To determine the presence of morphometric vertebral fractures, as well as their relationship with 25 OH vitamin D, body mass index, and age in elderly women.
Materials and methodsA cross-sectional study was conducted on 319 elderly women from the study ‘Musculoskeletal Health in the Elderly’. The morphometric determination of vertebral fractures was performed with radiography, while the levels of 25 OH vitamin D were determined by the chemiluminescent immunoassay (CLIA) method using the Liaison® 25 OH vitamin D Total Assay 25 (Ref 310600), using the Liaison® Analyser. The body mass index was obtained as recommended by the World Health Organization; weight in kilograms over height in meters squared. The age of the participants was verified by their identity card, and their income details from the national data bases (SISPRO-FOSYGA).
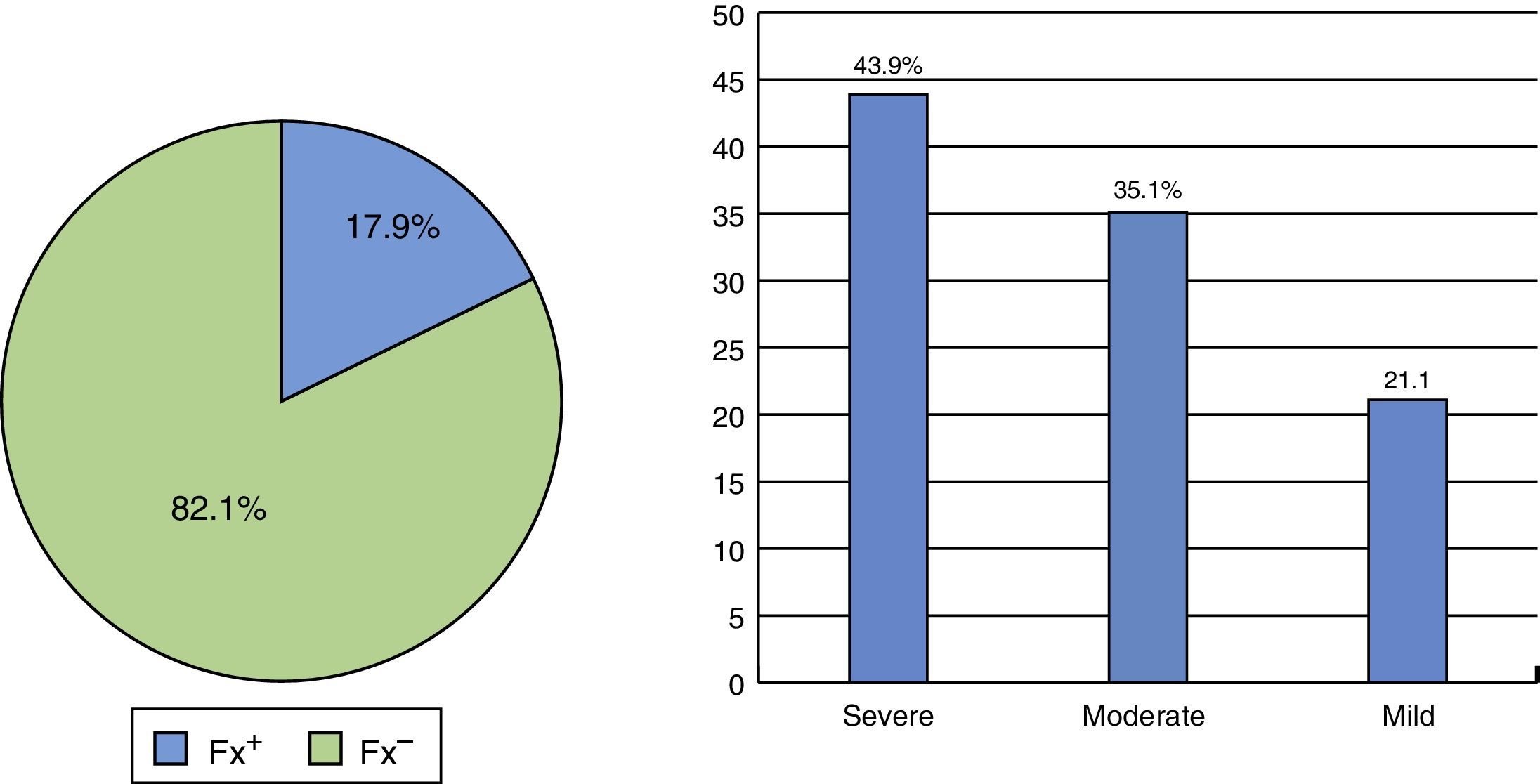
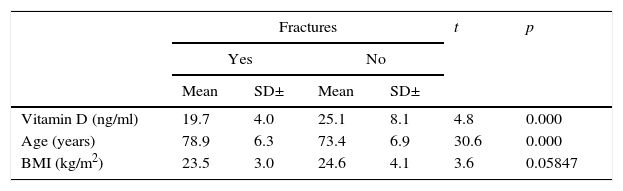
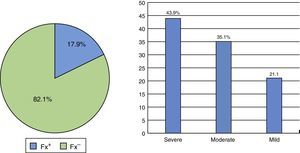
ResultsThe mean age was 74.3 years (SD±7.2). The overall prevalence of fractures was 17.9%; 54.9% of participants had values between 20 and 29ng/ml 25 OH vitamin D, and 58.9% had body mass index values less than 25kg/m2. The mean 25 OH vitamin D was lower in participants with fractures (19.7 vs. 25.1) (p<0.05). Body mass index was also lower in those with fractures (23.5 vs. 24.6) (p<0.05), but age was higher: 78.9 versus 73.4 (p<0.05). When comparing the mean levels of 25 OH vitamin D in fractured and non-fractured participants, significantly lower levels of 25 OH vitamin D were found in participants with fractures over 69 years-old, and on comparing the body mass index, the values of 25 OH vitamin D were significantly lower in each of the categories of participants with a fracture.
ConclusionA statistically significant relationship was found between morphometric vertebral fractures and: (1) low levels of 25 OH vitamin D, (2) being older and, and (3) a lower body mass index.
Determinar la presencia de fracturas vertebrales morfométricas y su relación con 25 OH vitamina D, índice de masa corporal y edad en mujeres seniles.
Materiales y métodosEstudio transversal. Se analizaron 319 mujeres seniles, provenientes del estudio «Salud osteomuscular del anciano». La determinación de fracturas vertebrales morfométricas se realizó de manera radiográfica, en tanto que los niveles de 25 OH vitamina D se midieron por inmunoanálisis por quimioluminiscencia (CLIA) Liaison® 25 OH vitamina D Total Assay Ref 310600, utilizando el equipo Diasorin Liaison® Analyzer. El índice de masa corporal se obtuvo, según las recomendaciones de la Organización Mundial de la Salud, como el peso en kilogramos sobre la talla en metros al cuadrado; la edad fue verificada con el documento de identidad y el ingreso del mismo a las bases de datos nacionales (SISPRO-FOSYGA).
ResultadosEl promedio de edad fue de 74,3 años (DE ±7,2). La prevalencia global de fracturas fue de 17,9%; así mismo, el 54,9% de las participantes tenía valores entre 20 y 29ng/ml de 25 OH vitamina D y el 58,9% tenía valores de índice de masa corporal inferior a 25kg/m2. El promedio de 25 OH vitamina D fue inferior en las participantes fracturadas (19,7 vs. 25,1) (p<0,05); el índice de masa corporal también fue menor en las fracturadas (23,5 vs. 24,6) (p>0,05), pero la edad fue mayor: 78,9 vs. 73,4 (p<0,05). Al comparar los promedios de 25 OH vitamina D en participantes fracturadas y no fracturadas, se encontraron niveles significativamente menores de 25 OH vitamina D en las participantes con fractura mayores de 69 años, y al considerar el índice de masa corporal, los valores de 25 OH vitamina D fueron significativamente inferiores en cada una de las categorías de las participantes con fractura.
ConclusiónSe encontró una relación estadísticamente significativa entre poseer fracturas vertebrales morfométricas y tener: (1) niveles bajos de 25 OH vitamina D, (2) mayor edad, y (3) menor índice de masa corporal.
Vertebral fractures (VF) are a serious consequence of osteoporosis and often tend to be underdiagnosed due to their variable clinical presentation and to the lack of an ultimate test for their definition.1 According to Pasco et al.,2 about 75% of the VF are not clinically diagnosed due to the absence of specific symptoms. One of the big concerns is that VF are predictors of future osteoporotic fractures3 and are associated with detriments in the quality of life4 and increased mortality.5
Decreased levels of vitamin D have been associated with increased incidence of fractures, mainly of the hip.6 It is known that 80% of the circulating vitamin D in blood is obtained from the exposure to the sun,7 which is why, a low sunlight exposure, whatever the reason, is a risk factor for suffering from hypovitaminosis D. Studies conducted in Europe found that 75% of people living in geriatric institutions have serum vitamin D levels lower than 10ng/ml.8 This means that this population, being deprived of the sun due to physical limitations and in the case of women, having gone through menopause, has a greater risk of suffering fractures because of the fragility of their bones.
The other 20% of the vitamin comes from nutrition. A diet rich in vitamin D (egg, milk, fish, some oils) is a protective factor. This has been demonstrated in different studies conducted in countries with a high consumption of fish such as Japan, Norway and the Netherlands, which showed lower indexes of hypovitaminosis D compared with neighboring countries.9–11 In the United States, an evaluation carried out in 20,289 individuals in the National Health And Nutrition Evaluation Survey (NHANES III) showed that, as the age advanced, the prevalence of hypovitaminosis D was more marked, and 77% of women older than 70 years had values lower than 30ng/ml.12 This result is alarming because the geriatric population has higher rates of morbidity and mortality due to osteoporosis. Annually, 30% of people older than 65 years suffer falls from their own height, and this proportion increases to 40–50% in people over 80 years of age.13
In a study conducted in Chile, in 2007, in a population of menopausal women, it was found densitometric osteoporosis (T score lower than –2.5) in 35%. 31.9% of patients had osteoporosis in the lumbar spine, 14.1% in the femoral neck and 10.7% had osteoporosis in both locations14; while another study demonstrated that 47.5% of patients (between 55 and 84 years) had hypovitaminosis D, by using a limit level of 17ng/ml.15
In Brazil, in the district of Porto,16 the mean value of 25 OH vitamin D3 was 25.6ng/ml; 26.2% of the individuals had levels >30ng/ml, 45.2% exhibited insufficiency (with values from 20 to 29ng/ml), in 23.8% of cases there was a deficit (25 OH vitamin D3 between 8 and 20ng/ml), and severe deficit (25 OH vitamin D3 <8ng/ml) in 4.8% of cases.
Meanwhile, the Lavos study demonstrated an overall prevalence of VF of 14.2% in women older than 50 years.17 However, a research carried out in Argentina demonstrated that the latitude influences the blood levels of vitamin D, finding that the vitamin D levels were higher in the North of the country than in the South,18 giving strength to the fact that, in the latitudes closer to the Equator, there is more UV radiation which, as already mentioned above, is necessary for the cutaneous absorption of vitamin D.
Vitamin D insufficiency/deficiency has a negative effect at the level of the bone and the muscle, with a greater number of falls with subsequent osteoporotic fractures. This has been demonstrated in studies which indicate that the use of vitamin D reduces the risk of falls by 22%.19
It has been considered that a dose of 700–800IU of vitamin D reduces the risk of suffering hip fractures by 26% and non-vertebral fractures by 23%.19 In postmenopausal women this is more serious,20 since they loss the protective effect of estrogen, which is consistent with the fact that approximately 33% of women between 60 and 70 years of age and 66% of women older than 80 years have osteoporosis.21,22
Traditionally, the bone mineral mass is measured only in the hip, but this may not be sufficient to identify all patients with osteoporosis, since bone loss can occur mainly in the spine.23 In 2009, the Lavos study17 revealed an overall prevalence of VF of 10.7% in women between 50 and 79 years, and in Colombia the highest index was found for women between 70 and 79 years: 22% of the participants of this age range showed radiological evidences of VF.
This is noteworthy because, even though it has not been declared by the authorities as a “public health problem”, it is believed that 47% of women over 50 years of age will suffer an osteoporotic fracture in their remaining lifetime24 and, in that order of ideas, osteoporotic vertebral fractures play a protagonist role, since 2/3 of them are usually silent.25,26
Therefore, taking into account that studies at local, regional or national level, that account for vitamin D levels as an important marker to estimate and assess the occurrence of VF have not been found, it arose the need to carry out the present study.
Materials and methodsA descriptive cross-sectional study was conducted in 319 postmenopausal women who attended the Center of Rheumatology and Orthopedics of the city of Barranquilla, during the period 2011–2014, participants in the study “Musculoskeletal Health in the Elderly”.
The ages were verified with the identity card (birthdate vs. current date), and its entry to the state database open to the public: Fosyga and Sispro.
The sample was obtained by convenience, taking into account the total of potential participants that met the selection criteria. A morphometric radiographic study for the detection of fractures was carried out to the participants when they entered in the study, and a blood sample was taken to determine vitamin D levels.
Inclusion criteria- -
Patient oriented to person, time and place (physical examination).
- -
Age ≥60 years
- -
Being able to walk independently.
- -
Approval to participate in the study by signature of the informed consent.
- -
A disease that impedes to continue participating in the research: of musculoskeletal or mental type.
- -
Known metabolic condition or history of cancer.
- -
Use of drugs that can alter the bone mass: heparins, oral anticoagulants (warfarin), immunosuppressive agents (cyclosporine and azathioprine), medroxyprogesterone acetate, luteinizing hormone-releasing hormone agonists, thyroid hormone replacement therapy, vitamin A and synthetic retinoids and diuretics and antiresorptive agents.
- -
Use of drugs that can alter the vitamin D levels: anticonvulsants (phenobarbital, phenytoin, primidone and valproic acid), cholestyramine and colestipol, rifampicin, and corticosteroids.
The studied variables were:
- -
Age: years completed at the time of the study, verified with the date of birth of the identity document.
- -
Body mass index (BMI): weight in kg taken using a calibrated electronic scale, divided by height in m2, measured with a calibrated measuring rod.
- -
Presence of VF: the assessment was carried out by morphometric radiographic study, analyzed by a single radiologist, using Genant's method for the classification of the fractures.8
- -
Values of 25 OH vitamin D: from a blood sample, the levels of vitamin D were measured: 25 OH vitamin D total metabolite, by the chemiluminescent immunoassay (CLIA) method Liaison 25 OH vitamin D Total Assay Ref 310600, using the Diasorin Liaison® Analyzer. Cut-off points (deficient/insufficient/adequate) for vitamin D were not used, but rather were taken the values at ratio and interval levels in decennial groups.
The variables were analyzed at univariate level, using percentages and averages in the quantitative variables: age, BMI and vitamin D. Subsequently, it was determined the existence of statistically significant differences (p<0.05) regarding the prevalences of fractures in relation with the categories of age, BMI and vitamin D, and the means of these 3 variables according to having or not VF (t-test and p-value). Finally, the means of vitamin D values were compared by age and BMI, according to whether having or not VF (t-test and p-value).
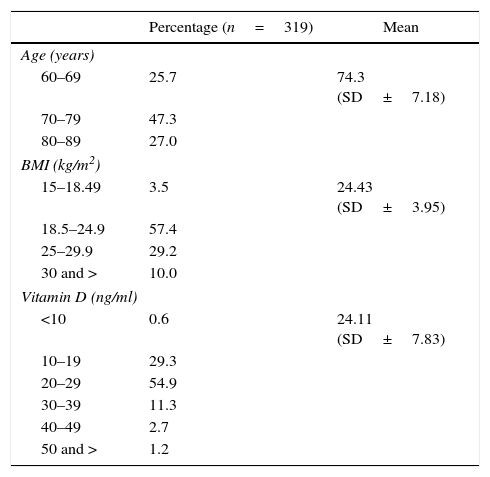
ResultsThe mean age was 74.3 years (SD±7.18); the largest proportion of participants was between 70 and 79 years old (47.3%). Around 39% had a BMI>24.9kg/m2, i.e., they were overweight or obese.
With respect to vitamin D, 54.9% of the participants had values between 20 and 29ng/ml, with an average of 24.11 (SD±7.83) (Table 1), and the overall prevalence of fractures in the studied group was 17.9% (43.9% were severe, 35.1% moderate and 21% mild) (Fig. 1).
Frequency distribution of the participants by age and body mass index values.
| Percentage (n=319) | Mean | |
|---|---|---|
| Age (years) | ||
| 60–69 | 25.7 | 74.3 (SD±7.18) |
| 70–79 | 47.3 | |
| 80–89 | 27.0 | |
| BMI (kg/m2) | ||
| 15–18.49 | 3.5 | 24.43 (SD±3.95) |
| 18.5–24.9 | 57.4 | |
| 25–29.9 | 29.2 | |
| 30 and > | 10.0 | |
| Vitamin D (ng/ml) | ||
| <10 | 0.6 | 24.11 (SD±7.83) |
| 10–19 | 29.3 | |
| 20–29 | 54.9 | |
| 30–39 | 11.3 | |
| 40–49 | 2.7 | |
| 50 and > | 1.2 | |
Source: own elaboration.
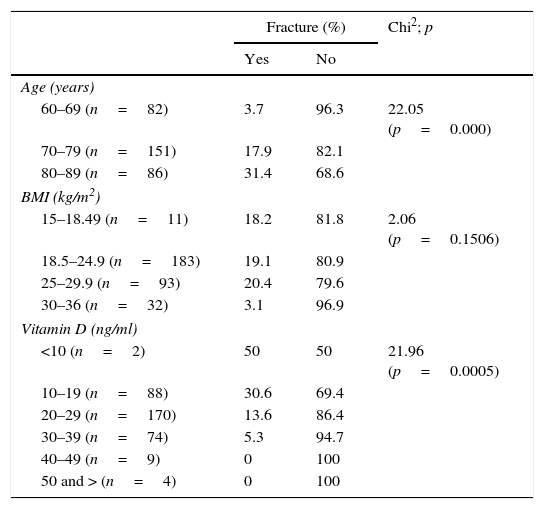
The prevalence of fractures was higher as age increased, going from 3.7% in the group of 60–69 years, to 17.9% in the one of 70–79, and to 31.4% in the group of 80–89; when comparing the group of participants with fractures with those without fractures, the differences in the proportions were statistically significant (p<0.05) (Table 2).
Prevalence of fractures according to age, BMI and vitamin D values.
| Fracture (%) | Chi2; p | ||
|---|---|---|---|
| Yes | No | ||
| Age (years) | |||
| 60–69 (n=82) | 3.7 | 96.3 | 22.05 (p=0.000) |
| 70–79 (n=151) | 17.9 | 82.1 | |
| 80–89 (n=86) | 31.4 | 68.6 | |
| BMI (kg/m2) | |||
| 15–18.49 (n=11) | 18.2 | 81.8 | 2.06 (p=0.1506) |
| 18.5–24.9 (n=183) | 19.1 | 80.9 | |
| 25–29.9 (n=93) | 20.4 | 79.6 | |
| 30–36 (n=32) | 3.1 | 96.9 | |
| Vitamin D (ng/ml) | |||
| <10 (n=2) | 50 | 50 | 21.96 (p=0.0005) |
| 10–19 (n=88) | 30.6 | 69.4 | |
| 20–29 (n=170) | 13.6 | 86.4 | |
| 30–39 (n=74) | 5.3 | 94.7 | |
| 40–49 (n=9) | 0 | 100 | |
| 50 and > (n=4) | 0 | 100 | |
Source: own elaboration.
As for the BMI values, the prevalences of VF were similar: 18.1% in women with BMI between 15 and 18.49kg/m2, 19.1% in the group between 18.5 and 24.9kg/m2, and 20.4% in the overweight participants, while in women with obesity (BMI>29.9kg/m2), the prevalence of VF was much lower: 3.1%. When the 4 categories of BMI were compared according to whether or not having VF, the differences were not statistically significant (p>0.05).
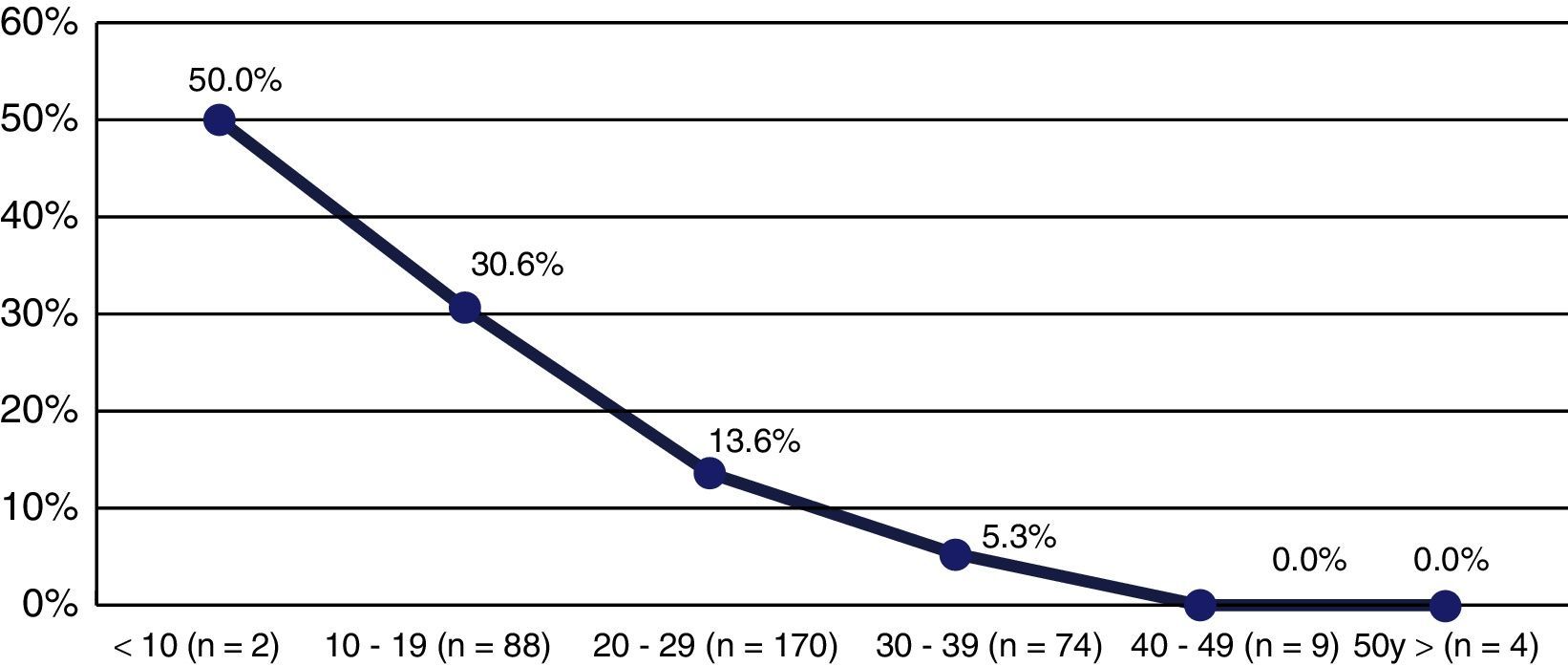
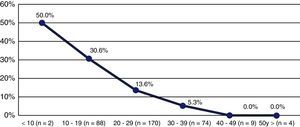
When the participants were grouped according to the vitamin D values (in decennial groups), in the category of <10ng/ml the prevalence of VF was 50%, and in the group of 10–19ng/ml about 3 out of 10 participants had VF, while in the other groups the percentage of participants with VF was decreasing, until reaching 0% in women with vitamin D >39ng/ml (Fig. 2). Likewise, when comparing the categories of vitamin D, according to the fact of having or not fractures, the differences resulted statistically significant (p>0.05) (Table 2).
When the mean vitamin D levels were compared, according to the fact of having or not VF, statistically significant differences were found (p<0.05), with a lower mean in the participants with fracture: 19.7ng/ml, versus in those without fracture: 25.1ng/ml (Table 3).
Likewise, the mean age was significantly higher in the participants with fracture than in those without fracture (p<0.05): 78.9 versus 73.4 years (Table 3), and the mean BMI was similar between the participants with and without fracture: 23.5kg/m2 and 24.6kg/m2, respectively (p>0.05) (Table 3).
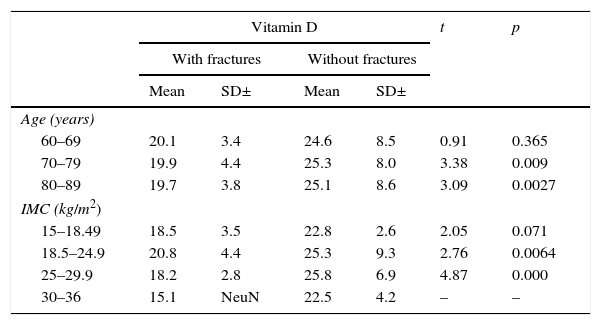
When comparing the mean vitamin D levels in fractured and non-fractured participants, according to each of the age groups, it was found that in women between 60 and 69 years old the differences were not significant (p>0.05), but they were significant in women between 70 and 79 years and between 80 and 89 years of age (Table 4).
Mean vitamin D levels by age and BMI, according to the fact of having or not vertebral fractures.
| Vitamin D | t | p | ||||
|---|---|---|---|---|---|---|
| With fractures | Without fractures | |||||
| Mean | SD± | Mean | SD± | |||
| Age (years) | ||||||
| 60–69 | 20.1 | 3.4 | 24.6 | 8.5 | 0.91 | 0.365 |
| 70–79 | 19.9 | 4.4 | 25.3 | 8.0 | 3.38 | 0.009 |
| 80–89 | 19.7 | 3.8 | 25.1 | 8.6 | 3.09 | 0.0027 |
| IMC (kg/m2) | ||||||
| 15–18.49 | 18.5 | 3.5 | 22.8 | 2.6 | 2.05 | 0.071 |
| 18.5–24.9 | 20.8 | 4.4 | 25.3 | 9.3 | 2.76 | 0.0064 |
| 25–29.9 | 18.2 | 2.8 | 25.8 | 6.9 | 4.87 | 0.000 |
| 30–36 | 15.1 | NeuN | 22.5 | 4.2 | – | – |
Source: own elaboration.
As for the BMI, the mean vitamin D level was significantly lower (p<0.05) in the participants with fracture versus the non-fractured, in the groups of 18.5–24.9kg/m2 and of 25–29.9kg/m2 (Table 4).
DiscussionOsteoporosis is a metabolic disease that affects millions of people worldwide, and is the main risk factor for the development of fractures.27 In Colombia, the average prevalence of osteoporosis is 57% in people older than 40 years,28 while in the Colombian Caribbean region, it has been documented a prevalence of 32.6% after 50 years of age.29
Among the multiple secondary causes of osteoporosis, is found the deficiency of vitamin D, since it is involved in bone metabolism and can contribute to the pathogenesis of low bone mass and predispose to fragility fractures; and high rates of insufficiency or deficiency of this component have been documented in Colombia: 71.7% in Medellin30 and 69.5% in Bogota.31 Likewise, it has been found globally that 64% of postmenopausal women have hypovitaminosis D.32,33
In the present study, rather than inquire the prevalence of hypovitaminosis, it was found that low vitamin D levels are associated with an increased likelihood of developing VF, which are a serious result and in many cases irreversible of osteoporosis in older adults and, once they occur, the risk of recurrence usually increases,34 demonstrating the urgency in identification and intervention for this segment of the population.35 Therefore, it would be necessary to carry out an annual follow up to the studied population, taking into account the time of occurrence of the fracture.
The results found are similar to what was documented by Molina et al.,30 in whose study, after comparing patients with deficient and insufficient levels, it was found that patients with deficient vitamin D levels constituted a risk factor for the presence of VF (RR: 1.02; 95% CI: 0.96–1.06); however, unlike the aforementioned study, in the present one, the results were statistically significant (p<0.05).
On the other hand, there are some limitations in the present study, since the exact time of occurrence of the observed VF is not known. Nevertheless, because of their asymptomatic appearance, in many cases it is difficult to determine the time of occurrence of these fractures, especially in mild cases. Some of them could be recent, and in this case, the relationship with the vitamin D values would need to be adjusted as a function of time. However, is a factor in favor that other studies have demonstrated that the effects of the prevalent fractures are independent of the bone mass (directly related with the vitamin D values).36,37
In the same way, it is necessary to carry out an assessment of BMI, taking into account the parameters of the World Health Organization for older adults, because, as it is known, the depletion of muscle mass in them can induce false positives or false negatives, and this variable could be correlated with the presence of VF in the study population, as a function of age and interacting with the vitamin D levels.
ConclusionsIt was found a significant relationship between low vitamin D levels and the presence of vertebral fractures. This relationship may be influenced by age, but not by the BMI. However, it is required to carry out longitudinal studies to confirm this association. Despite this, this is the preliminary step that sets an important precedent nationwide.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
FundingMetropolitan University of Barranquilla; Center of Rheumatology and Orthopedics.
Conflict of interestThe authors expressly state that there is no conflict of interest.
Please cite this article as: Jaller Raad JJ, Jaller Char JJ, Vargas Moranth R, Suárez Landazábal O, Jaller Char A, Jaller JA, et al. Fracturas vertebrales morfométricas y su relación con 25 OH vitamina D, índice de masa corporal y edad en mujeres seniles. Rev Colomb Reumatol. 2016;23:229–235.