Henoch-Schönlein purpura is the most common vasculitis in children, with kidney involvement remaining the main cause of morbidity and mortality. The spectrum of kidney involvement ranges from mild symptoms to the development of a nephrotic and/or nephritic syndrome or kidney failure.
ObjectiveTo determine the clinic features at onset, and kidney involvement of patients with a final diagnosis of Henoch-Schönlein purpura during the first month, 3 months, and up to the first year of follow-up.
MethodsA retrospective study conducted on patients with a final diagnosis of Henoch-Schönlein purpura in a Pediatric Rheumatology Department in an institution of Bogota, Colombia, during the period between 2010 and 2016.
ResultsThe study included 86 patients, 42 girls and 44 boys. The median age at disease onset was 5.3 years (SD 2.4 years: range 1–14 years). Kidney involvement was present in 39/86 (45%) patients. A trend to kidney involvement was observed in patients with abdominal symptoms (p=0.053). The most frequent clinical finding was isolated proteinuria (49%), followed of proteinuria/hematuria (28%), and isolated hematuria (15%). Renal biopsy was performed on 8/39 patients with Henoch-Schönlein purpura nephritis. The mean follow-up was 26.8 months (SD 17 months: range 1–72). There was no evidence of kidney damage in the last assessment in any of the 39 patients with kidney involvement.
ConclusionIn this group of patients, kidney involvement was more severe and common in the first weeks of the disease onset.
La púrpura de Henoch-Schönlein es la vasculitis más frecuente en la infancia. La afectación renal continúa siendo la causa de morbimortalidad principal en niños. El espectro del compromiso renal va desde manifestaciones leves hasta el desarrollo de síndrome nefrótico o nefrítico, o insuficiencia renal.
ObjetivoDeterminar las características clínicas al comienzo y el compromiso renal de los pacientes con diagnóstico definitivo de púrpura de Henoch-Schönlein, durante el primer mes, a los 3 meses y al año de seguimiento.
MétodosEstudio descriptivo, retrospectivo, de pacientes con diagnóstico definitivo de púrpura de Henoch-Schönlein, de la consulta de Reumatología Pediátrica, en una institución de Bogotá, Colombia, en el período comprendido de 2010 a 2016.
ResultadosOchenta y seis pacientes fueron incluidos en el estudio, 42 niñas y 44 niños, edad media de presentación 5,3 años, DE 2,4 años (1 a 14 años). Se presentó compromiso renal en 39 pacientes (45%). Se evidenció una tendencia mayor a compromiso renal entre los pacientes con artritis (p=0,053). El hallazgo clínico más frecuente fue proteinuria aislada (49%), seguido de proteinuria/hematuria (28%) y hematuria aislada en el 15%. Había 8/39 pacientes con compromiso renal durante el año de seguimiento que fueron llevados a biopsia, 6 (75%) con compromiso renal al inicio y 25% al mes. El promedio de seguimiento fue de 26,8 meses con una desviación estándar de 17 meses (1 a 72 meses), no hubo disfunción renal a la última valoración en ninguno de los 39 pacientes con compromiso renal.
ConclusiónEl compromiso renal fue más frecuente en las primeras semanas de la enfermedad, así como en las formas severas.
Henoch-Schönlein purpura (HSP) is the most common vasculitis in childhood. Described in 1837 by Johann Schönlein as an entity characterized by the presence of purpura and arthralgia, some years later Eduard Henoch evidenced renal involvement and gastrointestinal affectation as additional manifestations, thus acquiring the name with which it is known today. It is usually a benign and self-limited disease.1
HSP has an approximate incidence of 13.5 cases per 100,000 preschool age children and of up to 70 cases per 100,000 school age children, although it can affect all age groups.2,3 The distribution by gender is usually homogeneous, with a slight male predominance described in some series (1.2:1). Increases in cases have been described in winter seasons or during peaks of respiratory infections, often associated with infections of the upper tract in up to 30–50% of cases.4
It is postulated that children with HSP have an innate susceptibility added to an external triggering event, among which infectious agents, along with other antigenic stimuli such as insect bites, vaccines, drugs or food allergens have been identified; being probable that there is not a single specific mediator.5,6
The involvement of small vessels mainly of the skin, joints, gastrointestinal tract and kidneys is what determines the clinical behavior or this entity, being documented the presence of deposits of immunoglobulin A in the biopsy tissue.7,8
Renal affectation is still the leading cause of morbidity and mortality in children.9 Glomerulonephritis occurs in 30–50% of patients with HSP, 85% of cases during the first 4 weeks of the initial manifestation,10–12 91% within the first 6 weeks and 97% in the first 6 months. The spectrum of renal involvement ranges from mild manifestations to the development of nephrotic or nephritic syndrome, or kidney failure.13–15 Some risk factors which are predictors of the development of nephritis, such as persistent or recurrent purpura, severe abdominal symptoms, older age at the onset, and relapse of the disease have been identified.16,17
Renal biopsy continues to be an important tool in cases of severe or persistent renal involvement, to determine the type of structural commitment, the need for immunosuppressive treatment and the risk of progression to renal failure.18
Materials and methodsIt is a descriptive, retrospective study of patients with final diagnosis of HSP, from the Pediatric Rheumatology outpatient service of an institution of Bogota, Colombia, to whom a single data collection form was applied in the period between 2010 and 2016.
The objective was to determine the clinical characteristics and renal involvement during the first year of follow-up.
Demographic, clinical, laboratory and histological data were included. The organ involvement was determined in each patient. The patients with renal involvement were classified according to the time in which the involvement occurred: at the onset of the disease, at one month, at 3 months, or between 3 months and one year of follow-up. The type of renal involvement was defined as: isolated hematuria, isolated proteinuria, hematuria/proteinuria, nephrotic syndrome or nephritic syndrome. Histopathological findings were documented in the patients with commitment that deserved the performance of a renal biopsy.
The quantitative variables were analyzed using measures of central tendency and standard deviation, and the qualitative variables by ratios and proportions. Bivariate analysis was conducted to establish the degree of correlation between the variables studied. The p-values <0.05 were considered statistically significant.
The data were stored on a database in Excel 2007 and were later statistically analyzed using the software SPSS version 23.0.
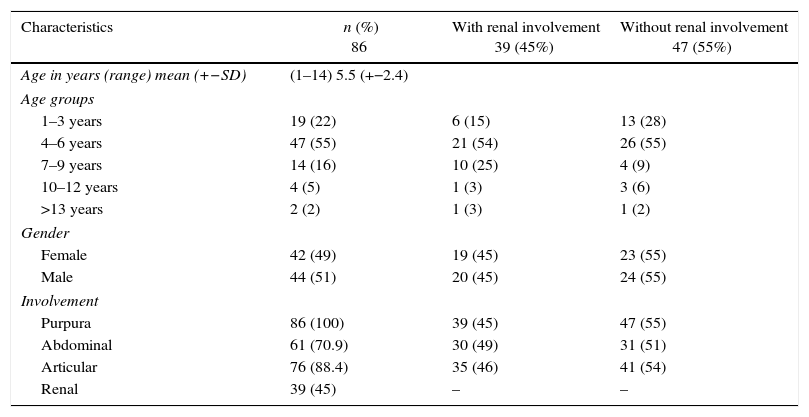
Results86 patients who attended the Pediatric Rheumatology outpatient service of an institution in Bogota were included. Of the total of 86 patients, 42 (49%) were girls and 44 (51%) boys, the mean age of presentation was 5.3 years with a range between 1 and 14 years. In terms of age distribution, the group with greater affectation was that of patients aged between 4 and 6 years (55%), in contrast to a low occurrence in patients older than 13 years (2%). All patients had palpable purpura, 88.4% arthritis, 70.9% abdominal pain and 45% renal involvement. The socio-demographic characteristics are shown in Table 1.
Socio-demographic characteristics.
| Characteristics | n (%) 86 | With renal involvement 39 (45%) | Without renal involvement 47 (55%) |
|---|---|---|---|
| Age in years (range) mean (+−SD) | (1–14) 5.5 (+−2.4) | ||
| Age groups | |||
| 1–3 years | 19 (22) | 6 (15) | 13 (28) |
| 4–6 years | 47 (55) | 21 (54) | 26 (55) |
| 7–9 years | 14 (16) | 10 (25) | 4 (9) |
| 10–12 years | 4 (5) | 1 (3) | 3 (6) |
| >13 years | 2 (2) | 1 (3) | 1 (2) |
| Gender | |||
| Female | 42 (49) | 19 (45) | 23 (55) |
| Male | 44 (51) | 20 (45) | 24 (55) |
| Involvement | |||
| Purpura | 86 (100) | 39 (45) | 47 (55) |
| Abdominal | 61 (70.9) | 30 (49) | 31 (51) |
| Articular | 76 (88.4) | 35 (46) | 41 (54) |
| Renal | 39 (45) | – | – |
Renal involvement was documented in 39 (45%) of the 86 patients included in the study, with a male: female ratio of 1:1. Of the 39 patients with renal involvement, 56% presented it at the time of diagnosis, 31% during the first month, 5% between the first and the third month, and the remaining 8% between 3 and 12 months of follow-up.
Renal involvement occurred most frequently in the age group between 4 and 6 years (54%), followed by children between 7 and 9 years (25%), being less frequent in the groups of 1–3 years and older than 10 years. There were no significant differences between genders in terms of renal affectation (p=0.57).
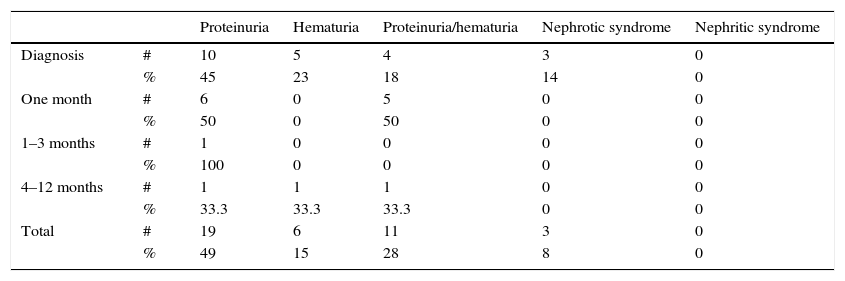
The most frequent clinical finding was isolated proteinuria, which was found in 49% of patients with renal involvement, followed by proteinuria/hematuria in 28%, isolated hematuria in 15%; nephrotic syndrome as a severe manifestation was present in 8% of patients and there were no data of patients with nephritic syndrome. In all patients with manifestations of severe renal involvement, they appeared during the first weeks after disease onset (Table 2).
Type of renal involvement.
| Proteinuria | Hematuria | Proteinuria/hematuria | Nephrotic syndrome | Nephritic syndrome | ||
|---|---|---|---|---|---|---|
| Diagnosis | # | 10 | 5 | 4 | 3 | 0 |
| % | 45 | 23 | 18 | 14 | 0 | |
| One month | # | 6 | 0 | 5 | 0 | 0 |
| % | 50 | 0 | 50 | 0 | 0 | |
| 1–3 months | # | 1 | 0 | 0 | 0 | 0 |
| % | 100 | 0 | 0 | 0 | 0 | |
| 4–12 months | # | 1 | 1 | 1 | 0 | 0 |
| % | 33.3 | 33.3 | 33.3 | 0 | 0 | |
| Total | # | 19 | 6 | 11 | 3 | 0 |
| % | 49 | 15 | 28 | 8 | 0 |
#: number of cases; %: percentage corresponding to that number of cases.
A higher trend to kidney involvement was observed among the patients with abdominal commitment (p=0.053), association not seen in the patients with joint involvement (p=0.53).
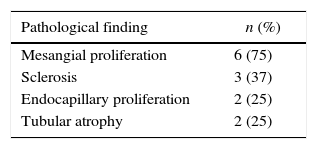
Biopsies were performed to 8 (20.5%) of the 39 patients with renal involvement during the 12 months of follow-up, 5 (62.5%) with involvement at the onset, being nephrotic syndrome and hematuria/proteinuria the indications for the procedure, the remaining 3 (37.5%) patients were biopsied because they presented with nephrotic-range proteinuria without nephrotic syndrome associated with hematuria during the first 4 weeks of evolution. None of the patients with renal involvement after the fourth week required histopathological study.
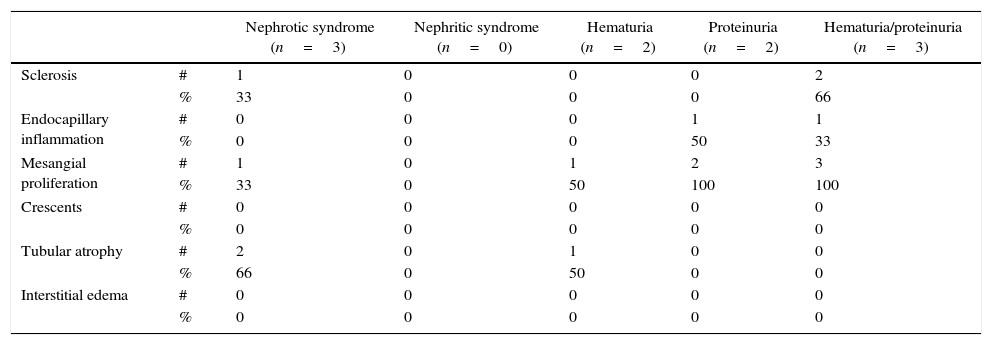
Mesangial proliferation was the most frequent finding in 6/8 patients, sclerosis in 3/8 patients (one patient with nephrotic syndrome and 2 patients with proteinuria/hematuria). There was no evidence of crescents in the biopsies (Tables 3 and 4).
Histopathological findings according to the renal involvement.
| Nephrotic syndrome (n=3) | Nephritic syndrome (n=0) | Hematuria (n=2) | Proteinuria (n=2) | Hematuria/proteinuria (n=3) | ||
|---|---|---|---|---|---|---|
| Sclerosis | # | 1 | 0 | 0 | 0 | 2 |
| % | 33 | 0 | 0 | 0 | 66 | |
| Endocapillary inflammation | # | 0 | 0 | 0 | 1 | 1 |
| % | 0 | 0 | 0 | 50 | 33 | |
| Mesangial proliferation | # | 1 | 0 | 1 | 2 | 3 |
| % | 33 | 0 | 50 | 100 | 100 | |
| Crescents | # | 0 | 0 | 0 | 0 | 0 |
| % | 0 | 0 | 0 | 0 | 0 | |
| Tubular atrophy | # | 2 | 0 | 1 | 0 | 0 |
| % | 66 | 0 | 50 | 0 | 0 | |
| Interstitial edema | # | 0 | 0 | 0 | 0 | 0 |
| % | 0 | 0 | 0 | 0 | 0 |
#: number of cases; %: percentage corresponding to that number of cases.
The mean follow-up was 26.8 months, with a standard deviation of 17 months (range: 1–72 months), in which the renal function was periodically evaluated. At the end of the 12 months and at the completion of the follow-up as a whole, none of the 39 patients with renal involvement had deterioration of the nitrogen compounds or commitment of the glomerular filtration.
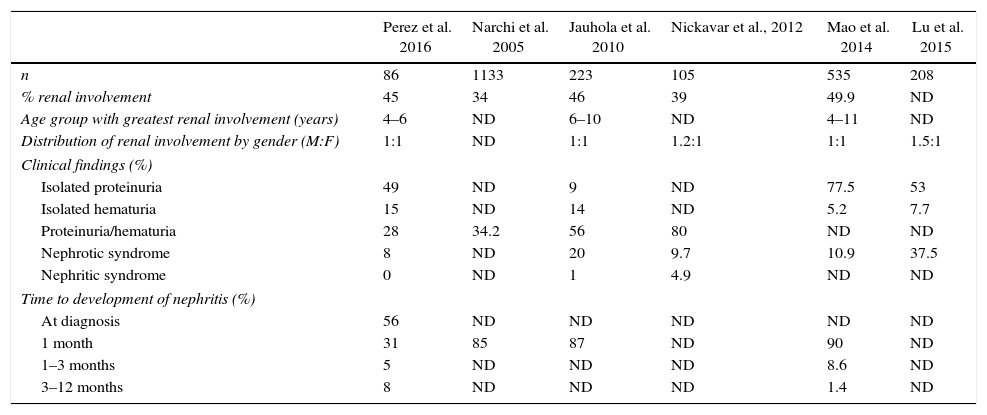
DiscussionRenal involvement in HSP ranges between 30 and 50% of patients, conditioning in general the long-term prognosis. In the present study, renal affectation was documented in 39 of the 86 participants (45%), a percentage of affectation similar to that was described in several series. The largest study reported in the literature so far is a systematic review which included 1133 patients with a frequency of renal involvement of 34%,19 smaller series have reported rates of renal affectation between 39 and 49.9% of patients with HSP20–23 (Table 5).
Comparison of clinical and epidemiological manifestations.
| Perez et al. 2016 | Narchi et al. 2005 | Jauhola et al. 2010 | Nickavar et al., 2012 | Mao et al. 2014 | Lu et al. 2015 | |
|---|---|---|---|---|---|---|
| n | 86 | 1133 | 223 | 105 | 535 | 208 |
| % renal involvement | 45 | 34 | 46 | 39 | 49.9 | ND |
| Age group with greatest renal involvement (years) | 4–6 | ND | 6–10 | ND | 4–11 | ND |
| Distribution of renal involvement by gender (M:F) | 1:1 | ND | 1:1 | 1.2:1 | 1:1 | 1.5:1 |
| Clinical findings (%) | ||||||
| Isolated proteinuria | 49 | ND | 9 | ND | 77.5 | 53 |
| Isolated hematuria | 15 | ND | 14 | ND | 5.2 | 7.7 |
| Proteinuria/hematuria | 28 | 34.2 | 56 | 80 | ND | ND |
| Nephrotic syndrome | 8 | ND | 20 | 9.7 | 10.9 | 37.5 |
| Nephritic syndrome | 0 | ND | 1 | 4.9 | ND | ND |
| Time to development of nephritis (%) | ||||||
| At diagnosis | 56 | ND | ND | ND | ND | ND |
| 1 month | 31 | 85 | 87 | ND | 90 | ND |
| 1–3 months | 5 | ND | ND | ND | 8.6 | ND |
| 3–12 months | 8 | ND | ND | ND | 1.4 | ND |
| Risk factor associated with nephritis | Abdominal involvement | ND | Abdominal involvement | >6 years | >6 years abdominal involvement | Abdominal involvement |
|---|---|---|---|---|---|---|
| Renal biopsy findings (%) | ||||||
| Mesangial proliferation | 75 | ND | ND | 100 | ND | ND |
| Sclerosis | 37 | ND | ND | 53 | ND | ND |
| Endocapillary proliferation | 25 | ND | ND | 64.7 | ND | ND |
| Tubular atrophy | 25 | ND | ND | 29.4 | ND | ND |
| Crescents | 0 | ND | ND | 59 | ND | ND |
| Mean follow-up time (months) | 26.8 | 85 | 6 | ND | 24 | ND |
| Renal failure or insufficiency at the end of the follow-up (%) | 0 | 1.8 | 0 | ND | 0 | 1.9 |
In the present study, children between 4 and 6 years of age were the age group in which most cases of HSP were documented, being the same group the one with the highest frequency of renal involvement. In the series of Jauhola et al.,20 the greatest renal affectation is reported in the range between 6 and 10 years of age, and in those of Mao et al.,22 the highest frequency of nephritis was concentrated in patients between 4 and 11 years of age, very wide age ranges, but in which is evident that children younger than 3 years remain being a population with low incidence of nephritis due to HSP.
Renal affectation can occur from the beginning, late or in successive outbreaks conditioning in most cases the prognosis of the disease. In the 6 series compared in Table 5, it is repeatedly evidenced that renal involvement occurred in up to 90% of cases during the first 4 weeks of evolution of the disease, being in this same period when the severe clinical manifestations such as nephrotic syndrome, nephrotic hematuria/proteinuria and renal failure appear.20–23 This is the reason why a strict follow-up should be done during this time looking for alterations at the level of the sediment and functional urine tests for the early instauration of treatment and prevention of progression to renal failure.4
In the present study the most frequently identified finding was isolated proteinuria, finding also reported by Mao et al.22 and by Lu et al.,23 in 2014 and 2015, with a presentation of 77.5 and 53%, respectively, being evident as forms of nephrotic syndrome in the 3 studies, in contrast with other series in which the most frequent finding was isolated hematuria followed by the combination of non-nephrotic hematuria/proteinuria.24 It is worthwhile to highlight that in most series the nephritic syndrome has a low incidence, as evidenced in our study in which no case was documented.
It has been clearly identified that some manifestations have been associated as predictors of increased renal commitment: patients with severe gastrointestinal manifestations, palpable purpura prolonged for more than 4 weeks, older age at the onset of the disease and need for treatment with systemic steroids.25 In the present study, a greater tendency to renal involvement was only documented in patients with abdominal commitment (p=0.05), finding also reported in previous studies, in which the mean of the onset of nephritis was 14 days after diagnosis, being identified the abdominal commitment as a risk factor for it (OR 2.1; p=0.017, CI 1.1–3.7).20 Mao described in 2014 that abdominal commitment, age over 6 years and purpura in sites other than the lower limbs, were the risk factors identified for the development of nephritis in 535 Japanese children22; situation not evidenced by Nickavar et al., in which the age greater than 6 years was the only predictor of renal affectation.21
The type of renal compromise, the severity and the time of appearance during the evolution of the disease have been correlated with the histopathological findings of renal biopsies. Coppo et al., report that patients with severe renal insufficiency and acute nephritis are correlated with histopathological findings of poor prognosis.26 In our study was evidenced that patients with nephritis during the first 4 weeks, presented isolated proteinuria, nephrotic syndrome and proteinuria/hematuria, being directly correlated with the presence of mesangial proliferation, sclerosis and endocapillary inflammation. Similar data were reported by Assadi et al., with direct correlation between these initial clinical manifestations and the glomerular involvement.27 It was not possible to document this relationship in all series because of the small number of patients who underwent renal biopsy and the use of different types of histopathological classification, which did not allow to establish a statistically significant correlation. In our study we took into account the general histopathological findings described in the biopsies, the correlation with the clinical manifestations, their time of appearance and the presence of risk factors for renal failure.
HSP is considered a benign and self-limited disease, although some series describe renal failure in up to 1.9% of the patients who develop nephritis.19,22,23 In our study, at one year and at the end of the follow-up none of the patients had renal failure. Despite the type of treatment established was not included in the study, the patients with important involvement received steroids and immunosuppressive agents which could have limited the progression to renal failure.
20% of our patients with nephritis were subjected to renal biopsy, frequency reported in other series in up to 25%.24 As for the positive correlation in this study between renal involvement at the onset of the disease, severe manifestations and histopathological findings, it is recommended a strict clinical follow-up and consideration of early biopsy in severe cases, as well as to consider this intervention in patients with persistent or increasing isolated proteinuria and hematuria.28 Studies that include a greater number of patients with histopathological study are required to establish a definitive recommendation.
ConclusionsRenal affectation in patients with HSP is more frequent in the first 4 weeks after diagnosis. The manifestations can be severe such as nephrotic syndrome and nephrotic proteinuria/hematuria. Renal involvement occurs most frequently in children between 4 and 6 years of age and isolated proteinuria is the most prevalent clinical finding in these patients.
Close monitoring during the first 4–6 weeks of diagnosis and education of the family are essential to ensure the identification of patients with renal involvement and thus guide the treatment and prevent the deterioration of renal function in the long term.
In severe or persistent forms, it is important to perform a renal biopsy in order to document the presence of factors for poor prognosis that allow decision making and modification of treatment.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestThe authors declare they do not have any conflict of interest.
Please cite this article as: Pérez López P, Mosquera Ponguta C, Malagón Gutiérrez C. Prevalencia del compromiso renal durante el primer año de seguimiento en pacientes con púrpura de Henoch Schönlein en una institución pediátrica de Bogotá, Colombia. Rev Colomb Reumatol. 2017;24:63–69.