Diffuse idiopathic skeletal hyperostosis (DISH) is a condition characterized by calcification and progressive ossification of ligaments and entheses. Most patients remain asymptomatic until advanced stages of the disease, where limitation and pain are characteristic.
ObjectiveTo describe the demographic, clinical, and radiological characteristics of patients with DISH evaluated in the Centro Médico Imbanaco and Clínica de Artritis Temprana, in Cali, Colombia.
Materials and methodsA descriptive, cross-sectional study was conducted by reviewing the records of patients diagnosed with DISH between January 2000 and October 2018. The diagnosis was confirmed according to the Resnick-Niwayama criteria. A total of 24 patients were found, and all were included for the final analysis.
Results and discussionThe series included 20 men and 4 women, with a median age at diagnosis of 70.5 years (IQR 61.3–73.8 years), being lower in women (71.5 versus 60 years; p=0.04). The median time of onset of the symptoms was 5 years (IQR 3–10 years), and the duration was shorter in women (5 versus 4 years; p=0.20). It was observed that 54% were overweight and 20% were diabetic. The main symptom was cervical limitation. The most affected vertebral segments due to the ossification of the anterior longitudinal ligament (ALL) were C5-C6, T8-T10 and L1-L3 (cervical C; thoracic T; lumbar L). The peripheral involvement was mainly in the iliac crests. All patients received physiotherapy, and three of them underwent cervical surgery. The degree of functional limitation was assessed in 19 patients using the mHAQ (Modified Health Assessment Questionnaire) and BASFI (Functional Ankylosing Spondylitis Functional (BASFI) questionnaires. The median score of both questionnaires was 2 times higher in women.
ConclusionDiffuse idiopathic skeletal hyperostosis was more frequent in men over 65 years of age, and was associated with metabolic conditions such as obesity and diabetes. Although the differences were not significant, the results suggest that women have a more severe phenotype of the disease, explained by the early onset and progressive course of symptoms, as well as greater functional limitation measured by mHAQ and BASFI.
La hiperostosis esquelética idiopática difusa (DISH, por sus siglas en inglés) es una afección caracterizada por la calcificación y la osificación progresiva de los ligamentos y las entesis. La mayoría de los pacientes permanecen asintomáticos hasta etapas avanzadas de la enfermedad, donde la limitación y el dolor son característicos.
ObjetivoDescribir las características demográficas, clínicas y radiológicas de los pacientes con DISH evaluados en el Centro Médico Imbanaco de Cali y en la Clínica de Artritis Temprana, en Cali, Colombia.
Materiales y métodosEs un estudio descriptivo, de corte transversal. Se revisaron los registros de pacientes diagnosticados con DISH, seguidos entre enero de 2000 y octubre de 2018. El diagnóstico se confirmó según los criterios de Resnick-Niwayama. Se encontraron 24 pacientes, todos se incluyeron para el análisis final.
Resultados y discusiónEn esta serie se encontraron 20 varones y 4 mujeres. La mediana de edad al diagnóstico fue de 70,5 años (RIQ: 61,3-73,8 años), siendo menor en las mujeres (71,5 versus 60 años; p=0,04). La mediana de tiempo de evolución de los síntomas fue de 5 años (RIQ: 3-10 años), la duración fue menor en el grupo de las mujeres (5 versus 4 años; p=0,20). El 54,2% tenían sobrepeso y el 20,8% eran diabéticos. El síntoma principal fue la limitación cervical. Los segmentos vertebrales (C: cervical; T: torácico; L: lumbar) más afectados por la osificación del ligamento longitudinal anterior (LLA) fueron C5-C6, T8-T10 y L1-L3. La afección periférica predominó en las crestas ilíacas. Todos los pacientes realizaron terapia física y 3 fueron sometidos a cirugía cervical. El grado de limitación funcional fue valorado en 19 pacientes a través de los cuestionarios modified Health Assessment Questionnaire (mHAQ) y Bath Ankylosing Spondylitis Functional Index (BASFI). La mediana del puntaje de ambos cuestionarios fue 2 veces más alta en las mujeres.
ConclusiónLa DISH fue más frecuente en varones mayores de 65 años y se asoció con enfermedades metabólicas como la obesidad y la diabetes. Aunque las diferencias no fueron significativas, los resultados sugieren que las mujeres presentan un fenotipo grave de la enfermedad explicado por el inicio temprano y curso progresivo de los síntomas, así como mayor limitación funcional medida por mHAQ y BASFI.
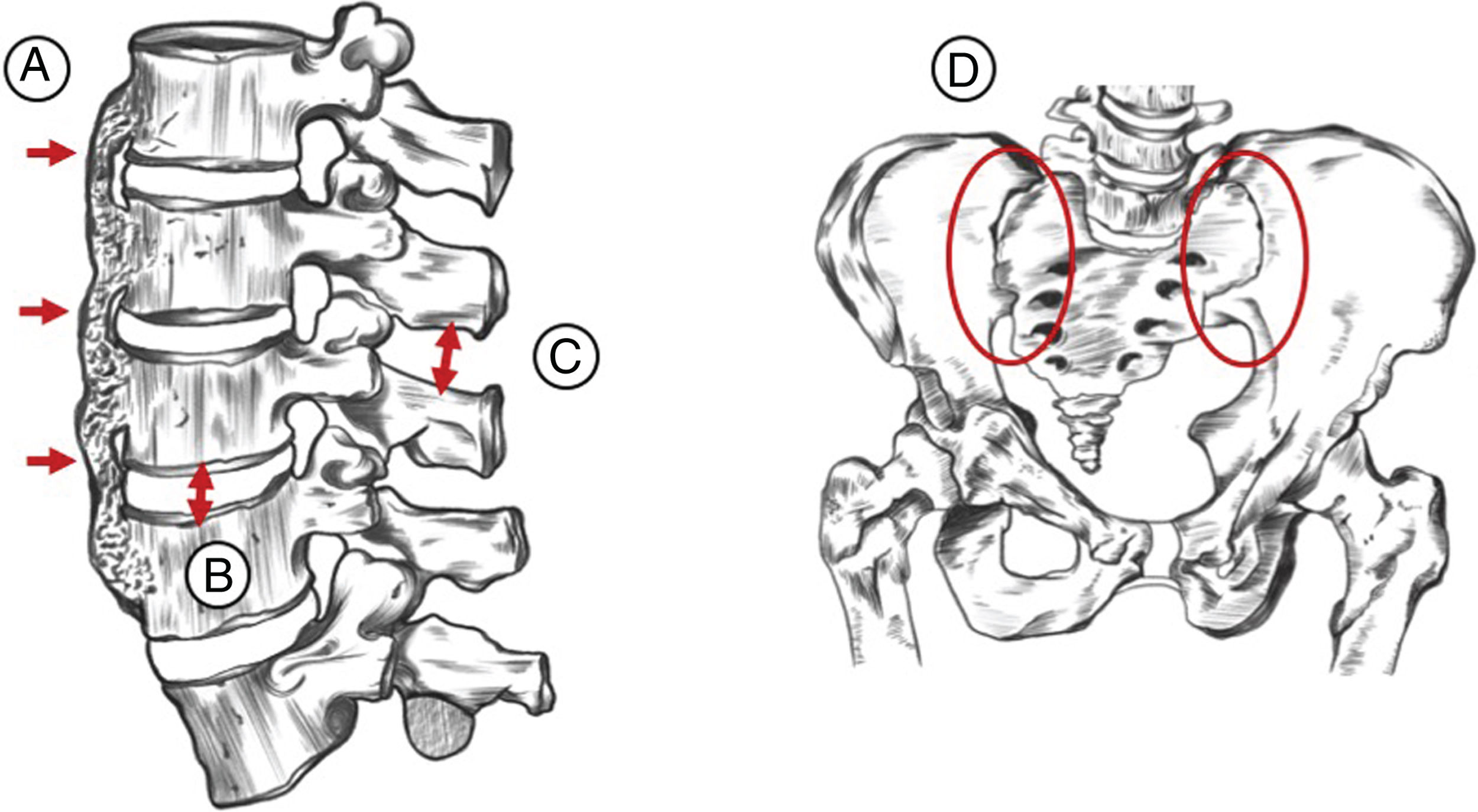
Diffuse idiopathic skeletal hyperostosis (DISH) is a systemic non-inflammatory type condition. Its main characteristic is ligament ossification and to a lesser extent, enthesis - predominantly axial – of the peripheral joints.1 The condition was originally described in 9 patients by Jacques Forestier and his student Jaume Rotés-Querol in 1950 under the denomination “senile ankylosing vertebral hyperostosis”.2 In 1976, Resnick and Niwayama coined the term DISH and established the diagnostic criteria that are currently the most broadly disseminated and used (Fig. 1).3
The last 3 decades have witnessed an increase in the number of DISH cases in the developed countries, probably as a result of the availability of improved imaging techniques as compared to X-rays, leading to an increase in the rate of diagnoses. The prevalence in both males and females over 50 years old is of 25 and 15%, respectively; with an increasing rate after 70 years of age, with 35% of males and 25% females.4 It has been shown over the last few years that computed tomography (CT) has better diagnostic performance. A recent trial conducted in Japan, assessed the prevalence of DISH in 1470 patients using spinal CT and it showed that in individuals over 70 years old, 50% of males and 19.4% of females presented the disease, with a 3:1 ratio.5 In contrast to the structural changes, most DISH patients remain asymptomatic and hence, to a large extent, the diagnosis is incidental or in late stages of the disease. The treatment options are limited to symptomatic pain management, and surgery is indicated in the presence of symptomatic compression of adjacent structures. Aware of the fact that in Colombia the epidemiology of this condition is poorly known, this case series is intended to describe the clinical and radiological characteristics of patients with DISH, in a local Colombian population.
Materials and methodsA descriptive, retrospective, cross-sectional, case series-type study was conducted, reviewing the medical records of patients diagnosed with DISH and receiving care at 2 referral medical centers between January 2000 and December 2018. The diagnosis was confirmed when patients met all of the radiological criteria suggested by Resnick-Niwayama (Fig. 1).
At admission, the clinical manifestations, any medical history, findings during the physical examination, laboratory results, and available imaging studies – including CR or MRI – were taken into consideration. By way of exploration, and upon verbal authorization by the patient, a telephone survey was administered to 19 patients using 2 questionnaires: one of them was validated to describe the level of difficulty to perform 8 basic activities of daily living (modified Health Assessment Questionnaire [mHAQ])6 and the other was validated to define the level of functional limitation in patients with ankylosing spondylitis (Bath Ankylosing Spondylitis Functional Index [BASFI]).7 The latter was used due to the lack of specific scales to assess the level of limitation of patients with DISH and based on the similarities between the two illnesses. The study complied with the guidelines of the Ethics Committee of the Centro Médico Imbanaco and the Clínica de Artritis Temprana.
Patients with radiological similarity with primarily axial osteoarthritis and spondylarthritis were excluded. Descriptive statistics were used to summarize the characteristics of the population. The quantitative variables were submitted using central tendency and scatter measurements. The qualitative variables were summarized as proportions and were presented in frequency tables. An exploratory analysis was conducted to determine the statistical significance among the quantitative variables using the Student-T test.
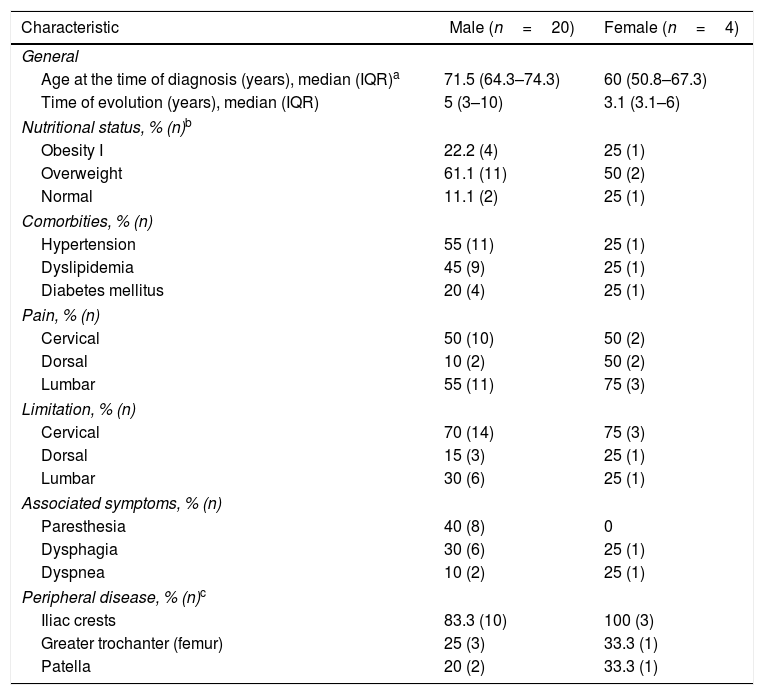
Results24 patients were selected, 20 males and 4 females, with a 5:1 ratio. The mean age at diagnosis was 70.5 years (IQR: 61.3–73.8 years), with females being younger than males (71.5 versus 60 years; p=0.04). The youngest patient was 41, and the oldest was 87 years old. The mean time of evolution of symptoms was 5 years (IQR: 3–10 years), the duration was shorter in the female group (5 versus 4 years; p=0.20). Table 1 describes the demographic, clinical and radiological variables according to gender. The body mass index was 26.9kg/m2 (IQR: 25.3–30.1kg/m2). 54.2% were overweight, and the most frequent comorbidity was hypertension (50%). No major cardiovascular events were documented (myocardial infarction, cerebrovascular disease or peripheral arterial disease), and neither any coexisting systemic autoimmune diseases.
Demographic, clinical and radiological characteristics.
| Characteristic | Male (n=20) | Female (n=4) |
|---|---|---|
| General | ||
| Age at the time of diagnosis (years), median (IQR)a | 71.5 (64.3–74.3) | 60 (50.8–67.3) |
| Time of evolution (years), median (IQR) | 5 (3–10) | 3.1 (3.1–6) |
| Nutritional status, % (n)b | ||
| Obesity I | 22.2 (4) | 25 (1) |
| Overweight | 61.1 (11) | 50 (2) |
| Normal | 11.1 (2) | 25 (1) |
| Comorbities, % (n) | ||
| Hypertension | 55 (11) | 25 (1) |
| Dyslipidemia | 45 (9) | 25 (1) |
| Diabetes mellitus | 20 (4) | 25 (1) |
| Pain, % (n) | ||
| Cervical | 50 (10) | 50 (2) |
| Dorsal | 10 (2) | 50 (2) |
| Lumbar | 55 (11) | 75 (3) |
| Limitation, % (n) | ||
| Cervical | 70 (14) | 75 (3) |
| Dorsal | 15 (3) | 25 (1) |
| Lumbar | 30 (6) | 25 (1) |
| Associated symptoms, % (n) | ||
| Paresthesia | 40 (8) | 0 |
| Dysphagia | 30 (6) | 25 (1) |
| Dyspnea | 10 (2) | 25 (1) |
| Peripheral disease, % (n)c | ||
| Iliac crests | 83.3 (10) | 100 (3) |
| Greater trochanter (femur) | 25 (3) | 33.3 (1) |
| Patella | 20 (2) | 33.3 (1) |
The medical records emphasized the presence of axial pathology expressed by limited mobility of the neck (74%) and lumbar region pain (58.3%). The primary associated symptom was upper limb paresthesia (34.8%). The most frequent finding during the physical examination was reduced neck mobility (70.8%). The lab results reported a mean hemoglobin of 15.3g/dl (IQR: 14.7–15.7g/dl), leukocytes 6870cells/mm3 (IQR: 5.650–9.065cells/mm3), creatinine of 0.94mg/dl (IQR: 0.89–1.03mg/dl), erythrocyte sedimentation rate 7.5mm/h (IQR: 2.25–20mm/h). Among the acute phase reactants, ESR was positive in 2/16 (12.5%) and CRP was positive in 4/13 (30.7%). HLA-B27 was negative in 8/8 patients.
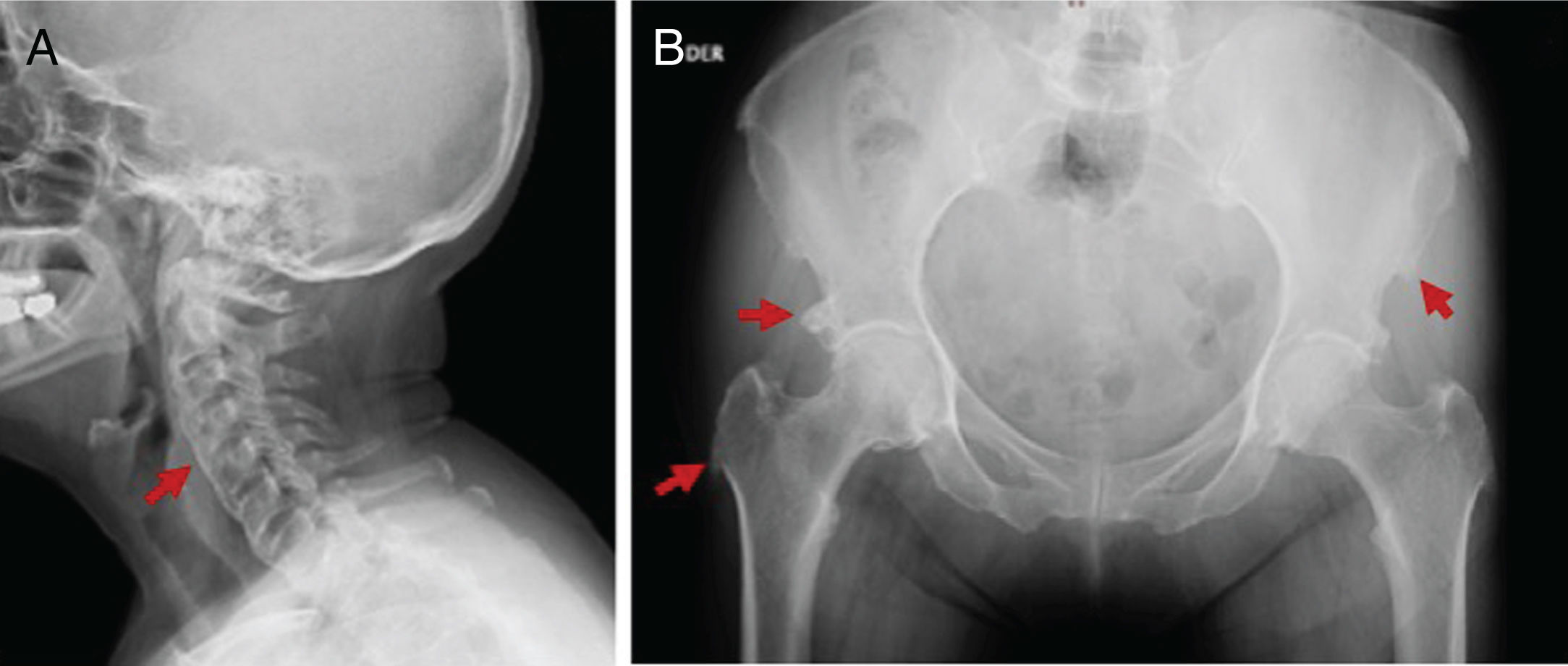
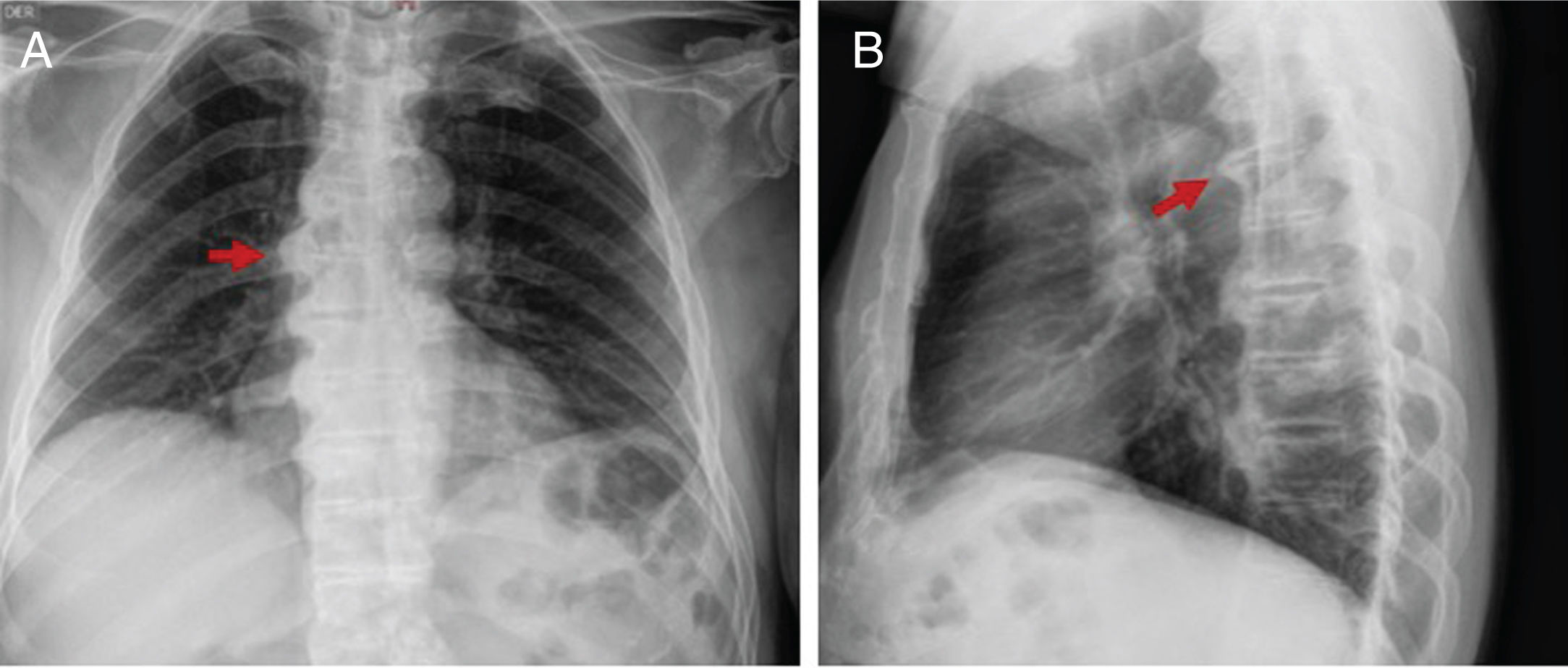
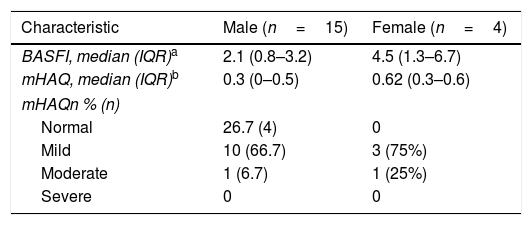
Although the DISH diagnosis in all cases was done with a plain spinal radiogram, 45.8% of the patients had additional studies, including CT and MRI. The mean number of affected vertebrae was 5 (IQR: 4–6). The main area affected was the thoracic spine (75%), followed by the cervical and lumbar spine (58.3%). The most affected vertebral segments based on the localization were: C5-C6 in the cervical spine, T8-T10 in the thoracic spine, and L1-L3 in the lumbar spine. The ossification of the Anterior Longitudinal Ligament (ALL) was predominantly in the right side in 72.2% of patients. Peripheral disease was documented in 62.5%, being more relevant in the iliac crests (86.7%) (Table 2). In 2 patients, displacement of adjacent structures, esophagus and glottic region was documented with CT. Figs. 2–4 exemplify the radiological findings in 3 patients. All patients received physical therapy as part of their treatment. 33.3% used pain killers and muscle relaxants. Three patients underwent surgery due to cervical disease, with subjective symptom improvement. In terms of functional limitation, data were collected from 19 patients, 15 males and 4 females. The mean MHAQ score was 0.5 (IQR: 0.125–0.65) and the mean BASFI score was 2.1 (IQR: 0.8–4). The classification of the severity of the limitation is illustrated in Table 2.
Functional limitation.
| Characteristic | Male (n=15) | Female (n=4) |
|---|---|---|
| BASFI, median (IQR)a | 2.1 (0.8–3.2) | 4.5 (1.3–6.7) |
| mHAQ, median (IQR)b | 0.3 (0–0.5) | 0.62 (0.3–0.6) |
| mHAQn % (n) | ||
| Normal | 26.7 (4) | 0 |
| Mild | 10 (66.7) | 3 (75%) |
| Moderate | 1 (6.7) | 1 (25%) |
| Severe | 0 | 0 |
BASFI: Bath Ankylosing Spondylitis Functional Index; mHAQ: modified Health Assessment Questionnaire.
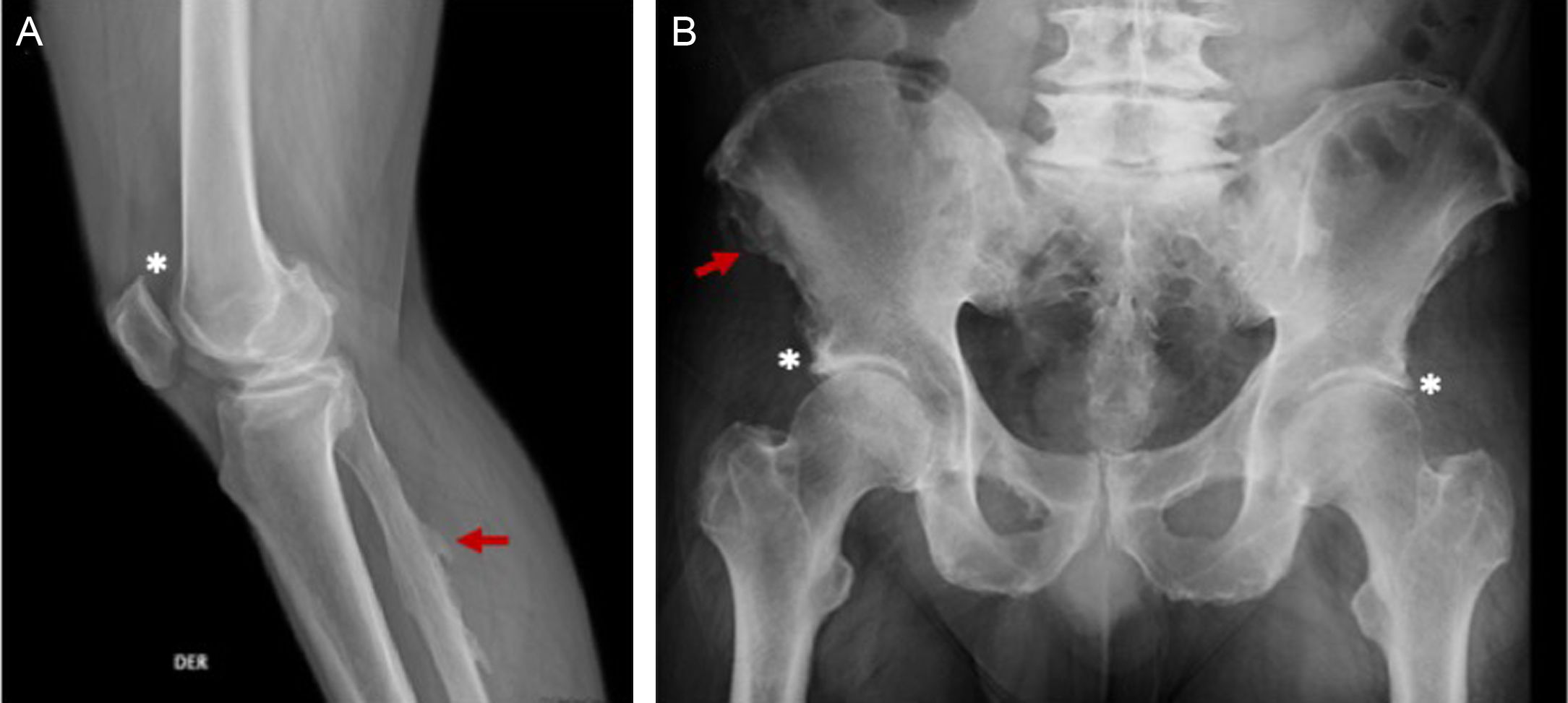
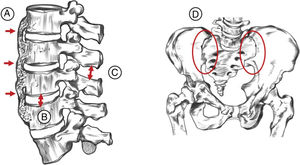
65-year old male, obese, with a history of 15 years of evolution of pain in the dorsolumbar spine and knees associated with right lower extremity paresthesia. Radiographic findings (A) right knee, bone excrescences in the patella (*) and in the fibular enthesis (red arrow), (B) ossification in enthesis of the iliac spines (red arrow) and the acetabulum. (*).
DISH mainly affects the elderly population. Its natural history has a benign course. The advent of new diagnostic imaging techniques has expanded our knowledge about the epidemiology of the disease.5,8 Our cohort shows a gender relationship of 5:1, consistent with the range described in previous trials (2:1–7:1).9,10 The mean age at the time of diagnosis was lower in women (p=0.04). Although DISH is less frequent among females, an earlier diagnosis in women suggests greater clinical involvement. A previous study supports these findings by concluding that women develop the disease earlier, and correlates with a higher mortality.11
The exact mechanisms contributing to bone formation in patients with DISH is still being debated. A significant association with metabolic disorders such as diabetes mellitus, obesity, dyslipidemia, and hyperglycemia has been described.12 This fact was substantiated in our cohort, where hypertension and overweight were the most frequent underlying conditions. Although the pathophysiology is poorly known, the main concept is based on disproportionate growth factors such as insulin, insulin-like growth factor 1, transforming growth factor beta 1, platelet-derived growth factor, prostaglandins I2 and endothelin 1, which lead to the transformation of mesenchymal cells into fibroblasts and osteoblasts. On the other hand, there is a reduction in the activity of bone promoter peptide inhibitors (matrix Gla protein, bone morphogenic protein 2, Dickkopf-1 protein).13 Angiogenesis is an important factor for the proliferation of osteoblasts, skeletal development, and bone repair. The role of angiogenesis in the atherosclerotic process of patients with metabolic disorders could well be the link between these 2 conditions.14
In general, the symptoms depend on the localization of the ossification. The most common manifestations are directly associated with the spinal changes, including axial pain and nerve root symptoms (pain, paresthesia and limb weakness). Furthermore, there is reduction in the axial range of movement, favoring the development of unstable vertebral fractures.15 Airway obstruction may be the result of tracheal compression due to large osteophytes.16 Dysphagia is the result of mass effect, direct lesion of the recurrent laryngeal nerve or inflammation and fibrosis of the esophageal wall.17 Peripheral manifestations include joint involvement usually not present in osteoarthritis (elbows, shoulders, ankles), presence of bony excrescences adjacent to the joints, and extra-articular calcification, mainly in the tibial tuberosity, the heel bone, the patella and the olecranon.18 There are even case reports where peripheral manifestations prevail.19 The symptomatology of the cohort presented is no different from the reports from previous studies, with the cervical limitation being common in approximately 75% of the patients, followed by neck pain (50%) and symptoms secondary to the compression of adjacent structures (mainly paresthesia) in one third of them.
The functional limitation of patients with DISH has been a controversial topic. Some authors have considered it a state rather than a disease; however, others have concluded that patients with DISH have a diminished functional capacity similar to patients with spondylarthrosis and higher than the normal population measured through questionnaires such as the Health Assessment Questionnaire (HAQ).20 Mader et al. found a decreased functional capacity in 87 patients with DISH, as compared to patients with osteoarthritis.21 In this regard, in our population, 68.4% had a mild limitation according to mHAQ. When separating the results by gender, women had a mean mHAQ score 3-fold higher, and in BASFI, 2-fold higher, as compared to the male population. Although these results were not statistically significant, possibly due to the small number of patients, the finding suggests a more severe impact on females. Based on the literature reviewed, no studies were found that compared the level of functional limitation according to gender.
The key characteristic depicted in the images is the presence of osteophytes converging onto the thoracic spine. The thick bone bridges develop along the ALL in a more horizontal orientation and mostly on the right side, on account of the impact of the pulsating aorta.13 A study conducted in 2017 prioritized spinal disease as follows: middle thoracic 21.9%, lower thoracic 21.3%, upper thoracic 10.4%, followed by cervical (7.9%) and lumbar (7.3%).22 No differences were found in the order of presentation between males and females.23 Hiyama et al. demonstrated in 289 patients with DISH, that the T8-T10 segment was the most affected, primarily in the right anterior region of the vertebral bodies.5 Consistent with such claim, in this study the most affected segment of the spine was also T8-T10. Other radiographic findings differ in part: while the thoracic segment was the most affected in terms of prevalence, over 50% of our population experienced changes in the cervical and lumbar spine.
In the literature, the Resnick-Niwayama criteria are the most popular and accepted, but they are limited to identify patients with advanced stages of the disease. Though numerous authors have suggested new criteria aimed at overcoming these limitations, currently there is no definitive consensus. The involvement of at least 3 continuous vertebrae (2 bone bridges) has been described as the primary criterion by Bregeon et al.,24 Harris et al.,25 Arlet t Mazière,26 Marcelli et al.27 and Rogers & Waldron.28 In 1985 Utsinger extended the classification criteria to include peripheral enthesopathies.29 Using Utsinger's criteria, a final DISH diagnosis is established when the thoracolumbar ossification is present in at least 4 continuous vertebrae; a probable diagnosis is when there are at least two continuous vertebrae compromised, accompanied by bilateral peripheral enthesopathy and a likely diagnosis when there are at least 2 vertebrae involved and if there is symmetrical enthesopathy in the absence of spinal compromise (particularly when affecting more than one anatomic site). The exclusion criteria are the loss of intervertebral space and anchyloses of the apophyseal joint. The probable or potential categories may identify patients with higher risk of developing DISH, though currently we do not have available a practical approach for treating these patients. Since this is a disease affecting mostly the elderly, it may coexist with spondylarthritis. Differentiating between these two conditions is not easy. The radiographic findings such as the absence of involvement of the apophyseal joint and preservation of the intervertebral disc height may be helpful. Anchylosing spondylitis (AS) is another differential diagnosis that shares a number of characteristics with DISH, such as the tendency to ossification of the ligaments and the enthesis; although in AS this process takes place as a result of different inflammatory mechanisms. The key differences are: sacroiliac joint involvement, the appearance and projection angle of the osteophytes and syndesmophytes, the presentation in young patients, the association with HLA-B27 and a higher level of pain and limitation.1,30
There are no randomized controlled trials on pharmacological therapy of patients with DISH. In clinical practice, the treatment approach is based on the guidelines for similar diseases. In fact, the treatment for axial and peripheral pain is based on the use of pain killers and non-steroid anti-inflammatory drugs (NSAIDs) as used for osteoarthritis, in addition to physical therapy and dietary programs. The use of NSAIDs could be adopted as a preventive measure for the development of heterotopic ossification, just as bisphosphonates have been used to reduce osteophyte formation.31 Due to the association with metabolic entities, it has been suggested that the use of drugs that increase insulin secretion such as sulphonylureas, betablockers, and thiazide diuretics should be avoided.13 Surgery is indicated when conservative maneuvers fail in patients with severe complications, such as airway obstruction, dysphagia, and fractures.32,33
The strength of this trial was the analysis of radiologically confirmed DISH cases and the inclusion of the different clinical and radiological variables between genders which enabled the comparison between our population against what is published in the literature. One of the drawbacks is the retrospective approach that prevents the analysis of other variables and the fact that the records were sourced by only two centers. These limitations call for further prospective cohort studies, preferably multicenter trials, providing a larger sample size and the identification of factors associated with the disease.
ConclusionIn this particular series, DISH was frequent among males over 65 years old, and was associated with metabolic diseases such as obesity and diabetes. Although the differences were non-significant, the results suggest that women present a severe phenotype of the disease as shown by an earlier onset and progression of symptoms, in addition to greater functional limitation as determined through mHAQ and BASFI. There was a clinical correlation between the symptoms and the radiological presentation. Different from other cohorts, cervical and lumbar ossification were frequent. Acute phase reactants are usually negative. There was no association with any autoimmune systemic or rheumatic documented disease, at least until the last follow-up of patients.
FinancingThe authors claim to have conducted this study with funding from the principal author.
Conflict of interestsThe authors have no conflict of interests to disclose.
Please cite this article as: Quintero-González DC, Arbeláez-Cortés Á, Rueda JM. Características clínico-radiológicas de la hiperostosis esquelética idiopática difusa en 2 centros médicos de Cali, Colombia: reporte de 24 casos. Rev Colomb Reumatol. 2020;27:80–87.