Vitamin D is a hormone that maintains a fundamental role in the phosphocalcic metabolism. In recent years, studies have shown an association between vitamin D deficiency and different rheumatic diseases.
PurposeTo evaluate vitamin D levels in patients at a rheumatology center during a period of 2015–2016.
MethodsA retrospective study of patients who attended a rheumatology center, who had an initial study of 25(OH)D serum. Vitamin D levels were classified as: normal: 30–40ng/mL, deficiency: 30–20ng/mL, insufficiency: 20–10ng/mL and severe insufficiency: <10ng/mL.
Results279 patients with a mean age of 58 years [8–93], 86% women [58.4 years] and 14% men [59.8 years] were included. The mean value of vitamin D was 29.09ng/mL. A total of 41.2% (115) of the patients had values >30ng/mL, and 58.8% (164) below this range. The most frequent primary diagnoses found were: osteoarthrosis, rheumatoid arthritis, fibromyalgia and osteoporosis; from which low levels of vitamin D ≤30ng/mL were identified in 53.8%, 69.7%, 76.5% and 42.9%, respectively.
ConclusionThere is a high incidence of hypovitaminosis D in Ecuadorian patients who came to a rheumatology center.
La vitamina D es una hormona que mantiene un papel fundamental en el metabolismo fosfocálcico. En los últimos años, los estudios han demostrado una asociación entre la deficiencia de vitamina D y diferentes enfermedades reumáticas.
ObjetivoEvaluar los niveles de vitamina D en pacientes en un centro de reumatología durante el período de 2015-2016.
MétodosEstudio retrospectivo de pacientes que acudieron a un centro de reumatología, que realizaron un estudio inicial de suero 25 (OH) D. Los niveles de vitamina D se clasificaron como normal: 30-40 ng/mL, deficiencia: 30-20 ng/mL, insuficiencia: 20-10 ng/mL e insuficiencia severa: <10 ng/mL.
ResultadosSe incluyeron 279 pacientes con una edad media de 58 años (8-93), 86% mujeres (58,4 años) y 14% hombres (59,8 años). El valor medio de la vitamina D fue de 29,09 ng/mL. Un total de 41,2% (115) de los pacientes tenía valores> 30ng/ml y 58,8% (164) por debajo de este rango. Los diagnósticos primarios más frecuentes encontrados fueron: osteoartrosis, artritis reumatoide, fibromialgia y osteoporosis; de los cuales se identificaron niveles bajos de vitamina D ≤ 30 ng/mL en 53,8; 69,7; 76,5 y 42,9%, respectivamente.
ConclusiónExiste una alta incidencia de hipovitaminosis D en pacientes ecuatorianos que acudieron a un centro de reumatología.
Vitamin D [25 (OH) D] is known to be a hormone that forms part of a group of sterols with a fundamental role in phosphocalcic metabolism.1 The main source of this vitamin is the conversion of 7-dihydrocholesterol to pre-vitamin D3 in the skin through ultraviolet (UV) radiation, which makes up 98% of the body's vitamin D.2,3 Other sources of vitamin D are obtained from foods, mainly fish, in the form of vitamin D2 or ergocalciferol.4
The synthesis of vitamin D begins at the cutaneous level by converting 7-dihydrocholesterol to the previtamin-D in the keratinocytes, which isomerized to vitamin D3, by means of a heat-mediated process, when the levels are sufficient, it can be photoisomerized to inert forms such as lumisterol or tachisterol or even to become 7-dihydrocholesterol and degraded to suprasterol I and II.1–5
The main function of vitamin D is the regulation of calcium absorption at the intestinal level, a process called transcaltachia, by means of the phosphocalcic metabolism maintains the bone and muscular homeostasis,3–7 in addition it plays a fundamental role in the immunological response and inflammatory processes, by the inhibition of proinflammatory cytokines (IL-6 and TNF-α) in monocytes.8
Although non-classical actions of vitamin D are still under discussion; it has been shown that vitamin D levels are decreased in diseases that have immunological components.8–12
A study by Kostoglou-Athanassiou et al. Showed that patients with rheumatoid arthritis had vitamin D deficiency versus a control group, and a significant association was found between hypovitaminosis and elevated levels of inflammatory markers.8
In Latin America there is an initiative to carry out studies on the prevalence of vitamin D levels, a systematic review by Brito et al. Identified approximately 243 studies and selected 28, of which they concluded that there is a vitamin D deficiency in the region, however, the exact magnitude.13
Orces showed that in a larger Ecuadorian adult population approximately 21.6% had deficiency and 67.8% insufficient levels of vitamin D,14 however, there is a lack of data regarding levels of vitamin D in other age groups.
The objective of the study was to evaluate vitamin D levels in patients of a rheumatology center in Ecuador during a period of one year (2015–2016).
MethodsThis is a retrospective study of patients who came to a rheumatology center, who had an initial study of plasmatic 25(OH)D. The selection of patients was performed using inclusion and exclusion criteria, mentioned below:
Inclusion criteriaPatients who came to a rheumatology center (Rheumatology and Rehabilitation Center) with an established diagnosis of rheumatic diseases (osteoarthritis, rheumatoid arthritis, fibromyalgia, osteoporosis, soft tissue rheumatism, etc.).
Have an initial study of vitamin D.
Exclusion criteriaPatients who do not wish to participate in the study. Patients under Vitamin D supplementation.
All participants signed an informed consent and the anomicity of the patients was respected during the research process.
Vitamin D determinationPlasma levels of 25 (OH) D of the patients were performed in a previously determined laboratory. Samples were analyzed by the chemiluminescence method with an Advia Centaur® assay system. Vitamin D levels are not standardized for each population, however the following1,4,6,13 are considered:
Normal: 30–40ng/mL
Deficient: 30–20ng/mL
Insufficiency: 20–10ng/mL
Severe Insufficient: <10ng/mL
The sampling of vitamin D in these patients was during the year 2015–2016; the inclusion range of the patients was performed according to the following age groups:
Ultraviolet (UV) and sun exposure indexThe origin of the patients was the city of Manta located in the province of Manabí at six meters above sea level and at latitude of −0.95, with a solar exposure index of 10-11UV.
Statistic methodThe data were analyzed in the statistical program SPSS v 22, in which quantitative variables, T-test of two tails and for the qualitative variables, chi-square and logistic regression were determined, in addition, multiple linear regression models were used to study The relationship of vitamin D levels and concomitant disease together with comorbidities. p values below 0.05 were considered statistically significant.
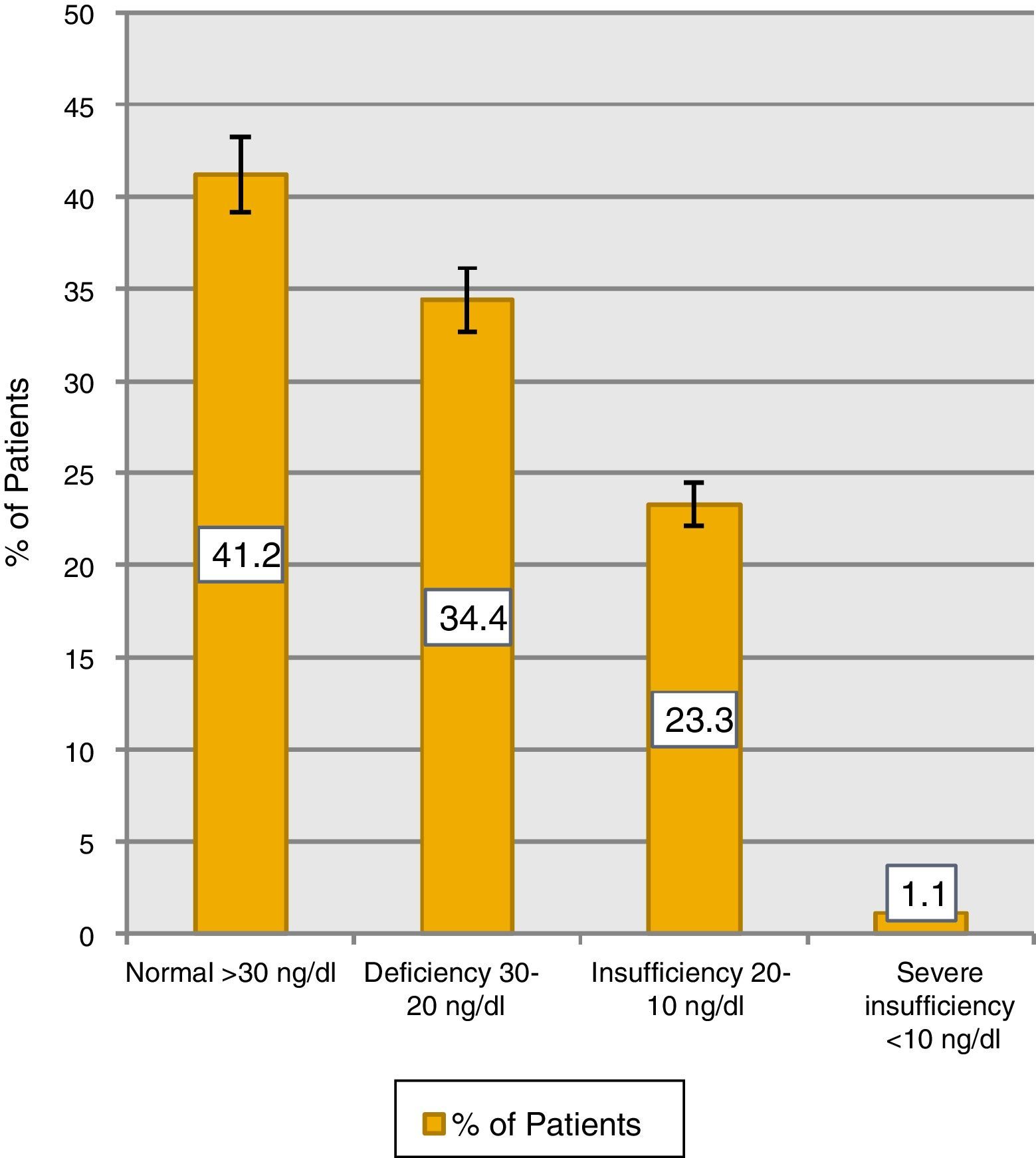
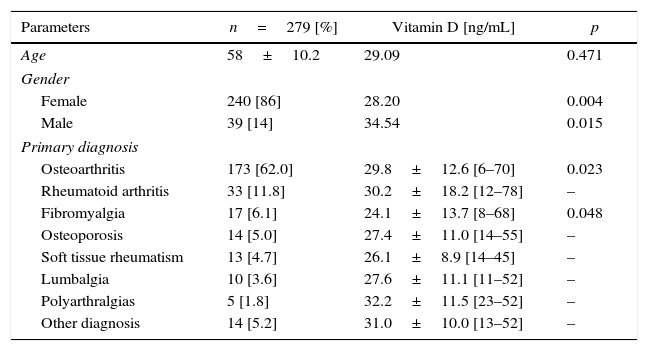
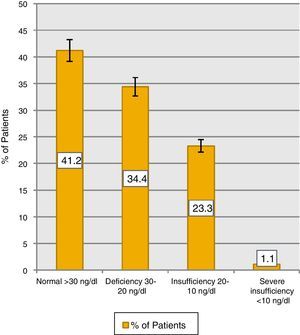
ResultsWe included 279 patients with a mean age of 58 years [8–93], 86% women [58.4 years] and 14% men [59.8 years] (Table 1). The mean value of vitamin D was 29.09ng/mL, 41.2% (115) of patients with values >30ng/mL and 58.8% (164) below this: 34.4% (96) deficiency, 23.3% (65) insufficiency and 1.1%3 severe insufficiency (Fig. 1).
General characteristics of the population studied.
| Parameters | n=279 [%] | Vitamin D [ng/mL] | p |
|---|---|---|---|
| Age | 58±10.2 | 29.09 | 0.471 |
| Gender | |||
| Female | 240 [86] | 28.20 | 0.004 |
| Male | 39 [14] | 34.54 | 0.015 |
| Primary diagnosis | |||
| Osteoarthritis | 173 [62.0] | 29.8±12.6 [6–70] | 0.023 |
| Rheumatoid arthritis | 33 [11.8] | 30.2±18.2 [12–78] | – |
| Fibromyalgia | 17 [6.1] | 24.1±13.7 [8–68] | 0.048 |
| Osteoporosis | 14 [5.0] | 27.4±11.0 [14–55] | – |
| Soft tissue rheumatism | 13 [4.7] | 26.1±8.9 [14–45] | – |
| Lumbalgia | 10 [3.6] | 27.6±11.1 [11–52] | – |
| Polyarthralgias | 5 [1.8] | 32.2±11.5 [23–52] | – |
| Other diagnosis | 14 [5.2] | 31.0±10.0 [13–52] | – |
When comparing vitamin D means by gender, it was found that women had lower levels than men (28.20 vs 34.54, 95% CI, p=0.004). 61.7% of the women had some degree of hypovitaminosis compared to 41.0% of the men (95% CI, p=0.015). 38.3% of women had a normal value compared to 59.0% of men.
When analyzing the 4 most frequent diagnoses (osteoarthritis, osteoporosis, rheumatoid arthritis and fibromyalgia), it was found that patients with osteoarthritis presented hypovitaminosis in 53.8%. Of the group with hypovitaminosis D, 31.8% had levels considered deficient, 20.8% insufficient and 1.2% severe insufficiency.
In patients with rheumatoid arthritis, hypovitaminosis was present in 69.7%, of which 33.3% were deficient and 36.4% were insufficient.
Of the fibromyalgia group, 23.5% presented normal values of vitamin D and 76.5% under this with 29.4% insufficiency, 41.2% deficiency and 5.9% had severe deficiency.
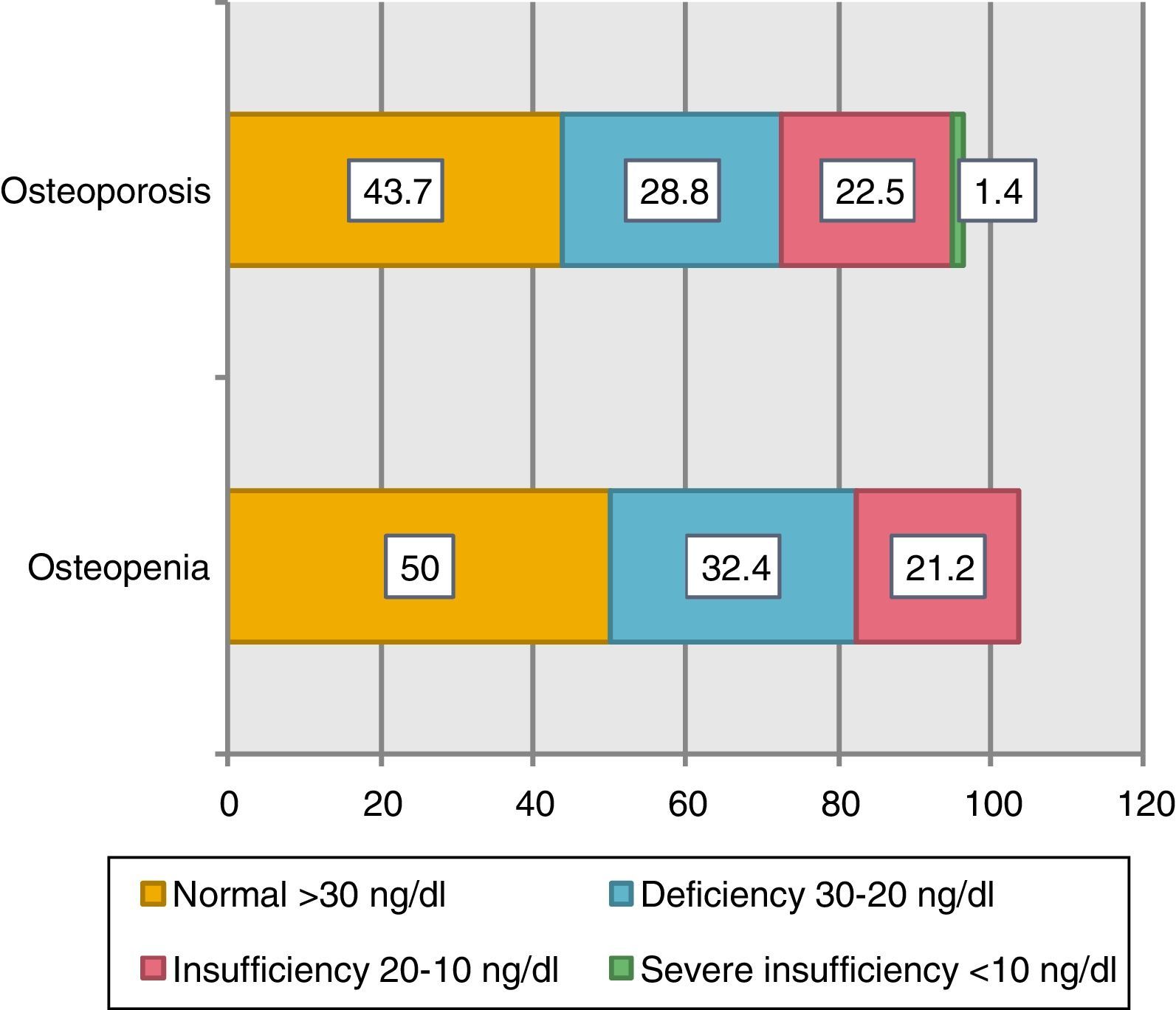
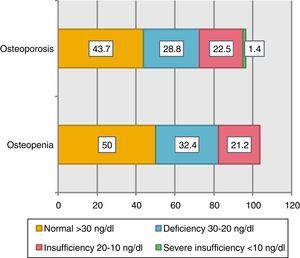
As for the osteoporosis group, 71.4% had hypovitaminosis. Of those patients, 42.9% had deficiency and 28.6% had insufficiency. When the patients with bone densitometry were evaluated, 44.1% [n=123] of the patients had undergone the study, 58% [n=71] had a diagnosis of osteoporosis with a mean age of 67 years and 42% [n=52] diagnosis of osteopenia. When comparing these groups, those with osteoporosis had lower mean vitamin D levels than those with osteopenia (29.9ng/mL vs. 31.0ng/mL) (Fig. 2).
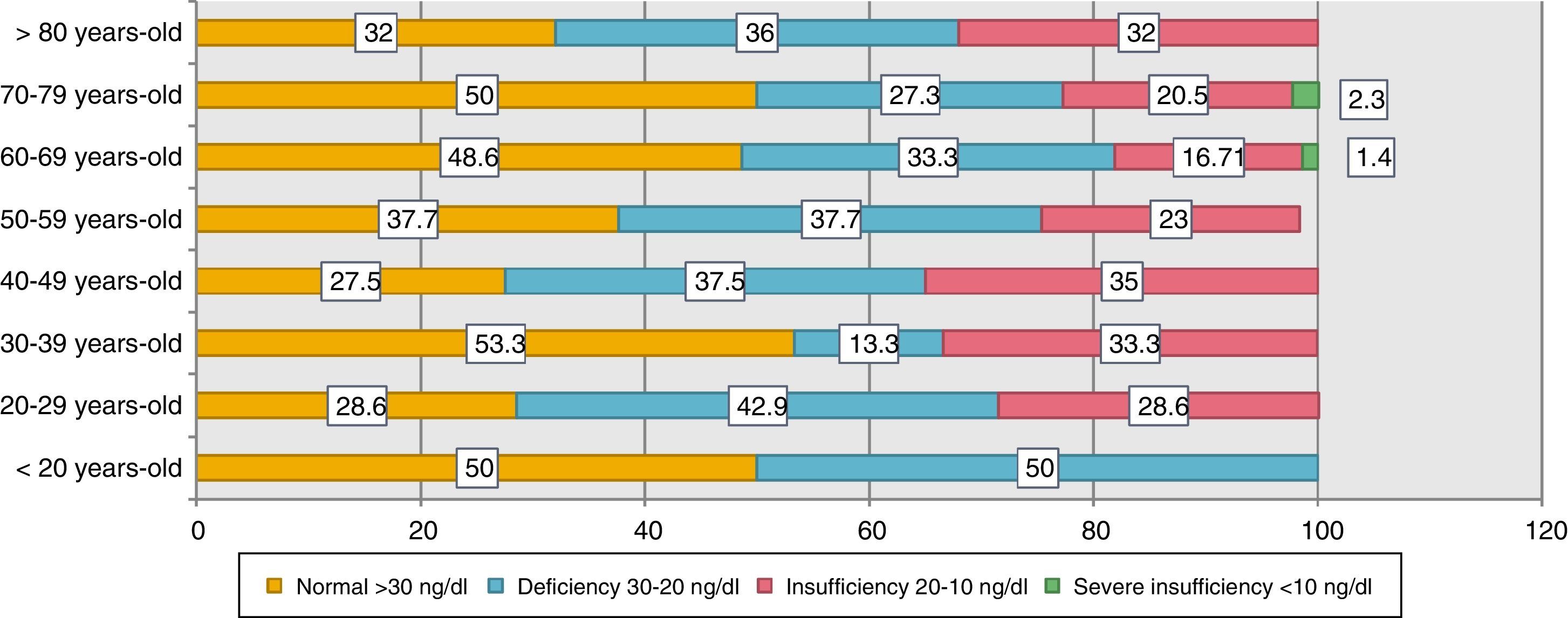
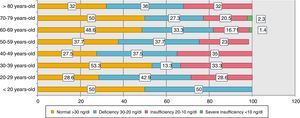
Comparing the means of vitamin D by age groups, it was found that those younger than 20 years had the highest value of vitamin D [32ng/mL] and those between 40 and 49 years had the lowest value with 25.6ng/mL (95% CI, p=0.471). Patients were stratified according to age ranges and vitamin D levels were determined according to their classification (Fig. 3). It is evident that the group with the highest hypovitaminosis D are patients under 20 years of age, which presented levels below 30ng/mL by 50%. The groups that presented higher normal levels of vitamin D were those between 30–39 years and 70–79 years.
DiscussionThe importance of vitamin D in the immune system lies in the increase of innate immunity and multiple regulations of adaptive immunity, this being the beginning of a series of studies demonstrating an association between vitamin D deficiency and an increase in Incidence of autoimmune diseases.15
This is a retrospective study of 25-(OH)-D determination in patients at a rheumatology center. A vitamin D deficiency was evident in 58.8%.
A similar study by Mouyis et al. Determined serum levels of 263 patients attending the outpatient rheumatology clinic, mean vitamin D was 44nmol/L; (rheumatoid arthritis, rheumatism of soft tissues, arthritis, chronic pain, etc.), and those with a diagnosis of osteoporosis/osteopenia (46%), The mean vitamin D in the rheumatic disease group was 39nmol/L and 49nmol/L for the osteoporosis/osteopenia group.16 These results were higher than those reported in our study, where the mean vitamin D for the group of Osteoporosis was 27.4ng/mL and the total studied population was 29.09ng/mL, we believe that this difference is because the patients in our study were not under vitamin D supplementation.
Haroon et al. Studied vitamin D levels in rheumatology clinic patients and found that 70% of the patients had vitamin D deficiency (≤21.2ng/mL) and 26% severe deficiency (≤10ng/mL). According to age, 65% of patients over 65 years had vitamin D deficiency, while patients under 30 years of age 78% had levels below ≤21.2ng/mL,17 data similar to our study where the prevalence of hypovitaminosis in the group of patients aged 20–29 years was 71.5% and in the 60–69 group it was 51.41%, this may be due to the fact that the populations studied were similar.
The mean vitamin D in patients with osteoarthritis was 29.8ng/mL and 53.8% of these patients had vitamin D deficiency, in contrast to the study presented by Mouyis et al. where patients with osteoarthritis had an average vitamin D of 40.4ng/mL, we believe that the difference between the mean is due to the fact that the patients in Mouyis study were under supplementation and regular follow-up regarding the vitamin D levels.16
In the group of patients with rheumatoid arthritis, mean vitamin D was 30.2ng/mL and 69.7% had lower levels of vitamin D, the CARMA study determined vitamin D levels in rheumatic inflammatory diseases, the rheumatoid arthritis group (775) had hypovitaminosis in 40.5% and the mean of the disease was 20.4ng/mL.18
In recent years, the relationship between vitamin D levels and chronic pain syndromes such as fibromyalgia has been discussed. It is believed that the key role of vitamin D is the perception of chronic pain in these patients.19–21 To which vitamin D has been shown to be a bioregulator of pain,21,22 however, more studies are needed to demonstrate these mechanisms in a more precise way, in our study 17 patients were included, of which 76.5% showed having levels below 30ng/mL of vitamin D, the mean of the vitamin was 24.1ng/mL; Maafi et al. studied vitamin D levels in Iranian patients with fibromyalgia, approximately 88.4% had levels below <30ng/mL and the mean vitamin D was 17.24ng/mL23; we hypothesized that the levels of vitamin D in our population of patients with fibromyalgia, were due to the culture of sun protection and the avoidance of prolonged exposure to sunlight, whereas in Maafi study, the studied population was Iranian, where cultural and Religious play a key role because women are accustomed to wear clothing that covers most of the body, decreasing sun exposure and vitamin D metabolism by cutaneous route.
The mean of vitamin D levels in the osteoporosis group was 27.4ng/mL, 42.9% of them were deficient, data higher than those demonstrated by Mouyis et al. Where the mean vitamin D in these patients was 19.6ng/mL.16 Another study presented by Stoll et al. showed an average vitamin D of 25ng/mL in patients with osteoporosis and approximately 69% of them had some degree of hypovitaminosis D.24
It is important to emphasize the prognosis of the patients in this study, since Ecuador is located on the equatorial line at a latitude of −0.95, where the radiation and intensity of the UV rays are greater, however, the general population takes measures to Avoid sun exposure. The intensity of UV radiation will depend on25:
- •
Sun height and UV radiation: In tropical areas like Ecuador the highest radiation intensity occurs around midday and during the summer months (May–December), where the sun reaches its maximum height.
- •
Latitude: The closer to the equator (0°) the more intense the UV radiation.
- •
Cloudiness: Radiation reaches its maximum limit when there are no clouds.
- •
Altitude: The atmosphere is thinner at higher altitudes; it is considered that with every 1000m of altitude increase the intensity of UV radiation increases by 10–12%.
- •
Ozone layer.
- •
Reflection of the soil: The reflection will depend on the type of surface.
Currently there are no epidemiological data on vitamin D in Ecuadorian population according to climatic seasons and sun exposure during the year, however, a study conducted in the village of Atahualpa located on the equatorial coast, determined vitamin D levels in 220 subjects, Of which 25% had levels below 20ng/mL and was directly related to ischemic events and diffuse subcortical brain damage,26 another reason why the determination and management of vitamin D is essential. Within the strengths of this study, we can conclude that the 279 patients were not institutionalized, the determination of vitamin D was performed in a single specialized laboratory with a universal technique, the patients did not receive supplementation and the objectives were reached. Within the limitations of the study, we find the lack of information gathering about the time of solar exposure. However, the study was not altered by these limitations, since the main objective was to determine vitamin D levels in a population of rheumatic patients. In summary, a high incidence of hypovitaminosis was demonstrated in patients attending a rheumatology center, being an important factor in the evaluation of these patients and motivating institutions to create guidelines for the management and treatment of this deficiency.
ConclusionAn increased prevalence of hypovitaminosis D was observed in patients in the rheumatology area, being important the development of specific studies of vitamin D supplementation in rheumatic conditions. This is the first study to determine vitamin D levels in patients attending a rheumatology center in Ecuador.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestsAuthors declare no conflict of interest.