Purtscher-like retinopathy is a rare ocular disease that manifests with sudden loss of vision, associated with a systemic pathology such as systemic lupus erythematosus. We present the case of a 25-year-old male patient with Purtscher-like retinopathy as the first manifestation of systemic lupus erythematosus, evaluated in a high-complexity centre in the city of Medellín, Colombia. Improvement of signs and symptoms was observed after the start of corticosteroids and monthly intravenous cyclophosphamide therapy. We consider prompt ophthalmological evaluation essential in patients with suspected autoimmune diseases, to make an early diagnosis and improve the prognosis.
La retinopatía de Purtscher-like es una enfermedad ocular poco común que se manifiesta con pérdida súbita de la visión, asociada con una patología sistémica como lo es el lupus eritematoso sistémico. Se presenta el caso de un paciente masculino de 25 años, con retinopatía Purtscher-like como primera manifestación de lupus eritematoso sistémico, evaluado en un centro de alta complejidad de la ciudad de Medellín, Colombia. Se observa mejoría de signos y síntomas posteriormente al inicio de corticoesteroides y terapia con ciclofosfamida intravenosa mensual. Se considera fundamental la valoración oftalmológica temprana en pacientes con sospecha de enfermedades autoinmunes, para realizar diagnósticos tempranos y mejorar el pronóstico de los pacientes.
Purtscher retinopathy was described in 1910 by Omar Purtscher in a male patient, after a severe cranioencephalic trauma.1 It is rare ocular disease, associated with a systemic pathology that manifests itself with areas of intraretinal whitening and clearing areas on each side of the retinal arterioles, venules, and precapillary arterioles. This contrast with the cotton wool spots, which have poorly defined borders and lie superficially over the vessels.1,2 On a global scale, it has been described an incidence of the disease of approximately 0.24 cases per million people per year.1
The pathophysiology of this entity is still not clear; an association with an occlusive embolic microvasculopathic component is suggested, with sudden loss of vision after trauma or at the onset of associated systemic diseases such as systemic lupus erythematosus (SLE).3
SLE is a multisystem autoimmune inflammatory disease in which ocular involvement can be one of the first manifestations, with an incidence of 29% in patients with active disease.4
The diagnosis of Purtscher-like retinopathy is essentially clinical, based on the commitment of the visual acuity or the visual fields, after the onset of an associated underlying condition.2
In the ophthalmological examination of the fundus, cotton-wool spots (Purtscher-flecken) are typically found, in addition to retinal hemorrhages.5 Complementary diagnostic aids include optical coherence tomography (OCT), optical coherence tomography angiography (OCT-angio), and fluorescein angiography (FA), which provide essential information for the diagnosis and follow-up of the patients.5
The treatment of this pathology is still not clear, it has been evidenced that there is symptomatic improvement with the use of corticosteroids, but there are reviews that are not conclusive and are based on the opinion of experts. The case of a patient with Purtscher-like retinopathy as the first manifestation of SLE is presented.
Case descriptionA 25-year-old male patient with a 10-month history of isolated hearing loss and progressive alopecia. Eight months later, he began having episodes of global headache, associated with daily objective fever peaks of up to 40° C, with the appearance of painless cervical lymph nodes, accompanied by asthenia, adynamia, myalgia and paresthesia in the lower limbs, in addition to an objective weight loss of approximately 10 kg in two months.
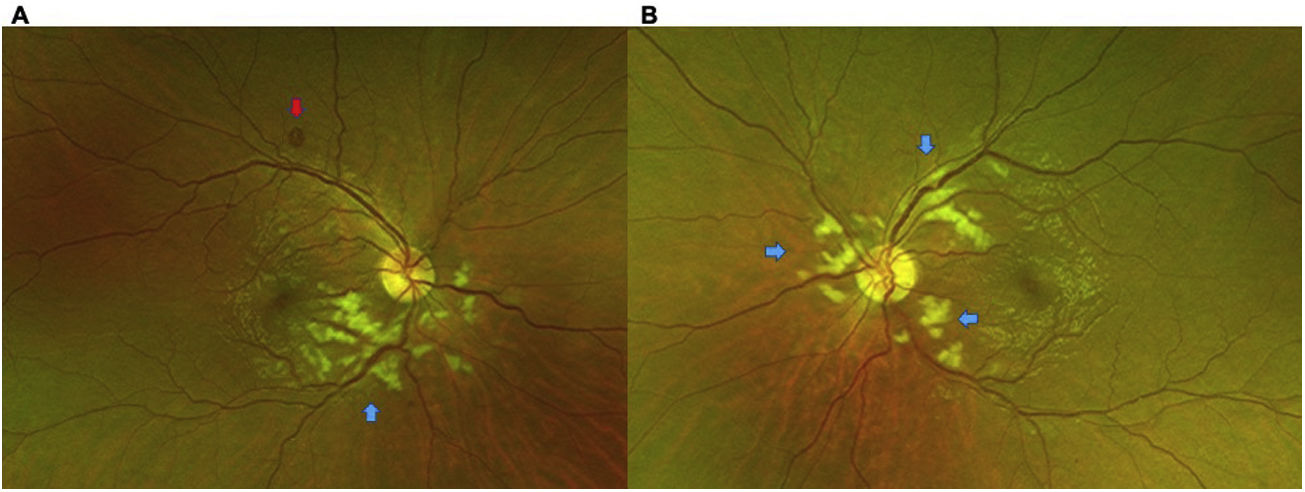
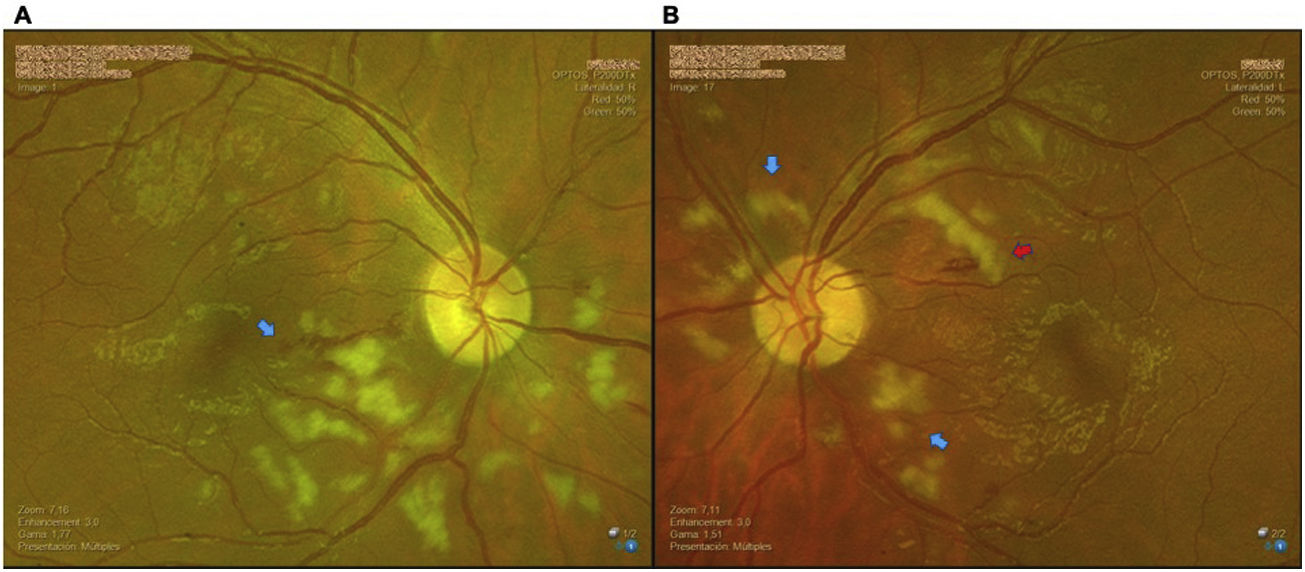
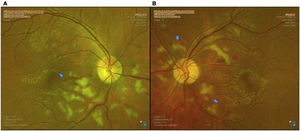
A month later, he began having blurred vision, for which he consulted the Ophthalmology Service of a private clinic in the city of Medellín, Colombia. In the initial ophthalmological examination, he had a visual acuity of 20/25 in the right eye and 20/20 in the left eye, without alterations in the ocular adnexa or in the anterior segment, and with normal intraocular pressure in both eyes. In the eye fundus, the presence of cotton wool spots (Purtscher-flecken) was observed from the optic nerve to the macula in both eyes. In the right eye there was a spot hemorrhage over the superior temporal arcade, with marked vascular dilatation at the lower level (Fig. 1).
(A) Color photo of the right eye: nerve with excavation of 0.1, with defined edges, vessels with dilation of inferior temporal predominance, with rectification at the macular level, peripapillary white cotton wool spots with inferior predominance, hypopigmentation of the retina at the peripapillary level sparing the vessels, corresponding to Purtscher-flecken (blue arrow). Spot hemorrhage towards the superior temporal arcade (red arrow). (B) Color photo of the left eye: nerve with excavation of 0.1, with defined edges, dilated vessels of superior temporal predominance, peripapillary white cotton wool spots, hypopigmentation of the retina at the peripapillary level, sparing the vessels, corresponding to Purtscher-flecken (blue arrows).
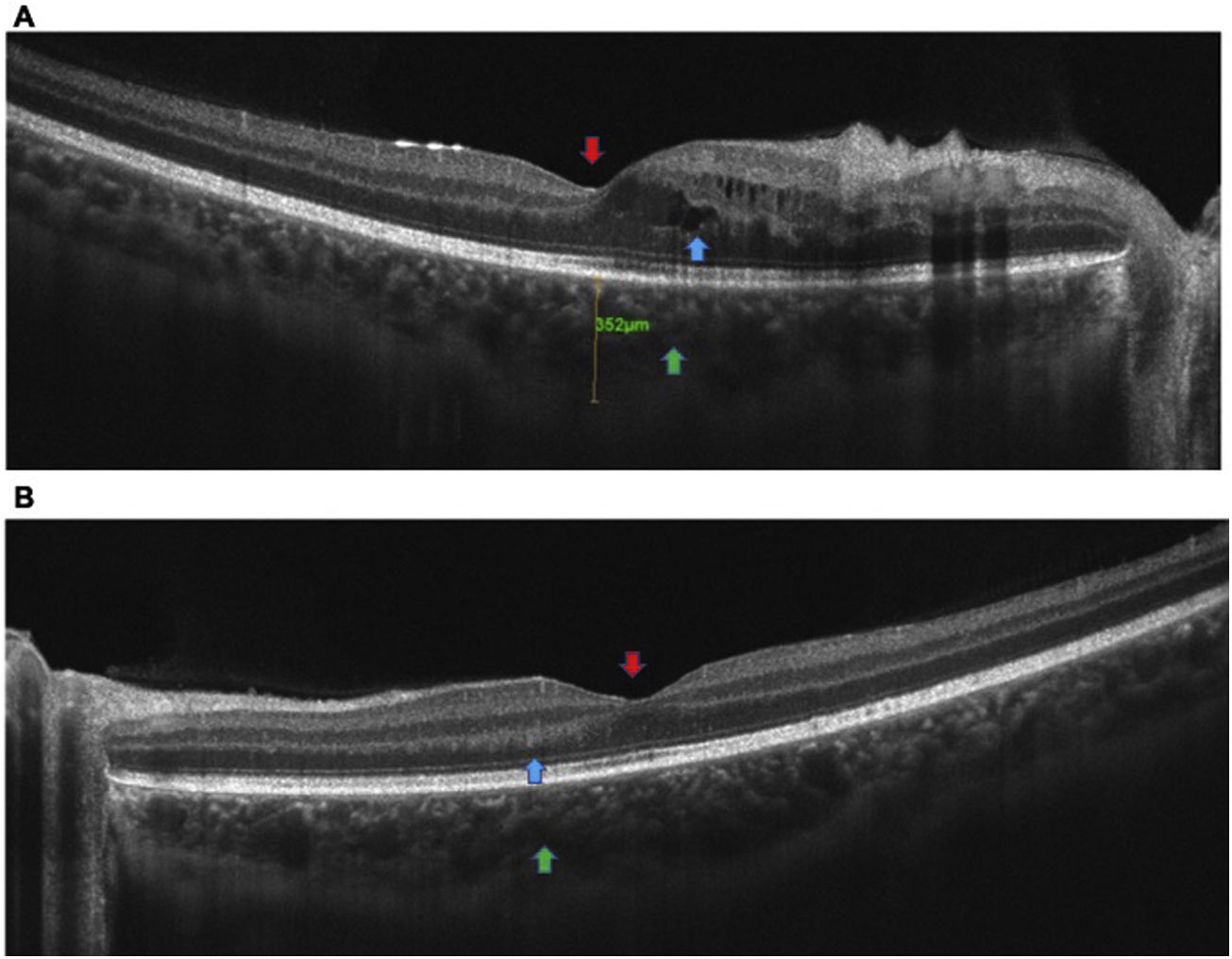
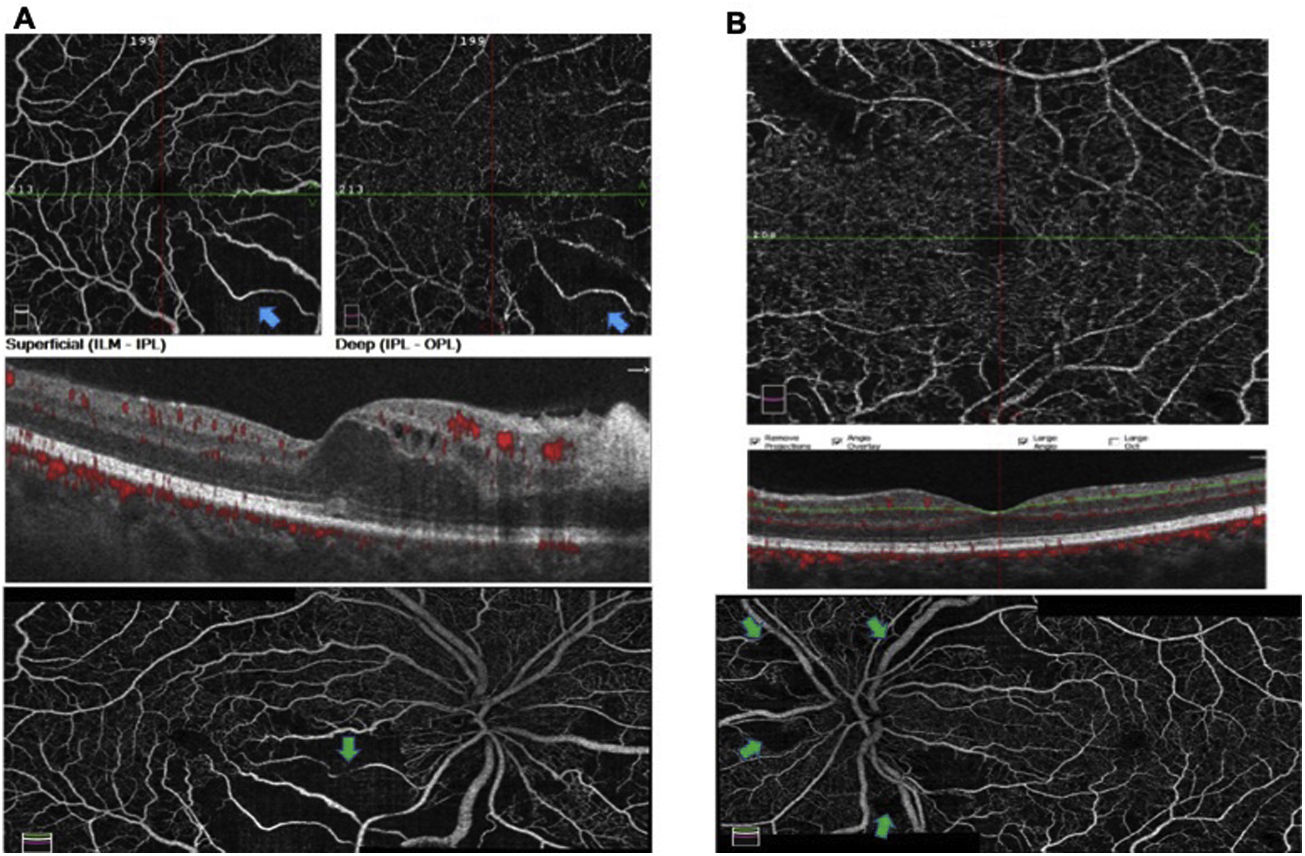
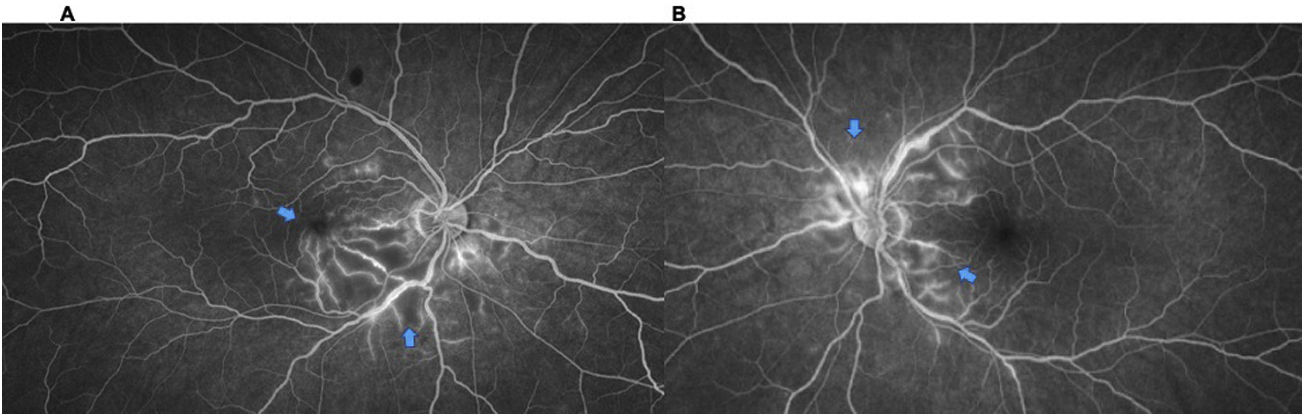
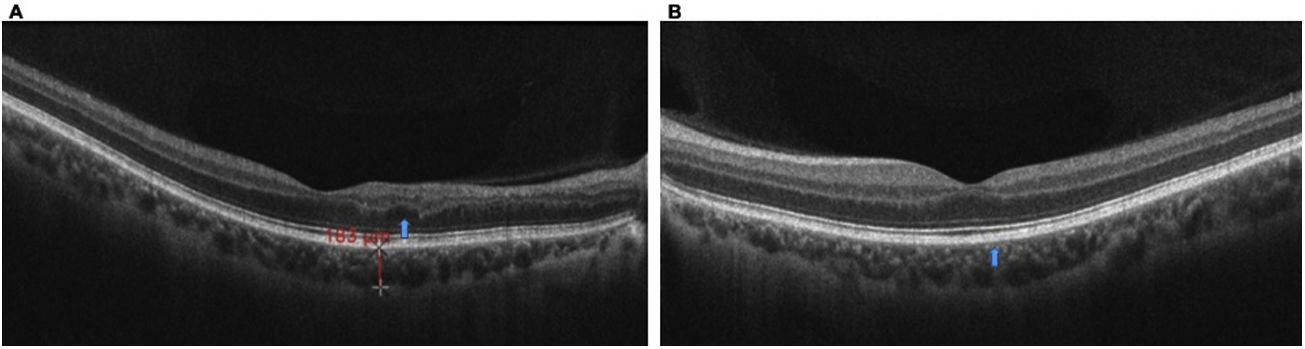
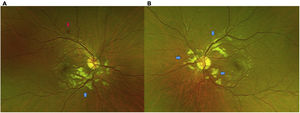
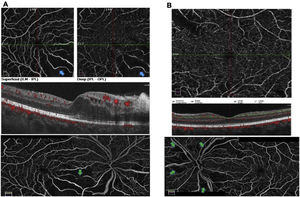
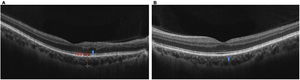
Macular OCT (Fig. 2) and Angio-OCT of both eyes (Fig. 3) were requested, which showed a partial loss of the foveal contour in the right eye, presence of intraretinal cystic lesions with a predominance of the inferonasal sector with foveal compromise, thickening and increased reflectivity of the internal segments of the nasal sector (retinitis vs. vascular congestion), with slightly increased choroidal thickness, but with congestive choriocapillaris and dilation of Haller's vessels. In the left eye, partial loss of the foveal contour, and presence of intraretinal cystic lesions were observed, as well as thickening and increased reflectivity of the internal segments of the nasal sector (retinitis vs. vascular congestion), with slightly increased choroidal thickness, congestive choriocapillaris and dilation of Haller's vessels. The complementary angio-OCT suggested an inferotemporal vascular occlusion with areas of non-perfusion in the right eye and it was recommended to complement studies with fluorescein angiography of both eyes (Fig. 4).
(A) OCT of the right eye: partial loss of the foveal contour (red arrow), presence of intraretinal cystic lesions predominantly in the inferonasal sector with foveal compromise (blue arrow), thickening and increased reflectivity of the internal segments of the nasal sector (vascular congestion), with slightly increased choroidal thickness, but with congestive choriocapillaris and dilation of Haller's vessels (green arrow). (B) OCT of the left eye: partial loss of foveal contour (red arrow), with thickening and increased reflectivity of the internal segments of the nasal sector (blue arrow), with slightly increased choroidal thickness, congestive choriocapillaris, and dilation of Haller's vessels (green arrow).
(A) Angio-OCT of the right eye: areas suggestive of hypoperfusion are observed at the inferonasal macular level, both in the superficial and deep plexus, which correlate with areas of macular edema (blue arrows). OCT-A reconstruction showing peripapillary vascular dilatation, areas suggesting hypoperfusion at the nasal and temporal peripapillary level, as well as at the inferonasal macular level (green arrow). (B) Angio-OCT of the left eye: deep plexus with areas of possible superotemporal hypoperfusion vs. artifacts, explained by whitish lesions. Reconstruction of the OCT-A angiography of the nerve and macula showing predominantly superior vascular dilatation, with peripapillary non-perfusion areas (green arrows).
Fluorescein angiography of both eyes. (A) Right eye: image in late phases in which hyperfluorescence begins to be observed at the venous level of the inferior temporal arcade and macular vessels at the nasal level, with areas of inferonasal macular and peripapillary hypoperfusion and inferonasal (blue arrows). (B) Left eye: angiography image showing peripapillary hypoperfusion at the superior nasal, superior and inferior temporal level, with venous vascular dilation at the superior level, in addition to late venous perivascular staining (blue arrows).
Among the initial paraclinical tests performed there was a negative infectious profile (toxoplasmosis, cytomegalovirus, syphilis, hepatitis C, hepatitis B, human immunodeficiency virus and dengue), negative tuberculin test at 0 (zero) and negative simple chest computed axial tomography (CAT). The patient presented a normal peripheral blood smear, and normal renal and hepatic profiles, however, high lactate dehydrogenase levels are noteworthy, associated with positive antinuclear antibodies with a 1:160 speckle pattern, positive anti-Smith (Sm) antibodies, C3 hypocomplementemia and lymphopenia, with no other associated cytopenias. In addition, he presented a positive direct Coombs test, with no evidence of hemolysis. It was decided to hospitalize him for evaluation and studies.
Subsequently, a contrasted nuclear magnetic resonance of the skull was carried out, which showed cortical atrophy and scarce diffuse periventricular hyperintensities, without signs of demyelinating pathology. Lumbar puncture with cerebrospinal fluid (CSF) within normal limits, with negative India ink and KOH in CSF. The contrast-enhanced CT of the neck shows small lymph nodes of 5 mm in stations II and V, without a conglomerate of lymphadenopathies. The contrast-enhanced chest CT reveals small right paratracheal nodes smaller than 5 mm, while the contrast-enhanced abdominal CT reveals bilateral inguinal nodes measuring 5 mm in their short axis. The electromyography of the lower limbs shows isolated left anterior tibial denervation due to fibular nerve involvement.
Additional studies were performed to rule out antiphospholipid syndrome, with negative IgM and IgG anticardiolipin antibodies, negative beta 2 glycoprotein 1 IgM and IgG, and negative lupus anticoagulant. The validation report for IgM antiphospholipid antibodies was negative (beta 2 glycoprotein I, cardiolipin, phosphatidyl serine, phosphatidyl inositol, and phosphatidic acid).
ResultsWith all of the above and taking into account the revised criteria of the European League Against Rheumatism (EULAR) and the American College of Rheumatology (ACR), a diagnosis of de novo SLE was established and management was started with pulses of methylprednisolone 500 mg, intravenously (IV), every 24 h, for three doses, continuing with 50 mg, every 24 h, orally, plus chloroquine 150 mg, every 24 h, orally.6
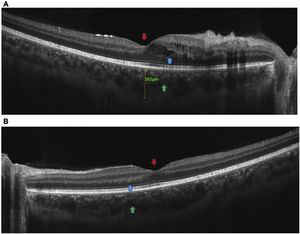
After the intravenous (IV) steroid pulses, the patient reported improvement in his visual symptoms, however, in subsequent ophthalmological evaluations, mild hemorrhagic changes were also found in the left eye, with a visual acuity of 20/20 in both eyes (Fig. 5). Consequently, it was decided to start cyclophosphamide boluses of 750 mg, IV.
Control color photographs of both eyes one week after the initiation of treatment. (A) Right eye: persistence of vessels with dilation of inferior temporal predominance, with rectification at the macular level, peripapillary white cotton wool spots predominantly inferior, and hypopigmentation of the retina at the peripapillary level, sparing the vessels, corresponding to Purtscher-flecken (blue arrow). (B) Left eye with mild hemorrhagic changes (red arrow). Persistence of dilated vessels of superior temporal predominance, peripapillary white cotton-wool spots, hypopigmentation of the retina at the peripapillary level, sparing the vessels, corresponding to Purtscher-flecken (blue arrows).
The patient was followed up and a marked improvement in the retinal findings was observed three months after the start of the established therapy (corticosteroids and monthly IV cyclophosphamide), with control OCT of the macula with evidence of decreased edema at the nasal level in the right eye, and in the ophthalmological examination, visual acuity with a pinhole of 20/20 was found in the right eye (previous 20/25), and in the left eye with a pinhole of 20/20-2 (previous 20/20), without alterations in ocular adnexa or anterior segment and intraocular pressure within normal limits in both eyes (Fig. 6). When evaluating the fundus, slight cotton-wool spots and punctate hemorrhages were found at the inferior peripapillary level in the right eye, with a healthy macula and healthy peripheral retina, while in the left eye slight cotton-wool spots were observed in the inferotemporal area, with a healthy macula and peripheral retina.
OCT of the macula in both eyes: control images after three months of follow-up. (A) Right eye: macula with alteration of the linear continuity of the layers of the juxtafoveal external retinal plexus, without involvement of the ellipsoid zone, with high reflectivity of the RPE/choriocapillaris complex with minimal atrophic changes (blue arrow). (B) Left eye: macula with normal architecture, with high reflectivity of the RPE/choriocapillaris complex and minimal atrophic changes (blue arrow).
Purtscher-like retinopathy is a rare entity that presents with severe angiopathy, characterized by confluent lesions of cotton wool spots in the posterior pole, associated with retinal hemorrhages, with sudden decrease in visual acuity in the context of a systemic disease, in this case SLE.5
The exact mechanism of this entity remains unclear, current evidence suggests an association with an occlusive embolic microvasculopathic component, mainly of precapillary arterioles, with sudden loss of vision after trauma or at the onset of special systemic diseases. Similar retinal findings have been described in a wide range of pathologies such as pancreatitis, renal failure, and autoimmune diseases such as SLE, among others.7,8
In patients with a diagnosis of SLE, retinopathy usually manifests in those with active disease and is commonly associated with antiphospholipid syndrome. The presence of antiphospholipid antibodies alone or in association with SLE increases the risk of retinopathy.9
The diagnosis of Purtscher-like retinopathy is clinical, with a broad presentation that ranges from sudden loss of vision in hours or days to loss of central or paracentral visual fields or arcuate scotomas, usually with preserved peripheral vision, after the start of an associated underlying pathology.2
The signs found in the fundus include cotton-wool spots (Purtscher-flecken), generally bilateral, in addition to retinal hemorrhages that have been described in up to 83–92% of the cases.5
Wu et al. reported a case series of Purtscher-like retinopathy in patients previously diagnosed with SLE between the years 2002 and 2013. In the eye fundus they found Purtscher-flecken lesions, cotton-wool spots, retinal hemorrhages, macular edema, optic disc edema and a pseudo-cherry red spot. The abnormalities of the fluorescein angiography include areas of capillary nonperfusion, late leak, peripapillary staining, precapillary occlusion, and slow vessel filling.10
Li et al. described extensive non-perfusion macular areas on angio-OCT, with compromise of internal and deep capillary plexuses, OCT with macular edema, and AF with non-perfusion areas, retinal ischemia, and slow vessel filling. Some recent studies have demonstrated cystoid macular edema and associated subretinal fluid.11 In our case, the OCT and the angiography revealed mild cystoid macular edema, with partial loss of foveal contour, slightly increased choroidal thickness, congestive choriocapillaris, dilated vessels of Haller, and inferotemporal vascular occlusion with areas of nonperfusion.
Differential diagnoses to consider include occlusion of the central retinal artery or branch, commotion retinae, and fat embolism. The association with other systemic diseases such as HIV retinopathy, which also presents with cotton wool spots, must also be ruled out.2
At present, there are no clinical guidelines in the literature that guide the treatment of these patients, so management has been based on expert opinion, in which two strategies or lines of management are observed: administration of corticosteroids or immunosuppressants vs. follow-up without pharmacological treatment, since it is considered that the course of the disease tends to be self-limited. Significant improvement has been shown with the use of corticosteroids, but there are reviews that are not conclusive, since a homogenization of the patients and the triggering pathologies is required.2,12
Our case report illustrates the natural history of Purtscher-like retinopathy associated with systemic disease of SLE-type, which due to its clinical presentation, manifestations, and ophthalmological findings, led us to think of this pathology, with improvement of signs and symptoms after the initiation of corticosteroids and monthly intravenous cyclophosphamide boluses.9
ConclusionsIt is a case of Purtscher-like retinopathy with bilateral occlusive vasculitis, whose ocular involvement and early ophthalmological evaluation guided and made possible the diagnosis of de novo SLE, as well as the initiation of treatment in a timely manner in a young patient.
We consider essential the complete ophthalmological evaluation in patients with suspected autoimmune diseases, since certain ophthalmological findings are the first manifestation of some systemic diseases, which can lead us to make early and comprehensive diagnoses in order to improve the prognosis of our patients.
Ethical considerationsThe authorization and signature of the informed consent was obtained from the patient and from the Ethics Committee of the institution. The ethical code of the WHO (Declaration of Helsinki) on experiments on humans was followed, respecting the right to privacy.
FundingThis work has not received any type of funding.
Conflict of interestThe authors declare that they have no conflict of interest.