Ergotism is a vasospasm that affects visceral and peripheral muscle arteries. Classically, symmetrical involvement of lower limb arteries is described, and is often associated with a history of chronic consumption of ergotamine derived medications (Cafergot).
Case reportA 22 year-old healthy man with infectious mononucleosis syndrome, who presented with a sudden onset of paraesthesias in the lower limbs, as well as livedo reticularis. The initial diagnosis was a medium-sized vessel vasculitis (polyarteritis nodosa). The symptoms were preceded by the administration of Cafergot for headache treatment, and resolved spontaneously. The magnetic resonance angiography (MRA) of the lower limbs showed occlusion of peroneal arteries, with filiform distal flow. Other infectious, autoimmune and cardiovascular origins were ruled out.
DiscussionErgotism is an important differential diagnosis in the study of the patient with vasculitis, especially in acute onset presentations. Its treatment is the suspension of the causal drug, with vasodilator and surgical vascular procedures, if necessary.
ConclusionsErgotism is an imitator of vasculitis, especially in young patients with a history of difficult to control migraine. The concomitant administration of CYP3A4 inhibitors (mainly, protease inhibitors and macrolides) enhances the toxic effects of ergot.
El ergotismo es un vasoespasmo que afecta las arterias musculares periféricas y viscerales. Clásicamente se describe la afectación simétrica de las arterias de las ex-tre-mi-da-des inferiores, a menudo asociada con el consumo crónico de medicamentos derivados de ergotamina (Cafergot®).
Caso clínicoVarón sano de 22 años con síndrome de mononucleosis, presentó parestesias en las extremidades inferiores y livedo reticularis de forma súbita, el diagnóstico inicial fue una vasculitis de mediano vaso (poliarteritis nodosa). Los síntomas fueron precedidos por la administración de Cafergot® para el tratamiento de cefalea, y se resolvieron espontáneamente. La angiografía por resonancia magnética (ARM) de las extremidades inferiores mostró oclusión de las arterias peroneas, con flujo distal filiforme. Se descartaron otras etiologías infecciosas, autoinmunes y cardiovasculares.
DiscusiónLos ergotismos son un diagnóstico diferencial importante en el estudio del paciente con vasculitis, especialmente en presentaciones de inicio agudo. Su tratamiento es la suspensión del fármaco causal, vasodilatadores y procedimientos vasculares quirúrgicos, si es necesario.
ConclusionesEl ergotismo es un imitador de vasculitis, especialmente en pacientes jóvenes con antecedentes de migraña de difícil control. La administración concomitante de inhibidores del CYP3A4 (principalmente, inhibidores de proteasa y macrólidos) potencia los efectos tóxicos del ergot.
Ergotism was initially described as an epidemic that appeared in medieval Europe between the 9th and 11th centuries1; There were two forms: a convulsive, directly related to the consumption of the ergot fungus (Claviceps purpurea) and a gangrenous characterized by the appearance of blisters, acral necrosis and paresthesias in upper and lower limbs, referred as fire of Saint Anthony.1,2 Currently, the use of ergot alkaloids is not recommended as first-line medications neither for migraine nor for postpartum haemorrhage; however, their wide distribution, particularly of ergotamine and methylergonovine, has led to the presence of vasospastic complications, although it remains a rare adverse effect (0.001–0.002% among patients with migraine).3 The chronic use of ergotamine with other medications (macrolide antibiotics, non-selective beta-blockers, protease inhibitors, nicotine and cocaine) is associated to acute arterial occlusion; the differential diagnoses are atherosclerosis, primary vasculitis, fibromuscular dysplasia and thromboembolic phenomena.4 We present a case of ergotism that was initially diagnosed as polyarteritis nodosa.
Clinical caseA previously healthy 22-year-old man was admitted to the hospital after 14 days of fever, asthenia, headache and sore throat, without any significant findings at physical examination. In the admission laboratories, lymphopenia, C Reactive Protein (CRP) of 12.14mg/dl (range 0–2mg/dl) and positive heterophil antibodies were documented. After several days, the initial symptoms, as well as the lymphopenia and elevation of CRP resolved spontaneously; a diagnosis of an infectious mononucleosis syndrome was made.
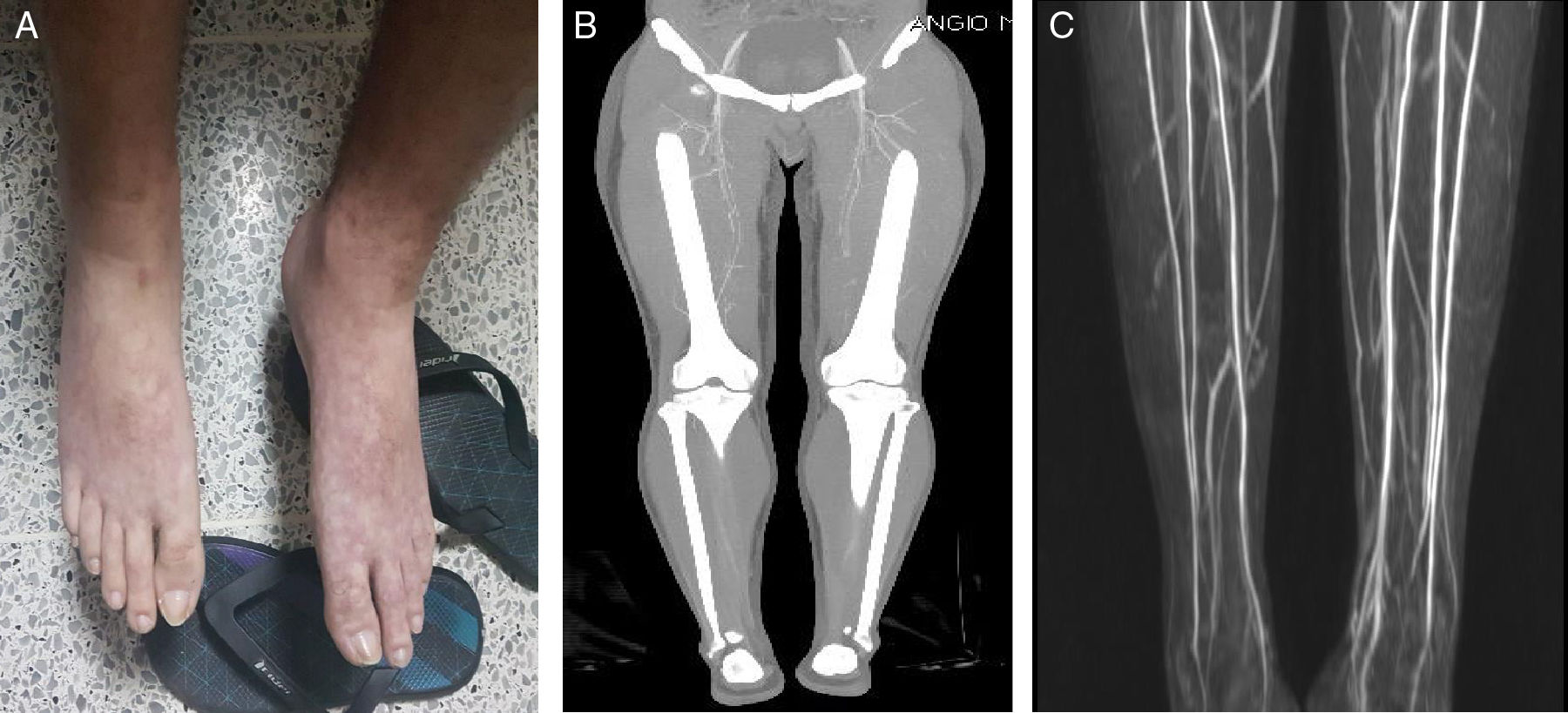
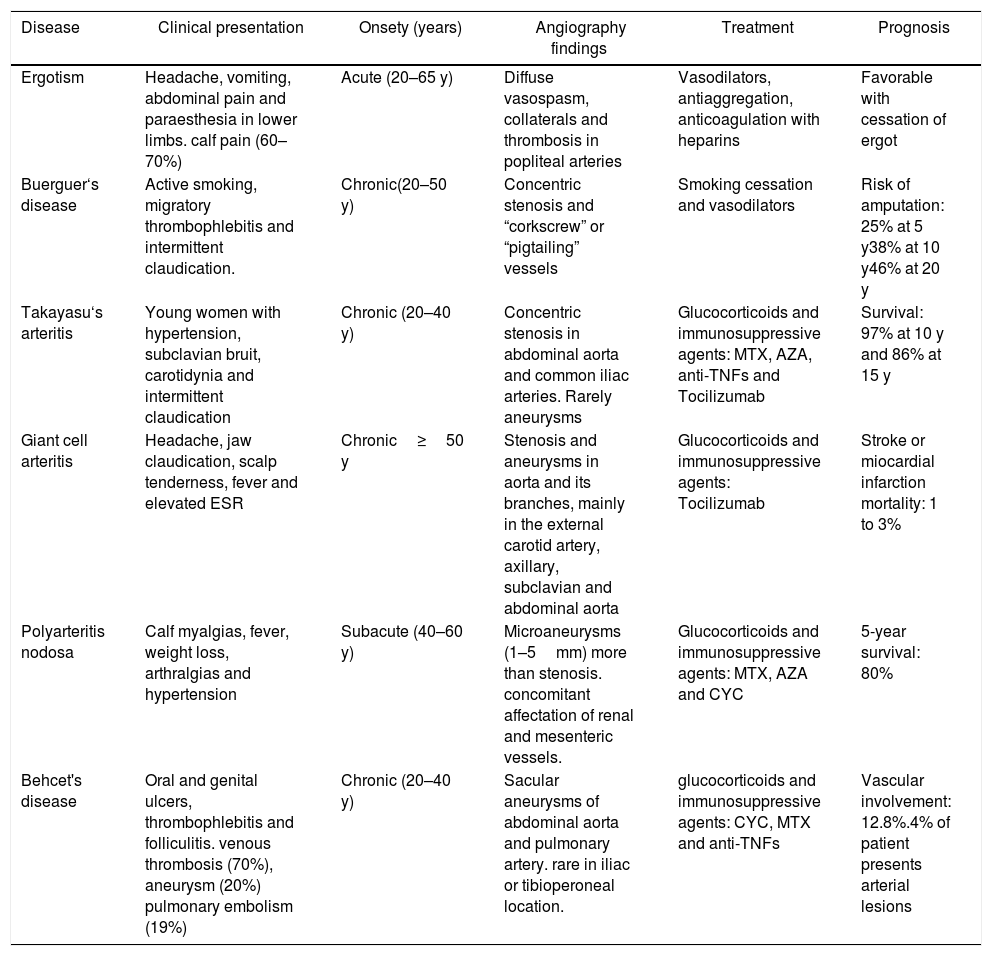
A lumbar puncture was performed; after the procedure, the patient complained of headache only present while seated or standing up, which ameliorated in recumbent position. A diagnosis of intracranial hypotension due to lumbar puncture was made. Paracetamol 500mg and caffeine 100mg/ergotamine 1mg three times daily were administered. Four days after, the headache and all the initial symptoms disappeared, but he developed pressure in both flanks, and myalgia in calves, the caffeine/ergotamine pills were suspended; two days after, the patient presented livedo reticularis in the feet, absence of distal pulses and severe pain (Fig. 1A). Aspirin 300mg orally, saline solution 500ml in a bolus, and hydromorphone 0.4mg intravenously, were administered without improvement. Blood cultures, HIV, Hepatitis B virus, hepatitis C, VDRL, ANAs, ENAs, ANCAs, complement and cryoglobulins were negative. The thorax radiography and the transthoracic echocardiography were normal. A computed tomographic angiogram was performed, which reported occlusion of both peroneal arteries, with filiform flow distal to them (Fig. 1B). Due to suspicion of vasculitis, pulses of intravenous methylprednisolone 500mg daily were administrated for three days. After the first infusion, all signs and symptoms of vascular occlusion resolved without sequelae or recurrence. A magnetic resonance angiogram was performed 13 days after the symptoms disappeared, which showed a completely normal artery system in both lower limbs, without changes in soft tissues (Fig. 1C).
Due to the time closeness of administration of ergotamine, the characteristic symptoms (pressure in both flanks, arterial claudication) previous to vasospasm, the onset of vascular occlusion signs, and the absence of common causes, a diagnosis of ergotism was made.
DiscussionWe described the case of a man who presented with diffuse lower limbs arteries vasospasm and livedo reticularis that was initially confused with polyarteritis nodosa, but improved after suspending Cafergot, a potent vasoconstrictor derived from ergotamine.
The ergot alkaloids are modified amino acids with central sympatholytic activity, α-adrenergic, dopaminergic and serotonergic agonist action together with a direct vasoconstrictor effect in the vascular and uterine smooth muscle.2 They have a poor absorption (50%) and oral bioavailability (less than 2%), mainly due to their extensive first-pass metabolism in the liver (90%, by CYP enzymes, especially the 3A4 isoform)1,3; they have an irreversible vasoconstrictor effect that is related to the greater amount of collagen and the lower presence of elastin at the arterial level, so it preferentially affects muscle arteries at the visceral and peripheral levels.5 The maximum doses of ergotamine tartrate are 4–6mg in a single dose and up to 10mg per week orally.1
Ergotamine tartrate and dihydroergotamine have potent α-agonist activity in contrast to methylergonovine, which has no α-activity but has preferential constrictor properties for uterine smooth muscle.2,5 Ergotism is a vasospastic condition that appears as an adverse effect in three scenarios1:
- 1.
Acute administration of high doses orally.
- 2.
Chronic administration of therapeutic doses by oral route.
- 3.
Administration of therapeutic doses with an idiosyncratic effect, not dose-dependent.
The appearance of ergotism is less frequent after the intravenous administration of dihydroergotamine in patients with abnormal autonomic regulation, for thromboembolic prophylaxis or for managing intractable cases of migraine.1,3 Vasospasm is clinically manifested acutely by headache, vomitus, diarrhea, abdominal pain, lumbar pain and later, calf claudication, livedo reticularis, pallor, coldness, cyanosis, paresthesias and ischemia in multiple territories: cerebral, carotid, ophthalmic, coronary, mesenteric, renal and more frequently in pelvic arteries and lower limbs, with severe cases of ulceration, gangrene and amputation.2,6 Sometimes, paresthesias in distal areas may precede the picture for weeks.1 An additive effect can be seen in patients who consume LSD (diethylamide of lysergic acid), propanolol, sumatriptan, clarithromycin, ritonavir, oral contraceptives, nicotine and cocaine.3,4,7,9 Convulsive ergotism has not been reported with the use of pure ergotamine compounds.1
The most affected are the popliteal arteries (60–70% of cases) symmetrically, although unilateral involvement has also been reported4; The findings described in arteriography are: a diffuse or pencil-shaped spasm, collateral circulation (which can be reversed with the suspension of the drug) and thrombosis.1 It is very rare that aneurysms appear and their presence forces to rule out other causes of arterial occlusion.4
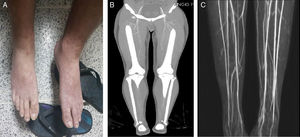
The diagnosis is clinical and confirmed by arteriography or, more recently, by non-invasive studies such as computed angiotomography and angioresonance, which demonstrate reversible vascular changes unless there is extensive necrosis, which correlates with more serious lesions.1,4 However, it requires a high suspicion and is considered a diagnosis of exclusion within the imitators of vasculitis. In the group of primary vasculitis, it is necessary to differentiate between six pathologies: Buerguer's disease, Takayasu's arteritis and less frequently, polyarteritis nodosa, Behcet's disease, giant cell arteritis with extracranial involvement and Kawasaki disease4,6,9 (Table 1).
Differential diagnoses of ergotism and primary vasculitis.
| Disease | Clinical presentation | Onsety (years) | Angiography findings | Treatment | Prognosis |
|---|---|---|---|---|---|
| Ergotism | Headache, vomiting, abdominal pain and paraesthesia in lower limbs. calf pain (60–70%) | Acute (20–65 y) | Diffuse vasospasm, collaterals and thrombosis in popliteal arteries | Vasodilators, antiaggregation, anticoagulation with heparins | Favorable with cessation of ergot |
| Buerguer‘s disease | Active smoking, migratory thrombophlebitis and intermittent claudication. | Chronic(20–50 y) | Concentric stenosis and “corkscrew” or “pigtailing” vessels | Smoking cessation and vasodilators | Risk of amputation: 25% at 5 y38% at 10 y46% at 20 y |
| Takayasu‘s arteritis | Young women with hypertension, subclavian bruit, carotidynia and intermittent claudication | Chronic (20–40 y) | Concentric stenosis in abdominal aorta and common iliac arteries. Rarely aneurysms | Glucocorticoids and immunosuppressive agents: MTX, AZA, anti-TNFs and Tocilizumab | Survival: 97% at 10 y and 86% at 15 y |
| Giant cell arteritis | Headache, jaw claudication, scalp tenderness, fever and elevated ESR | Chronic≥50 y | Stenosis and aneurysms in aorta and its branches, mainly in the external carotid artery, axillary, subclavian and abdominal aorta | Glucocorticoids and immunosuppressive agents: Tocilizumab | Stroke or miocardial infarction mortality: 1 to 3% |
| Polyarteritis nodosa | Calf myalgias, fever, weight loss, arthralgias and hypertension | Subacute (40–60 y) | Microaneurysms (1–5mm) more than stenosis. concomitant affectation of renal and mesenteric vessels. | Glucocorticoids and immunosuppressive agents: MTX, AZA and CYC | 5-year survival: 80% |
| Behcet's disease | Oral and genital ulcers, thrombophlebitis and folliculitis. venous thrombosis (70%), aneurysm (20%) pulmonary embolism (19%) | Chronic (20–40 y) | Sacular aneurysms of abdominal aorta and pulmonary artery. rare in iliac or tibioperoneal location. | glucocorticoids and immunosuppressive agents: CYC, MTX and anti-TNFs | Vascular involvement: 12.8%.4% of patient presents arterial lesions |
The treatment of ergotism implies an early diagnosis to avoid severe and irreversible complications and is based fundamentally on the withdrawal of the drug.1,2 There is no dose-dependent relationship and, although the lesions typically improve over the course of 3–4 days, they may be more larvate given the accumulation of medication in the vessels.2,5 Acute attacks are treated with intravenous hydration associated with a direct arterial vasodilator and anticoagulation with heparins (preferably low-molecular-weight heparin).1 Nitroprusside is recommended as a vasodilator of choice and some authors have considered it the antidote in poisoning by ergotamine with vasoocclusive manifestations, for a short course of 48–72h.2
According to the severity, the therapeutic action can be1,2:
- 1.
Mild: oral vasodilators (non-dihydropyridine calcium channel blockers-Nifedipine, α-antagonists- Prazosin and PDE-4 inhibitors such as Sildenafil) and anticoagulation.
- 2.
Moderate to severe: intravenous vasodilators (sodium nitroprusside, prostaglandin E2 analogs such as Iloprost and intravenous Alprostadil) and anticoagulation with heparins. Antiagregation with acetylsalicylic acid is also recommended for 3–6 months. The use of glucocorticoids at a dose of 1mg/kg/day in cases refractory to nitroprusside has also been described.8 Empirically in difficult cases with high risk of gangrene, intraarterial papaverine and streptokinase has been used and there are anecdotal reports of intra-arterial balloon dilation.
The use of surgical sympathectomy in severe cases has not shown any usefulness, since sympathetic tone is not as important in physiopathogenesis as direct vasoconstriction mediated by α-adrenergic receptors.2,3 It has also been used successfully, pentoxifylline and hyperbaric oxygen.1,2 The recovery of the picture is usually complete and without recurrences, with a favorable prognosis as long as it avoids reintroducing the drug and triggering factors.3,5 The delay in the diagnosis implies a worse prognosis and more serious arterial injuries.2
ConclusionClinical ergotism is a reversible vasospastic phenomenon described in young people with no history of atherosclerosis and that mimics a primary vasculitis of medium-sized vessel, especially Buerguer's disease, Takayasu's arteritis and polyarteritis nodosa. Its sudden onset, as well as the preferential involvement symmetrically with stenosis of the arteries of the lower limbs, in patients exposed to oral ergotamine and its derivatives suggest this pathology. The essential management will be the withdrawal of the drug as well as of the associated triggers (smoking, LSD consumption) and control of comorbidities: primary hyperthyroidism, hypercoagulable states, heart disease, liver disease, kidney disease, malnutrition and hypertension.
Conflict of interestsThe authors declare that they have no conflict of interest.