Spondyloarthritis is a group of chronic inflammatory diseases that mainly affect the axial skeleton, and also the peripheral joints. In bone metabolism studies on these patients, it has been observed that there are lower levels of vitamin D in patients with spondyloarthritis.
ObjectiveTo estimate the prevalence of vitamin D deficiency/insufficiency, as well as calcium/phosphate metabolism and their implications in a cohort of patients with spondyloarthritis.
MethodologyObservational, descriptive, and cross-sectional study. A retrospective review of the databases was carried out on patients with spondyloarthritis who were treated in the outpatient clinics of the Rheumatology Department of the General University Hospital of Ciudad Real between June 2018 and June 2019. Variables are described using frequency and central tendency/dispersion measurements as appropriate.
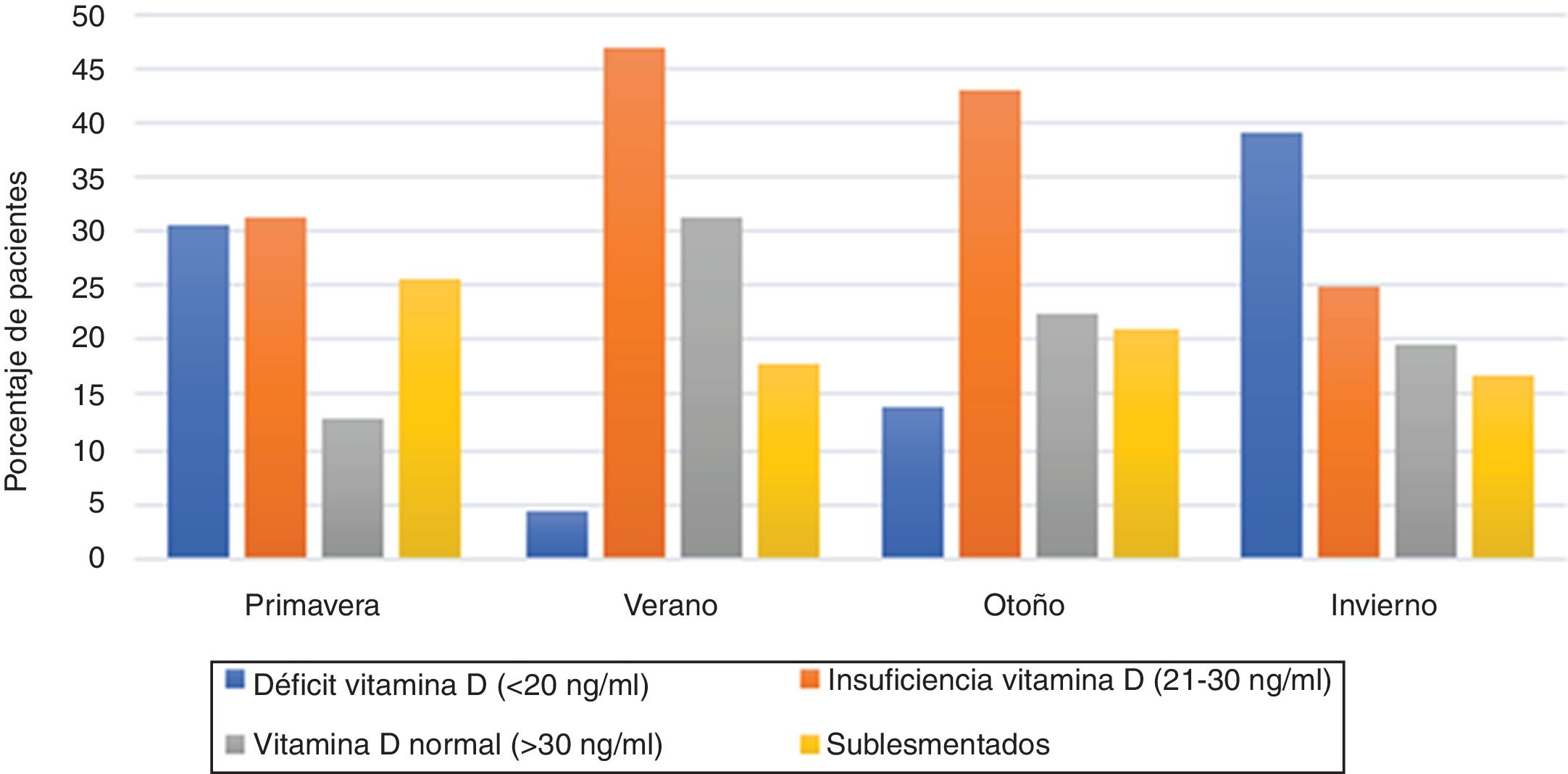
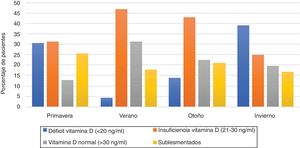
ResultsThe study included 115 patients, of whom 64 were men and 51 women, with a mean age of 45.97 years (±13.41 SD). They included 59 patients with ankylosing spondylitis, 24 with psoriatic arthropathy, 9 arthritis associated with inflammatory bowel disease, 12 non-radiographic axial spondyloarthritis, and 11 reactive arthritis. Vitamin D levels were 23.81 ng/mL (±10.5 SD), with 77.4% of patients with vitamin D deficiency/insufficiency levels. Grouped by the spondyloarthritis subtype, and according to vitamin D deficiency/insufficiency, 45 patients had ankylosing spondylitis, 19 psoriatic arthropathy, 9 arthritis associated with inflammatory bowel disease, 7 non-radiographic axial spondyloarthritis, and 9 reactive arthritis. Furthermore, vitamin D deficiency (<20 ng/mL) mainly occurred in the spring and winter seasons, with 31 and 26 patients, respectively.
ConclusionsAn optimization of vitamin D levels may lead to an improvement in the clinical situation of the patients, as measured by both BASDAI and DAPSA, as well as by PCR and ESR. Therefore, vitamin D monitoring and supplementation is recommended in patients with vitamin D deficiency.
Las espondiloartritis son un grupo de enfermedades inflamatorias crónicas con afectación principalmente del esqueleto axial y también de articulaciones periféricas. En cuanto al metabolismo óseo de estos pacientes, se ha observado en algunos estudios que existen niveles más bajos de vitamina D en pacientes con espondiloartritis.
ObjetivoEstimar la prevalencia de déficit/insuficiencia de vitamina D, el metabolismo fosfocálcico y sus implicaciones en una cohorte de pacientes con espondiloartritis.
MetodologíaEstudio observacional, descriptivo y transversal. Se llevó a cabo una revisión retrospectiva de la base de datos de pacientes con espondiloartritis que fueron atendidos en las consultas externas del Servicio de Reumatología del Hospital General Universitario de Ciudad Real entre junio del 2018 y junio del 2019. Las variables se describieron usando medidas de frecuencia o medidas de tendencia central/dispersión según correspondiera.
ResultadosSe analizaron 115 pacientes, de los cuales 64 fueron hombres y 51 mujeres, con una edad media de 45,97 años (±13,41 DE). Del total de los pacientes, 59 presentaron espondilitis anquilosante, 24 artropatía psoriásica, 9 artritis asociada a enfermedad inflamatoria intestinal, 12 espondiloartritis axial no radiográfica y 11 artritis reactiva. Los niveles de vitamina D fueron de 23,81 ng/mL (±10,5 DE), con un 77,4% de los pacientes con cifras de déficit/insuficiencia de vitamina D. Agrupados por el subtipo de espondiloartritis y según las cifras de déficit/insuficiencia de vitamina D, 45 pacientes tenían espondilitis anquilosante, 19 artropatía psoriásica, 9 artritis asociada a enfermedad inflamatoria intestinal, 7 espondiloartritis axiales no radiográficas y 9 artritis reactivas. Además, el déficit de vitamina D (<20 ng/mL) se presentaba las más de las veces en las estaciones de primavera e invierno, con 31 y 26 pacientes respectivamente.
ConclusionesUna optimización de los niveles de vitamina D puede implicar una mejoría en la situación clínica del paciente, medida tanto por BASDAI y DAPSA como por PCR y VSG. En consecuencia, se recomienda la monitorización y suplementación de vitamina D en pacientes con hipovitaminosis D.
The term spondyloarthritis (SpA) describes a group of chronic rheumatic inflammatory diseases that mainly affect the axial skeleton, although they can also affect the peripheral joints. They share other characteristics such as genetic predisposition and radiographic manifestations. This group of diseases includes ankylosing spondylitis (AS), psoriatic arthritis (PsA), reactive arthritis (ReA), spondyloarthropathy associated with inflammatory bowel disease (SpA-IBD), undifferentiated spondyloarthritis (UnSpA) and juvenile idiopathic arthritis (JIA), among others.1 All these pathologies share clinical characteristics such as inflammatory axial pain, enthesitis, dactylitis, and extra-articular manifestations such as uveitis, psoriasis, and inflammatory bowel disease. In addition, they share some pathogenic mechanisms, familial aggregation and a strong association with the histocompatibility complex B 27 (HLA-B27).2 It should be noted that, mainly in patients with axial spondyloarthropathy, the inflammation of the spine and the sacroiliac joints leads to a structural damage in the area, as a result of the bone neoformation to repair such damage (development of ankylosis, bony bridges, enthesophytes, among others). These structural modifications affect the general condition of the patients, limiting their mobility and in consequence, altering their quality of life.3 It is estimated that the global prevalence of spondyloarthritis ranges between 0.23 and 1.8%. As for ankylosing spondylitis, which is the predominant and most important disease in the group of axial spondyloarthritis, the estimated prevalence in Spain is 0.26% (95% CI: 0.14−0.49), while the estimated prevalence of psoriatic arthritis in the population older than 20 years in Spain is 0.58% (95% CI: 0.38−0.87), according to data from the EPI-SER2016 study.4,5
Vitamin D plays an important role in the regulation of the immune system. Immune cells not only metabolize calcifediol into calcitriol, but they also have vitamin D receptors (VDR), modulating the differentiation, activation and proliferation of these immune cells. The binding of vitamin D to VDR produces pleiotropic effects, by regulating the transcription of about 200 genes involved in cell growth and maturation processes; in the inhibition of the renin-angiotensin axis and angiogenesis; in insulin secretion and sensitivity thereto; in the ability to control genes related to the innate and acquired immune response, and in the regulation of apoptosis. These immunomodulatory effects could explain the epidemiological associations found between vitamin D deficiency and the appearance of certain neoplasms, diabetes, cardiovascular diseases and autoimmune rheumatic diseases, among others, and their greater severity. Although the beneficial effects of vitamin D have been proven in animal models, human intervention studies with vitamin D supplements have not been conclusive.6,7 Current epidemiological evidence shows a significant association between vitamin D deficiency and a higher incidence of activity in autoimmune diseases such as systemic lupus erythematosus, type 1 diabetes mellitus, multiple sclerosis, and rheumatoid arthritis.8–10 Recent research suggest that low levels of vitamin D are associated with an increase in disease activity and severity in patients with inflammatory arthritis. It has been observed that the plasma levels of 25(OH)-D3 can decrease in patients with spondyloarthritis, which could negatively affect the disease activity, the functional status and the quality of life of the patient with spondyloarthritis.
The objective of our study is to estimate the prevalence of vitamin D deficiency/insufficiency, the phosphocalcic metabolism and its implications in a cohort of patients with spondyloarthritis.
MethodologyStudy designObservational, descriptive and cross-sectional study. A retrospective review of a database of patients with spondyloarthritis was made, with a review of their clinical records and of their regular periodic follow-up.
PatientsPatients with spondyloarthritis diagnosed according to ASAS criteria by expert rheumatologists, who were treated in the outpatient clinics of the Rheumatology Service of the General University Hospital of Ciudad Real (referral center of the province of Ciudad Real, of the autonomous community of Castilla La-Mancha), between June 2018 and June 2019.
VariablesThe variables collected are the following: demographic data (sex and age); subtype of spondyloarthritis; presence of the histocompatibility complex HLA-B27; clinical manifestations; imaging findings to assess radiographic sacroiliitis (by conventional sacroiliac radiography), syndesmophytes (by lateral radiography of the dorsolumbar spine) and bone edema (by magnetic resonance imaging of the sacroiliac joints and according to ASAS-OMERACT criteria); and treatments used: symptomatic (used at some point in their disease) and base/maintenance (conventional/biological disease-modifying antirheumatic drugs, used at the time of data collection), among others. Furthermore, as a variable of interest for our study, the serum levels of 25(OH) vitamin D were collected and divided into 4 groups: deficiency (0−20 ng/mL); insufficiency (21−30 ng/mL); desirable/optimal (31−80 ng/mL) and risk of toxicity (110−150 ng/mL). Along with the 25(OH) vitamin D, the mean serum levels of parathyroid hormone, calcium and phosphorus are determined. Besides, we have selected as variables of disease activity the BASDAI Index (Bath Ankylosing Spondylitis Diseases Activity Index) for patients with axial spondyloarthritis and the DAPSA Index (Disease Activity for Psoriatic Arthritis) for patients with psoriatic arthritis. In addition, it has been studied whether there is an elevation of acute phase reactants by the ESR and CRP parameters. Finally, 2 determinations of vitamin D are registered together with the determinations of disease activity (BASDAI, DAPSA, ESR and CRP), separated by at least 4 months at different times of the year.
Statistical analysisNumerical variables with a normal distribution are expressed as mean and standard deviation. Among other variables described, measures of frequency and measures of central tendency/dispersion are used, as appropriate. Analysis of the main demographic and clinical data and of the stratified variables for each type of disease was made. All analyzes have been performed with a 95% confidence level using SPSS 21.
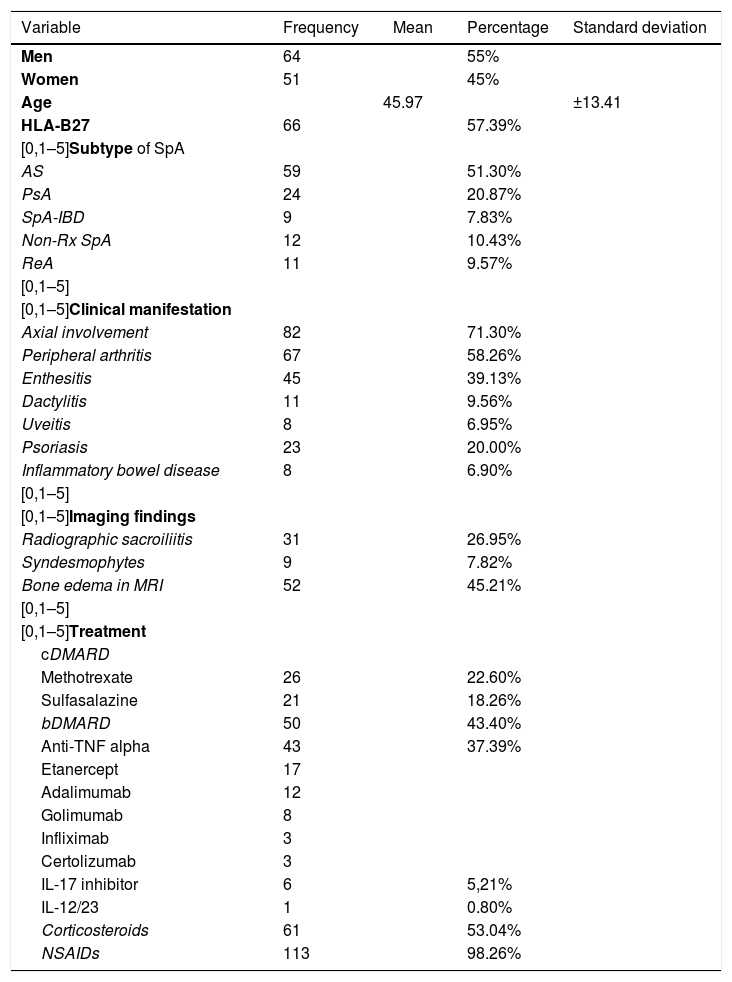
ResultsThe study included 115 patients with a diagnosis of spondyloarthritis, of whom 64 were men and 51 women, with a mean age of 45.97 years (±13.41 SD). As for the subtypes of spondyloarthritis, 51.3% of patients belong to the group of ankylosing spondylitis, 20.87% to the group of psoriatic arthropathy, 7.83% to that of arthritis associated with inflammatory bowel disease, 10.43% to non-radiographic axial spondyloarthritis and 9.57% to reactive arthritis. Regarding the treatment, and more specifically, the symptomatic treatment, 98.26% had received NSAIDs at some point of their disease and up to 53.04%, that is, 61 of the studied patients had ever received corticosteroids. On the other hand, and with reference to the basic treatment, 40.86% were receiving conventional disease-modifying antirheumatic drugs, while 37.39% were treated with biological disease-modifying antirheumatic drugs. In addition, positivity to the HLA-B27 histocompatibility complex, clinical manifestations, and imaging findings, among others, were studied (Table 1).
Demographic and clinical characteristics of the patients with spondyloarthritis in our study.
| Variable | Frequency | Mean | Percentage | Standard deviation |
|---|---|---|---|---|
| Men | 64 | 55% | ||
| Women | 51 | 45% | ||
| Age | 45.97 | ±13.41 | ||
| HLA-B27 | 66 | 57.39% | ||
| [0,1–5]Subtype of SpA | ||||
| AS | 59 | 51.30% | ||
| PsA | 24 | 20.87% | ||
| SpA-IBD | 9 | 7.83% | ||
| Non-Rx SpA | 12 | 10.43% | ||
| ReA | 11 | 9.57% | ||
| [0,1–5] | ||||
| [0,1–5]Clinical manifestation | ||||
| Axial involvement | 82 | 71.30% | ||
| Peripheral arthritis | 67 | 58.26% | ||
| Enthesitis | 45 | 39.13% | ||
| Dactylitis | 11 | 9.56% | ||
| Uveitis | 8 | 6.95% | ||
| Psoriasis | 23 | 20.00% | ||
| Inflammatory bowel disease | 8 | 6.90% | ||
| [0,1–5] | ||||
| [0,1–5]Imaging findings | ||||
| Radiographic sacroiliitis | 31 | 26.95% | ||
| Syndesmophytes | 9 | 7.82% | ||
| Bone edema in MRI | 52 | 45.21% | ||
| [0,1–5] | ||||
| [0,1–5]Treatment | ||||
| cDMARD | ||||
| Methotrexate | 26 | 22.60% | ||
| Sulfasalazine | 21 | 18.26% | ||
| bDMARD | 50 | 43.40% | ||
| Anti-TNF alpha | 43 | 37.39% | ||
| Etanercept | 17 | |||
| Adalimumab | 12 | |||
| Golimumab | 8 | |||
| Infliximab | 3 | |||
| Certolizumab | 3 | |||
| IL-17 inhibitor | 6 | 5,21% | ||
| IL-12/23 | 1 | 0.80% | ||
| Corticosteroids | 61 | 53.04% | ||
| NSAIDs | 113 | 98.26% | ||
NSAIDs: non-steroidal anti-inflammatory drugs; PsA: psoriatic arthritis; ReA: reactive arthritis; AS: ankylosing spondylitis; SpA: spondyloarthritis; SpA-IBD: spondyloarthropathy associated with inflammatory bowel disease; non-Rx SpA; non-radiographic axial spondyloarthritis; bDMARD: biologic disease-modifying anti-rheumatic drug; cDMARD: conventional disease-modifying anti-rheumatic drug; MRI: magnetic resonance imaging.
Globally, vitamin D levels are 23.81 ng/mL (±10.5 SD), with 37.4% and 40% of the patients with values of deficiency and insufficiency of vitamin D, respectively (77.4% of the patients with low vitamin D levels). Consequently, figures and levels of pharathyroid hormone were obtained, with a mean of 56.68 pg/mL, and the levels of calcium and phosphorus with 9.41 mg/dl and 3.33 mg/dl on average, respectively. Grouped by the subtypes of spondyloarthritis, the deficiency/insufficiency of vitamin D was distributed as follows: 45 patients with ankylosing spondylitis, 19 with psoriatic arthropathy, 9 with arthritis associated with inflammatory bowel disease, 7 with non-radiographic axial spondyloarthritis and 9 with reactive arthritis. Among the selected variables of disease activity, the mean BASDAI is 4.57 (±2.35 SD), with 65.93% of our patients presenting disease activity, while the mean DAPSA is 12.61 (±6.76 SD), with 70.88% of the patients with psoriatic arthritis with disease activity. As for the elevation of acute phase reactants, the mean CRP is 17.04 mg/l (±35.97 SD) and the ESR 19.12 mm/h (±20.79 SD).
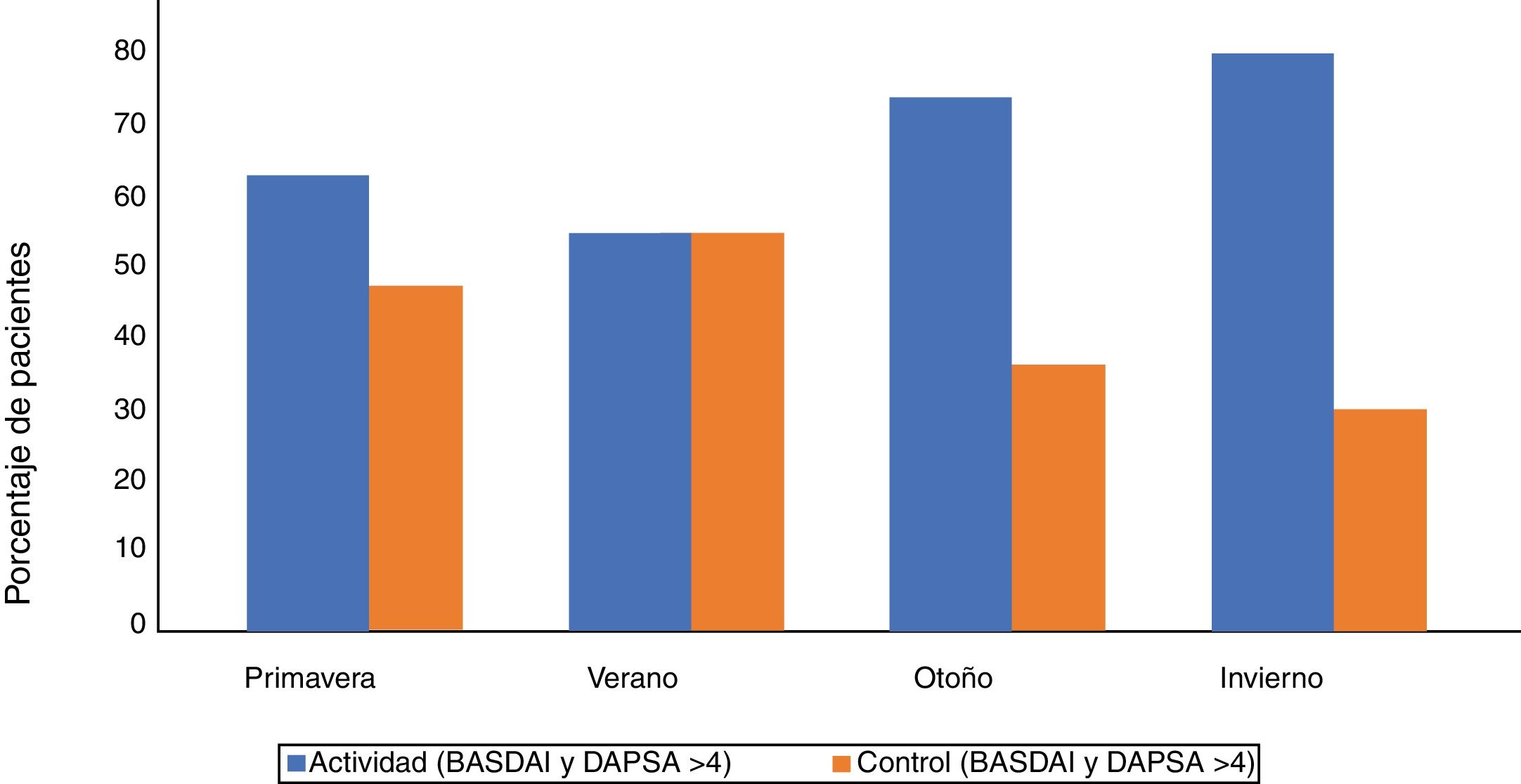
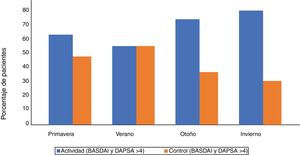
We also analyzed the time when the vitamin D sample was obtained and if the patient was previously supplemented. It has been observed that vitamin D deficiency (<20 ng/mL) occurred in most occasions in the spring and winter seasons, with 31 and 26 patients respectively. It has also been seen that vitamin D insufficiency (21−30 ng/mL) occurred mostly in spring and autumn, with 32 and 31 patients respectively, closely followed by the summer with 21 patients. Of all the patients analyzed, 26 of those whose sample was obtained in the spring were receiving vitamin D supplements, and of them: 6 continued presenting values of deficiency, 12 of insufficiency and only 8 had normal values (of the latter, 6 have a control of the disease activity by BASDAI or DAPSA). Of the patients who were supplemented and collected in the summer (8 in total), none had values of deficiency, 2 had values of insufficiency and 6 had normal levels (of the latter, 3 had a control of the disease activity by BASDAI or DAPSA). Of those in whom the sample was obtained in the fall and were supplemented (14 in total), 2 have vitamin D deficiency, 8 insufficiency and 4 normal levels of vitamin D (of the latter, 2 have a control of the disease activity by BASDAI or DAPSA). And of the patients supplemented with vitamin D with samples obtained in the winter (12 patients in total), 6 continue presenting vitamin D deficiency, 2 present insufficiency and 4 have normalized vitamin D levels (of the latter, 3 present a control of the disease activity by BASDAI or DAPSA) (Figs. 1 and 2).
In recent years, it has been studied the possible relationship between vitamin D and the pathogenic mechanism of certain inflammatory diseases such as systemic lupus erythematosus or rheumatoid arthritis. Vitamin D deficiency/insufficiency, almost endemic in the general Spanish population (contrary to what was initially believed in a Mediterranean country), seems to be more prevalent in patients with spondyloarthritis, as observed in the study conducted by Erten et al. in 2013, in which 161 patients with axial spondyloarthritis (113 with undifferentiated spondyloarthritis and 48 with ankylosing spondylitis) were selected and compared with controls. The researchers found significant differences between the mean level of 25 (OH) vitamin D and a higher proportion of deficiency in patients with spondyloarthritis, with no gender influence, with 80 and 78% of vitamin D deficiency in ankylosing spondylitis and in undifferentiated spondyloarthritis, respectively.11 In our study of 115 patients, it is observed that up to 77.4% of the patients diagnosed with spondyloarthritis have a deficiency/insufficiency of vitamin D, either ankylosing spondylitis, psoriatic arthritis, arthritis associated with inflammatory bowel disease, non-radiographic axial spondyloarthritis or reactive arthritis. All our patients are Caucasian and they come from the same geographic location, which is Castilla La-Mancha, a region of Spain located far from the sea level with a mean altitude of 628 masl.
In a review conducted by Pokhai et al. in 2014 it was observed that only 4 studies showed a significant negative correlation between vitamin D levels and BASDAI, mainly, and also with the acute phase reactants ESR and CRP, in patients with ankylosing spondylitis. The authors concluded that the patients diagnosed with ankylosing spondylitis appeared to have lower levels of vitamin D compared to healthy controls, but that further studies were needed to determine if there is a causal relationship between vitamin D deficiency and ankylosing spondylitis.12 In another study carried out by Kolahi et al. in 2019, vitamin D levels were compared in 86 patients with spondyloarthritis versus a control group of 117 healthy patients, and the results obtained showed that vitamin D levels in patients with spondyloarthritis were significantly lower than in healthy controls (P < .001), but no significant differences were observed in the activity of patients with spondyloarthritis in the different serum levels of vitamin D or significant correlations between vitamin D levels with the clinical findings, as well as with BASDAI and BASFI (P > .05).13 The researchers found that vitamin D deficiency occurred in 51.2% of the total of patients with spondyloarthritis, and therefore, they carried out an association analysis, and observed that vitamin D deficiency was independently associated with the presence of radiographic sacroiliitis, with an OR of 2.1 (95% CI: 1.3–3.3), and with a vitamin D measured in winter and spring with an OR of 1.88 (95% CI: 1.2–2.9).14 For this reason, in our study we wanted to discern when, that is, at what time of the year the vitamin D sample was obtained, so we have recorded at least 2 vitamin D determinations in all patients, separated by at least 4 months, at different times of the year. It has been observed that vitamin D deficiency and insufficiency in patients with spondyloarthritis were found mostly in the spring, autumn and especially in winter seasons, and they also presented higher disease activity measured by BASDAI and DAPSA. This is probably due to the fact that vitamin D depends mostly on the sun exposure and that in the months of winter, autumn and spring there is less exposure to sunlight and fewer hours of sunshine, among others. In addition to the parameters used to measure the disease activity by BASDAI and DAPSA, we wanted to use others that are more objective such as CRP and ESR, and it has been observed that patients with higher activity had more elevated levels of these acute phase reactants.
There are also other studies such as that conducted in 2018 by Guta et al., in which a preliminary cross-sectional study of patients with axial spondyloarthritis and peripheral spondyloarthritis was published, wherein it is stated that there is no statistically significant negative correlation between the level of vitamin D and the disease activity of patients with axial spondyloarthritis and peripheral spondyloarthritis, in terms of clinical symptoms (arthritis, enthesitis, dactylitis), inflammatory markers (ESR, CRP) and disease activity scores (BASDAI, ASDAS), and there is no alteration of these results after supplementation with vitamin D and the seasonal change. Along the same line, there is a study published in 2020 by Deng et al.,15 who found no association between vitamin D and pain and disease activity in patients with a recent diagnosis of axial spondyloarthritis, despite the prevalence of hypovitaminosis D, both in cases and in healthy controls.16
In our study, it seems to be a marked prevalence among patients with spondyloarthritis to present levels of 25-OH vitamin D below 30 ng/mL (89 patients), being of 37.4% for patients with deficiency and of 40% for patients with insufficiency and with a mean vitamin D of 23.81 ng/mL. As an addition to our study, we have observed that depending on the season of the year in which the vitamin D sample was obtained, patients with spondyloarthritis who present a vitamin D deficiency (<20 ng/mL) are in their majority in the seasons of winter and spring, and they also have higher disease activity measured by BASDAI and DAPSA.
The final conclusion reached is that an optimization of vitamin D levels may imply an improvement in the clinical situation of the patient, measured both by BASDAI and DAPSA and by CRP and ESR. Therefore, vitamin D supplementation and monitoring is recommended in patients with hypovitaminosis D, as well as to perform bone densitometry depending of the risk of low bone mineral density or fracture, in case it would be necessary the use of antiresorptive or bone-forming drugs.
Conflict of interestThe authors declare that they do not have any conflict of interest.
Please cite this article as: Castro Corredor D, Ramírez Huaranga MA, Mínguez Sánchez MD, Luque Zafra M, Cuadra Díaz JL. El déficit de vitamina D en pacientes con espondiloartritis en un hospital de Castilla-La Mancha. Rev Colomb Reumatol. 2021;28:171–177.