A 52-year-old male presented with pain and induration of the skin and muscles. Physical examination revealed swelling and induration of the skin and muscles of the arms, forearms, hands, thorax, abdomen, and legs, accompanied by the characteristic orange peel appearance. In addition to bilateral hearing impairment, there was enlargement of both lacrimal glands. Laboratory results revealed hyper-eosinophilia, elevated C-reactive protein, and erythrocyte sedimentation rate, hypocomplementaemia, polyclonal hypergammaglobulinaemia, elevated IgE, IgG, and increased IgG1 and IgG4. MRI of the lower limbs reported enhanced contrast in the muscles of both thighs with thickening of the semimembranosus vastus lateralis fascia and arms. A skin and fascia biopsy indicated lymphoplasmacytic infiltrate, eosinophils, and non-storiform fibrosis. Immunohistochemistry showed IgG4 positivity in less than 10%, with an IgG4/lgG range of less than 40%. The patient meets the criteria for eosinophilic fasciitis and ACR/EULAR criteria for IgG4-RD. For this reason, we would like to report the first case found of eosinophilic fasciitis associated with IgG4-RD.
Varón de 52 años que presenta dolor e induración de piel y músculos. Al examen físico se constata tumefacción e induración de piel y músculos de brazos, antebrazos, manos, tórax, abdomen y piernas, acompañado del característico aspecto de piel en cascara de naranja. Además de la disminución bilateral de la audición, presenta un aumento de ambas glándulas lagrimales. En el laboratorio presentó dos registros de hipereosinofilia (26%), aumento de proteína C reactiva y eritrosedimentación, hipocomplementemia, hipergammaglobulinemia policlonal, aumento de IgE, IgG y aumento de IgG1 y IgG4. La RM de miembros inferiores informa realce del contraste en los músculos de ambos muslos, con engrosamiento de la fascia del vasto lateral y semimembranoso y brazos. Se realiza biopsia de piel y fascia, la cual reporta infiltrado linfoplasmocitario, eosinófilos y fibrosis no esteliforme. Se solicita inmunohistoquímica, que presenta IgG4 positiva en menos del 10% y un rango IgG4/IgG menor 40%. El paciente cumple criterios para fascitis eosinofílica y criterios ACR/EULAR para ER-IgG4. Por esa razón, nos gustaría reportar el primer caso encontrado de asociación de fascitis eosinofílica con enfermedad relacionada con IgG4.
We have read with special interest the publication by Morf et al., where the authors described a patient's case of isolated fasciitis related to IgG4, presenting symptoms of pain, induration, and swelling in the right thigh. Symptoms had developed abruptly and progressed over a three-months period. The serum IgG4 level was elevated.
Magnetic resonance imaging (MRI) of both legs revealed fasciitis affecting the entire right hamstring muscle group, with fascial thickening and contrast enhancement, and an extension of the inflammatory reaction to the semitendinosus muscle near the fascia. The myofascial histological examination of the affected region showed a diffuse chronic, lymphoplasmacytic infiltrate with areas of acute inflammation and storiform fibrosis. Immunohistochemistry shows immunohistochemistry shows an IgG4/IgG ratio of 100%. Consequently, this is the first case described of isolated fasciitis, in an IgG4-related disease (IgG4-RD).1
To recognize that an organ or illness is related to IgG4-RD, it must have a minimum of 5 reported cases of such involvement before that organ can be considered part of the spectrum of IgG4-RD.
For this reason, in order to consider a previously unrecognized organ or site as involved in IgG4-RD, it is recommended that the following criteria be met: (1) histopathologic features findings with elevated IgG4 plasma cells and an increased IgG4/IgG ratio, (2) elevated serum concentrations of IgG4, (3) an effective response to glucocorticoid therapy, and 4-a report of another organ involvement that is consistent with IgG4-related disease. For this reason, we would like to report the first case found of association of eosinophilic fasciitis with IgG4-RD.2
DescriptionA 52-year-old male hypertensive patient presented with pain and induration of the skin and muscles in both arms, legs, thorax and abdomen respecting the face, accompanied by pruritus and stiffness in movement, myalgias and arthralgias. These symptoms had been present for about 6 months and had a sudden onset. They progressed over the following 3 months, during which time the patient developed bilateral hearing loss. Physical examination revealed swelling and induration of the skin and muscles of the arms, forearms, hands, thorax, abdomen, and legs, accompanied by the characteristic orange peel appearance and hyperalgesia.
In addition to bilateral hearing impairment, there is an enlargement of both lacrimal glands. The remainder of the physical examination was normal (no hair loss, malar rash, oral and nasal ulcers, arthritis, telangiectasias, Raynaud's phenomenon nor dysphagia). Laboratory results revealed two instances of hyper-eosinophilia (26%), elevated C-reactive protein 24mg/dL (nv: up to 6mg/dL), and an erythrocyte sedimentation rate of 56mm (nv: up to 15mm/h). Additionally, there was hypocomplementemia (C3: 12 and C4: 26), polyclonal hypergammaglobulinemia, elevated IgA 590 (nv: 70–400mg/dl), IgE 432.7 (nv: 0–100UI/ml), IgG 2306 (nv: 580–1822), and increased IgG subclasses: IgG1 14000g/L (nv: 4.05–10.11g/L), IgG4 7.73g/L (nv: 0.03–2.01g/L).
The rest of the laboratory results were normal, including antinuclear antibodies (ANA), anti-dsDNA antibodies, antibodies to extractable nuclear antigens (ENA), anti-Centromere, anti-Scl 70, IgM and subclasses IgG2, IG3. Electromyography of the four limbs was performed and was found to be normal. Audiometry reported bilateral sensorineural hearing loss, predominantly on the left. 18F-fluorodeoxyglucose (FDG)-PET-CT was requested, reporting cutaneous/subcutaneous increased uptake thickening in the lateral region of the right thorax and thinner face of the proximal third of both thighs, thorax, abdomen and pelvis, with less increased uptoke thickening compared to the previous findings. There were also air trapping areas in the right lower lobe and peribranchial thickening.
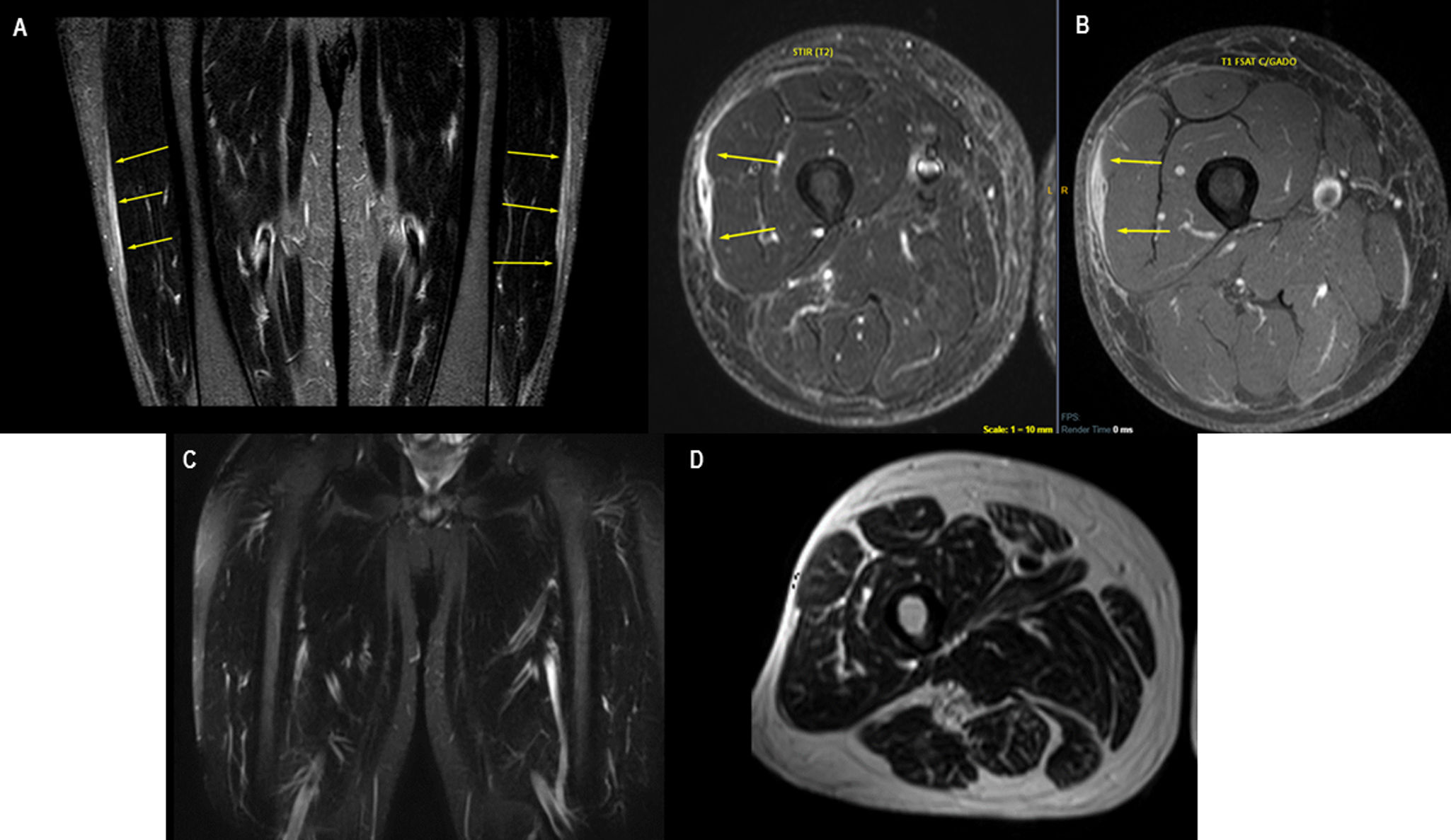
An MRI of the lower limbs was conducted reporting an enhanced contrast in the muscles of both thighs with thickening of the semimembranosus vastus lateralis fascia and arms (Fig. 1A, B). A skin and fascia biopsy were performed, indicating a lymphoplasmacytic infiltrate, abundant eosinophils, and non-storiform fibrosis. An immunohistochemical was requested, and it reported IgG4 positivity in less than 10%, with an IgG4/lgG range of less than 40%. The patient meets the criteria for eosinophilic fasciitis and ACR/EULAR criteria for IgG4-RD (the sum score of all domains and items would be 31).
MRI findings. (A, B) MRI FIRST: Peri muscular fascia thickening overlying the vastus lateralis as well as the posterior thigh group. Such thickening shows post-contrast enhancement, also involving the semimembranosus muscle, the long head of the biceps, and, to a lesser extent, the semitendinosus. The coronal plane displays lateral fascial thickening and enhancement similar to the contralateral thigh. These findings suggest inflammatory fasciitis. (C, D) MRI CONTROL: total remission of the thickening and edema that once affected the fascia of the muscles of both thighs.
Final diagnosis: Eosinophilic fasciitis associated with IgG4-related disease. Treatment was started with corticosteroid pulses 1g/day for 3 days and then prednisolone 1mg/kg/day for one month, in descending doses, methotrexate 15mg/weekly, folic acid and cyclophosphamide pulses 1g monthly for 6 months. The report of the second MRI showed total remission of the thickening and edema that once affected the fascia of the muscles of both thighs (Fig. 1B, C). The patient's symptoms improved, and the serum IgG4 levels returned to normal values.
DiscussionIgG4-related disease was not recognized as a systemic condition until 2003, when extra-pancreatic manifestations were identified in patients with autoimmune pancreatitis. It has been described in practically all organ systems: the biliary tree, salivary glands, periorbital tissues, kidneys, lungs, lymph nodes, meninges, aorta, breast, prostate, thyroid, pericardium and skin. Much is still unknown about IgG4-RD, including its natural history, pathophysiological mechanism, the exact role of IgG4, and the manifestations in individual organs. However, it is clear that IgG4-RD can affect virtually any organ, and that prompt recognition and management of the disease are necessary to prevent sclerotic changes and irreversible organ damage.3
Similar to the first case isolated fasciitis or similar to the first Morf case described, this patient's fascial involvement, according to IgG4-RD histologic criteria, would also be classified as “histologically highly suggestive”.4 The latter also exhibits other alterations related to IgG4-RD, such as enlargement of both lacrimal glands, bilateral sensorineural hypoacusis, peribranchial thickening on CT scan, elevated serum IgG4 levels (greater than 5 times normal), hypocomplementemia, polyclonal hypergammaglobulinemia and elevated serum IgE, along with the characteristic anatomopathological and immunohistochemical alterations.
As per the ACR criteria, we were unable to find clinical, serologic, radiologic, or pathologic evidence of any other underlying autoimmune or malignant condition outlined within the exclusion criteria. Nevertheless, the patient also fulfills the classification criteria for eosinophilic fasciitis, characterized by symmetrical swelling, induration, and thickening in all four limbs. The fascia biopsy reveals fibrosis of the subcutaneous connective tissue, along with thickening of the fascia and infiltration of eosinophils and monocytes and/or thickening of the fascia by imaging tests such as MRI.
In conclusion, our patient would be the first report of eosinophilic fasciitis associated with IgG4-RD.2,5
Ethical considerationsWritten informed consent was obtained from the patients who participated in this study.
FundingNo specific funding was received from any bodies in the public, commercial or not-for-profit sectors to carry out the work described in this article.
Conflict of interestNone.