Pulmonary rheumatoid nodules are an uncommon extra-articular manifestation of rheumatoid arthritis (RA). Its study is important because the clinical and imaging presentation could be confused with tuberculosis, fungal infections, and/or lung neoplasms. Pulmonary nodules produce few symptoms and can lead to fatal complications such as pneumothorax, bronchopleural fistula, and a superinfection with abscess formation. The fundamental diagnostic confirmation is the histopathological study because it is an exclusion diagnosis. The treatment needs clinical follow-up as there is no targeted therapy, with Rituximab and Tocilizumab being used in severe cases. In general, their appearance tends to lead to a poorer prognosis of patients with RA.
Los nódulos reumatoides pulmonares son una manifestación extra-articular infrecuente de la artritis reumatoide (AR). Su estudio es importante porque su presentación clínica e imagenológica puede confundirse con tuberculosis, infecciones fúngicas y neoplasias pulmonares. Producen pocos síntomas y pueden conducir a complicaciones fatales como neumotórax, fístula broncopleural y sobreinfección con formación de abscesos. La confirmación diagnóstica fundamental descansa en el estudio histopatológico, dado que es un diagnóstico de exclusión. El tratamiento precisa seguimiento clínico ya que no hay una terapia dirigida utilizándose en casos severos rituximab y tocilizumab. En general, su aparición tiende a empobrecer el pronóstico de los pacientes con AR.
Pulmonary manifestations of rheumatoid arthritis (RA) are infrequent and they include: involvement of the small airway and the pleura, pulmonary rheumatoid nodules, drug-induced lesions, interstitial lung disease and tumors.
Pulmonary rheumatoid nodules are oligosymptomatic, although they can produce upper respiratory symptoms and hemoptysis. Their radiological characteristics, serum markers and histopathology allow us to differentiate them from diagnosis such as infections, neoplasms or drug toxicity.
We present the case of a woman with a diagnosis of RA from the National University Hospital of Bogota, Colombia, in whom cavitating pulmonary nodules were documented.
Case descriptionA 65-year-old woman with 6 days of cough, hemoptoic expectoration and left pleuritic pain, without fever or dyspnea. History of RA for 15 years under treatment with methotrexate (MTX)-leflunomide, and former heavy smoker.
On admission, the patient had left chest pain and tachycardia. Auscultation with decreased breath sounds and fine crackles in the left hemithorax; bilateral ulnar deviation, swollen joints: 9, painful: 2, assessment of disease activity by CDAI: 14. Normal blood tests with hemogram and renal function, CRP: 24.8mg/dl, ESR: 48mm/h and rheumatoid factor: 40.7IU/ml (0-14IU/ml).
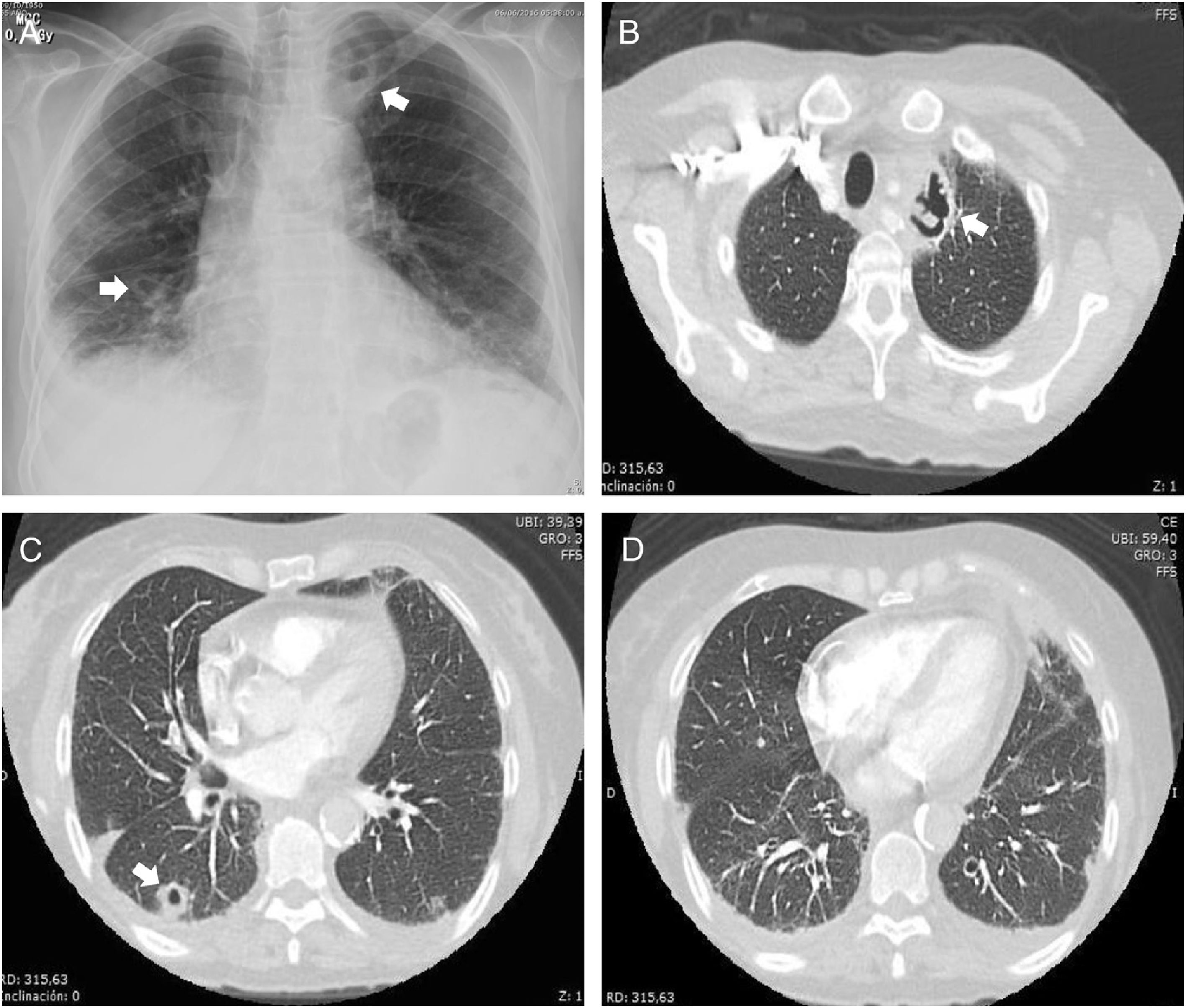
Antibiotic therapy with piperacillin/tazobactam plus clarithromycin was started. Due to suspicion of pulmonary thromboembolism (PTE), it was performed an angiotomography, observing multiple nodules of soft tissue density, poorly defined, of 16-30mm, subpleural and cavitary; cavitary mass in the apicoposterior segment of the left upper lobe of 37mm in diameter, with bilateral basal interstitial involvement (Fig. 1), negative for PTE.
The following differential diagnoses were proposed: septic embolism, tuberculosis, fungal infection, rheumatoid lung, and MTX-leflunomide toxicity.
Considering the risk of worsening the lung compromise with MTX and leflunomide, treatment with chloroquine 250mg/day and sulfasalazine was started and the antibiotic was discontinued; a fibrobronchoscopy with bronchoalveolar lavage showed 60% of polymorphonuclear cells without malignancy. The transbronchial biopsy evidenced an abundant polymorphonuclear inflammatory component without malignancy or granulomas. Negative PCR for tuberculosis. The patient presented improvement, reduction of joint pain and swelling, and was discharged after 7 days.
DiscussionPulmonary rheumatoid nodules are an uncommon extra-articular manifestation of RA. They predominate in men with a 7:1 ratio and appear late in the course of the disease.1
The risk factors include: male gender, age, smoking, HLA-DRB1, severe erosive arthritis, subcutaneous nodules and high titers of rheumatoid factor. Their prevalence varies according to the study: by chest X-ray 1%, by HRCT 20-22% and by biopsy 32%.2
They are oligosymptomatic, although they can occur with cough and hemoptysis. The latency period ranges between 6 months and 11 years. Imagenologically they are bilateral, peripheral and subpleural, they measure up to 7cm and 30% become cavitated. They can become calcified and be associated with pneumoconiosis, a condition called Caplan's syndrome.2
Differential diagnoses include:
- -
Pulmonary tuberculosis and infections with Aspergillus/Criptococcus: They occur with fever, constitutional symptoms and clinical course of relapse-remission.
- -
Septic emboli.
- -
Primary pulmonary neoplasm/metastases: Cavitating nodules, with irregular borders and size >1cm.
- -
Pulmonary nodulosis accelerated by methotrexate (associated with the HLA-DRB1*0401 allele) and nodules induced by leflunomide, azathioprine and etanercept.3–5
The diagnosis relies on the clinical presentation, radiology, serum markers, biopsy that rules out neoplasm or infection and absence of temporal relationship with the use of drugs associated with nodulosis (DMARDs and anti-TNF).6
Histopathologically, they show central necrosis surrounded by lymphocytes, plasma cells, polymorphonuclear cells and perivascular granulation tissue. They are T helper-1 lymphocytes-mediated granulomas. An extensive polymorphonuclear component was found in our case in contrast with the classical histological description.
The complications include hemoptysis, bronchopleural fistula, pneumothorax and abscesses.2
There is no specific treatment and most of them remit spontaneously, without any relation to the evolution of the arthritis.6 In symptomatic cases requiring treatment, rituximab7 and tocilizumab8 have shown to be useful.
The prognosis is worse in patients with RA and pulmonary rheumatoid nodules.
ConclusionPulmonary rheumatoid nodules are uncommon and have a poor prognosis because they are associated with severe joint commitment and greater mortality.
Their most serious complications are hemoptysis, bronchopleural fistula and pneumothorax. They should be considered in the differential diagnosis of nodules due to pulmonary tuberculosis and neoplasms; that is why their diagnosis is based on the clinical presentation and the histopathological study, after excluding other potentially serious causes. In the great majority of cases they do not require treatment.
Conflict of interestThe authors declare they do not have any conflict of interest.
Please cite this article as: León-Sierra LP, Cajas-Santana LJ, Torres-Saavedra FA. Nódulo pulmonar cavitado en artritis reumatoide: reporte de un caso. Rev Colomb Reumatol. 2018;25:146–148.