Involvement of the cervical spine in rheumatoid arthritis (RA) is frequent and it usually occurs in longstanding disease. Cervical spine involvement as an initial manifestation of the disease is rarely described.
Case descriptionA 64-year-old patient complaining of inflammatory neck pain. The physical examination was normal apart from pressure pain at the cervical spine. MRI showed an atlantoaxial subluxation and odontoid process inflammatory pannus. Rheumatoid factor and anti-citrullinated peptide antibody were positive. RA was therefore suspected. Ultrasound of the hands confirmed the diagnosis.
ConclusionsThe physician must be aware of atypical presentations of RA because of their potential risk.
La afectación de la columna cervical en la artritis reumatoide (AR) es frecuente y suele ocurrir en la enfermedad de larga evolución. Rara vez se describe la afectación de la columna cervical como manifestación inicial de la enfermedad.
Descripción del casoPaciente de 64 años con dolor de cuello inflamatorio. El examen físico fue normal, salvo dolor por presión en la columna cervical. La resonancia magnética mostró subluxación atlantoaxial y pannus inflamatorio del proceso odontoideo. El factor reumatoide y el anticuerpo antipéptido citrulinado fueron positivos; por tanto, se sospechó AR. La ecografía de las manos confirmó el diagnóstico.
ConclusionesEl médico debe estar atento a las presentaciones atípicas de la AR debido a su riesgo potencial.
Rheumatoid arthritis (RA) is the most common inflammatory rheumatism, with a prevalence of up to one percent worldwide.1 Indeed, the classical presentation of the disease is generally a bilateral and symmetrical polyarticular involvement affecting small joints of the hand as well as the forefoot.1
Spinal involvement could be observed in RA, particularly after an average of 10 years of disease duration. It is a common event with a prevalence of 14–88%.2,3 This involvement is the third most frequent after that of hands and feet2,3; However it is a very unusual form of RA presentation.4 Atlantoaxial subluxations dominates damage of the upper cervical spine, mainly related to the C1–C2 pannus and the rupture of the transverse ligament. Silent forms are common, but the clinical presentation is very polymorphic and can range from neck pain neglected by the patient to spinal cord compression.3
We underline in this case a cervical spine involvement as a first manifestation in a patient diagnosed with RA. We obtained the patient's consent for the publication of his personal data for scientific purposes.
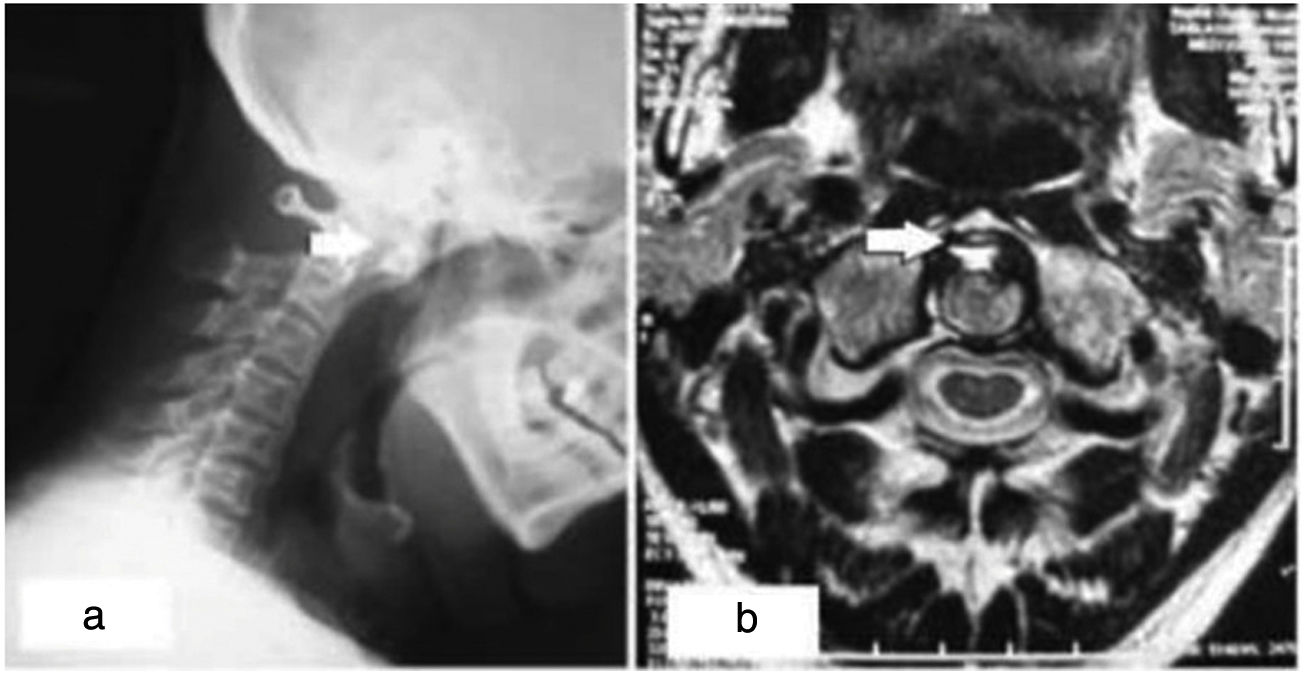
Case descriptionA 64-year-old man with a history of urolithiasis and with no family history of inflammatory rheumatism, was followed in pneumology department for a chronic cough and recurrent bronchitis, diagnosed as diffuse infiltrating pneumopathy. The patient also complained of an eight-year history of isolated inflammatory neck pain which is not improved by paracetamol or rest, but partially improved by non-steroidal drugs. He denied additional musculoskeletal manifestations. Vital signs were normal as well as chest, abdomen and limb examinations. The neck examination was normal apart from pressure pain in the cervical spine. The musculoskeletal examination was without any abnormalities in particular, there were neither synovitis nor pain at the joints pressure. The neurological examination was normal. X ray of the cervical spine showed C1–C2 diastasis and magnetic resonance imaging (MRI) showed a C1–C2 arthritis, an edematous pannus, an atlantoaxial subluxation with a C1–C2 distance at 4.6mm, the absence of basilar impression and the absence of morphological or spinal cord signal abnormality (Fig. 1).
C-reactive protein was 11.1mg/L, rheumatoid factor (RF) and anti-CCP antibodies were strongly positive (318IU/ml and 200U/ml, respectively). The diagnosis of RA was therefore suspected and we performed an ultrasound of the hands and feet which revealed an effusion of the right ankle and a synovial hypertrophy of the metatarsal–tarsal joints of the 1st, 2nd, 3rd and 4th range of the foot. The ultrasound study of the hands did not show synovial involvement.
The patient received intravenous methylprednisolone during the first three days at the dose of 500mg a day. He received methotrexate at a dose of 15mg per week. A suitable cervical collar has been indicated.
A follow-up by MRI after six months showed a steady state of the cervical involovment. The outcome was favourable and the patient reported a decrease in neck pain.
DiscussionThis case represented a diagnostic challenge because the inflammatory pattern of the patient's axial symptoms resembled a spondyloarthritis and his serum inflammatory markers were negative. However, the symmetric involvement of peripheral joints as well as the incomplete response to NSAIDs, the positive RF and anti-CCP raised the suspicion of RA. The earliest and most frequent symptom of cervical involvement in RA is neck pain radiating to the occiput.
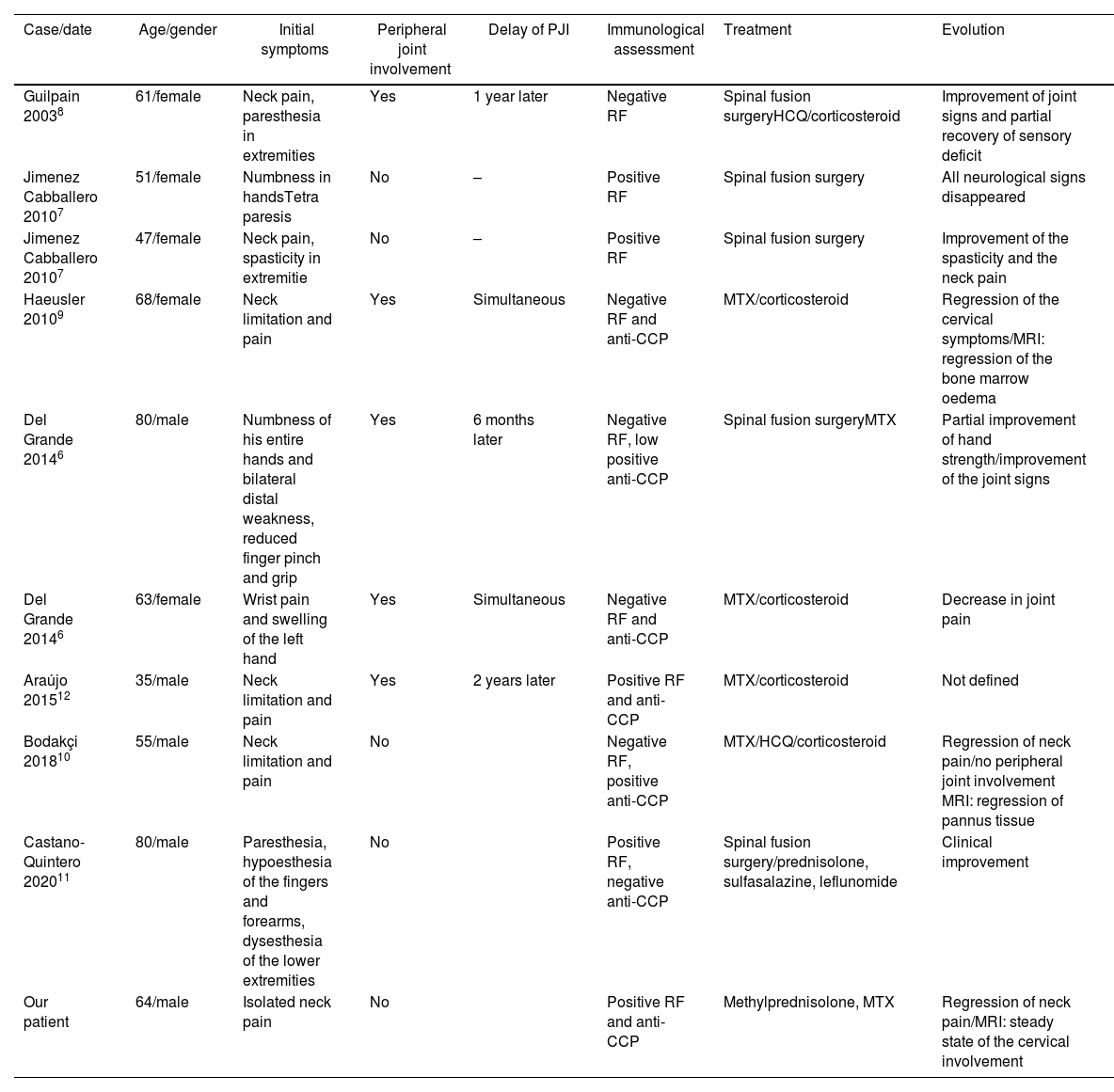
Although cervical spine involvement is a common feature in RA,2,5 it is a very unusual form of presentation of this affection. To our knowledge there are only nine reported cases of cervical involvement as a presenting feature of the disease.6–12 See Table 1.
Characteristics of the different cases of cervical spine involvement reported in the literature.
| Case/date | Age/gender | Initial symptoms | Peripheral joint involvement | Delay of PJI | Immunological assessment | Treatment | Evolution |
|---|---|---|---|---|---|---|---|
| Guilpain 20038 | 61/female | Neck pain, paresthesia in extremities | Yes | 1 year later | Negative RF | Spinal fusion surgeryHCQ/corticosteroid | Improvement of joint signs and partial recovery of sensory deficit |
| Jimenez Cabballero 20107 | 51/female | Numbness in handsTetra paresis | No | – | Positive RF | Spinal fusion surgery | All neurological signs disappeared |
| Jimenez Cabballero 20107 | 47/female | Neck pain, spasticity in extremitie | No | – | Positive RF | Spinal fusion surgery | Improvement of the spasticity and the neck pain |
| Haeusler 20109 | 68/female | Neck limitation and pain | Yes | Simultaneous | Negative RF and anti-CCP | MTX/corticosteroid | Regression of the cervical symptoms/MRI: regression of the bone marrow oedema |
| Del Grande 20146 | 80/male | Numbness of his entire hands and bilateral distal weakness, reduced finger pinch and grip | Yes | 6 months later | Negative RF, low positive anti-CCP | Spinal fusion surgeryMTX | Partial improvement of hand strength/improvement of the joint signs |
| Del Grande 20146 | 63/female | Wrist pain and swelling of the left hand | Yes | Simultaneous | Negative RF and anti-CCP | MTX/corticosteroid | Decrease in joint pain |
| Araújo 201512 | 35/male | Neck limitation and pain | Yes | 2 years later | Positive RF and anti-CCP | MTX/corticosteroid | Not defined |
| Bodakçi 201810 | 55/male | Neck limitation and pain | No | Negative RF, positive anti-CCP | MTX/HCQ/corticosteroid | Regression of neck pain/no peripheral joint involvement MRI: regression of pannus tissue | |
| Castano-Quintero 202011 | 80/male | Paresthesia, hypoesthesia of the fingers and forearms, dysesthesia of the lower extremities | No | Positive RF, negative anti-CCP | Spinal fusion surgery/prednisolone, sulfasalazine, leflunomide | Clinical improvement | |
| Our patient | 64/male | Isolated neck pain | No | Positive RF and anti-CCP | Methylprednisolone, MTX | Regression of neck pain/MRI: steady state of the cervical involvement |
PJI: peripheral joint involvement; PIP: proximal interphalangeal joint; MCP: metacarpophalangeal joint; MTP: metatarsophalangeal joint; RF: rheumatoid factor, anti-CCP anti-cyclic citrullinated peptide; MTX: methotrexate; HCQ: hydroxychloroquine; CT: computerized tomography; MRI: magnetic resonance imaging.
Described cases were six women and four men. Their average age was 57.39 years [35–80]. The main symptom of onset neck pain was reported in six cases. Other symptoms such as tetra paresis, paresthesia, spasticity and numbness of the hands were described. Peripheral joint involvement was present in three cases and immunological assessment was positive in six cases. In all reported cases, MRI was the gold standard for diagnosis. Five patients underwent surgery. Methotrexate, sulfasalazine, hydroxychloroquine, leflunomide and corticosteroid therapy were prescribed with good response.6–12
The involvement of the upper cervical spine, being more frequent than the involvement of the lower cervical vertebrae is dominated by atlantoaxial subluxation. This subluxation can be anterior, lateral, rotatory or posterior. The literature data estimates its prevalence between 52 and 75%.3,13 Among atlantoaxial subluxations, anterior subluxations are the most frequent with a prevalence ranging from 10 to 55%.13
The majority of studies link the occurrence of cervical involvement, especially atlantoaxial subluxation, to a long history of RA.13,14 Its onset mainly occurs after at least 5–10 years of evolution of RA.13 Several factors favouring rheumatoid cervical involvement have been reported in the literature, such as advanced age and duration of disease progression,15 polyarticular involvement13 and deformities.13–15
However, some authors have described earlier cervical involvement.10,16,17 Paimela18 has shown that cervical involvement can begin within the first 2 years of the course of RA. Del Grande has described a 20% prevalence of early cervical involvement.6 Rare case reports have described cases of cervical involvement revealing or preceding peripheral involvement in RA.10,11
A study published in 2020 investigated the link between the Simple Erosion Narrowing Score (SENS score) and cervical injury. SENS score (hand) was used. A total of 32 joints were scored for erosions and 30 for joint space narrowing. A total of 56 patients with RA were evaluated. A correlation between the SENS score of hands and the prevalence of cervical spine subluxation was confirmed. A higher prevalence of cervical spine subluxation correlated with an increase in the SENS score of hands. The erosion and joint space narrowing scores of the hands also correlated with the prevalence of cervical spine subluxation. These scores may be used as a predictor of cervical spine subluxation in RA patients.19
The coexistence of extra-articular manifestations20,21 as well as the presence of clinical and biological activity elements of the disease21 would favour cervical involvement of RA. There is also a relationship between RF and cervical involvement.22 Our patient had no extra-articular manifestations but his RF was strongly positive.
Treatment at an early stage is very important and there is a low incidence of cervical involvement in this case,3 more marked if several DMARDs are combined. A study published in 2000 showed that the combination of several DMARDs (methotrexate, sulfasalazine, nivaquine) reduced the development of rheumatoid cervical damage compared to monotherapy.23
We described the experience of a male patient presenting a vertebral joint inflammatory compromise as the debut manifestation of RA, which is not common. We also summarized cases reported with cervical involvement as presenting manifestation of RA. This may motivate the development of further research aiming to determine the real frequency of this situation and raise awareness to suspect this condition.
Nevertheless, faced to inflammatory neck pain, investigations must be carried out in order to rule out other etiologies, in particular spondyloarthtritis, since C1–C2 involvement could occur during this disease.
ConclusionThe reported case of cervical arthritis, as a presenting feature of RA, corroborates that this is a heterogeneous disease. This suggests that RA may have atypical presentations for which the physician must be aware. Thus, they must investigate any isolated inflammatory cervical spine pain with MRI.
Informed consentAn informend consent was signed by the patient for the publication of his data and images.
Ethical approvalThis manuscript was approved by the ethical committee.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interestAuthors declare having no conflict of interest.