Models in health care have been static for a long time, but recently there has been a change in recognizing that technology in the area of information and communication could lead to a change in improving health services. Telemedicine has been increasing and its use now extends to the entire process of health care. It is beginning to be implemented in the rheumatology area, in Colombia. The characteristics of a tele-rheumatology service are described, as well as a more detailed observation of a cohort of patients with rheumatoid arthritis (RA), in order to identify strengths and improvements.
MethodsA descriptive observational cross-sectional study was conducted on the total population of patients who were treated by the tele-rheumatology service in the synchronous modality for a period of 30 months. As regards the follow-up of patients with RA, all patients who were treated exclusively by means of synchronous telemedicine for a minimum period of 6 months with at least three follow-ups, in which it was possible to calculate the clinimetry by DAS28 with the use of C reactive protein (CRP) were included. Measures of frequency, central tendency and dispersion according to the type of variable will be used for the descriptive analysis.
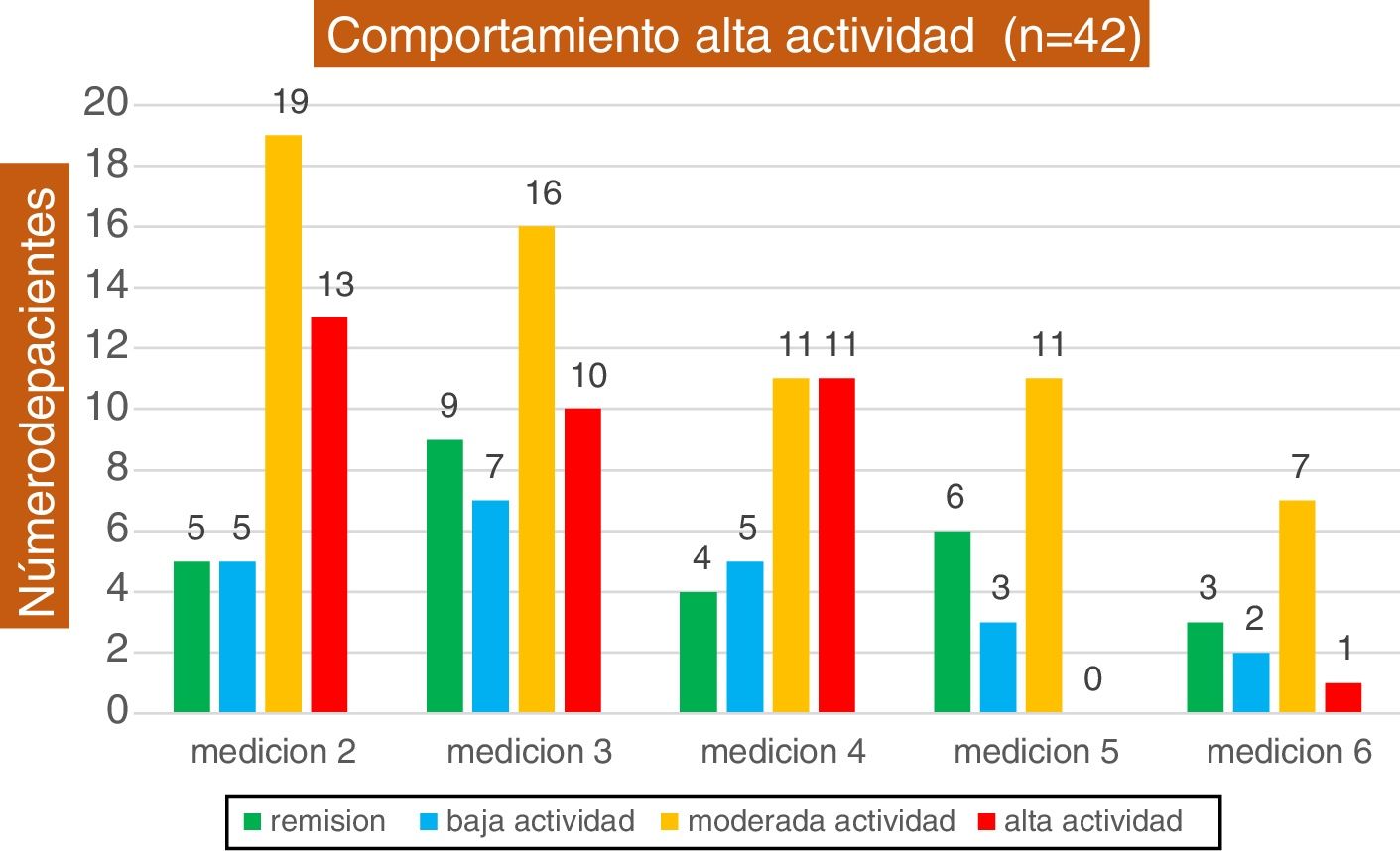
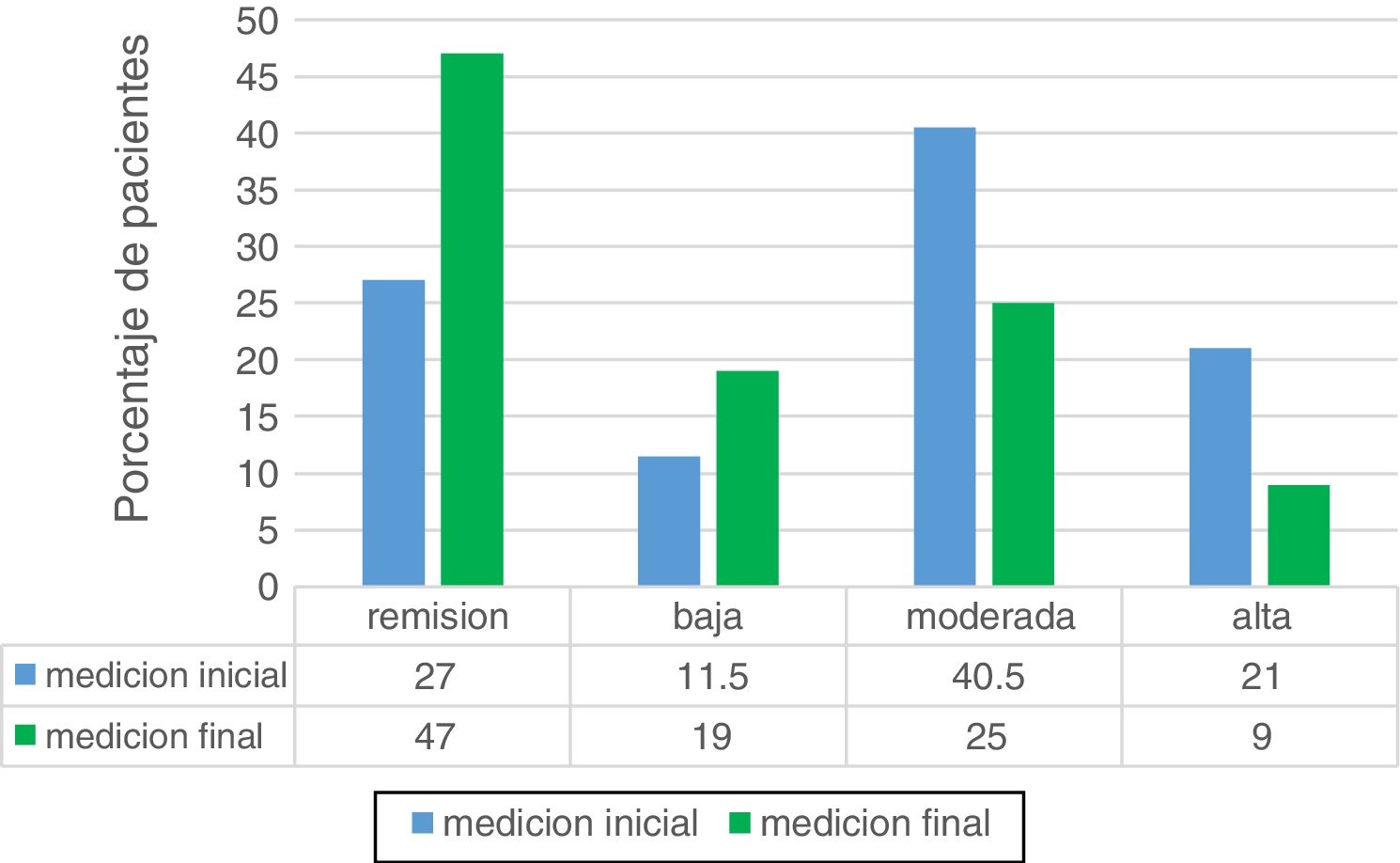
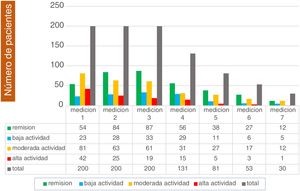
ResultsData was collected from 1905 patients during the period between August 2017 and March 2020. A total of 4864 consultations were made. Non-attendance of 368 (7.85%) consultations was registered. There were 1784 (83%) patients with a definitive diagnosis established by the rheumatologist. A total of 284 patients (14.9%) were discharged by the rheumatology service, and 85 (4.46%) were referred for an exclusively face-to-face evaluation. Auxiliary medical care at the place of origin was provided by a general practitioner in 1749 (91%) cases. There was no security during the care process as regards the physical examination in 46 (2.4%) cases. Of the total number of patients, 184 (9.6%) cases came from rural areas or municipalities far from the place of care. Biological therapies were prescribed in 139 patients, 56 new prescriptions during the 30 months. Of 479 RA patients, 200 met the criteria for follow-up. Of these, according to the activity measured by DAS28 with the use of ultrasensitive CRP, 54 patients (27%) were found on admission to the program in remission, 23 (11.5%) patients had low activity, 81 (40.5%) patients had moderate activity, and high activity was found in 42 (21%) patients. Regarding the start of follow-up, there was a 47% increase in the number of patients in remission, and in low activity to 19.5%, in contrast to a reduction of 25% in patients with moderate activity and of 9% in high activity in their last measurement, possible during monitoring. In the group of 200 patients from long-term follow-up, biological therapies were used 61 times. Of the 166 patients during follow-up without biological therapies on admission, these were required in 16%.
DiscussionA detailed follow-up of the patients was carried out in the telemedicine service in a synchronous way for a period of two and a half years. The low percentage of absences shows a good adherence to the program. Physical examination, the main reason for medical care at the remission site, was not without difficulties, in this minority it was necessary to carry out diagnostic images. It would be important to assess this group of patients where there are doubts regarding the physical examination, those who have a certain number of appointments without a definitive diagnosis, or in whom biological or high-cost therapies would be used should necessarily be referred to face-to-face consultation. In the group of patients with RA, the percentage of use of biologics is considered high in relation to the expected standards. This may be for several reasons, such as the high number of patients with prior use of biological agents, the majority of patients with long-term disease, and difficulties in accessing follow-up by rheumatology, as well as the small number of sero-negative patients in the study population, and practices related to non-presential medical practice may overestimate the activity of the disease. In conclusion, telemedicine has great advantages in the care of rheumatology patients, although it requires modifications to improve these services in favor of patients.
Los modelos de atención en salud fueron por largo tiempo estáticos. Sin embargo, recientemente se dio un cambio al reconocer que la tecnología en el área de información y comunicación podría generar un cambio en favor de los servicios de salud. La telemedicina ha venido en aumento y su uso se ha extendido a todo el proceso de la atención en salud. En Colombia está iniciando su implementación en el área de la reumatología. En el presente escrito se describen las características de un servicio de telerreumatología, así como una observación más detallada de una cohorte de pacientes con artritis reumatoide (AR) atendidos mediante modalidad sincrónica, con el fin de identificar fortalezas y mejoras.
MétodosSe realizó un estudio observacional descriptivo de corte transversal de la población total de pacientes que fueron atendidos en el servicio de telerreumatología en la modalidad sincrónica, por un periodo de 30 meses. Para la descripción del seguimiento de pacientes con AR se incluyó a todo paciente atendido exclusivamente mediante telemedicina por un periodo mínimo de 6 meses, con al menos 3 seguimientos en los que fue posible el cálculo de la clinimetría mediante DAS28 con uso de proteína C reactiva (PCR). Para el análisis descriptivo se usaron medidas de frecuencia, tendencia central y dispersión según el tipo de variable.
ResultadosDurante el periodo comprendido entre agosto del 2017 y marzo del 2020 fueron recolectados los datos de 1905 pacientes. Se realizó un total de 4864 consultas. Se registró una inasistencia de 368 consultas (7,85%). Los pacientes con un diagnóstico definitivo por parte del reumatólogo fueron 1784 (83%). Se dio alta por el servicio de reumatología a 284 pacientes (14,9%) y se remitieron para valoración exclusivamente presencial a 85 (4,46%). La atención médica auxiliar en el lugar de origen fue facilitada por médico general en 1749 casos (91%). Durante el proceso de atención sucedió que no había seguridad respecto al examen físico en 46 casos (2,4%). Del total de pacientes, 184 (9,6%) provenían de áreas rurales o municipios lejanos al lugar de atención. Las terapias biológicas se formularon en 139 pacientes, 56 nuevas formulaciones durante los 30 meses. De 479 pacientes con AR, 200 cumplían los criterios para el seguimiento. De estos, según la actividad medida por das28 con uso de PCR ultrasensible, se encontraron al ingreso al programa en remisión 54 pacientes (27%); baja actividad, 23 pacientes (11,5%); moderada actividad, 81 pacientes (40,5%) y alta actividad, 42 pacientes (21%). Respecto al inicio del seguimiento se encontró un aumento en el número de pacientes en remisión a 47% y baja actividad a 19,5%, en contraste con una reducción de pacientes con moderada actividad a 25% y de alta actividad a 9% en su última medición posible durante el seguimiento. En el grupo de 200 pacientes del seguimiento a largo plazo las terapias biológicas se usaron en 61 ocasiones. De los 166 pacientes durante el seguimiento sin terapias biológicas al ingreso, estas fueron requeridas en el 16%.
DiscusiónDurante un periodo de dos años y medio se llevó un detallado seguimiento de los pacientes en el servicio de telemedicina en modo sincrónico. Llama la atención el bajo porcentaje de inasistencias, lo que puede representar una buena adherencia al programa. El examen físico, razón principal para la atención médica en el sitio de remisión, no estuvo exento de dificultades. Esta minoría obligó a la realización de imágenes diagnósticas. Sería importante valorar si este grupo de pacientes, sobre los cuales hay dudas respecto al examen físico, quienes llevan un número de citas sin diagnóstico definitivo o en quienes se usarían terapias biológicas o de alto costo, debería necesariamente ser referido a consulta presencial. En el grupo de pacientes con AR, el porcentaje de uso de biológicos se considera elevado en relación con los estándares esperados, aunque el número de formulaciones, sin incluir los pacientes previamente formulados con biológicos, es bajo. Esto puede tener varias explicaciones, como el alto número de pacientes con uso previo de biológicos, la mayoría de los pacientes con enfermedad de larga evolución y dificultades para el acceso al seguimiento por reumatología, el escaso número de pacientes seronegativos y las prácticas propias del ejercicio médico no presencial que pueden sobreestimar la actividad de la enfermedad. En conclusión, la telemedicina tiene grandes ventajas en la atención de pacientes reumatológicos, aunque requiere modificaciones para la mejoría de estos servicios en favor de los pacientes.
The health care needs of the populations have changed over time. The development of new technologies and new scientific knowledge of each pathology triggered an increase in the prevalence of chronic diseases and then, a greater demand for better opportunities for specialized care, greater consumption of human and consequently, economic resources. All this in the global context of economic and health care inequality, more marked in rural areas, a problem that exists in developed countries such as Australia1 and is more noticeable in countries such as Colombia and in general in Latin America.2
The health care models were static for a long time. However, a change recently occurred when it was recognized that technology in the area of information and communication could generate a change in favor of health services that allows the creation of telemedicine services in different fields of medical care, including the entire health-disease process. These services make possible not only the improvement at the qualitative level, but also at the quantitative, with greater efficiency and opportunity.
Specifically in the clinical area, telemedicine has been useful in the diagnosis, treatment, follow-up and rehabilitation of patients. In other words, in almost the entire care process.3
Telemedicine is defined internationally as the use of communication technologies for the provision of health services.4 The advantages of this type of service are, among others, that it limits the use of hospital visits, allows care in remote or rural areas, facilitates access to specialized care, enables more timely care, reduces time and stress of traveling, lowers travel expenses and reduces costs for insurers and for the system.5–7
The disadvantages include costs, technology development and maintenance; the absence of physical examination in some cases; the depersonalization of the medical act, especially when there is no doctor in the place of origin; the management and privacy of the patients and their data; the acceptability of patients and health professionals, who also require a cultural change and new training in these technologies.
In Colombia, telemedicine has been used for more than one decade8 in different areas such as, for example, radiology, in which it has shown both benefits in care and economic advantages. Among the different telemedicine programs implemented in the country stand out those carried out by the University of Cauca and the National University of Colombia, which include educational and assistential activities aimed at remote areas of the national territory such as Leticia, San Andrés Islands, Arauca and Chocó.
Despite almost two decades of development of telemedicine in Colombia, we face great limitations, such as the still low acceptance for the expansion of the services due to the generation of initial costs and the difficult access to technology in very remote areas. All this contrasts with the increase in life expectancy and chronic diseases, the population growth, the greater health coverage,9 the concentration of human talent in large cities, as well as the poor implementation in cities where there are human resources and only economic performance is sought.
According to the needs of the country in this matter, efforts have been made aimed at its regulation, by Law 1448 of 2006 in the case of habilitation and Law 1419 of 2010 for its development. The latter defines telemedicine as the «provision of health services from a distance in the components of promotion, prevention, diagnosis, treatment and rehabilitation, by health care professionals who use information and communication technologies, which allow them to exchange data with the purpose of facilitating the access and opportunity in the provision of services to the populations with limited supply, access to the services or both in their geographic area», governed by basic principles of health care such as efficiency, universality, solidarity, integrality, unity and participation, in the terms defined by Article 2 of Law 100 of 1993.
From the technical point of view, there are several modalities of telemedicine: synchronous, asynchronous and remote monitoring. The synchronous modality uses real time communication between the two locations, including systems of audio, video or both, and the physician and the patient see each other simultaneously. The asynchronous modality, which is the most recognized, the eConsult, is based on the strategy of real-time messaging between the parties. Finally, remote medical monitoring is based on the submission of data by the patient to a database for subsequent review, as for example applications for monitoring symptoms or telephone answering systems.5,10,11
Specifically in the area of rheumatology, in Colombia, as in the rest of the world, telemedicine is on the rise. In addition, the current COVID-19 pandemic, in which it is sought to maintain social distancing, has made it become an imperious need. Adult or pediatric tele-rheumatology are special due to certain characteristics of the patients and their pathologies that generate impact on mobility and independence related or not to pain, and therefore limit the displacement to larger cities where the human talent is concentrated.12–14
If the models established in the provision of medical services are taken into account, one of the concerns is the acceptance by patients of the change to telemedicine, despite being more accessible in many cases. In this regard, a Colombian study measured the degree of satisfaction of some patients who used the telemedicine service in an area near Bogotá, through the synchronous modality and patient monitoring, and the researchers found that 75% of the respondents considered that the service was equal to or better than the conventional, 80% were satisfied or very satisfied, and 63% would use the service again. As additional data, 90% of patients considered that the doctor showed more interest in them, compared with the usual medical appointments, and 93% sustained that communication was not difficult.15 In the specific area of rheumatology, the satisfaction was measured in a rural population of Australia, and it was found that 90% of the patients considered that telemedicine is a satisfactory method for health care. Of these patients, almost 70% totally disagreed with switching from telemedicine to a conventional method in which they had to travel.13 These results were similar to those of other countries.16,17
Not only the acceptance by patients is important, but these alternatives must show to be effective in resolving the health problem. Two systematic reviews tried to summarize the data in the literature until 2017 in the area of rheumatology, and found that the populations studied were highly variable with respect to telemedicine modalities; the purpose was mostly for follow-up and the majority had a significant level of bias.18,19 Even so, are more the studies that show to be effective in the diagnosis and follow-up of inflammatory pathologies, specifically in rheumatoid arthritis, which makes telemedicine an acceptable model of health care in rheumatologic pathology.
This descriptive study seeks to show the characteristics of one of the largest telerheumatology services in the country regarding its operation and population, as well as a more detailed observation of a cohort of patients with rheumatoid arthritis (RA), followed-up exclusively by telemedicine, also in order to identify strengths and improvements.
MethodsA descriptive observational cross-sectional study was conducted on the total population of patients who were treated by the tele-rheumatology service in the synchronous modality in the different cities, during a period of 30 months, starting in August 2017 and ending in March 2020, in an institution of fourth level of care in the city of Bogota as the place of reception. In addition, a descriptive follow-up of a cohort of rheumatoid arthritis patients that met the inclusion criteria was carried out.
The main objective was to determine the characteristics of the population and the operation of the service of rheumatologic telemedicine in the Clínica Universitaria Colombia. The specific objectives were to describe the use of biological therapies in the population, as well as the behavior of a cohort of patients with a diagnosis of RA with respect to the change in disease activity, in addition to describing the characteristics of this population.
All patients over 18 years of age who attended the telemedicine consultation of rheumatology during the study period were included for the description of the total population. All patients treated exclusively through the modality of synchronous telemedicine, for a minimum period of six months and with at least three follow-ups in which it was possible to calculate clinimetry by means of DAS28 using the C reactive protein (CRP) were taken into account for the description of the follow-up of patients with RA. This protein was chosen over the follow-up with the erythrocyte sedimentation rate, since it was found with less frequency in the history.
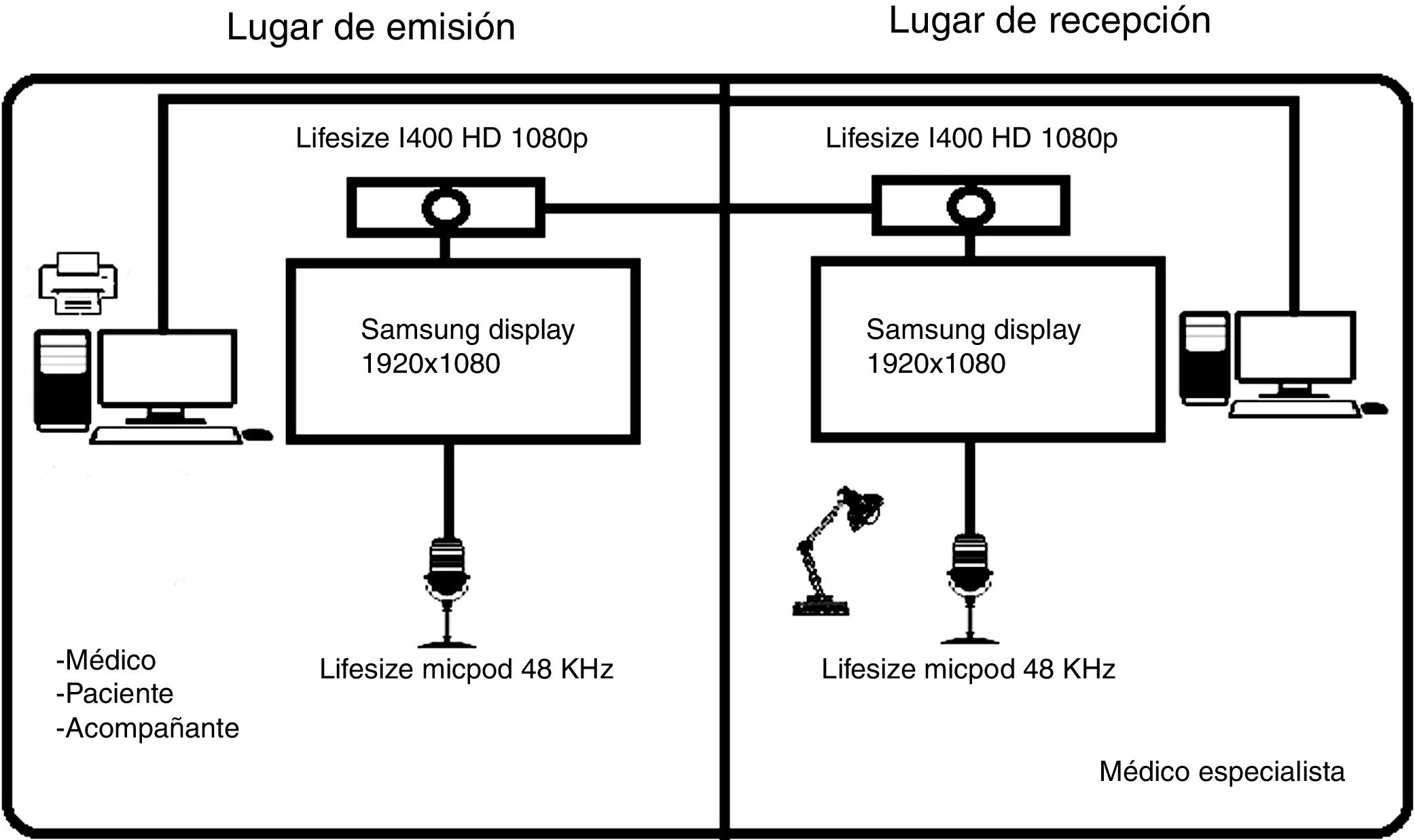
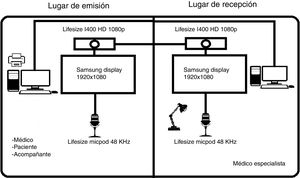
The entire interrogatory and the analysis of the results of paraclinical tests were carried out by the medical specialist at the reception site, taking into account the model of synchronous medical care. Authorized and duly secure channels are available for care, according to the legal provision for a telemedicine office enabled for sending diagnostic images or clinical photographs, with the authorization of the patient in the consultation. The primary role of the physician at the referral site is the physical examination. Due to its special importance in rheumatology, and even more in the realization of clinimetry, the professional has received training and has minimal knowledge for carrying out the exam. In this regard, most of the supporting physicians are general practitioners in charge of the program of rheumatoid arthritis in their respective city, accompanied by rheumatologists.
Data were obtained from medical records, retrospectively or prospectively, depending on the case. This was done with prior authorization from the ethics committee and the research unit of the Sanitas University Foundation, where data protection is specifically contemplated. All patients, by legal provision, signed consent for the provision of medical care through the modality of synchronous telemedicine.
It will be taken the universe of the patients who attend the rheumatology service by telemedicine during the period of 30 months. Sampling will be non-probabilistic for convenience.
Measures of frequency, central tendency and dispersion will be used for the descriptive analysis, according to the type of variable. The statistical analysis of the data will be performed using the Statistical Package for the Social Sciences (SPSS-15).
ResultsDuring the period between August 2017 and March 2020, data of 1905 patients seen under the modality of synchronous medicine were collected. Of the patients, 1645 were women (86.3%) and 260 men (13.7%). The average age was 51 years. The model of care is explained in Fig. 1. In this process, the medical specialist is on charge of the entire care, except for the physical examination, as mentioned previously.
In these 30 months, a total of 4864 consultations were made and a non-attendance of 368 consultations was registered (7.85%).
The patients with a definitive diagnosis established by the rheumatologist were 1784 (83%) and the remaining 121 continue under study (17%). Of the latter, 74 patients (61%) were seen only on one occasion, 25 patients (21%) on two occasions, 12 patients (10%) on three occasions, and the remaining 10 were seen on more occasions.
284 patients (14.9%) were discharged from the rheumatology service and 85 (4.46%) were referred for an exclusively face to face evaluation, the vast majority due to the complexity of the pathologies or because of hearing difficulties. In addition, it should be mentioned that the patients with initial evaluation by telemedicine in the city of Villavicencio, and with a diagnosis of rheumatoid arthritis (RA), were discharged by telemedicine for administrative reasons, which required medical consultations in Bogotá, and were not counted as egresses or referrals.
The auxiliary medical care in the place of origin was provided by a general practitioner in 1749 cases (91%), a family physician in 138 cases (7%) and an internist in the remaining 19 cases (2%).
During the care process, there was no certainty regarding the physical examination in 46 cases (2.4%). Consequently, the following aids were requested to solve the problem: 23 patients with magnetic resonance imaging of the hands, 14 patients with joint ultrasound (the majority of the knee), referral to dermatology in 5 patients (determination of the presence of scleroderma, 2 of them required biopsy) and referral to face-to-face rheumatology in 4 cases.
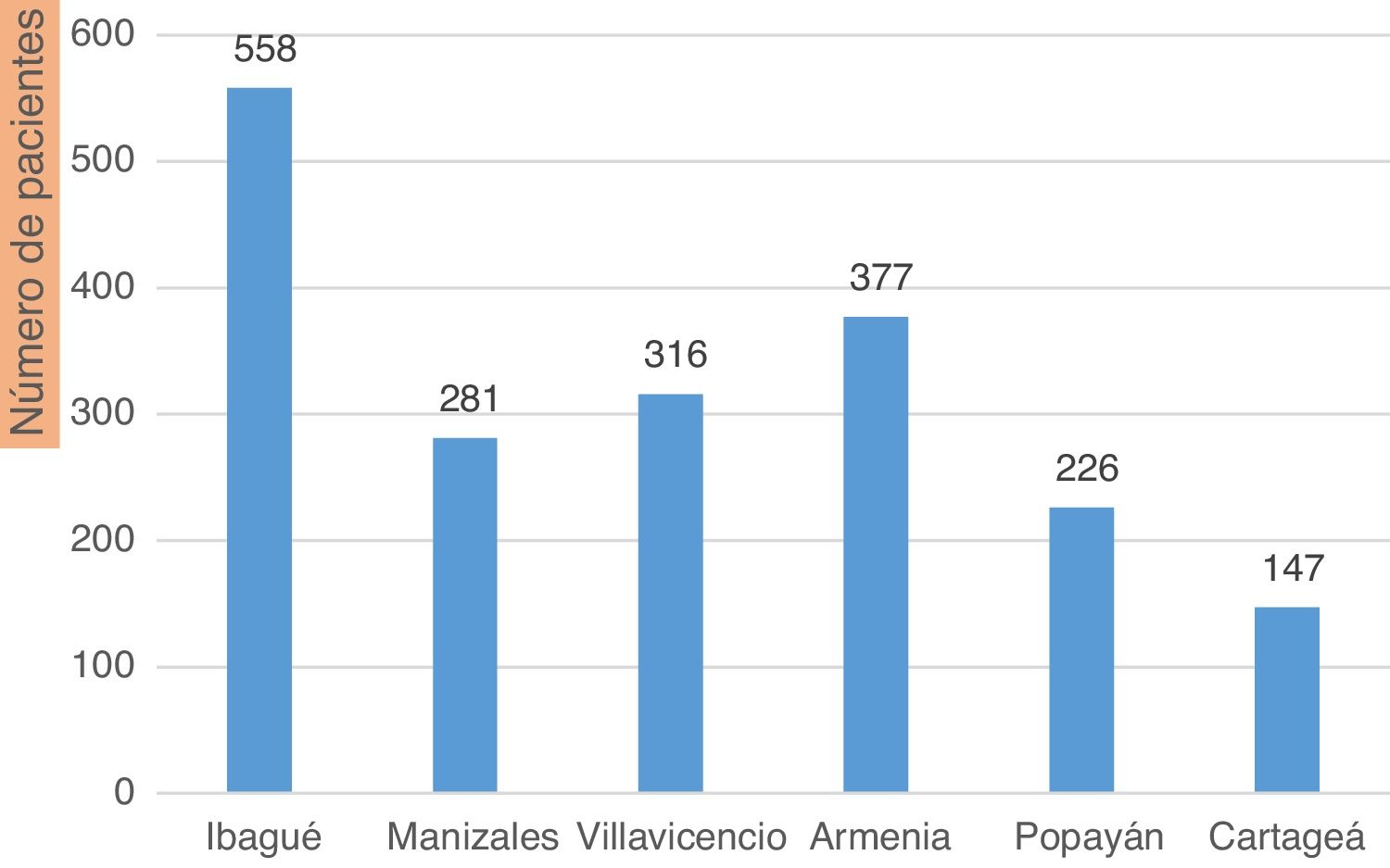
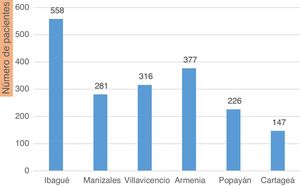
The place of the consultation is discriminated in Fig. 2. Of the total number of patients, 184 (9.6%) came from rural areas or municipalities far from the place of care; the majority of consultations were made in intermediate cities.
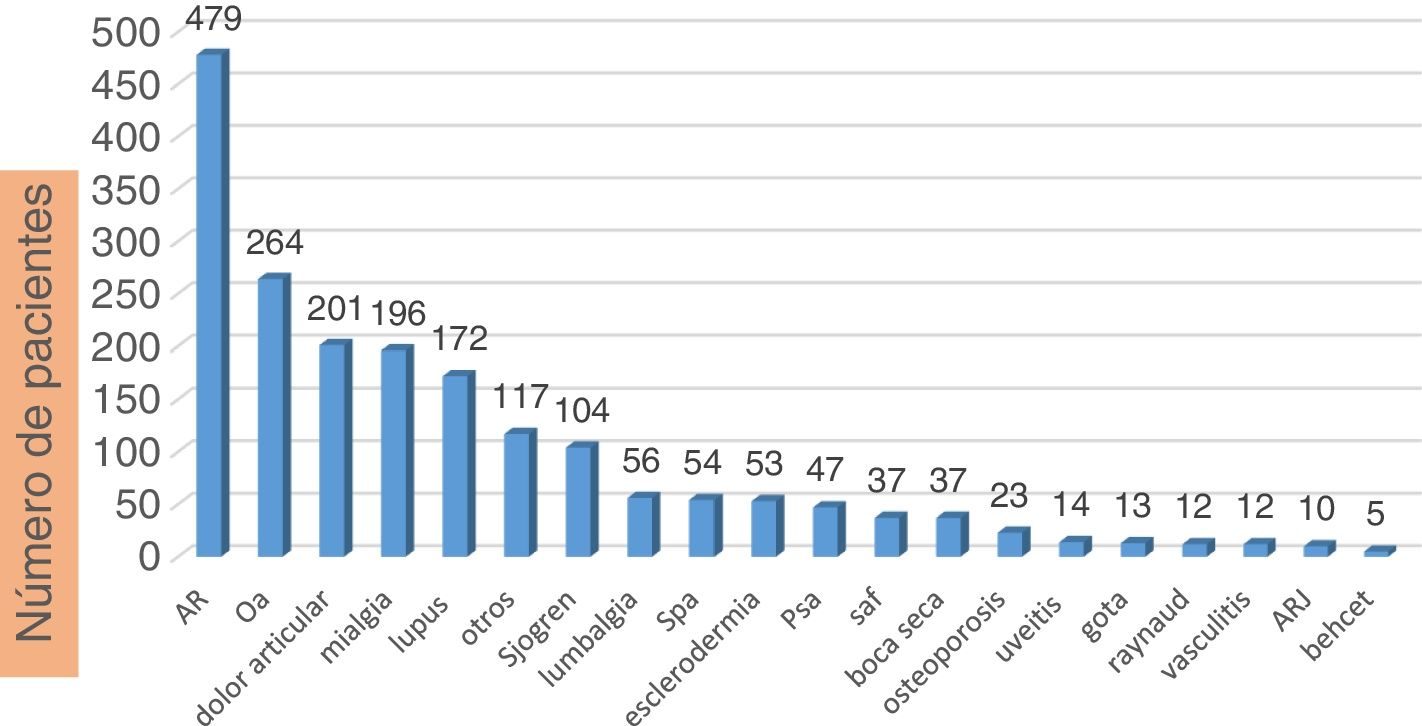
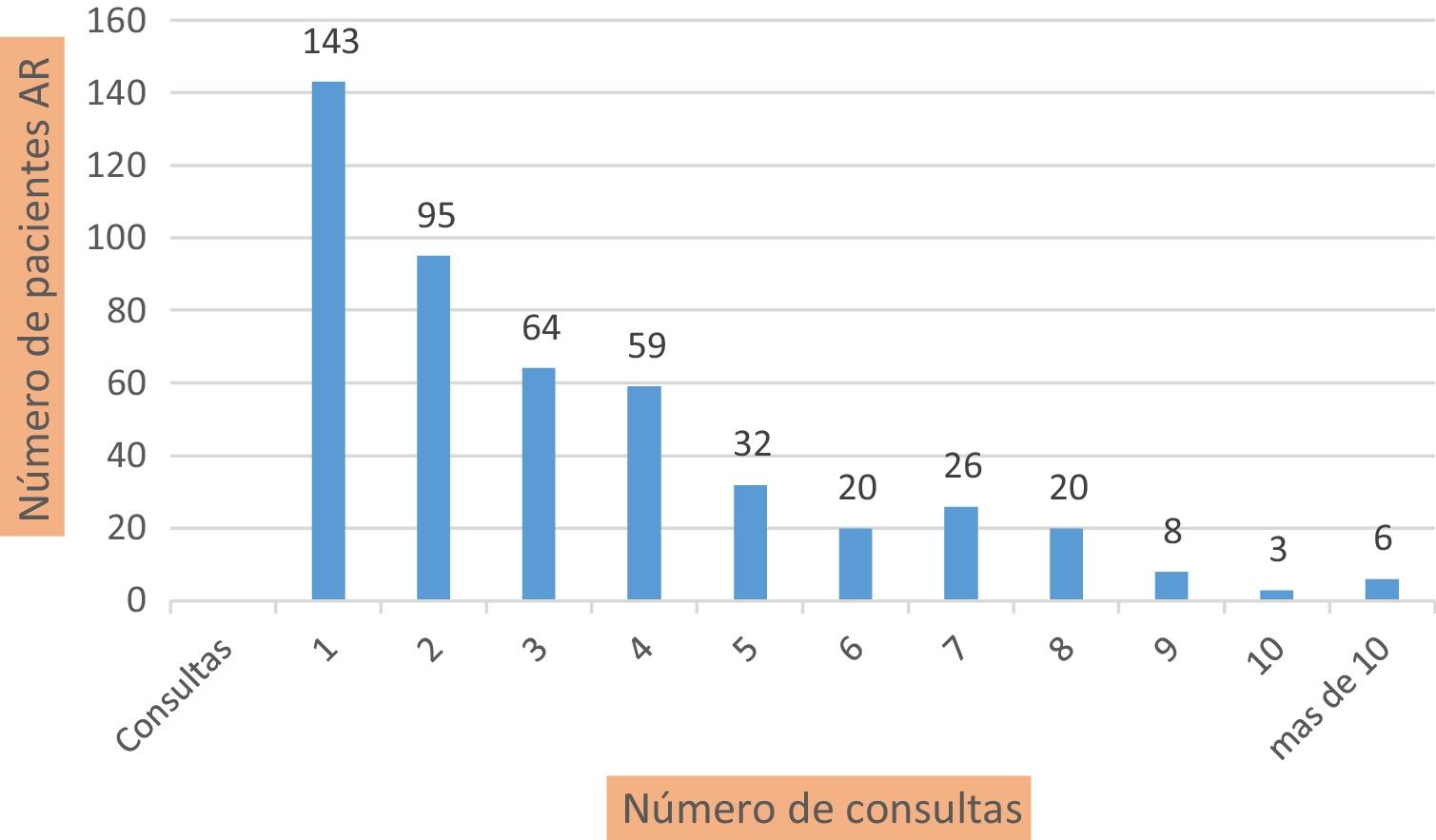
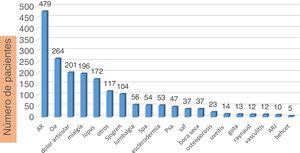
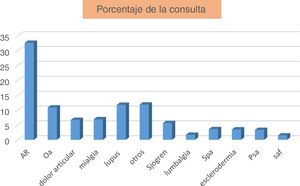
The most frequent main diagnoses were: RA in 479 patients (25%), osteoarthritis in 264 patients (13.8%), joint pain in 201 patients (10.5%), myalgia in 196 patients (10.2%; including diagnosis of fibromyalgia M797) and systemic lupus erythematosus in 172 patients (9%). The summary of the diagnoses is presented in Fig. 3. In Fig. 4, these diagnoses are shown according to the number of consultations, over a total of 4864.
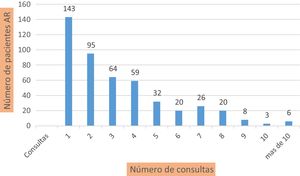
As shown in the graphic representations, the largest number of patients, and therefore of consultations, corresponds to patients with RA. This group is discriminated in Fig. 5, in which the number of consultations is related to the number of patients.
A separate analysis regarding the use of special therapies was conducted. In the city of Cartagena, gamma globulin was used for refractory dermatomyositis in one patient, with a good response. Cyclophosphamide in monthly or semi-monthly pulses was required in 15 patients, mostly for the management of lupus nephritis. Biological therapies were prescribed in 139 patients, 83 (60%) were reformulations prior to entering the telemedicine program and 56 corresponded to new formulations during the 30 months. In this period, 7 biological therapies were withdrawn.
Of the 478 patients seen with RA, 87 used biological therapy (18%; including patients with synthetics of specific target). Of these patients, 59 (68%) were reformulations and 28 (32%) were new prescriptions. Therefore, of the 419 patients who were admitted without biological agents, 6.6% were prescribed.
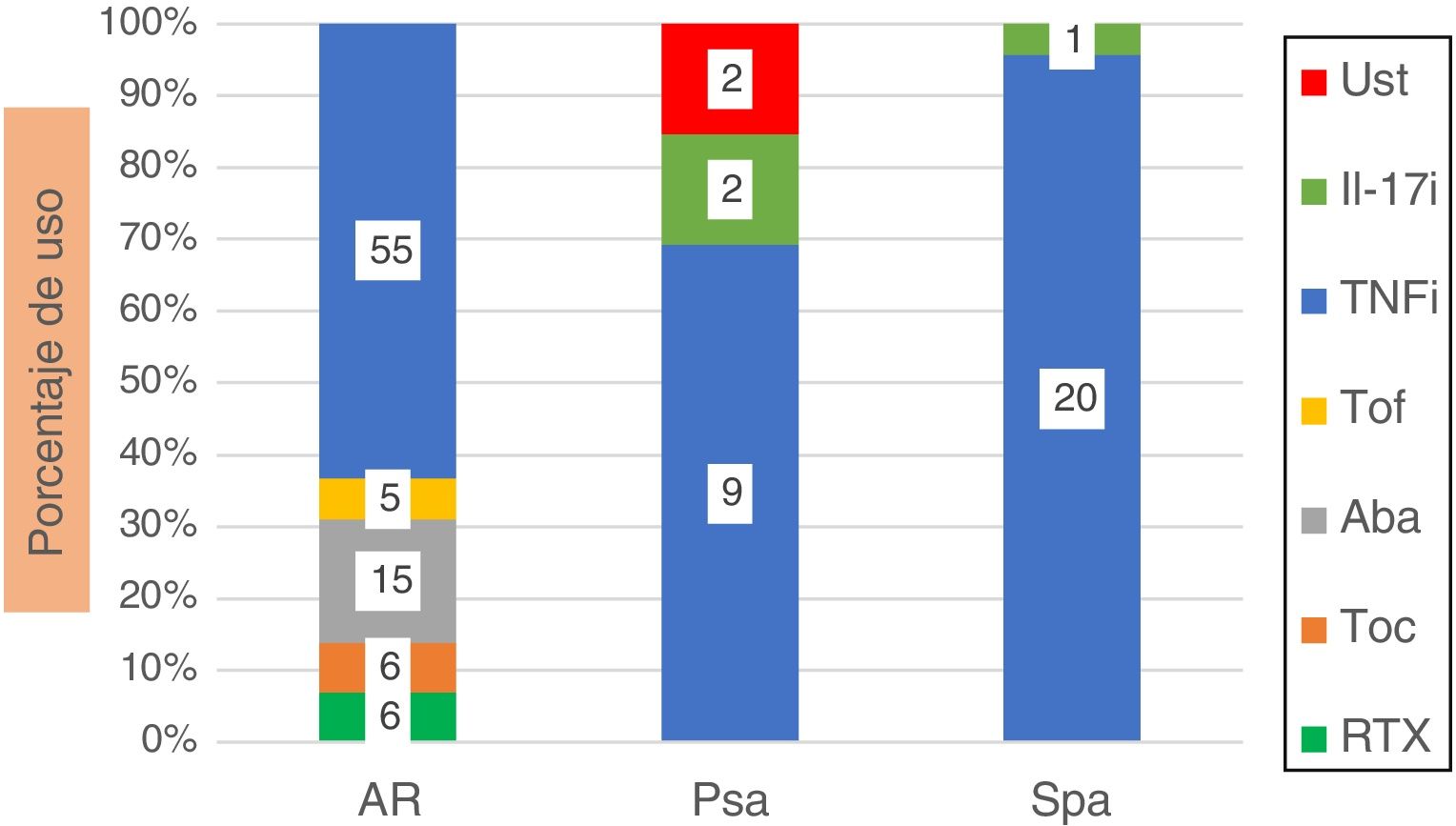
In other diagnoses, such as psoriatic arthritis, biological therapies were used in 27% of patients (77% reformulations in 10 patients) and in spondyloarthropathies (SpA, including ankylosing spondylitis and non-radiographic spondyloarthropathy) in 38% (42% reformulations in nine patients). The distribution of the use of biological therapy by drug is presented in Fig. 6.
Use of biological therapy according to pathology. In boxes, the number of patients. Ust (ustekinumab), IL-17i (IL-17 inhibitors), TNFi (tumor necrosis factor inhibitors), Tof (tofacitiniv), Aba (abatacept), Tc (tocilizumab), RTX (rituximab), RA (rheumatoid arthritis), PsA (psoriatic arthritis), SpA (spondyloarthropathies).
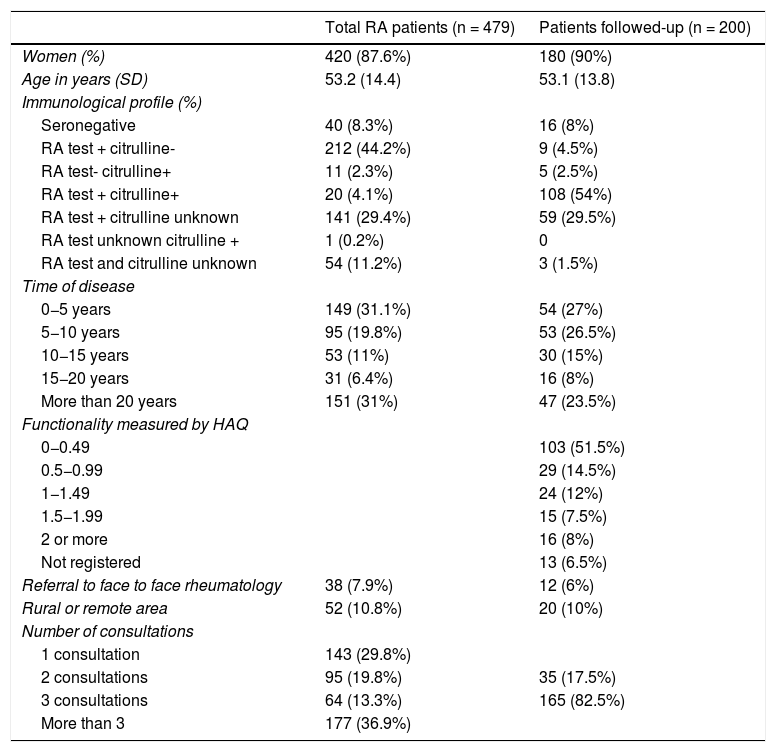
Regarding the analysis of the cohort of patients with RA during these 30 months of study, a total of 479 patients were obtained, and of them, 200 met the criteria for follow-up. The data of these groups of patients are presented in Table 1.
Characteristics of the RA populations, total of patients and follow-up group.
| Total RA patients (n = 479) | Patients followed-up (n = 200) | |
|---|---|---|
| Women (%) | 420 (87.6%) | 180 (90%) |
| Age in years (SD) | 53.2 (14.4) | 53.1 (13.8) |
| Immunological profile (%) | ||
| Seronegative | 40 (8.3%) | 16 (8%) |
| RA test + citrulline- | 212 (44.2%) | 9 (4.5%) |
| RA test- citrulline+ | 11 (2.3%) | 5 (2.5%) |
| RA test + citrulline+ | 20 (4.1%) | 108 (54%) |
| RA test + citrulline unknown | 141 (29.4%) | 59 (29.5%) |
| RA test unknown citrulline + | 1 (0.2%) | 0 |
| RA test and citrulline unknown | 54 (11.2%) | 3 (1.5%) |
| Time of disease | ||
| 0−5 years | 149 (31.1%) | 54 (27%) |
| 5−10 years | 95 (19.8%) | 53 (26.5%) |
| 10−15 years | 53 (11%) | 30 (15%) |
| 15−20 years | 31 (6.4%) | 16 (8%) |
| More than 20 years | 151 (31%) | 47 (23.5%) |
| Functionality measured by HAQ | ||
| 0−0.49 | 103 (51.5%) | |
| 0.5−0.99 | 29 (14.5%) | |
| 1−1.49 | 24 (12%) | |
| 1.5−1.99 | 15 (7.5%) | |
| 2 or more | 16 (8%) | |
| Not registered | 13 (6.5%) | |
| Referral to face to face rheumatology | 38 (7.9%) | 12 (6%) |
| Rural or remote area | 52 (10.8%) | 20 (10%) |
| Number of consultations | ||
| 1 consultation | 143 (29.8%) | |
| 2 consultations | 95 (19.8%) | 35 (17.5%) |
| 3 consultations | 64 (13.3%) | 165 (82.5%) |
| More than 3 | 177 (36.9%) |
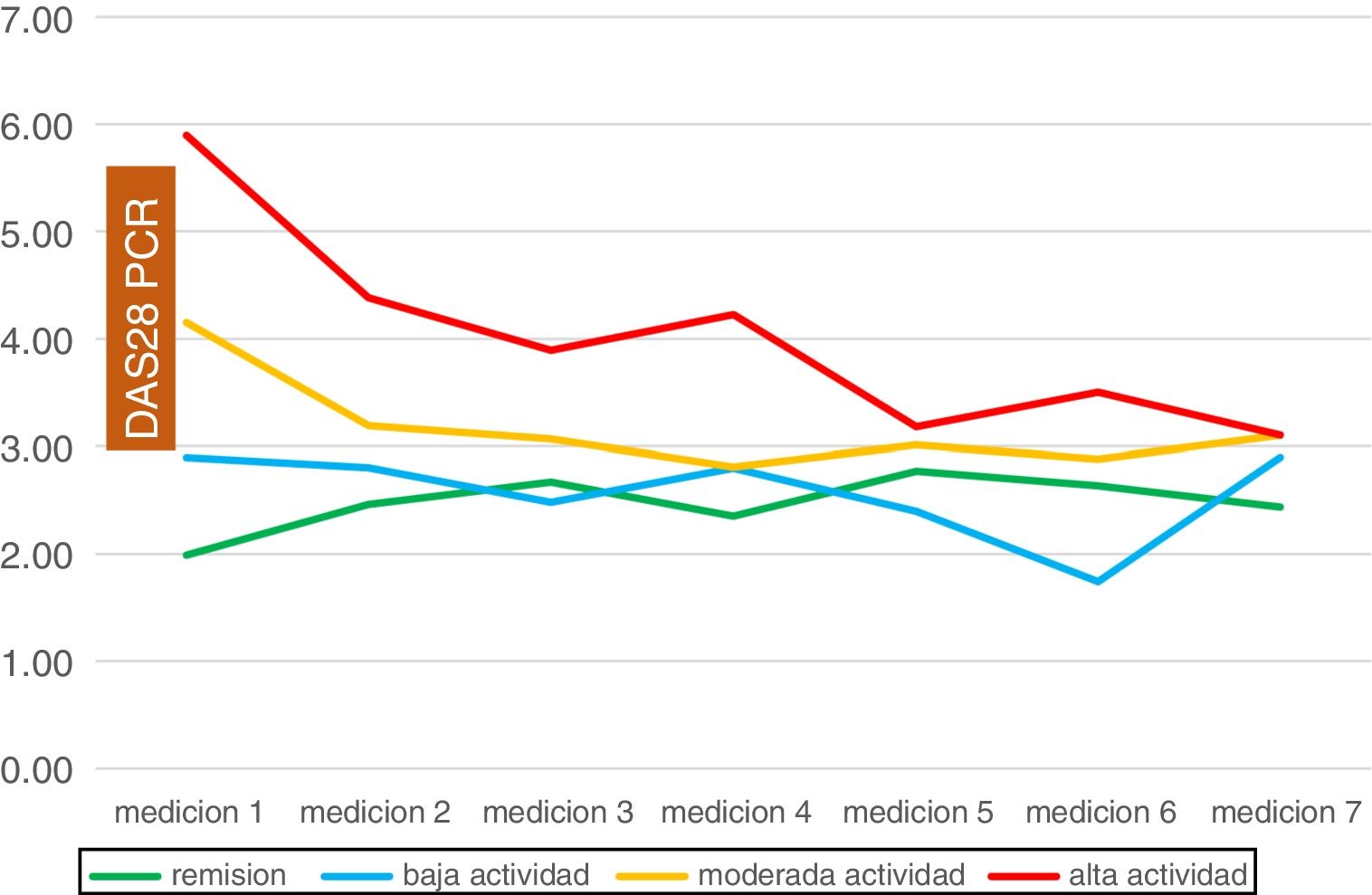
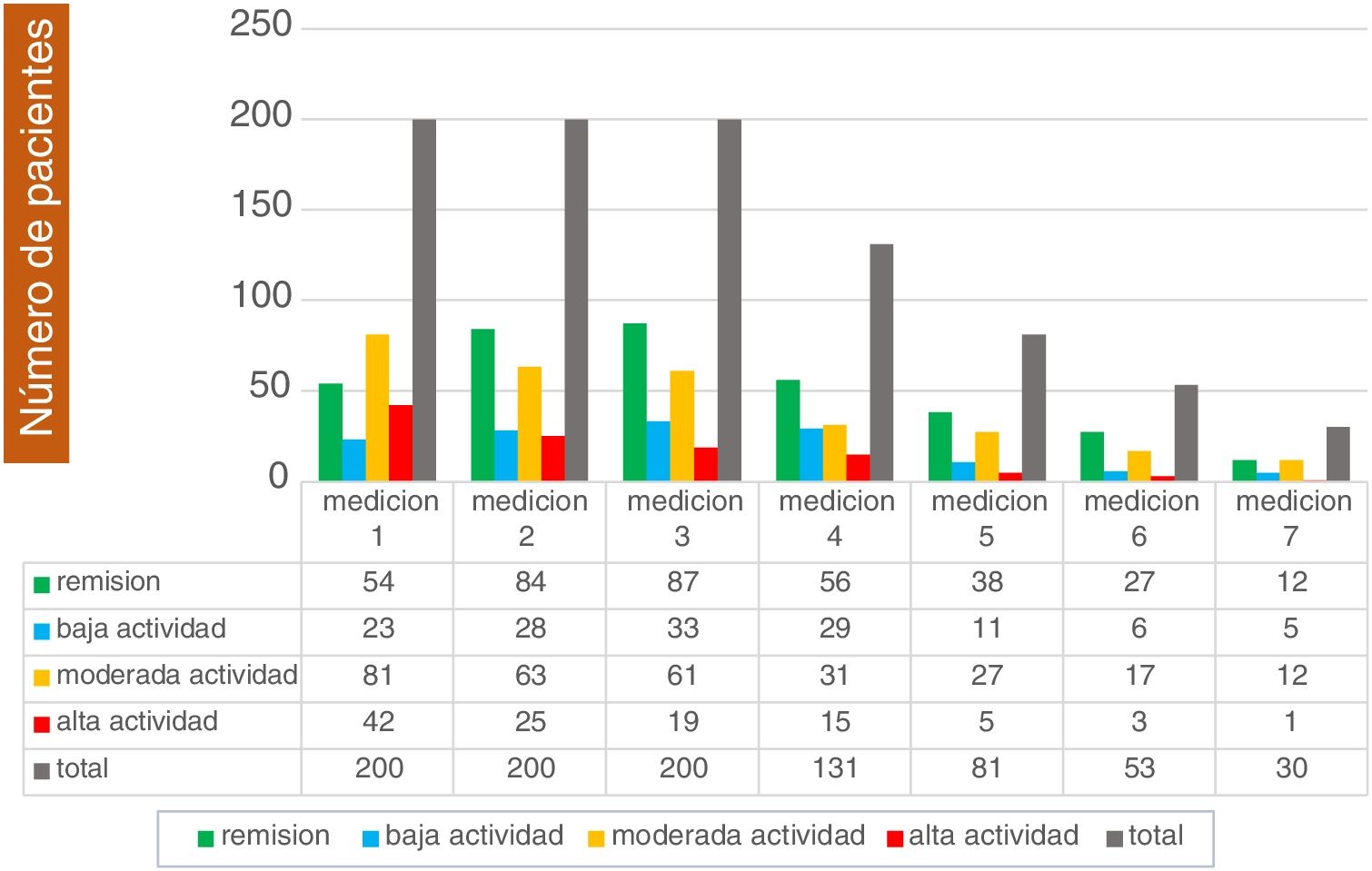
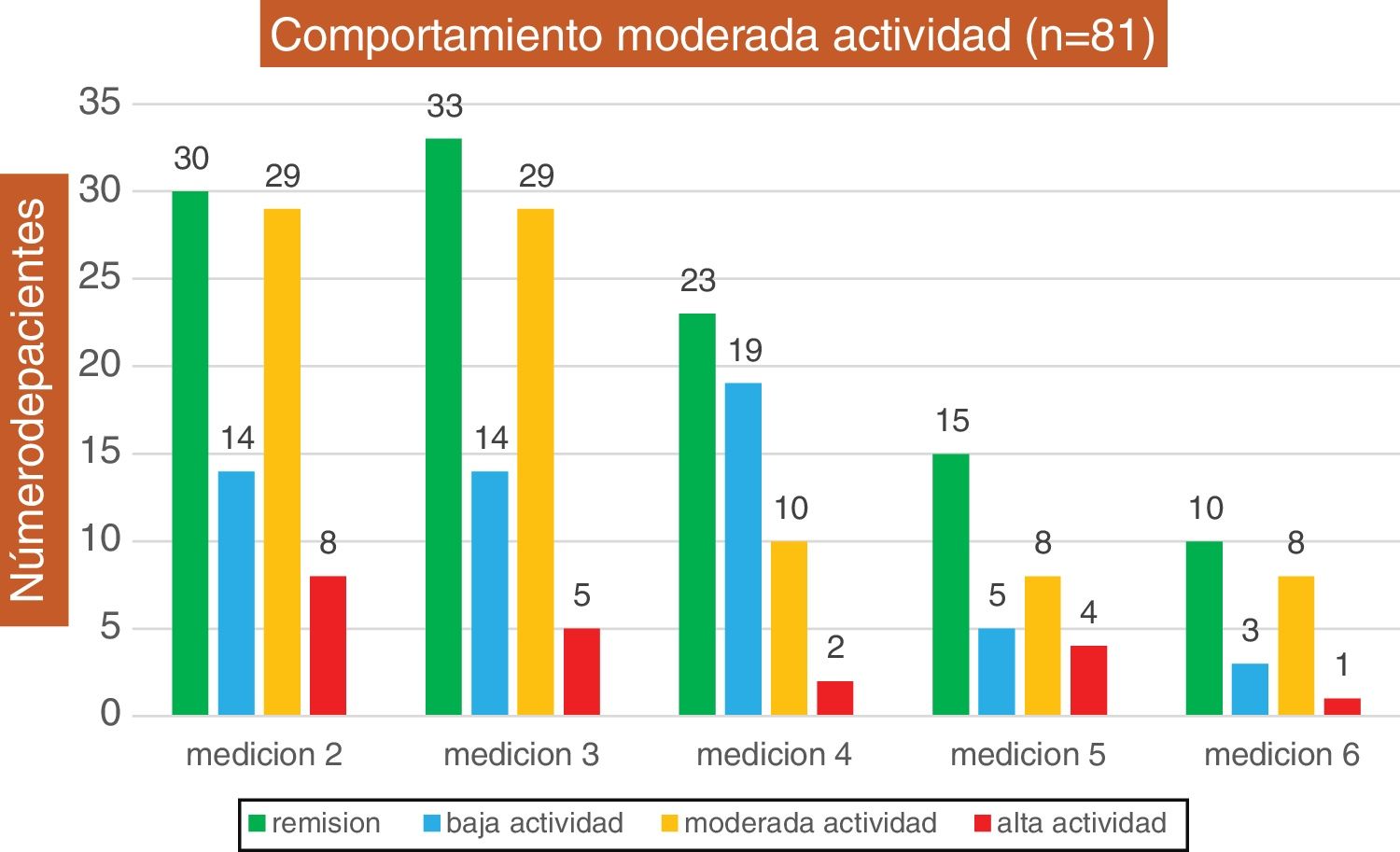
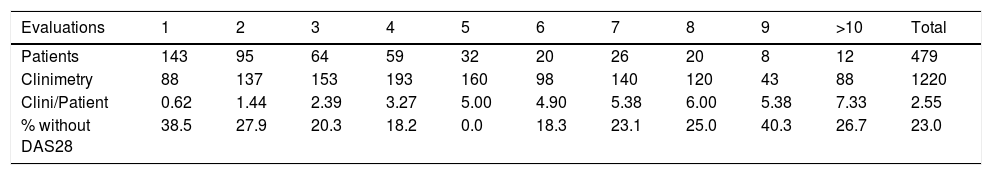
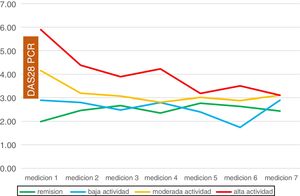
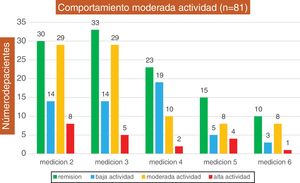
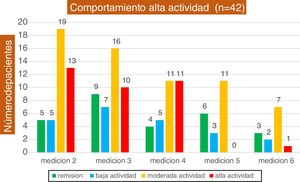
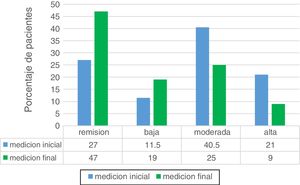
According to the activity measured by DAS28 with the use of ultrasensitive CRP, on admission, of these 200 patients, 54 (27%) were found in remission (DAS28 CRP < 2.6), 23 (11.5%) with low activity (DAS28 PCR 2.6–<3.2), 81 (40.5%) with moderate activity (DAS28 CRP 3.2–5.1), and 42 (21%) with high activity (DAS28 CRP > 5.1). The evolution of these patients in their subsequent follow-ups is shown in Figs. 7–11. It is only taken into account until the evaluation number 7, since the subsequent number of patients is low: 7 patients with 8 evaluations, 5 patients with 9 evaluations and 2 with 10 evaluations by DAS28 CRP.
The data related between the number of controls and the possibility of performing clinimetry are found in Table 2, in which it can be evidenced that there are a large number of visits in which control by DAS28 CRP was not possible. A total of 1587 consultations were made in the 479 patients, for a total of 1220 estimations. Therefore, only 77% were made and 367 medical assessments were not accomplished.
Number of clinimetries by DAS28 CRP, according to the number of evaluations.
| Evaluations | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | >10 | Total |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Patients | 143 | 95 | 64 | 59 | 32 | 20 | 26 | 20 | 8 | 12 | 479 |
| Clinimetry | 88 | 137 | 153 | 193 | 160 | 98 | 140 | 120 | 43 | 88 | 1220 |
| Clini/Patient | 0.62 | 1.44 | 2.39 | 3.27 | 5.00 | 4.90 | 5.38 | 6.00 | 5.38 | 7.33 | 2.55 |
| % without DAS28 | 38.5 | 27.9 | 20.3 | 18.2 | 0.0 | 18.3 | 23.1 | 25.0 | 40.3 | 26.7 | 23.0 |
Clini/patient: clinimetries per patient.
Regarding the start of the follow-up, it was found an increase in the number of patients in remission to 47% and with low activity to 19.5%, in contrast with a reduction of patients with moderate activity to 25% and with high activity to 9% in the last measurement possible during the follow-up (Fig. 11).
The follow-up time of the patients is variable due to the difference in the number of evaluations. The patients with 3 evaluations were followed-up on average 43.5 weeks; those with 4 evaluations, 58.7 weeks; with 5 evaluations, 81 weeks; with 6 evaluations, 94 weeks; with 7 evaluations, 101 weeks; and with more than 7 evaluations, 110 weeks.
In the group of 200 patients in long-term follow-up, biological therapies were used on 61 occasions (30%). Of them, 34 patients (56%) were receiving biologic agents when they were admitted to the telemedicine program and 27 (44%) were new prescriptions. Of the 166 patients without biological therapies on admission, these therapies were required in 16% during follow-up.
DiscussionDuring a period of two and a half years, a detailed follow-up of the patients in the telemedicine service was carried out in synchronous mode. A large number of patients were captured, showing the great variety of pathologies, inflammatory and non-inflammatory, which are representative of the entire diagnostic spectrum of the rheumatology specialty.
The origin of the patients was mostly from the city of Ibagué, since the program was initially implemented there. The low percentage of non-attendance draws attention, which could represent a good adherence to the program by the population studied. Unfortunately, we do not have data of non-attendance from face-to-face programs to make a comparison.
The usefulness of this model of care includes a group of 184 patients, which, although it is a minority, resides in rural municipalities or far from the center of care, thus avoiding long displacements to the big cities of the country.
The physical examination, which is the main reason for medical attention at the referral site, was not exempt from difficulties. In this minority it forced to perform diagnostic images such as magnetic resonances in 23 patients. It would be important to assess whether this group of patients in which there are doubts regarding the physical examination (2.4% of the total), as well as those who have a certain number of appointments without a definitive diagnosis, 22 patients with 3 or more appointments (1.5% of the total), should necessarily be referred to face-to-face consultation, taking into account the difficulties to travel and the lack of human talent in certain regions of the country.
The use of biological therapies considered of high cost is an important factor to be analyzed: 39 patients required the use of biologics without previous formulations in the three most important pathologies (RA, SpA, PsA), which represents 2% of the total population. It is proposed as part of the improvements to see this group of patients also in person prior to the start of biologics, provided that their referral does not delay the start of the treatments and therefore does not lead to the deterioration of the patient or the appearance of complications. In the group of patients with RA in whom the follow-up analysis was done (200 patients), the percentage of use of biologic agents is considered a little bit high in relation to the expected standards. This could have many explanations, such as the high number of patients with biologic agents before entering the program; the high proportion of patients with long-standing disease and the difficulties to access the follow-up by rheumatology before entering telemedicine; the high number of seropositive patients and therefore with factors of poor prognosis; and practices characteristic of non-face-to-face medical practice that can overestimate disease activity as some symptoms cannot be differentiated from secular or non-inflammatory medical conditions, a situation that occurs in face-to-face specialized consultation and is also a major diagnostic challenge.
Regarding the group of patients with RA (479 individuals), half of them were evaluated only once or twice, largely because many of them are referred to face-to-face consultations or their admission to the program was close to the cut of follow-up. In a third (33%) of the follow-ups, clinimetry by DAS28 was not possible due to the lack of recent laboratory tests of at least two previous months.
For the follow-up of patients with RA and their behavior in telemedicine, those who had at least 6 months with 3 clinimetries were selected. This occurred in 200 patients, of whom 60% had no control of their disease upon admission, because it was in moderate or high activity.
It was observed that the groups of patients in remission and low activity at admission remained in this group of activity throughout the observation, and due to the effect of medical control, there was a significant reduction in the number of patients with moderate activity by 39% and with high activity by 57%, at the end of the observed period.
The foregoing shows that telemedicine services can be efficient and effective in the care of the rheumatologic population, ensuring that the entire spectrum of the disease is treated, in addition to improving the access to healthcare of high level of complexity. To those to whom the service is offered, this is a reason for review and control, preventing it for being used for purely economic purposes, since as it is recognized, telemedicine will not replace face-to-face care, even if it is carried out with all the legal conditions and habilitations that imply no affectation of the quality of care. Likewise, there is evidence that allows making recommendations for the improvement of these services, focusing on the groups in which an early referral to face-to-face consultation is made in a timely manner
In a group of patients which is very representative of the specialty of rheumatology, such as that made up of those who suffer from rheumatoid arthritis (RA), it is shown that care by this synchronous method, added to a medical examiner with basic experience and a minimum of training can improve the condition of patients, allowing them to continue to control their disease and reducing the number of cases of moderate and high activity.
Among the limitations of the study is the possibility of information and observation bias, taking into account that the data were taken with the knowledge that an assessment of the service and its care model by the staff of the place of emission and reception was being carried out.
ConclusionTelemedicine is a tool generated by the need to cover health services with greater impact in remote places, or where there is no human resource. It has advantages and disadvantages, but in general when is well applied it has shown significant potential to improve these health and even economic and social indices. It was shown a cohort of patients with results in favor of this technique in our service. It is recommended to implement it in appropriate cases, such as when local specialized human resources for health care are insufficient or not available; that patients cannot move due to physical, economic, or even cultural limitations; and that a good technical-scientific application, data care, patient privacy and no deterioration of the working conditions of health personnel can be ensured.
Conflict of interestThe authors declare that they have no conflict of interest.
Please cite this article as: Cajas Santana LJ, López JG. Descripción de un servicio de telerreumatología en una institución colombiana. Rev Colomb Reumatol. 2021;28:161–170.