Intervention thresholds for the treatment of osteoporosis have been based historically on the measurement of bone mineral density. The development of FRAX® has permitted more accurate assessment of fracture risk.
ObjectiveThe aim of the present study was to explore treatment paths and characteristics of women eligible for treatment in Ecuador based on FRAX.
Methodology and methodsA total of 2367 women aged 60–94 years were selected from the National Health, Welfare and Aging Survey (SABE) conducted in Ecuador. Probabilities of major osteoporotic and hip fracture were computed using the Ecuadorian FRAX model. The proportion of women eligible for treatment and bone mineral density assessment was determined based on age-specific intervention thresholds and a hybrid threshold was fixed from age 75 years.
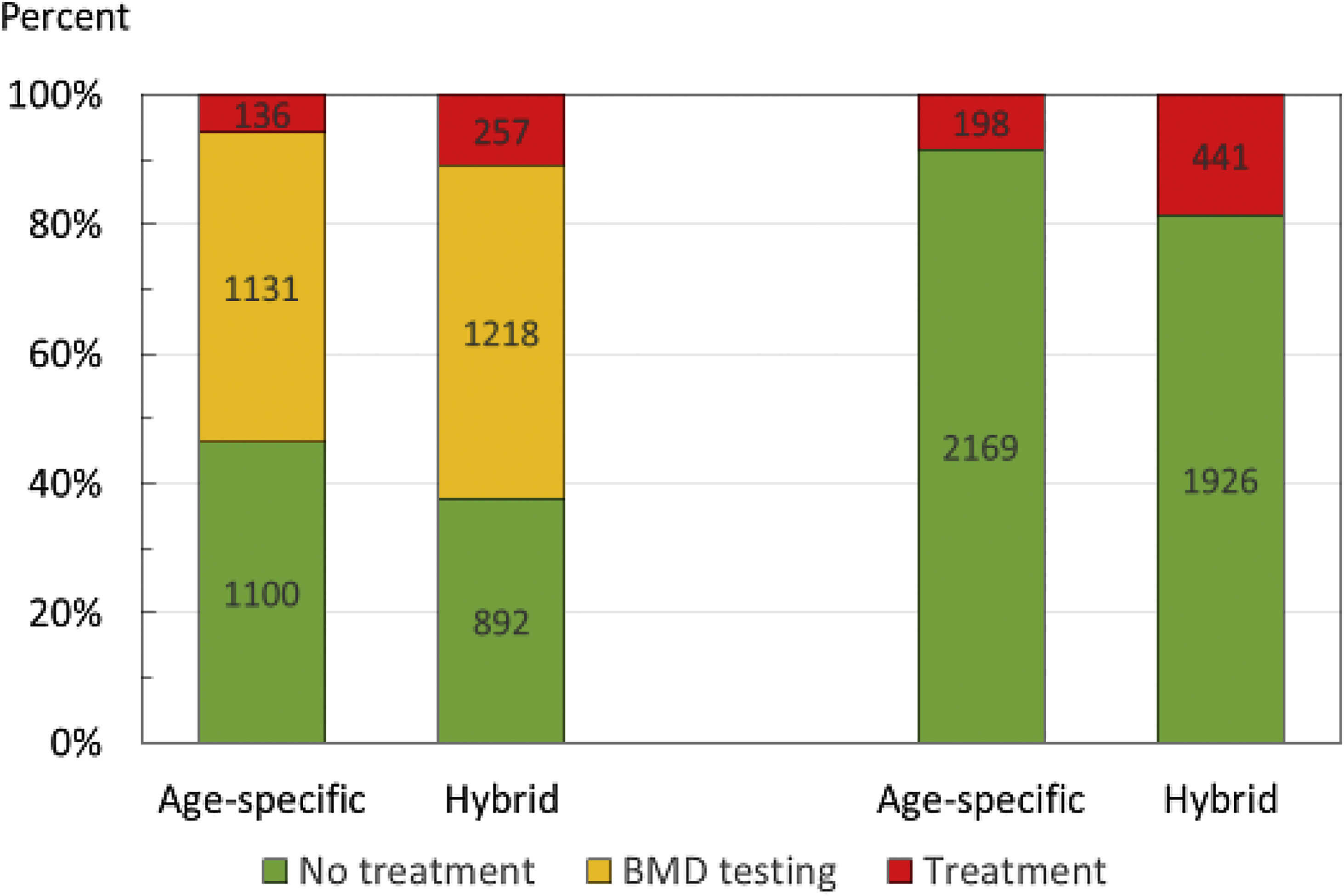
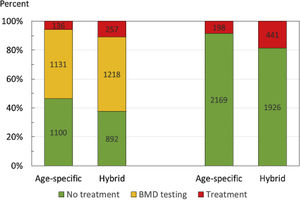
ResultsA total of 87 women (3.7%) had a prior fragility fracture and would be eligible for treatment for this reason. An additional 49 women were eligible for treatment in that MOF probabilities lay above the upper assessment threshold using age-specific thresholds. An BMD test would be recommended in 1131 women (48%) so that FRAX could be recalculated with the inclusion of femoral neck BMD. With the hybrid threshold, an additional 170 women were eligible for treatment and an BMD test recommended in 1218 women.
ConclusionsThe hybrid threshold identifies more women eligible for treatment than age-specific thresholds. Although age-specific thresholds identify women at higher risk of fracture, the lower number of women identified results in fewer identified fracture cases.
Los umbrales de intervención para el tratamiento de osteoporosis se han basado históricamente en la medición de la densidad ósea. El desarrollo del FRAX® ha permitido una evaluación más precisa del riesgo de fractura.
ObjetivoEl objetivo del estudio fue explorar las rutas de tratamiento y las características de las mujeres elegibles para tratamiento en Ecuador con base en FRAX.
Materiales y métodosSe seleccionó a 2.367 mujeres de 60 a 94 años de la encuesta SABE. Se calcularon las probabilidades de fracturas osteoporóticas principales y de cadera utilizando el modelo FRAX ecuatoriano. Se calculó la proporción de mujeres elegibles para tratamiento y evaluación de la densidad ósea, con base en umbrales de intervención específicos de la edad y de un umbral fijo a partir de los 75 años.
ResultadosOchenta y siete mujeres (3,7%) tenían una fractura previa y eran elegibles para tratamiento. Utilizando umbrales específicos de edad, otras 49 mujeres eran elegibles para recibir tratamiento debido a que las probabilidades de fractura osteoporótica principal estaban por encima del umbral de evaluación superior. Se recomienda medir la densidad ósea en 1.131 mujeres para que el FRAX pueda ser recalculado con la inclusión de la densidad ósea del cuello femoral. Con el umbral híbrido, otras 170 mujeres fueron elegibles para tratamiento y la medición de la densidad ósea se recomendó a 1.218 mujeres.
ConclusionesEl umbral híbrido identifica a más mujeres elegibles para tratamiento que los umbrales específicos de la edad. Aunque estos últimos identifican a las mujeres con mayor riesgo de fractura, el menor número de mujeres identificadas resulta en menos casos de fractura identificados.
A wide range of treatments is available that improve bone mass and decrease the risk of fractures associated with osteoporosis.1 The use of such interventions by health care practitioners is assisted by instruments that assess patients’ fracture risk to optimize clinical decisions about prevention and treatment. The most widely used web-based tool FRAX® (https://www.sheffield.ac.uk/FRAX/) meets these requirements and computes the 10-year probability of fragility fractures based on several common clinical risk factors and, optionally, a bone densitometry result obtained from dual X-ray absorptiometry (DXA).2,3 FRAX models are available for 73 countries covering more than 80% of the world population at risk4 and have been incorporated into more than 100 guidelines worldwide.5
The adoption of FRAX demands the development of intervention thresholds, namely the fracture probability above which treatment should be recommended. Many different approaches to intervention thresholds have been adopted but in those countries where FRAX rather than BMD is used as a gateway to patient assessment, age-specific thresholds are widely used1,5–7 based on criteria originally developed by the National Osteoporosis Guideline Group (NOGG) in the UK.8,9 More recently NOGG modified their age-dependent intervention thresholds and now use a ‘hybrid’ threshold where the intervention threshold is constant from the age of 70 years.10,11
A country specific FRAX model was developed for Ecuador in 2012, subsequently updated with the availability of more recent epidemiology of hip fracture and death.12,13 The aim of the present study was to explore potential assessment pathways for treatment and characteristics of women selected for treatment in Ecuador based on FRAX using either an age-specific intervention threshold or a hybrid threshold.
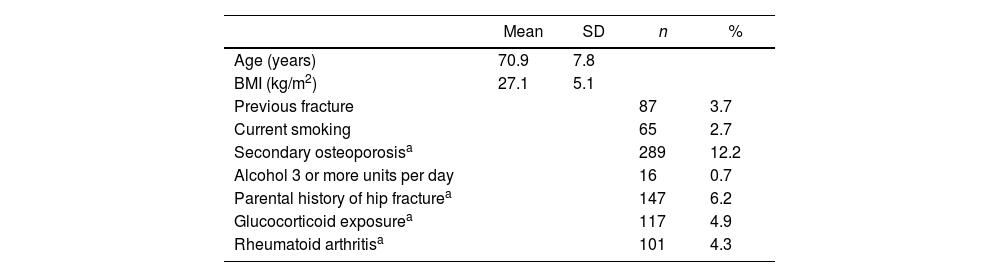
MethodsPopulation sampleThis study used data from 2370 women age 60 years or more in the SABE survey (National Survey of Health, Wellbeing, and Aging)14 residing in the Andes and the coast of Ecuador. The SABE survey was conducted in the continental regions of Ecuador (only the island territory and Amazon was excluded because of its lower population density, 4.4%), therefore it is a representative sample of the Ecuadorian population. This survey is a probability sample of households with a least one person aged 60 years or older residing in the Andes Mountains and coastal regions of Ecuador. In the primary sampling stage, a total of 317 sectors from rural areas (<2000 inhabitants) and 547 sectors from urban areas of the country were selected from the 2001 population Census cartography. In the secondary sampling stage, 18 households within each sector were randomly selected based on the assumption that at least one person aged 60 years or older live in 24% and 23% of the households along the coast and Andes Mountains region, respectively. Between April and August 2010, participants underwent biochemical evaluation to determine their metabolic risk factors. Survey data and methodology, including operation manuals are publicly available.14
A structured questionnaire was used to collect information from all participants and used to provide risk variables for the calculation of FRAX probabilities in the absence of bone mineral density (BMD). Age and sex were self-reported by survey participants. Body height in centimeters and weight in kilograms were measured and the body mass index was calculated (kg/m2).
Smoking was classified as current, former, and never. Average alcohol consumption per week during the previous three months was classified as none, one day, or two or more days per week. Participants self-reported forearm and hip fractures in the past year. The SABE survey questioned participants; Has he/she fallen in the last year?, Did he suffer a fracture when he/she fell?, In the last year he fractured his hip?, In the last year, he/she fracture his wrist?, so we assumed it was frailty fractures. The SABE survey did not collect data on the long-term use of glucocorticoids, family history of hip fractures, or secondary osteoporosis. These missing data were simulated. In a sensitivity analysis, missing data were coded as a ‘no’ response to determine the impact of missing variables on fracture probability.
Simulation of variablesData from the derivation cohorts used to synthesize FRAX were used to simulate missing values. Logistic regression equations were identified to generate data for the dichotomous FRAX variables as described previously.15–17 The equations were applied to the data in the cohort to predict the probability of having a positive value for the missing key risk factor for each individual. Next, a random number was generated using a computer program, which was then compared with the predicted probability for that variable for that individual. If the random number was less than or equal to the predicted probability, the individual was assigned a positive response for the risk factor. If the random number was larger than the predicted probability, the person was assigned a negative response for the risk factor.
Fracture probabilitiesThe 10-year probabilities of hip fracture and a major osteoporotic fracture (clinical spine, hip, humerus or distal forearm fracture) were calculated using the FRAX model for Ecuador (version 4.1). Calculations were undertaken without the inclusion of femoral neck BMD. The upper age limit for the calculation of FRAX probabilities is 90 years. FRAX estimates for women age greater than 90 years was set at 90 (28 women).
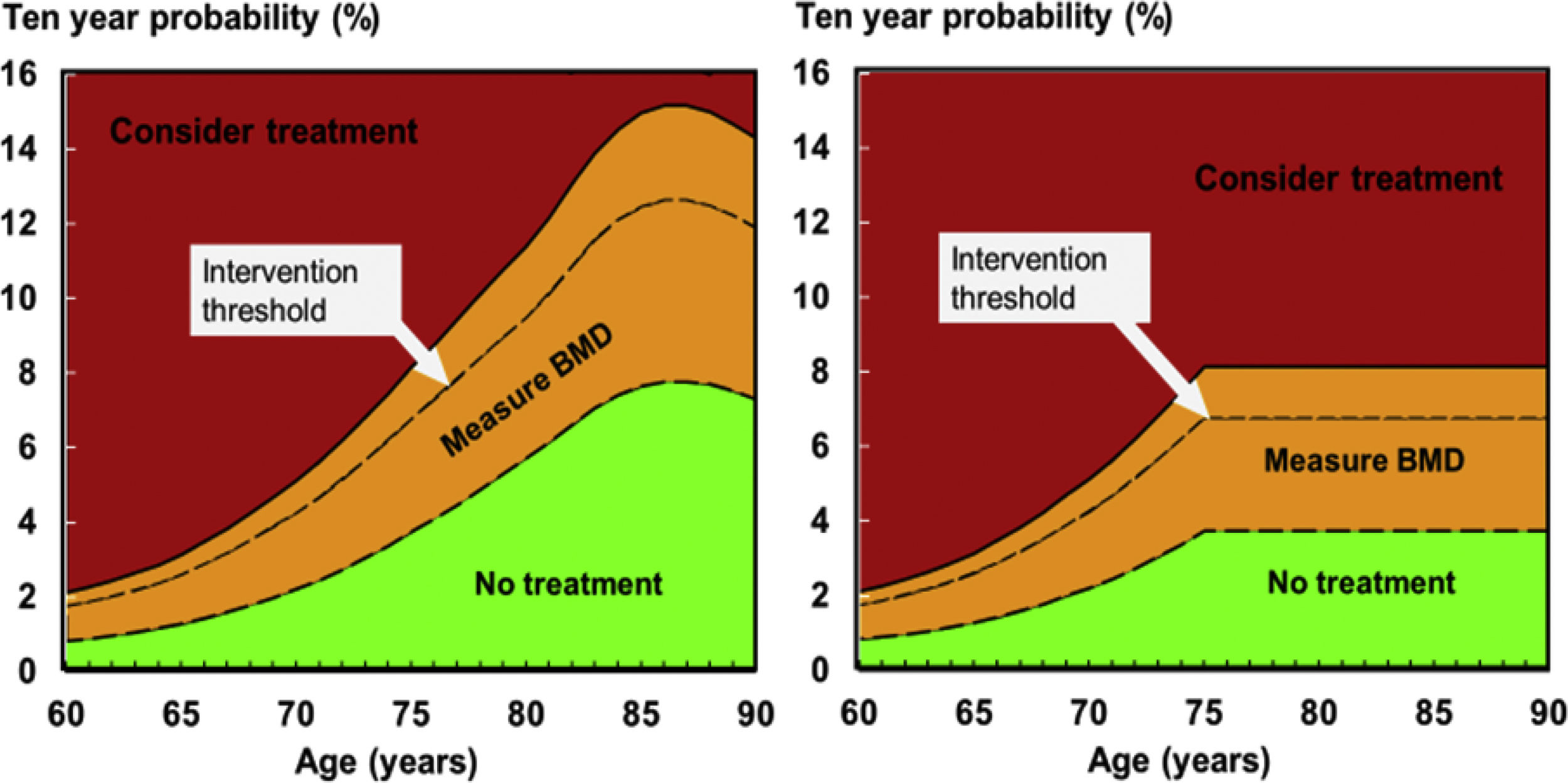
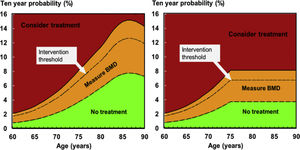
Intervention thresholds based on FRAXTwo intervention thresholds were explored: an age-specific threshold and a hybrid threshold, shown in Fig. 1.
- a.
Age-specific thresholds
Graphs of intervention and assessment thresholds showing the original (left) and current (right) NOGG thresholds applied to the FRAX model for Ecuador. The dotted line represents the intervention threshold while the assessment thresholds enclose the amber area (see text for details).
Many guidelines recommend that postmenopausal women with a prior fragility fracture may be considered for intervention without the necessity for a BMD test (other than to monitor treatment).5,7,9,19 Given that a prior fracture was considered to carry a sufficient risk to recommend treatment, the intervention threshold in women without a prior fracture can be set at the age-specific 10-year probability of a major fracture (hip, spine, forearm or humerus) equivalent to women with a prior fragility fracture. The approach, originally developed for NOGG,8 has been widely adopted.1,5,7,9 The same approach was used in the present study using the Ecuadorian FRAX model. Body mass index was set at 25kg/m2.
- b.
Hybrid threshold
With age-specific thresholds, inequalities in access to therapy arose in the original NOGG guidelines especially at older ages (≥70 years) depending on the presence or absence of a prior fracture. An alternative threshold (a fixed threshold from the age of 70 years) reduced this disparity, increased treatment access and decrease the need for bone densitometry.11 This ‘hybrid’ threshold that combined age-dependent thresholds up to age 70 years and thereafter a fixed threshold with a single probability of fracture was subsequently adopted by NOGG.10 In the present study, the same approach was used using the Ecuadorian FRAX model but with a fixed threshold from the age of 75 years.
Assessment thresholds for BMD testingAssessment thresholds for making recommendations for the measurement of BMD followed the approach of the UK and European guidelines.5,7,8 The two thresholds comprised:
A threshold probability below which neither treatment nor a BMD test should be considered (lower assessment threshold).
A threshold probability above which treatment may be recommended irrespective of BMD (upper assessment threshold).
The lower assessment threshold was set to exclude a requirement for BMD testing in women without clinical risk factors, as given in current European guidelines.1,7 It was therefore set to the age-specific 10-year probability of a major fracture equivalent to women with no clinical risk factors. An upper threshold was chosen to minimize the probability that an individual, characterized to be at high risk using clinical risk factors alone, would be reclassified to be at low risk with additional information on BMD and vice versa.20 The upper assessment threshold was set at 1.2 times the intervention threshold.
Assessment strategyAs noted above, women with a prior fragility fracture were considered to be eligible for treatment without the need for further assessment. In women without a previous fragility fracture, the management strategy was based on the assessment of the 10-year probability of a major osteoporotic fracture (MOF; clinical spine, hip, forearm or humerus). Women with probabilities below the lower assessment threshold were not considered eligible for treatment. Women with probabilities above the upper assessment threshold were eligible for treatment. Women with probabilities between the upper and lower assessment thresholds were to be referred for BMD measurements and their fracture probability reassessed.
Where BMD is not available, FRAX can be used for the assessment of fracture probability. The performance characteristics of FRAX without BMD are approximately equal to BMD without FRAX.21 Assessment strategies were additionally examined in the absence of BMD.
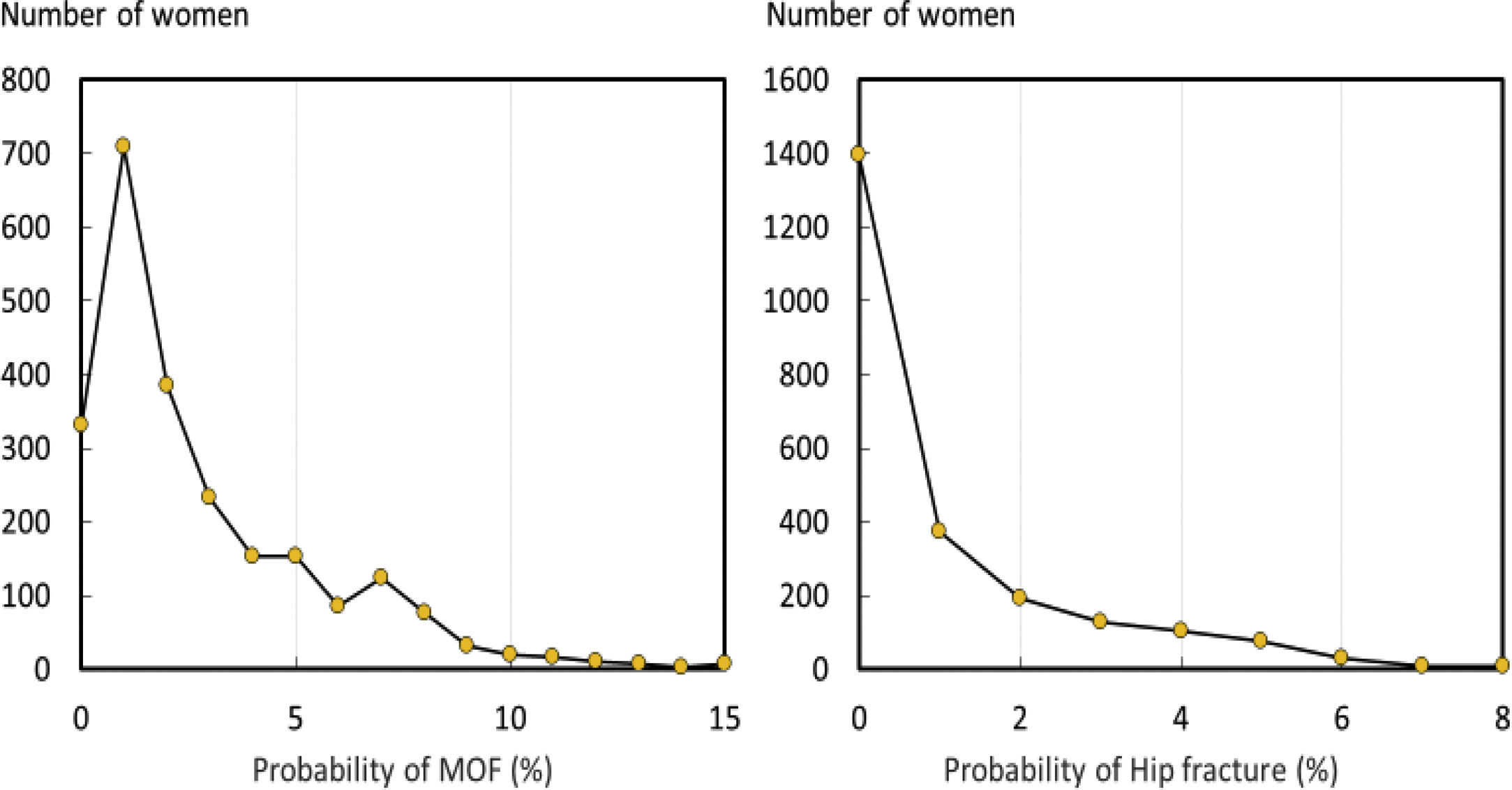
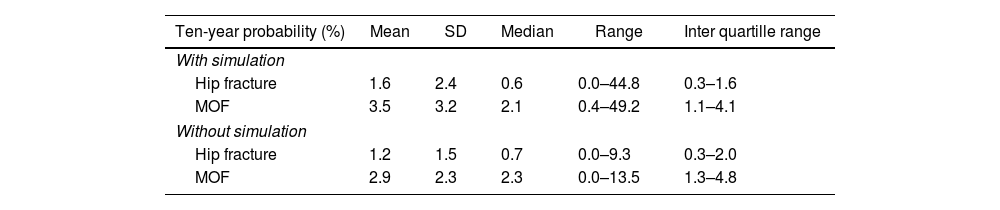
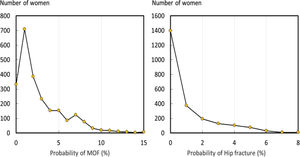
ResultsThe baseline characteristics are given in Table 1. The ten-year probability of MOF and hip fracture (calculated without BMD) is shown in Table 2. The distribution of fracture probabilities was skewed to the left both for MOF and hip fracture (Fig. 2). The effect of simulation uplifted probabilities by more than 20%.
Summary description of the baseline variables in women age 60 years or more (N=2367).
Ten-year probability of fracture of major osteoporotic fracture (MOF) and hip fracture.
| Ten-year probability (%) | Mean | SD | Median | Range | Inter quartille range |
|---|---|---|---|---|---|
| With simulation | |||||
| Hip fracture | 1.6 | 2.4 | 0.6 | 0.0–44.8 | 0.3–1.6 |
| MOF | 3.5 | 3.2 | 2.1 | 0.4–49.2 | 1.1–4.1 |
| Without simulation | |||||
| Hip fracture | 1.2 | 1.5 | 0.7 | 0.0–9.3 | 0.3–2.0 |
| MOF | 2.9 | 2.3 | 2.3 | 0.0–13.5 | 1.3–4.8 |
The intervention threshold in women (set at the age specific fracture probability equivalent to women with a prior fragility fracture) rose with age from a 10-year probability of 1.8% at the age of 60 years to 12.5% at the age of 85 years (Supp Table 1 and Fig. 1). At older ages, the intervention threshold decreased due to the competing effect of mortality.
Supp Table 1 and Fig. 1 also give the age-specific upper and lower assessment thresholds for recommending the measurement of BMD in the assessment of fracture probability. At the age of 65 years, for example, a BMD test would not be recommended in an individual with a fracture probability below 1.3%. At the same age, a BMD test would be recommended with a fracture probability that lay between 1.3 and 3.1%. Treatment would be recommended without the requirement of a BMD test (for fracture risk assessment, though possibly for monitoring of treatment) in individuals with a fracture probability that exceeded 3.1%. In women in whom a BMD test was undertaken, treatment would be recommended in those with a fracture probability that was 2.6% or greater.
Management pathwaySuppl Fig. 1 shows the distribution of 10-year probabilities of a major osteoporotic fracture set against age-specific thresholds. 87 women (3.7%) had a prior fracture and would thus be eligible for treatment. 1131 women (47.8%) had probabilities above the lower assessment threshold but below the upper assessment threshold, so that a BMD test would be recommended. Treatment without the necessity for a BMD test could be recommended in 49 women (2.1%).
In the case of using a hybrid threshold, 87 women (3.7%) had a prior fracture and would thus be eligible for treatment. 1218 women (51.4%) had probabilities above the lower assessment threshold but below the upper assessment threshold, so that a BMD test would be recommended. Treatment without the necessity for a BMD test could be recommended in 170 women (7.2%).
If treatment was allocated solely of FRAX without BMD (excluding those with a prior fracture), the number of women eligible for treatment was 111 with an age-specific intervention threshold and 354 with the hybrid threshold.
The disposition of the various scenarios is shown in Fig. 3. The hybrid threshold allocated substantially more women to treatment than the age-specific threshold.
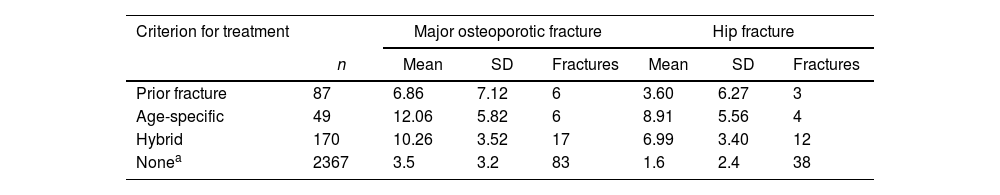
Table 3 gives the fracture probabilities in women eligible for treatment according to the categorisation. Fracture probabilities were highest in those eligible for treatment on the basis of age-specific thresholds, intermediate with the hybrid threshold and lowest in those with a prior fracture. The table also provides the number of fractures expected in each category. Including those with a prior fracture, the age-specific threshold would identify 12 women who would sustain a MOF in the next 10 years including 7 hip fractures. The hybrid threshold would identify 23 women who would sustain a MOF in the next 10 years including 15 hip fractures.
Ten-year fracture probabilities (%) in women eligible for treatment according to the criteria shown. The columns headed fractures denote the number of patients sustaining a MOF or hip fracture over 10 years.
| Criterion for treatment | Major osteoporotic fracture | Hip fracture | |||||
|---|---|---|---|---|---|---|---|
| n | Mean | SD | Fractures | Mean | SD | Fractures | |
| Prior fracture | 87 | 6.86 | 7.12 | 6 | 3.60 | 6.27 | 3 |
| Age-specific | 49 | 12.06 | 5.82 | 6 | 8.91 | 5.56 | 4 |
| Hybrid | 170 | 10.26 | 3.52 | 17 | 6.99 | 3.40 | 12 |
| Nonea | 2367 | 3.5 | 3.2 | 83 | 1.6 | 2.4 | 38 |
In this report, we present a method of categorizing women on the basis of fracture probabilities derived from FRAX. The categories identified comprised those women at low risk, those at intermediate risk in whom a BMD test might be recommended, and those eligible for treatment. The triage used was similar to that originally adopted by the National Osteoporosis Guideline Group (NOGG) in the UK and more recently in European guidelines,1,7–9 but applied to the FRAX model for Ecuador. As noted above, the intervention threshold was set at a fracture probability equivalent to a woman of the same age with a prior fragility fracture. The rationale is that if women with a prior fragility fracture are considered eligible for treatment, as commonly considered, then women without fracture but with equivalent probabilities are also eligible for treatment.
The starting point in the assessment of women is the presence of a clinical risk factor that alerts the physician to consider osteoporosis. The opportunistic case finding strategy arises because screening the general population is not widely recommended in Europe, though advocated in North America.18,19 In those eligible for assessment and in common with the NOGG guidelines, we limited the use of BMD testing. Those individuals with fracture probabilities equivalent or lower than women with no clinical risk factors (as used in FRAX) would not be assessed with BMD. At the other extreme, BMD testing was not universally recommended in individuals at high risk. The rationale is that reclassification of risk with the addition of a BMD test (from high risk to low risk and vice versa) is high when fracture probabilities estimated without BMD are close to the intervention threshold but the likelihood of reclassification decreases the further away the probability estimate is from the intervention threshold.20 The approach used has been well validated in the UK and Canada.20,22,23
The attraction of this approach is that this makes efficient use of BMD resources. The strategy implies, however, that patients at high risk, but identified without BMD, would respond to pharmacological intervention. The evidence that such patients respond to treatment is strong.24–27 The principal reason is that BMD values are low in patients identified with FRAX but without a BMD test.
From the present survey, the proportion of the female population potentially eligible for treatment was 5.8 or 10.9% depending on the intervention threshold that was applied (age-specific or hybrid). As would be expected, the proportion of women eligible for treatment was higher with the application of the hybrid thresholds. The proportion of women who would ultimately be treated would be higher. Approximately 50% of women would be recommended for a BMD test and an uncertain proportion of these would have fracture probabilities above the intervention threshold and be eligible, therefore, for treatment. The uncertainty arises because BMD was not measured in this population sample.
It should be noted that, where facilities for BMD testing are limited, FRAX can be used without BMD. The performance characteristics of FRAX without BMD are approximately equivalent to BMD without FRAX.21 When applied to women in the present study, those eligible for treatment increased by 46 or 71% depending whether the age-specific or hybrid threshold was used.
The implementation of these thresholds is expected to avoid unnecessary treatment of individuals at low fracture risk and direct treatments to those at high risk but there are a number of limitations of the present study to consider. First, the cohort itself had missing variables for the calculation of FRAX which were simulated. Simulation creates some uncertainty with regard to individual probabilities but improves the population estimate. Indeed, the quantum of effect of simulation on fracture probabilities was sufficiently marked that without it the treatment pathway could not have been assessed. Several of the other FRAX variables provided limited information particularly the history of prior fracture. This was limited to hip and forearm fractures in the previous year and would thus underestimate the prevalence of prior fragility fracture and hence, the proportion of women eligible for treatment on this basis. The approach to intervention thresholds is based on the principles of case finding and does not consider a health economic perspective. Although the approach has been shown to be cost-effective in a UK setting,28 cost-effectiveness will necessarily differ in Ecuador because of different fracture risks and cost. It will be important, therefore, to underpin these approaches to fracture risk assessment with an economic assessment.
ConclusionThe present study has shown that it is possible to apply FRAX-based assessment guidelines using the same principles that have been applied to guidelines elsewhere but tailored to the epidemiology of Ecuador. The hybrid threshold identifies more women eligible for treatment than age-specific thresholds. Although age-specific thresholds identify women at higher risk of fracture, the lower number of women identified results in fewer identified fracture cases.
FundingNone.
Conflict of interestThe authors declare no conflict of interests.
The Author wishes to thank ENAGO for professional academic English proofreading.