to dependent only on voluntary or involuntary admissions, because many other factors may interfere with these outcomes, which should be measured and controlled in future studies with different designs and larger samples.19
It's worth to take in mind that in this study only 1 outcome (relapse) measure was evaluated. Previously studies showed that involuntary admission can increased retention time in treatment, reduction of risk of aggression against third persons, has lower criminal involvement at post discharge.15 It also is being related to an opportunity to clear up the diagnostic or the initial medication for those more resistant to accept it or with psychoses comorbidity, to solve an acute situation.20 A literature review revealed that most involuntarily admitted patients show considerable clinical problems improvement over time.21 Therefore, between 33% and 81% of patients regard the admission as justified and/or the treatment as beneficial.21
Our results corroborate those of previous studies that showed that involuntary admission has also been associated with socio-economic deprivation in several countries and, especially, low social support and psychosocial vulnerability. The demographic and clinical variables associated with involuntary admission in Brazil for substance dependent patients are yet incompletely understood. In addition, studies on involuntary hospitalization are revisions of literature16 and focusing on ethical political, legal and human rights, and less on clinical and health aspects.22
Another important finding of our study refers to the motivational levels (URICA) that influence the type of treatment (voluntary/involuntary) and relapse. Several are the barriers for behavioral changes related to drug use, which might influence the patients of this study. It is noteworthy that the low motivational levels, stages of precontemplation and contemplation, remained associated with the final model related to relapse and type of admissions. The motivation has been considered the cornerstone of success and failure in treatment outcomes between drug users. It has been brought out that lack of motivation is among the main reasons for abandoning treatment, failure therapeutic commitment, relapses and negative results during treatment.23 Studies indicate that motivations surrounding behaviour change and treatment entry have consistently been found to be predictive of engagement in treatment. In adolescent and adult, literature studies the factors that influence motivational variables, including substance use quantity and frequency, family support, peer and legal involvement, and mental health status (eg, anxiety, depression…).24
Clearly, there is a scarcity of population and clinical studies evaluating any outcome of involuntary admissions for drug users in the country. Although there is a paucity of data to compare the findings of our study with other national ones, it is worth highlighting the originality of this study. This is one of the first studies to evaluate the relationship between admission groups (voluntary and involuntary), motivational stages and relapse after 3 months of follow-up after discharge in a Brazilian sample of substance users admitted to treatment in a TC care model.
LimitationsRelapse rates were not monitored through urinalysis, but only through self-reporting of patients. This sample consisted of only men and was obtained from a single TC. It is also worth mentioning as limitations that no other information was collected on the pattern and severity of substance dependence that may influence the outcome after the admission period.
Implications to Clinical PracticeIt is imperative the development of supplementary professional guidelines and training in motivations techniques for all professionals involved in the rehabilitation treatment acceptance process of alcohol and other drugs in involuntary model. It is important that the staff can be fully aware of their ethical boundaries and care, respecting the laws of the country and especially guarantee the dignity of persons with problems by substance use and their families.25
Implications to Future StudiesIt is suggested that future studies on TC should evaluate other variables outcome such as comorbidity, violence, and criminality, and the use of other methodologies, such as clinical trial and naturalistic studies.
ConclusionsIn this sample, the relapse outcome in involuntary admission was no different from the voluntary model.
Conflict of interestThe authors have no conflict of interest to declare.