To determine the clinical profile of patients infected with the chikungunya virus.
Materials and methodsDescriptive longitudinal, prospective study on 109 individuals referred to the outpatient or emergency department of the Fundación Hospital Universitario Metropolitano de Barranquilla for serological confirmation, after being previously diagnosed with chikungunya virus infection by rheumatologists from the Rheumatology and Orthopedics Center. Patients with serologically confirmed diagnosis underwent immunological test for differential diagnosis with rheumatoid arthritis.
ResultsELISA test were performed to serologically diagnose chikungunya virus, IgG and IgM antibodies. No chikungunya IgM test was positive, while 109 were positive for chikungunya IgG antibody. The age range was 22–82 years. The main clinical manifestations were: (1) localized pain in the hands: 82%, ankles joints: 82%, feet: 72%, headache 69%, back: 61%, and elbow: 57%. (2) Pain in other joints: 76%, and muscles 72%. (3) Peri-articular swelling: 55%. (4) Other symptoms of clinical interest: cutaneous manifestations: 53%, fever 89%, rash: 5%, nausea 31%, and incapacity: 19%.
ConclusionsMost signs and symptoms presented by patients with chikungunya have an extensive rheumatological component that merits further study. The joint compromise in acute and subacute phase resembles the behavior of rheumatoid arthritis, but not so similarly in the chronic phase. There was no autoimmune reaction, and therefore cannot be classified as a type of Rheumatoid process.
Caracterizar clínicamente una población infectada con el virus chikungunya.
Materiales y métodosEstudio descriptivo longitudinal, prospectivo con 109 pacientes remitidos a consulta externa o urgencia, de la Fundación Hospital Universitario Metropolitano de Barranquilla, para realizar confirmación serológica, previo diagnóstico clínico de infección por virus chikungunya, por reumatólogos del Centro de Reumatología y Ortopedia. Los pacientes con diagnóstico confirmado serológicamente se sometieron a pruebas inmunológicas para diagnóstico diferencial con artritis reumatoide.
ResultadosSe realizó diagnóstico serológico por ELISA para virus chikungunya anti-IgG y anti-IgM; ninguno resultó positivo para anticuerpo antichikungunya tipo IgM, mientras que 109 fueron positivos para anticuerpo antichikungunya tipo IgG. El rango de edad fue de 22 a 82 años. Las principales manifestaciones clínicas fueron: 1. dolor localizado: manos: 82%, tobillos con afectación articular: 82%, pies: 72%, cabeza: 69%, espalda: 61%, codos: 57%. 2. Dolor en distintas articulaciones: 76%, músculos: 72%. 3. Edema: región periarticular: 55%, 4. Otra sintomatología de interés clínico: manifestaciones cutáneas: 53%, fiebre: 89%, rash: 5%, náuseas: 31% e incapacidad laboral: 19%.
ConclusionesLos signos y síntomas presentados por los sujetos con chikungunya tienen un amplio componente reumatológico. El compromiso articular en las fases agudas y subagudas semeja el comportamiento de la artritis reumatoide, más no así el compromiso en la fase crónica. No hubo reacción autoinmunitaria y por tanto no se puede clasificar como proceso de tipo artritis reumatoide.
The infection with the chikungunya virus (CHIKV) has become a real epidemic in the Colombian Caribbean Region, Barranquilla does not escape from these statistics, and therefore, the concern among the community and the health authorities is notorious. The disease began to be monitored in September 2014 and at the end of this epidemiologic period, in October 4 of that year, 14,936 cases had occurred, figure that by 2015 has been virtually multiplied by 14.1
According to the National Institute of Health, Bolivar is the Department of the Caribbean Region with the greatest number of people diagnosed with CHIKV, with approximately 30,834 cases, surpassing the Departments of Norte de Santander, Tolima, Huila and Sucre. Bolívar is located in the geographical area whereby the virus entered the country in 2014 and in which it has expanded from North to South and from East to West.2
The Ministry of Health and Social Protection, in the first phase of attack of the virus, projected that between 900,000 and 1,000,000 people would be affected in the country, being currently calculated in 200,000 the cases of CHIKV, with the aggravating factor that the joint pain that characterize the clinical picture of the disease has become a major health problem due to the high demand for medical care and analgesics.3
In recent publications is shown that between 88 and 100% of the people present some articular involvement, calculating among them, that when the acute phase is over, 30% remain with periodic or permanent joint pain, whose duration is estimated between 3 and 5 years after the infection, remaining between 10 and 12% with sequelae.4
The CHIKV fever is transmitted to the human by the bite of a vector infected with CHIKV. These transmitter vectors are the same mosquitoes (Aedes aegypti, Aedes albopictus) involved in the transmission of the dengue.5
A variable number of clinical manifestations associated with the CHKV infection can be described as an autoimmune or rheumatic affection, or can be attributable to infectious diseases such as: dengue, malaria and yellow fever, among others. Therefore, in areas of high distribution of the vector, such as the Caribbean region, it is important to consider the differential diagnosis between CHIKV fever and dengue, in patients who exhibit not-well defined rheumatologic pictures.5
The manifestations of chikungunya fever, during the acute phase (0–10 days), are characterized by fever of sudden onset higher than 38.5°C, exanthemas and presence of intense arthralgias. These symptoms usually resolve in 7–10 days, although a significant percentage of patients have relapses with rheumatoid symptoms (polyarthralgias, polyarthritis, tenosynovitis, Raynaud's syndrome), several months of years after the initial disease. Approximately 30% of the infected people manifest these long-term sequelae.4
The multiple joints involvement affects between 70 and 100% of patients. It is usually symmetric and affects the small joints of the hands and feet, although occasionally it attacks large joints of the limbs. It can be limited to arthralgia or joint tumefaction may occur, frequently due to tenosynovitis. The combination of joint pain, tenderness, inflammation and stiffness is usually very disabling and incapacitates many patients who are confined to bed during the acute period.5,6
Two to five days after the onset of fever, 50% of patients develop a maculopapular or occasionally petechial exanthema, which affects the trunk and less frequently the extremities and it may extend to the palms, the soles and the face. The exanthema tends to be fleeting, although it persists for more than 2 days in 10% of cases; it occasionally appears as a diffuse erythema that pales under pressure. 25% of adults suffer stomatitis and 15% develop oral ulcers.
In the sub-acute phase, most patients improve after 10 days of illness. However, some patients suffer a recurrence of the articular symptoms 2 or 3 months after the initial recovery, developing arthralgias in areas previously affected, distal polyarthritis and sub-acute hypertrophic tenosynovitis in wrists and ankles. They also can develop Raynaud's syndrome, depression, asthenia and weakness,7 this sub-acute phase of the infection with chikungunya does not persist for more than 3 months and it affects between 43% and 70% of cases.4
During the chronic disease the symptoms persist for more than 3 months, and although it has been described that the percentage of subjects who develop chronic manifestations ranges between 12 and 57%,7 this value tends to resolve over time, since 93% of the cases persist symptomatic after 3 months and this percentage decreases to 57% after 15 months and to 47% 2 years later.7
Exceptionally, severe forms of the disease can occur with atypical manifestations, among which stand out myocarditis, meningoencephalitis and mild bleeding. Guillain–Barre syndrome, loss of hearing acuity, uveitis and retinitis have also been observed,7 and it is rarely lethal, being this condition more frequent in children under one year and in adults older than 65 years with coexisting diseases.
Regarding the influence of factors such as gender and age in the presentation of the disease, it has been observed a higher frequency in men in terms of age, although it can appear at any age,6 its incidence is higher in the group of 20–50 years, with a peak between 30 and 40 years of age.
The signs and symptoms of the CHIKV disease are in many cases non-specific, prevailing among them the joint symptoms, however, the accuracy of the clinical diagnosis is limited, requiring a population screening by the isolated serological measurement, which constitutes the proposed test for the achievement of the diagnostic presumption.
Polyarthralgia has been described in more than 90% of the patients; it normally occurs within few minutes or several hours after the onset of the fever and results in a characteristic stooped posture when walking, which since the decade of the 50s has been recognized as one of the hallmarks of the disease.8
The rheumatic manifestations are fluctuating, symmetric arthritis has been described, but it can be asymmetric or even appear as oligoarthritis or monoarthritis, which mimics rheumatoid arthritis (RA); indeed, Bouquillard and Combe9 reported 21 cases that met the criteria of the American College of Rheumatology for RA after the infection with CHIKV. In addition, mild deformities and limitation of the joint mobility have been described, but joint redness has been uncommon.10 Besides the arthralgia, other rheumatic manifestations have been reported. Pain in the sacroiliac, lumbosacral and cervical vertebral joints has been found in some patients.10
The researches addressed to the study of the coexistence of infection with CHIKV and rheumatic affections, offer new horizons toward the knowledge and understanding of the pathogenesis of both conditions, and possibly responses to the mechanisms of certain autoimmune diseases; as well as new expectations on the immunologic activity of the patients who fully recover from CHKV infection and those who evolve into chronicity.
Because there is no precision in the definition of the signs and symptoms in the CHIKV disease, it is important to inquire exhaustively the status or the characterization of the clinical situation of the patients who acquire or who have the disease; that is why this research arises. The structured knowledge of the health status of the patients affected by the clinical picture of CHIKV and its incidence in the morbidity during the course of the therapy and in their survival can be defined, and intervention strategies can be outlined in the early studies of the disease in order to try to reduce its incidence. Unfortunately, the signs and symptoms of the CHIKV disease sometimes are nonspecific, but with a high prevalence of articular damage, and the accuracy of the clinical diagnosis is limited, and is there when come into play the indications for population screening through the isolated serological measurement, which constitutes, so far, the fundamental test to achieve a diagnostic presumption.
Although the CHIKV disease has been a frequent entity in Barranquilla in the last two years (2014 and 2015), the lack of accurate epidemiological data on this pathology in the Caribbean Coast and, in particular, in our city, encourages the institutions of superior education and researchers to the search of scientific knowledge on the behavior of this pathology, taking into account the quality of life of the subjects and the resulting high costs, since the potential years of life lost can come to represent around 265 per million, which accounted for 69% of these years.11
This study aims to carry out a clinical characterization of a population infected with CHIKV, on their admission to the emergency department of the Fundación Hospital Universitario Metropolitano (FHUM) and the outpatient service of the Rheumatology and Orthopedics Center of Barranquilla.
Materials and methodsA descriptive, longitudinal and prospective study of the cases of CHIKV was conducted in subjects aged between 22 and 82 years, treated during the study period in the FHUM and subsequently referred to the Rheumatology and Orthopedics Center, classified as suspected or confirmed cases of chikungunya (IgG seroconversion, presence of specific IgM). Clinical evaluations were carried out on admission, at 10–20 days, and after 20 days.
A sample calculation was not performed, but all the subjects who met the selection criteria were included. In total 109:
- •
Classified as suspicious case (fever higher than 38.5°C, severe arthralgia or arthritis of acute onset), without other medical condition that explains it.
- •
With increasing concentrations of specific anti-chikungunya IgG detected by ELISA.
- •
With positive results for specific anti-chikungunya IgM detected by ELISA.
- •
With signed informed consent.
Subjects with confirmed diagnosis of rheumatologic disease or positive results for rheumatoid factor, antinuclear antibodies higher than 1/160, ASTO and uric acid were not included; likewise, individuals with presumptive diagnosis, but who finally resulted negative, were excluded.
The medical history recorded the anthropometric characteristics, personal antecedents, vital signs and results of laboratory tests (which are analyzed in other article published in this Journal).
The data collection was carried out using a form designed for this purpose, building a database which allowed to evaluate the different signs and symptoms of the disease such as: pain or swelling in hands, feet, ankles, elbows, arthralgias, myalgias, headache, back pain, periarticular edema, coupled with cutaneous manifestations, fever, rash, nausea and inability to work.
The main information source was of primary order, given that the data were taken from a form designed by the researchers and applied to each patient with their respective laboratory tests, confirming the diagnosis of chikungunya; also, the patients were contacted periodically to follow-up the evolution of the symptoms and determine the phases of development of the disease.
The database allowed to conduct a descriptive and inferential statistical analysis developed based on frequency distributions, arithmetic mean, confidence intervals, and graphics that allowed to analyze the different signs and symptoms and the immunorheumatological implication of the affected patients and their medical follow-up.
On the other hand, the percentages of articular affection in the subjects with CHKV were compared with the percentages of RA taken from the study conducted by Qayyum et al.12
The Standards of Good Clinical Practices in Research were always met, and the patients signed informed consent for their inclusion and the access to their data.
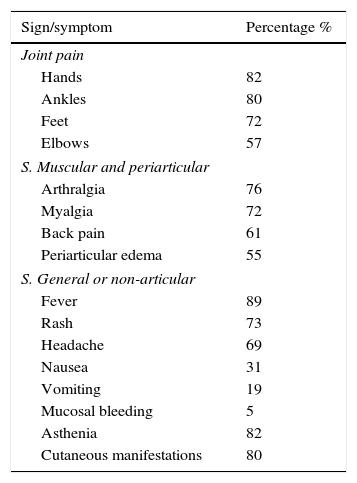
ResultsThe socio-demographic characteristics of the patients are shown in other article published in this Journal by the authors of this one. Regarding the clinical aspects (signs and symptoms), the hands and the ankles exhibited the higher percentage of rheumatologic pain, 82% and 80%, respectively. Patients express in 72% presence of significant pain in the feet and the lowest variation appears in the elbows 57% (Table 1). It should be noted that 89% of the studied patients are women, although the big differences between the percentages make it difficult to carry out comparative analyses.
Signs and symptoms present in the participants.
| Sign/symptom | Percentage % |
|---|---|
| Joint pain | |
| Hands | 82 |
| Ankles | 80 |
| Feet | 72 |
| Elbows | 57 |
| S. Muscular and periarticular | |
| Arthralgia | 76 |
| Myalgia | 72 |
| Back pain | 61 |
| Periarticular edema | 55 |
| S. General or non-articular | |
| Fever | 89 |
| Rash | 73 |
| Headache | 69 |
| Nausea | 31 |
| Vomiting | 19 |
| Mucosal bleeding | 5 |
| Asthenia | 82 |
| Cutaneous manifestations | 80 |
The most frequent muscle and periarticular symptoms are: arthralgia in 76%, followed by myalgia in 72%. Back pain accounts for 61% and slightly more than half of the cases exhibit periarticular edema, 55% (Table 1). The most frequent non-articular general symptoms are: fever 89%, asthenia 82%, cutaneous manifestations 80% (rash 77%) and headache 69%. The less frequent symptoms are: nausea 31%, vomiting 19% and mucosal bleeding 5% (Table 1).
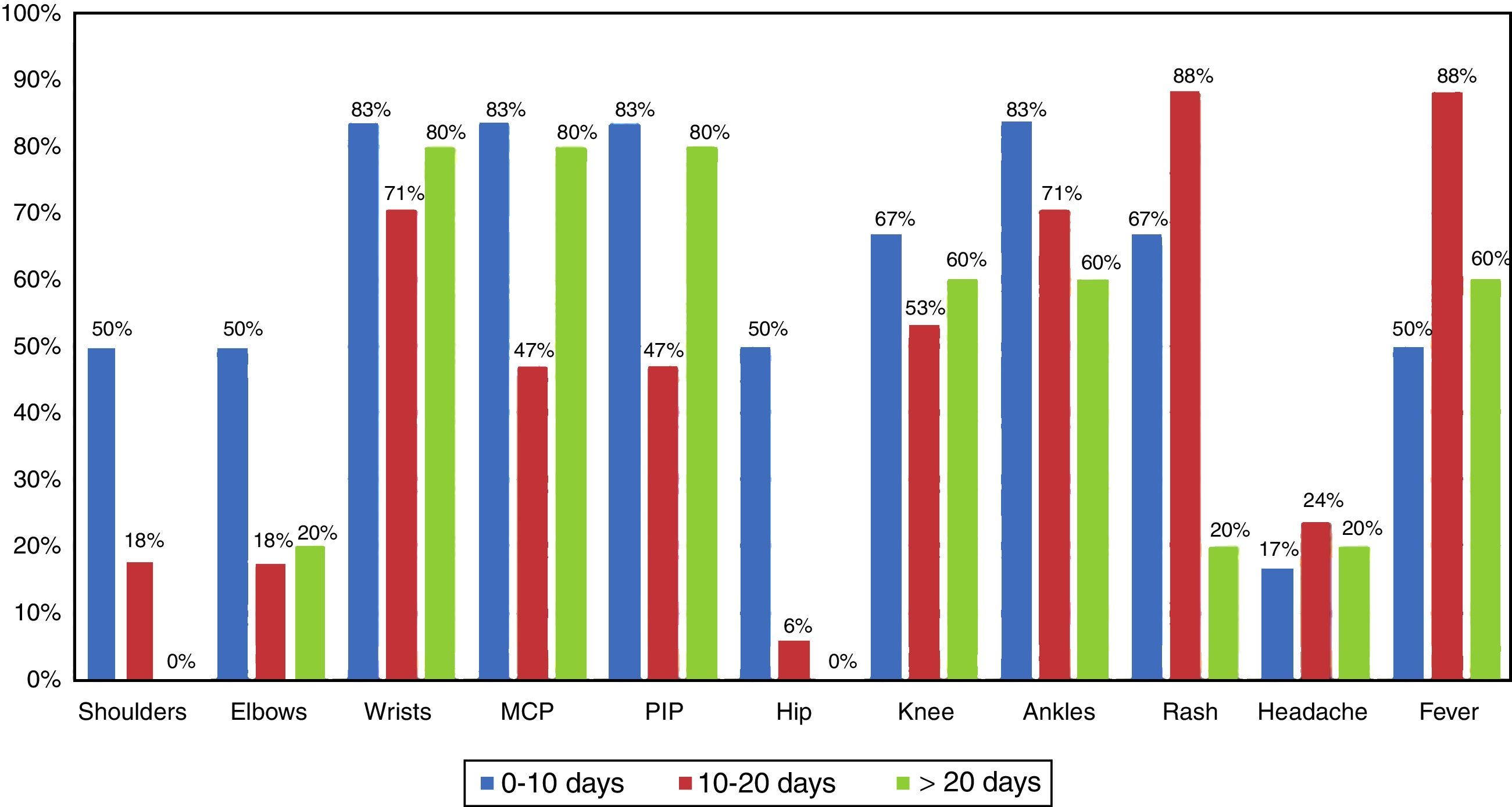
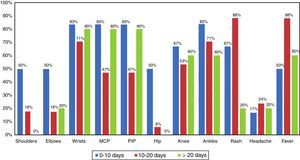
On the other hand, regarding the results of the acute phase, in the patients diagnosed with chikungunya, who make up the sample of this research, it was found that during the first 10 days, most of them (83%) manifested the presence of symmetric pain in wrists, ankles, MCP and PIP joints, followed by symmetric pain in knees and rash in 67%, and in a lower proportion they manifested pain in shoulders, elbows and hips in up to 50%, the fever reached this same percentage. In Fig. 1 is shown that some symptoms were decreasing over time, such as the cases of pain in the shoulders (50% in the first 10 days, 18% between 10 and 20 days, and 0% after 20 days), in the hips (50, 6 and 0%), in the ankles (83, 71 and 65%), while others showed a higher percentage between 10 and 20 days: rash (88%) and fever (86%), and others presented a significant increase after 20 days, following the decrease between 10 and 20 days: pain in the wrists, MCP joints, PIP joints; and knees.
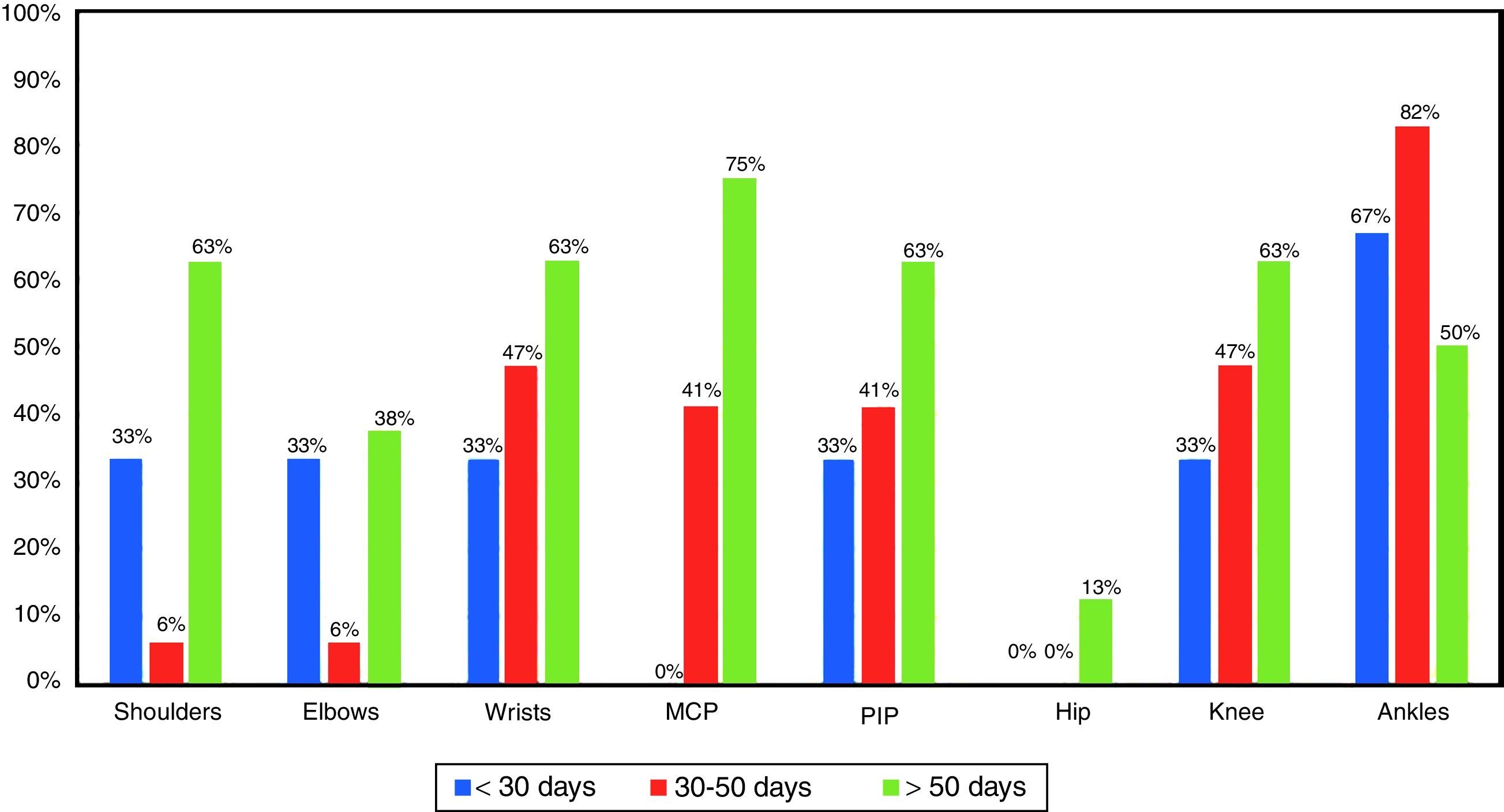
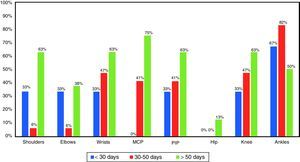
In the period of time between 30 and 50 days of the sub-acute phase, it was observed a marked decrease of the involvement of the shoulders and elbows, both representing 6%, while the wrists and knees decreased to 47%. The affection in the MCP and PIP joints reached 41%, and conversely the manifestations in the ankles increased to 82% (Fig. 2).
As for the period longer than 50 days, it was evidenced an increase in the commitment of all the joints (except the ankles) with respect of what was found in the previous interval of the sub-acute phase. 75% for the MCP joints, and 63% for the shoulders, wrists, PIP, and knees. In the ankles, instead, there was a decrease in symptomatology to 50%. It draws attention, also, that in this stage, longer than 50 days, the affection of the hip appeared again in 13% (Fig. 2).
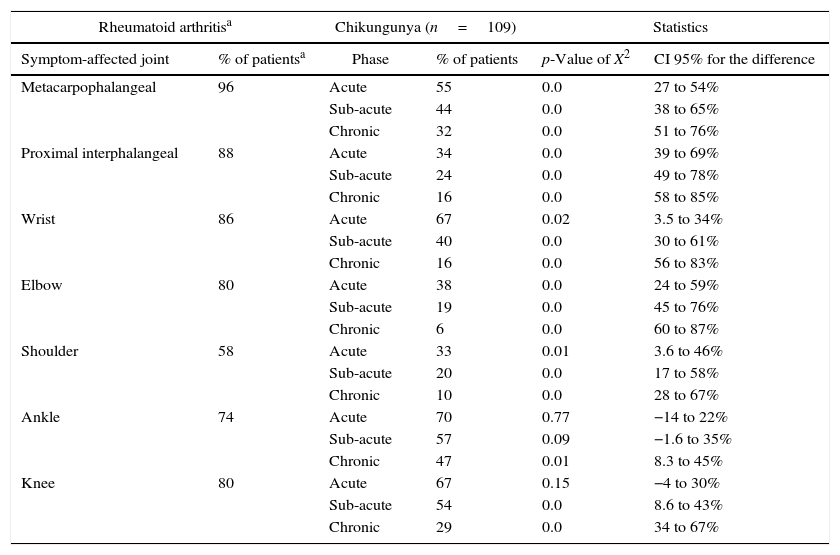
When comparing the symptomatology of the study subjects in each of the phases (acute, sub-acute and chronic) with the classic articular symptoms of RA, it was found that the patients with this pathology have a higher percentage of ailments in the following locations, compared with those with CHKV of the present study in the 3 phases: metacarpophalangeal, proximal interphalangeal, wrist, elbow and shoulder joints (Table 2).
Comparison of classical symptoms of rheumatoid arthritis with articular affection in acute, sub-acute and chronic phases of subjects with chikungunya. Source: Tracking template for laboratory tests results of FHUM.
| Rheumatoid arthritisa | Chikungunya (n=109) | Statistics | |||
|---|---|---|---|---|---|
| Symptom-affected joint | % of patientsa | Phase | % of patients | p-Value of X2 | CI 95% for the difference |
| Metacarpophalangeal | 96 | Acute | 55 | 0.0 | 27 to 54% |
| Sub-acute | 44 | 0.0 | 38 to 65% | ||
| Chronic | 32 | 0.0 | 51 to 76% | ||
| Proximal interphalangeal | 88 | Acute | 34 | 0.0 | 39 to 69% |
| Sub-acute | 24 | 0.0 | 49 to 78% | ||
| Chronic | 16 | 0.0 | 58 to 85% | ||
| Wrist | 86 | Acute | 67 | 0.02 | 3.5 to 34% |
| Sub-acute | 40 | 0.0 | 30 to 61% | ||
| Chronic | 16 | 0.0 | 56 to 83% | ||
| Elbow | 80 | Acute | 38 | 0.0 | 24 to 59% |
| Sub-acute | 19 | 0.0 | 45 to 76% | ||
| Chronic | 6 | 0.0 | 60 to 87% | ||
| Shoulder | 58 | Acute | 33 | 0.01 | 3.6 to 46% |
| Sub-acute | 20 | 0.0 | 17 to 58% | ||
| Chronic | 10 | 0.0 | 28 to 67% | ||
| Ankle | 74 | Acute | 70 | 0.77 | −14 to 22% |
| Sub-acute | 57 | 0.09 | −1.6 to 35% | ||
| Chronic | 47 | 0.01 | 8.3 to 45% | ||
| Knee | 80 | Acute | 67 | 0.15 | −4 to 30% |
| Sub-acute | 54 | 0.0 | 8.6 to 43% | ||
| Chronic | 29 | 0.0 | 34 to 67% | ||
With respect to the pain located in the ankle, no differences were observed between the percentages of patients who suffer from RA and those who suffer from CHKV during the acute and sub-acute phases; whereas in the chronic phase, the percentage of patients with pain in the ankles was higher in patients with RA than in patients with CHKV (Table 2).
Likewise, the patients suffering from RA showed a higher percentage of pain in the knees compared with those with CHKV in the sub-acute and chronic phases, while this percentage of patients with RA and pain in the knees was similar (p>0.05) to the percentage of patients with chikungunya who in the acute phase had pain in these joints (Table 2).
DiscussionIt is noteworthy that 98% of all subjects with clinical suspicion of CHKV to whom serological tests were performed, had a positive result of immunoglobulin G, in addition, it was found that there are no statistically significant differences (p-value of 1.0 in the test of hypothesis of equality of proportions) between the percentages of individuals diagnosed with the disease by applying both methods (clinical and serological), which demonstrates a high potential capacity of the clinical criteria for the description of the disease; these results contrast with a similar study conducted in India, in which the percentage of confirmed cases was less than 50%,13 indicating a high level of immunity in our population. However, being a descriptive study, in which a series of cases is observed, there is an important limitation when trying to indicate causal relationships, for which an analytical study is required.
It can be stated that the symmetrical articular involvement of small joints is very similar to the articular behavior of RA. However, unlike the additive form of RA, the affectation due to CHKV occurs in an intermittent, non-migratory manner, and a chronic phase of affectation without formation of synovial pannus is observed.
Likewise, it stands out the great affectation of the feet and ankles that, although is also frequent in RA, in the CHKV infection is found with a high frequency and persistently. In this regard, it may be suggested that the involvement of the feet and ankles is an important clinical finding in the clinical diagnosis of chikungunya, especially the persistence of the periarticular involvement.
On the other hand, the articular commitment of the CHKV can be differentiated from the affectation of the joints in the reactive arthritis which, as is well known, is usually oligoarticular and asymmetrical.
The high percentage of subjects with articular affection is similar to that was described by Carey,5 according to which the multiple articular commitment affects between 70 and 100% of patients; it is usually symmetric and it affects small joints of the hands and feet, although occasionally it attacks large joints. Likewise, arthralgia is a persistent symptom in any of the phases of the disease, although it should be noted that in this case, according to the normal values of the disease, it is near to the lower limit of the standard range of 70–100%.
ConclusionMost of the signs and symptoms exhibited by the participants showed a big component of rheumatologic type, which indicates that the subjects must be followed-up not only in the acute phase, but also in the sub-acute and chronic.
Polyarticular symmetric involvement of small joints and the great affectation of the feet and the ankles with periarticular location would be the clinical criteria with greater sensitivity and specificity in the diagnosis of post-chikungunya arthritis.
The acute and sub-acute commitment of the post-chikungunya arthritis is very similar to the compromise of RA, however, the same cannot be said of the clinical characteristics in the chronic phase, where there is no formation of synovial pannus and also persists a periarticular involvement in the ankles and feet (Figs. 1 and 2).
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
FundingMetropolitan University and Rheumatology and Orthopedics Center.
Conflict of interestThe authors declare that they have no conflict of interest.
The authors express their gratitude to all the participant patients, to the National Health Institute, to the Rheumatology and Orthopedics Center of Barranquilla and finally to the Metropolitan University, sponsor of the project.
The collaborators in this article are: Miguel Giraldo Ramírez, Jorge Blanco Magdaniel, Dayana Caballero Tovar and Patricia Camargo López, Internal Medicine, Metropolitan University of Barranquilla, Colombia.
Please cite this article as: Jaller Raad J, Sánchez Rincones W, Santrich Martínez A, Sierra Hernández A, Fonseca Estrada Y, Parody A, et al. Caracterización clínica de sujetos infectados con virus chikungunya, en una población del Caribe colombiano. Rev Colomb Reumatol. 2016;23:170–176.