We describe the case of an 82-year-old man who had recently undergone cardiac surgery (quadruple coronary bypass), who consulted due to the appearance of a necrotic eschar on the thumb of the right index finger, together with paraesthesia and hypoaesthesia in the first 3 fingers of the same hand. An ultrasound scan of the right elbow was performed to rule out involvement of the median nerve and an anechoic, thick-walled mass was found, dependent on the wall of the proximal ulnar artery, compatible with a pseudoaneurysm of the same, compressing the nerve. Electromyography showed an acute lesion of the proximal median nerve and angio-CT confirmed the diagnosis of pseudoaneurysm of the proximal ulnar artery. Pseudoaneurysm is a dilatation by rupture of the arterial wall, which does not involve all three layers of the arterial wall and communicates with the vascular lumen. Its development after vascular manipulation is very rare, and it is uncommon for it to act by compressing a nerve structure. In our case, together with vascular surgery, treatment with intralesional thrombin was decided, with good evolution.
Se describe el caso de un varón de 82 años intervenido recientemente de cirugía cardíaca (cuádruple bypass coronario), que consulta por aparición de una escara necrótica en el pulpejo del dedo índice derecho, junto a parestesias e hipoestesias en los tres primeros dedos de dicha mano. Se realiza una ecografía del codo derecho para descartar afectación del nervio mediano y se objetiva una masa anecoica, de paredes engrosadas, dependientes de la pared de la arteria cubital proximal, compatible con pseudoaneurisma de esta, que comprime dicho nervio. En la electromiografía se evidencia una lesión aguda del nervio mediano a nivel proximal y en el angio-TC se confirma el diagnóstico de pseudoaneurisma de la arteria cubital proximal. El pseudoaneurisma es una dilatación por rotura de la pared arterial, que no implica a las tres capas de esta y se comunica con la luz vascular. Su desarrollo tras una manipulación vascular es muy infrecuente y que actúe comprimiendo una estructura nerviosa es poco común. En nuestro caso, conjuntamente con cirugía vascular se decidió tratamiento con trombina intralesional, con buena evolución.
An 82-year-old male who attended the rheumatology outpatient clinic in March 2020 due to the appearance of a necrotic eschar on the pad of the right index finger, as well as loss of strength in said hand. As history of interest, he presented arterial hypertension and dyslipidemia and had undergone a quadruple coronary bypass surgery in January 2020. The patient reported that since the intervention he had paresthesias, hypoesthesia, and loss of strength in the first three fingers of his right hand. A few weeks later he began to develop a necrotic lesion, for which he consulted.
On anamnesis, he denied Raynaud’s phenomenon or previous episodes of arthritis, he did not present sensation of dysthermia or other cutaneous or mucosal lesions, nor did he have infectious symptoms at the time he attended the visit. He had not objectified macroscopic alterations in the stools, his digestive rhythm had not changed, he denied loss of weight or appetite and he did not have macroscopic alterations in the urine.
The laboratory tests revealed elevated acute phase reactants (C-reactive protein 132.5 mg/dL, erythrocyte sedimentation rate 60 mm/h) and normochromic normocytic anemia (hemoglobin 9.9 g/dL). Autoimmunity was negative, the proteinogram was normal and the urinary sediment was anodyne. With the suspicion of mononeuritis of the median nerve associated with an established digital necrosis, the patient was admitted to rheumatology for study.
Physical explorationThe patient was conscious and oriented in all three spheres, with preserved higher functions.
NeurologicalDecreased strength (3/5) and hypoesthesia in the first three fingers of the right hand, strength and sensitivity preserved in the fourth and fifth fingers of said hand and in all the fingers of the contralateral hand.
VascularRadial pulse present, ulnar pulse abolished. Accurate capillary refill.
CutaneousNecrotic eschar in the pad of the right index finger, with no other lesions.
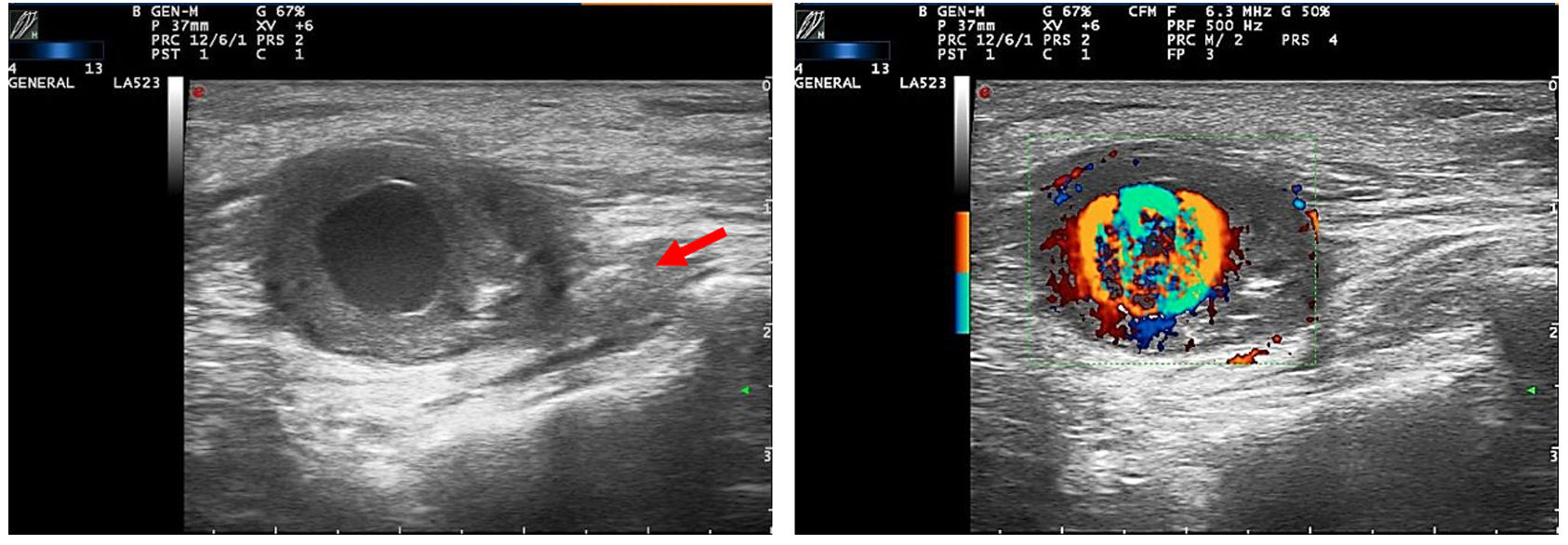
Complementary explorationsUltrasound of the right elbowAnechoic mass with thickened and hypoechoic walls, measuring 60 mm × 107 mm, dependent on the wall of the proximal ulnar artery, shortly after the bifurcation of the brachial artery, with intralesional power-Doppler signal, compatible with pseudoaneurysm vs. parietal aneurysm of the latter. In a position medial to the vascular lesion, the thickened median nerve is observed, with a diameter greater than 58 mm (Fig. 1).
Electromyography/electroneurophysiologySigns of denervation in the explored muscles, both proximal and distal, dependent on the right median nerve (located at the level of the insertion of the pronator teres muscle), with absence of voluntary activity. The rest of the explored muscles correspond to a different nerve and the same root within normality.
ConclusionAcute lesion of the proximal right median nerve at the level of the elbow, of severe degree.
Angio-CT
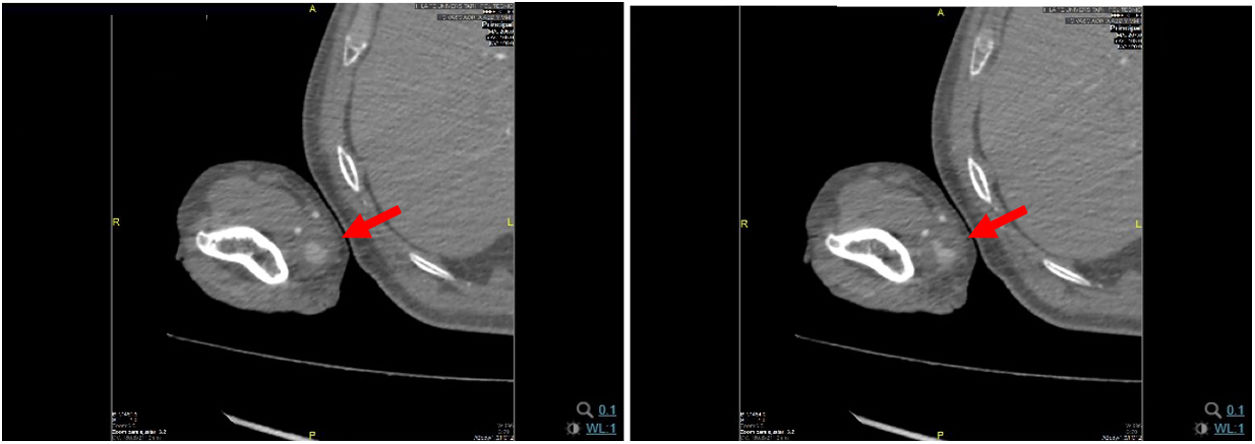
A pseudoaneurysm of the right ulnar artery measuring 22 × 21 mm in diameter, with a neck of 2 mm is observed (Fig. 2).
EvolutionAfter confirming the diagnosis of pseudoaneurysm of the ulnar artery by angio-CT, we requested evaluation by vascular surgery, which opted for interventional treatment through ultrasound-guided thrombin injection. Ultrasound control was performed 48 h after the procedure, in which total thrombosis of the lesion was observed. At discharge, they prescribed clopidogrel 75 mg/day for five days and clinical monitoring in their consultations.
The control at two and four months evidenced the complete resolution of the lesion, confirmed the recovery of the amplitude of the ulnar pulse and the absence of new necrotic lesions. Regarding strength, the patient attended several rehabilitation sessions in the months following hospital discharge, with complete recovery of weakness (strength 5/5).
DiscussionA pseudoaneurysm is a vascular dilatation due to rupture of the arterial wall, which does not involve the three layers that make it up and communicates with the vascular lumen.1 In general terms, pseudoaneurysms of peripheral arteries are rare and, specifically, the pseudoaneurysms that affect the upper limbs have a prevalence of 2%.1,2 Their etiology is usually traumatic after manipulation of displaced fractures or iatrogenic in the context of invasive vascular procedures.3,4 It is postulated that defective vascular manipulation or a coagulation disorder could participate in their development.3 Despite their low prevalence, the frequency is currently increasing as a consequence of the greater use of invasive intravascular techniques. In addition, it is also higher in parenteral drug addicts and in hemodialyzed patients.1,5
There are reported cases of compressive neuropathy of the median nerve at the level of the carpal tunnel or the elbow flexure, due to lesion of the brachial or the ulnar artery.2,5 The carpal tunnel syndrome is the most frequent nerve entrapment, with a prevalence of around 2.1% of the general population.6 The ulnar artery coincides anatomically with the median nerve at the level of the elbow, shortly after its bifurcation from the brachial artery. Ulnar artery aneurysms have been known since the 18th century, the first case was described by Guattani, being one of the causes that arise in the differential diagnosis of digital ischemia of the upper limbs.7 However, in the literature there is only one published case of compression of the median nerve by the ulnar artery, since it is most frequently compressed by the brachial artery,1–3 as inferred after the bibliographic review. In our case, the location of the pseudoaneurysm is unusual, since it is located in the most proximal portion of the ulnar artery, just after its bifurcation from the brachial artery.
In the presence of a patient with symptoms of compressive neuropathy, ultrasound could confirm the diagnosis and offer information about the morphology of the affected nerve and the state of nearby structures.6 In addition, it is useful in the differential diagnosis of elbow or forearm flexure injuries and facilitates follow-up.4 In the case of a pseudoaneurysm, hyperechoic flow or material corresponding to an intralesional thrombus will be observed. Finally, it is worth mentioning that it is an advantageous technique in terms of its low cost and wide availability. In relation to other imaging techniques, arteriography continues to be the gold standard, but angio-CT or MRI angiography are also useful and widely used tests.1
Finally, the treatment of any pseudoaneurysm depends fundamentally on the size, location, and pathogenesis.5 Due to the possibility of embolization or thrombosis, treatment should not be delayed.1 The therapeutic options currently available are endovascular techniques (embolization, stent placement) or traditional surgery, which offers very good outcomes.5 Intralesional thrombin injection was first described by Cope and Zeit in 1986. This technique, which has been shown to be highly effective, requires an ultrasound control at 24 h to confirm that it has been successful.4,5 Surgical treatment is preferred in cases where the lesion progresses rapidly, when there is already established ischemia, and when there is a high risk of distal embolization or small arterial caliber, which makes complex the placement of an endoprosthesis.4,5
Ethical considerationsThe work was approved by the Research Ethics Committee of the La Fe University and Polytechnic Hospital (Hospital Universitario y Politécnico La Fe) (Valencia). The authors have the informed consent of the patients.
FundingThis work has not received any type of funding.
Conflict of interestThe authors declare that they have no conflict of interest.