The 2019 coronavirus disease (COVID-19) outbreak caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has affected virtually every country and territory in the world, leading it to be declared a global pandemic on 11 March 2020.1 Eleven months since the outbreak of the infectious disease, people around the world continue to struggle without definitive measures to prevent or treat COVID-19, except for the widely proposed measures of social distancing, mask and hand hygiene.2 At the time of writing (27 February 2021), the number of confirmed COVID-19 cases exceeds 108.2 million worldwide.3
The long period of quarantine, along with the increasing number of deaths and confirmed cases, has caused many people to suffer from serious emotional problems, resulting in psychological disorders such as depression, anxiety and fear of death.4 An increase has also been found in the number of suicide deaths due to the psychological and social effects of the COVID-19 pandemic.5
Brooding about this infectious disease can be harmful and unhealthy. In fact, the above psychological health conditions can be influenced by excessive and repetitive thinking about COVID-19.6 Social isolation and repeated exposure to information about COVID-19 in the news can stimulate obsessive thoughts in some people, ultimately resulting in psychological distress and, in severe cases, mental disorders.6 University students are particularly vulnerable to mental health issues and obsessive thinking about COVID-19, as strict social distancing measures and lockdowns left many students not only unsure about their health, but also about their academic status and their career plans.7 University students are also prone to psychological problems due to the highly stressful and often overwhelming challenges they face in adjusting to a new lifestyle and a whole set of academic responsibilities resulting from closure of the universities and online teaching8, all of which has greatly changed their approach to academic tasks and organisation of their personal and social lives.
Death anxiety (DA) is a reaction people have when faced with death or a chronic or life-threatening illness. DA is expressed as the perception of hazard to life in day-to-day interactions.9
Due to its inherent adverse nature, death generates various types of attitude and emotion, and fear and anxiety are the most common findings.9 Nevertheless, the conceptualisation of death is abstract and complex and has multiple meanings, so approaching and understanding it will depend on many factors. Moreover, people's concepts of death are relative and temporary, and vary with the development of the individual during the different stages of life. Death during the COVID-19 pandemic is the thought that haunts the most and causes anguish and anxiety. Nobody feels good when faced with people infected by this virus or at risk of dying from complications, perhaps because it makes them think of their own death.9
Menzies et al10 argue that the COVID-19 situation presents unique challenges for our species because of the constant reminders of death. They report that images of death are ever present in daily updates of SARS-CoV-2 transmissions, while other signs of death (e.g., face masks) mean that there is essentially a significant experience of global mortality in progress.
At the same time, a relationship has been found between death anxiety and obsession.11,12 As the perception of a high risk of infection due to the pandemic causes symptoms of distress, the death of loved ones and the recommendation to wash hands repeatedly can create disturbing thoughts and behaviours related to the infectious disease, and this can then lead to obsessive-compulsive disorder (OCD). OCD is a psychiatric disorder involving persistent and intrusive thoughts and compulsive behaviours that consume a great deal of time and energy, and an escalation in the symptoms has been seen in the context of COVID-19.13,14
After a brief review of the scientific literature, we found no Latin American studies that include dynamic evaluation of obsession and death anxiety due to COVID-19 through network analysis. We believe it is essential to explore how the elements of both concepts are mutually reinforcing. Our objective was therefore to explore the correlation networks of obsession and death anxiety due to COVID-19 in Peruvian health science students.
We conducted an exploratory, correlational, cross-sectional study in the metropolitan city of Lima, Peru, during the second Peruvian lockdown in February 2021. We used the Spanish versions of the following instruments: Obsession with COVID-19 Scale (OCS), composed of four items that assess the symptoms of higher risk of obsession with COVID-196; and the Peruvian version of the Death Anxiety Scale, COVID-19 version (DAS), composed of 12 items15. However, three of these items were eliminated due to being written with the opposite meaning and deemed redundant (2, 5 and 6), leaving nine items. We estimated the alpha and omega reliability of the instruments, with the values being >0.83.
This study included 546 university health science students (69.35% female; mean age, 24.45 years). Due to the social distancing and restricted mobility measures introduced by the government, it became necessary to use online survey methods. Participants were recruited using a snowball sampling technique through social media, such as WhatsApp groups, Facebook and Google groups, and were encouraged to invite their family and friends to taken part in the survey. The survey was created and administered using Google Forms and included informed consent, which was obtained from all participants enrolled in the study.
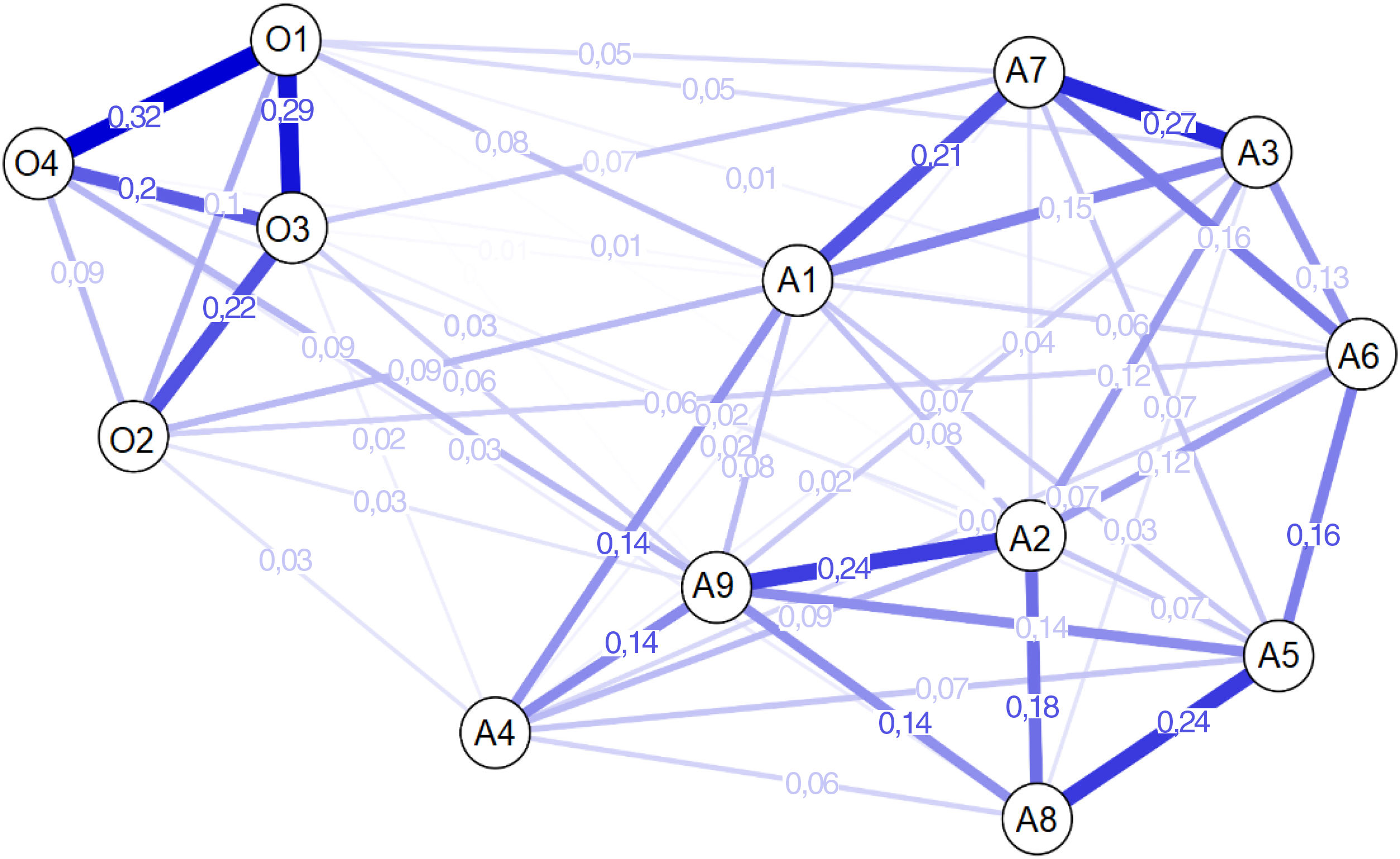
Through the R qgraph package and the graph-fused LASSO (least absolute shrinkage and selection operator), the patterns of the interactive system whose connections represent partial correlations on the network graph were assessed graphically; LASSO estimator allowed spurious relationships to be eliminated.16,17 The items (nodes) are interconnected by lines or edges that represent the partial correlations that tend to be located in the network according to the sum of connections with other nodes.16,17 The interpretation of the partial correlation measures shows effect sizes, interpretation of which in the health sciences is explained by Sullivan et al.18 The network approach includes centrality measures; the expected strength index is the most stable measure for determining the importance of the components in dynamic correlations.16,17
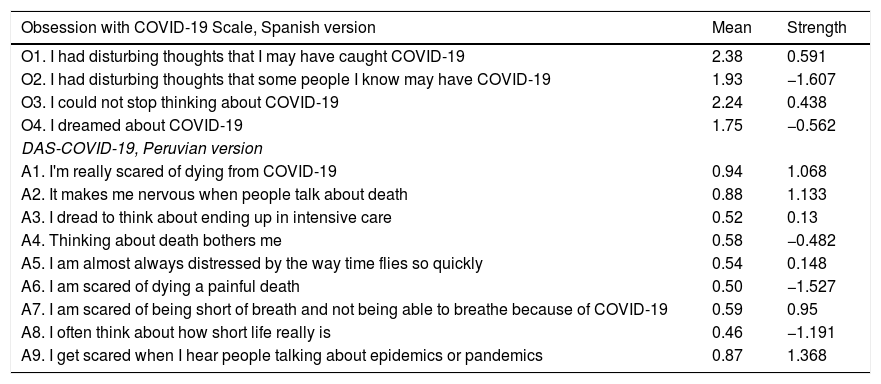
Table 1 shows the descriptive statistics of the participants' responses to the measures used. These data indicate a higher report of items O1 and O3 of the Obsession with COVID-19 Scale and items A1, A2 and A9 of the DAS-COVID-19, which in turn reported the best network strength centrality measures.
Mean of the items and strength centrality measures.
| Obsession with COVID-19 Scale, Spanish version | Mean | Strength |
|---|---|---|
| O1. I had disturbing thoughts that I may have caught COVID-19 | 2.38 | 0.591 |
| O2. I had disturbing thoughts that some people I know may have COVID-19 | 1.93 | −1.607 |
| O3. I could not stop thinking about COVID-19 | 2.24 | 0.438 |
| O4. I dreamed about COVID-19 | 1.75 | −0.562 |
| DAS-COVID-19, Peruvian version | ||
| A1. I'm really scared of dying from COVID-19 | 0.94 | 1.068 |
| A2. It makes me nervous when people talk about death | 0.88 | 1.133 |
| A3. I dread to think about ending up in intensive care | 0.52 | 0.13 |
| A4. Thinking about death bothers me | 0.58 | −0.482 |
| A5. I am almost always distressed by the way time flies so quickly | 0.54 | 0.148 |
| A6. I am scared of dying a painful death | 0.50 | −1.527 |
| A7. I am scared of being short of breath and not being able to breathe because of COVID-19 | 0.59 | 0.95 |
| A8. I often think about how short life really is | 0.46 | −1.191 |
| A9. I get scared when I hear people talking about epidemics or pandemics | 0.87 | 1.368 |
The most central components of greatest strength in the network belong to the death anxiety domain (A1, A2 and A9). Fig. 1 shows the highest relationships between symptoms O1–O4 and O1–O3 with respect to the symptom dynamics of obsession, and higher associations between items A3–A7, A2–A9 and A5-A8 in the death anxiety domain. Inter-domain relationships indicate that each obsessive symptom reports four causal associations with the components of death anxiety. Standing out for their greater size are items A1 (“I’m really scared of dying from COVID-19”) and O2 (“I had disturbing thoughts that some people I know may have COVID-19”), showing a higher prevalence of fear of death and thoughts that the people around them are infected; this denotes the state of anguish reported by Peruvian university students. This indicator of DA also showed a major dynamic association with item O1 (“I had disturbing thoughts that I may have caught COVID-19”), suggesting that fear of death is also reinforced by obsession about being infected, which together can lead to cognitive difficulties and increased mistrust, which limits social relationships.
Another significant relationship was between the measures of A9 (“I get scared when I hear people talking about epidemics or pandemics”) and O4 (“I dreamed about COVID-19”), which implies that a higher state of nervousness when receiving pandemic information can even affect sleep status. Two of the most central items (A1 and A9) show a greater association with the symptoms of obsession, which points to a new area for research in the psychiatric field from the perspective of complex models of comorbidity.19 Such connections reinforce possible activation routes of both variables of negative impact due to COVID-19. We therefore recommended that future interventions consider targeting these indicators, with the aim of reducing their intensity and preventing the development of potentially serious psychopathological disorders such as OCD.
Conflicts of interestNone.
Please cite this article as: Ramos-Vera C. Las relaciones dinámicas de red de la obsesión y la ansiedad ante la muerte por COVID-19 durante la segunda cuarentena en universitarios peruanos. Rev Colomb Psiquiat. 2021;50:160–163.