The case is described of a young man with severe acute renal failure, with anuria and toxic hyperkalaemia toxic related to rhabdomyolysis after physical aggression, and had gone unnoticed on two previous visits to the Emergency Service, and subsequently aggravated by amphetamines. This case illustrates the need to consider rhabdomyolysis in patients with any degree of muscular aggression.
Describimos el caso de un varón joven, con un fracaso renal agudo anúrico severo e hiperpotasemia tóxica, relacionados con una rabdomiólisis tras una agresión física y que había pasado desapercibida en 2 visitas previas a Urgencias y, posteriormente, agravada por consumo de anfetaminas. Este caso ilustra la necesidad de considerar la posibilidad de una rabdomiólisis ante paciente con cualquier grado de daño muscular.
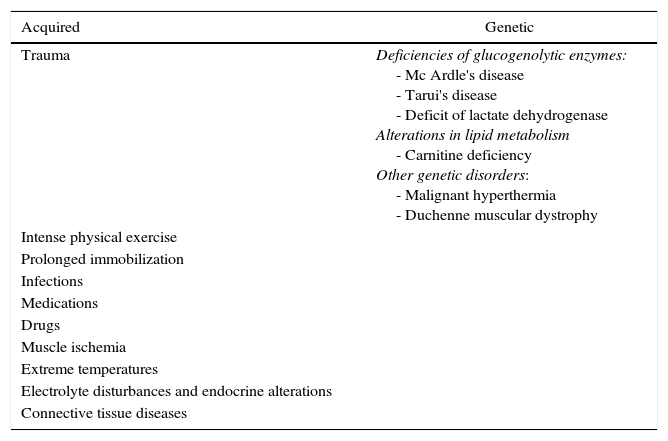
Rhabdomyolysis is a condition characterized by necrosis of the muscles and release of the intracellular components of the muscle into the systemic circulation.1 It is a common condition with different causes that are summarized in Table 1.2 Its clinical manifestations are varied: from asymptomatic elevations of muscle enzymes to life-threatening complications.3 We describe the case of a young man with severe complications associated with an extreme rhabdomyolysis due to a physical aggression, which could have gone unnoticed the days after the assault, and aggravated by the consumption of toxic substances (amphetamines).
Leading causes of rhabdomyolysis.
| Acquired | Genetic |
|---|---|
| Trauma | Deficiencies of glucogenolytic enzymes: - Mc Ardle's disease - Tarui's disease - Deficit of lactate dehydrogenase Alterations in lipid metabolism - Carnitine deficiency Other genetic disorders: - Malignant hyperthermia - Duchenne muscular dystrophy |
| Intense physical exercise | |
| Prolonged immobilization | |
| Infections | |
| Medications | |
| Drugs | |
| Muscle ischemia | |
| Extreme temperatures | |
| Electrolyte disturbances and endocrine alterations | |
| Connective tissue diseases |
A 38 year-old male, of Bulgarian origin, who a few years before had been in the Emergency Room on two occasions (with other filiation data), being apparently a victim of a physical aggression (he was punched and beaten with sticks in a generalized way) and was diagnosed with multiple bruises being discharged with analgesia with paracetamol. The patient was brought to the Emergency Service for the third time, 6 days after the initial physical aggression, due to impossibility to move. The anamnesis in this new visit to the Emergency Room was impossible, due to restlessness and agitation, as well as language difficulties.
The physical examination upon his arrival to the ER was: blood pressure 82/61mmHg, heart rate 83bpm. Multiple excoriations were detected, primarily on the forehead, the right elbow and pretibial areas, as well as hematomas in the left hemithorax and the 9–12 lateral costal arches. The rest of the physical examination was normal.
The laboratory analyses upon his arrival showed creatinine 13.6mg/dl, sodium 118mmol/l, potassium 8.1mmol/l, magnesium 3.7mg/dl, glucose 134mg/dl, creatine phosphokinase (CPK) 343,115U/l, troponin T 129pg/ml, amylase 502U/l, pH 7.09, bicarbonate 10mmol/l, hematocrit 39.5%, leukocytes 15,760, platelets 87,000, coagulation study normal. Systematic urine analysis: blood +++; toxic substances in urine: positive for amphetamines.
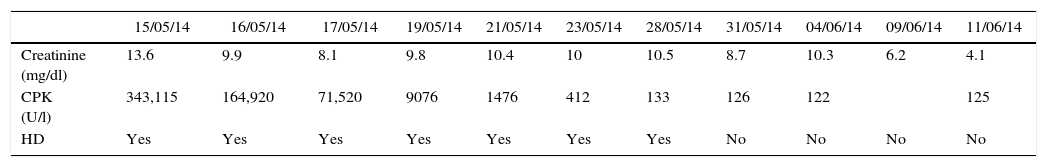
Signs of toxic hyperkalaemia (widening of the QRS complex, peaked T waves in all leads) were detected in the electrocardiogram. Given the gravity of the situation, due to the electrolyte disorders with electrocardiographic repercussion and the acute renal failure, we contacted the Nephrology Department in order to start renal replacement therapy with hemodialysis through a catheter in the right femoral vein and, subsequently, to study the etiology of the acute renal failure. Once he started to be dialyzed we received the rest of the results of the ordinary analyses: calcium 4.4mg/dl, phosphorus 19.2mg/dl, iPTH 619pg/ml, cholesterol 244mg/dl, triglycerides 310mg/dl, GOT 1578U/l, GPT 1030U/l, GGT 35U/l, LDH 11096U/l, albumin 3.8g/dl, C-reactive protein 4.9mg/dl; the immunological study (ANA, ANCA, immunoglobulins, complement) was normal. The serology for B, C and HIV virus was negative. Therefore, once clarified the situation that a previous trauma had existed, along with the analytical findings that we detected, with elevation of CPK and other liver enzymes, it was reached the diagnosis that the acute renal failure was due to a severe rhabdomyolysis of traumatic origin. Perhaps the consumption of amphetamines was a further cause of rhabdomyolysis in our patient; however, we cannot accurately reflect neither the amount nor the time of consumption of this substance, since the patient never informed of its consumption, and it was when positivity for amphetamines was detected in the toxicological analysis of the urine when we considered this etiology of rhabdomyolysis. The subsequent evolution of renal function and CPK is shown in Table 2. One month after admission, with the clinical and renal function improvement, he was discharged with a serum creatinine of 4mg/dl with views to a follow-up on an outpatient basis, to which he did not attend and therefore we do not know the final situation of the renal function.
Evolution of renal function and CPK.
| 15/05/14 | 16/05/14 | 17/05/14 | 19/05/14 | 21/05/14 | 23/05/14 | 28/05/14 | 31/05/14 | 04/06/14 | 09/06/14 | 11/06/14 | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Creatinine (mg/dl) | 13.6 | 9.9 | 8.1 | 9.8 | 10.4 | 10 | 10.5 | 8.7 | 10.3 | 6.2 | 4.1 |
| CPK (U/l) | 343,115 | 164,920 | 71,520 | 9076 | 1476 | 412 | 133 | 126 | 122 | 125 | |
| HD | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | No | No | No |
CPK, creatine phosphokinase; HD, hemodialysis.
Rhabdomyolysis is a condition characterized by the breakdown of the skeletal muscle, and as a consequence of this, the release of the intracellular contents into the systemic circulation (CPK, LDH and transaminases, among other components).3 For this reason, is usually diagnosed by an elevation of CPK levels (generally 5 times their normal level, approximately 1000U/l).4,5 Many causes can contribute to its occurrence: trauma, medications, drugs, infectious processes, metabolic disorders and connective tissue diseases, among others.2,6 In this case that we expose, we believe that the most likely primary cause of the rhabdomyolysis was the severe physical aggression that the patient had received a few days before (with generalized punches and blows), indeed, the beating was the main reason why the patient had gone to the Emergency Service on two previous occasions (and in these two visits there was no evidence of a state of agitation and restlessness). And perhaps the consumption of toxic substances (amphetamines),7,8 could have secondarily contributed (in a patient who already had a muscle destruction due to the previous trauma), to aggravate the muscle damage.
As pointed out previously, many causes can contribute to rhabdomyolysis and a pathogenic pathway common to all causes is the depletion of ATP and secondarily the dysfunction of the ATP-dependent pumps such as Na/K-ATPase and calcium-ATPase. As a consequence of this, there is an increase in intracellular free calcium that leads to the destruction of myocytes. By the release of muscle components into circulation, the excess of myoglobin produces an obstruction of the renal tubules and thus an acute renal failure occurs.3
For the diagnosis of rhabdomyolysis is required a high degree of suspicion in order that this condition does not go unnoticed, since its associated complications (arrhythmias, electrolyte disturbances…) can be lethal.2 In our case, the diagnosis of rhabdomyolysis was made concomitantly with the appearance of all its severe associated complications (anuric acute renal failure, metabolic acidosis, hyperkalaemia, hypocalcaemia and hyperphosphataemia).
The recognition time of rhabdomyolysis is the key to its treatment.9 In a recent study of systematic review of the literature to evaluate the evidence-based recommendations to prevent the acute renal failure associated with rhabdomyolysis, it was concluded that the administration of intravenous fluids should be started as soon as possible, preferably within the first 6h of the muscle damage and reach a urine volume in adults of 300ml/h or more, at least, in the first 24h.10
Regarding the clinical factors that predict the occurrence of acute renal failure, the study of Chen et al.,11 suggests that an initial value of 600ng/dl of myoglobin is a predictor of acute renal failure. In our case, such preventive measures had not been considered on the previous days in his visits to the Emergency Room (since the degree of physical aggression was possibly underestimated and, therefore, the possibility of rhabdomyolysis was not considered). In addition, the muscle damage could have been aggravated subsequently by the consumption of toxic substances (amphetamines), together with the absence of a recommendation for an adequate hydration.
In conclusion, in patients with any degree of muscle damage we should not ignore the possibility of rhabdomyolysis, since its knowledge and the early institution of therapeutic measures could be useful to prevent the onset of serious complications associated, such as those presented in this case.
Ethical responsibilitiesProtection of people and animalsThe authors declare that no experiments were performed on human beings or animals for this research.
Data confidentialityThe authors state that patient data do not appear in this article.
Right to privacy and informed consentThe authors state that patient data do not appear in this article.
FundingThere is no funding.
Conflict of interestThe authors declare that they have no conflict of interest.
Please cite this article as: Heras M, Callejas R, Rodríguez MA, Molina Á, Fernández-Reyes MJ. Rabdomiólisis severa tras una agresión física y agravada por anfetaminas. Rev Colomb Reumatol. 2016;23:44–46.