Uveitis is inflammation of the middle layer of the uveal tract. The paediatric population is at risk of chronic evolution and permanent visual loss.
ObjectivesTo characterize children diagnosed with uveitis in 5 institutions in Bogotá city, evaluated by the paediatric rheumatology and ophthalmology service.
Materials and methodsA retrospective cohort study in children with a previous uveitis diagnosis between January 2015 and January 2018 in 5 Institutions of Bogotá. A univariate and bivariate analysis of the demographic, clinical characteristics, complications, treatment, and evolution of the disease was performed.
Results91 patient histories were analysed. Of the patients, 51.65% were male. The average age was 8.44 years (SD 3.66 years). Bilateral presentation (63.74%), intermediate location (35.16%), and uveitis (25.27%) were more frequent. Idiopathic and infectious aetiology predominated in intermediate uveitis. Bilateral presentation was greater in intermediate uveitis and unilateral in anterior uveitis. Unilateral involvement was more frequent in idiopathic aetiology (42.1%) and bilateral in autoimmune aetiology (60%) (p=0.005). Uveitis associated with juvenile idiopathic arthritis, corresponded to 45.2% of those secondary to autoimmunity. Infectious aetiology was more frequent in boys, while autoimmune aetiology was more frequent in girls. The most frequent infectious cause was tuberculosis in 44%. Of the children, 25.7% arrived with some complications on admission: 69.5% synechiae, 30.5% retinal detachment, and 26% glaucoma.
ConclusionsPaediatric uveitis is an important disease in children, in our study the most frequent cause was idiopathic followed by an autoimmune disorder and infection. Almost half the patients had associated complications with a major impact on the children’s lives.
La uveítis es la inflamación de la capa media del tracto uveal, la población pediátrica afectada por esta enfermedad tiene riesgo de evolución crónica y pérdida visual permanente.
ObjetivosCaracterizar a los niños diagnosticados con uveítis en cinco instituciones ubicadas en Bogotá, evaluados por el servicio de reumatología pediátrica y oftalmología.
Materiales y métodosEstudio de tipo cohorte retrospectiva en niños con diagnóstico de uveítis anterior entre enero del 2015 y enero del 2018, en 5 instituciones de Bogotá. Se llevó a cabo un análisis univariado y bivariado de las características demográficas y clínicas, de las complicaciones, del tratamiento y de la evolución de la enfermedad.
ResultadosSe analizaron 91 historias de pacientes, el 51,65% de los cuales fue masculino, en tanto que la edad promedio fue de 8,44 años (DE=3,66 años). Fueron más frecuentes la presentación bilateral (63,74%), la localización intermedia (35,16%) y la panuveítis (25,27%). La etiología idiopática e infecciosa predominó en la uveítis intermedia, mientras que el compromiso bilateral fue mayor en la uveítis intermedia y unilateral que en la uveítis anterior. El compromiso unilateral fue más frecuente en la etiología idiopática (42,1%), en tanto que fue predominantemente bilateral en la etiología autoinmune (60%) (p=0,005). La uveítis asociada a artritis idiopática juvenil correspondió al 45,2% de las secundarias a autoinmunidad. La uveítis infecciosa fue más frecuente en niños, mientras que en las niñas lo fue la autoinmune. La causa infecciosa más frecuente fue tuberculosis (44%). El 25,7% llegó con alguna complicación al ingreso: sinequias (69,5%), desprendimiento de retina (30,5%) y glaucoma (26%). Al final del seguimiento, el 44% de los pacientes tuvo manejo con corticoide oral, el 64% manejo inmunosupresor no biológico (80% metotrexate) y el 30% terapia biológica.
ConclusionesLa uveítis es un proceso inflamatorio intraocular que afecta a la población pediátrica. En este estudio se encontró mayor frecuencia de etiología idiopática, seguida de la autoinmune e infecciosa, como se ha descrito en la literatura. Cerca de la mitad de los pacientes presenta complicaciones, con importantes implicaciones en la calidad de vida.
Uveitis is inflammation of the middle layer of the eye or uveal tract, which includes the iris, ciliary body, and choroid.1 Uveitis is classified, according to location, into anterior (synonymous with iritis), intermediate (iridocyclitis), posterior (choroiditis, retinochoroiditis, and chorioretinitis), and panuveitis.2 It can occur isolated or in the context of systemic diseases; the most frequent causes are infectious, autoimmune, or idiopathic.1–3
In the pediatric age, its prevalence is 5%–10%. Children and adolescents are more likely to experience severe chronic inflammation and, consequently, a higher risk of developing ocular complications and permanent vision loss.3,4
Many times, uveitis is diagnosed by an abnormal finding during a routine check-up or because the child has already developed significant visual impairment.1 During the ophthalmologic evaluation, in addition to assessing visual acuity, disease severity, and complications in each eye, a slit-lamp examination is required to classify uveitis according to uveitis nomenclature standardization criteria (SUN). Establishing the etiology (infectious or non-infectious) is the most important consideration to direct treatment. For this reason, it the patient must be clinically evaluated to determine if there is any systemic involvement. Within the group of non-infectious uveitis, an idiopathic form is included, which are those in which, despite exhaustive investigation, no etiologic factor has been identified, including autoimmune etiology, which may be associated with the presence of autoantibodies, susceptibility genes (HLA B-27), or an established autoimmune disorder such as Juvenile Idiopathic Arthritis (JIA) or sarcoidosis, among others. Hence, the assessment of these patients by a multidisciplinary team that includes the ophthalmologist and pediatric rheumatologist is crucial.
The objective of this study was to characterize children diagnosed with uveitis from 5 institutions in the city of Bogota, Colombia evaluated by the pediatric rheumatology service.
Materials and methodsA multicenter retrospective cohort study was conducted. The medical records of patients diagnosed with uveitis between January 2015 and January 2018, in 5 institutions in Bogota, Colombia, were reviewed. Patients under 18 years of age referred for assessment by pediatric rheumatology were included, all of them with consultation for a clinical diagnosis of uveitis and follow-up by pediatric ophthalmology and rheumatology.
Demographic and etiological variables of the disease were analyzed, as well as complications detected during diagnosis, follow-up, evolution, and treatment. In addition, a univariate and bivariate analysis was carried out according to the type and complications of the disease. Comparisons of qualitative variables were performed using the chi-square or Fisher’s exact tests, and in the case of quantitative variables, the T-test was employed for the mean difference in independent samples, and Mann–Whitney’s U-test was used depending on the nature of data (parametric or non-parametric). These data were classified in Microsoft Excel and processed in the SPSS software, version 21.
Ethical considerationsAll data collection procedures were treated confidentially, following the Helsinki Declarations5 and national regulations (Resolution 8430 of 1993), which classifies this study as risk-free research.6
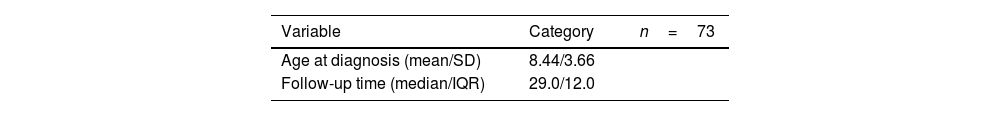
ResultsA total of 91 patients’ records diagnosed with uveitis were analyzed, the follow-up time had a median of 12 months (IQR: 29), while the male: female ratio was 1:1.06, with a male percentage of 51.65%. The average age at diagnosis was 8.44 years (SD=3.66), with bilateral involvement in 63.74% of cases, while the most frequent locations were intermediate (35.16%) and panuveitis (25.27%) (Table 1).
Demographic and disease characteristics in children diagnosed with uveitis.
| Variable | Category | n=73 |
|---|---|---|
| Age at diagnosis (mean/SD) | 8.44/3.66 | |
| Follow-up time (median/IQR) | 29.0/12.0 |
| n | % | |
|---|---|---|
| Sex | ||
| Male | 47 | 51.65 |
| Female | 44 | 48.35 |
| Laterality | ||
| Bilateral | 58 | 63.74 |
| One-sided | 25 | 27.47 |
| No data | 8 | 8.79 |
| Etiology | ||
| Idiopathic | 32 | 35.96 |
| Infectious | 26 | 29.21 |
| Autoimmune | 31 | 34.83 |
| Location | ||
| Anterior | 22 | 24.18 |
| Posterior | 7 | 7.69 |
| Intermediate | 32 | 35.16 |
| Panuveitis | 23 | 25.27 |
| No data | 7 | 7.69 |
SD: standard deviation; IQR: interquartile range.
Table 2 depicts that posterior uveitis was more frequent in males, while idiopathic and infectious etiology were more frequent in intermediate uveitis. Regarding laterality, in the case of intermediate uveitis and panuveitis, they were more frequently bilateral, while anterior and posterior uveitis were more frequently unilateral.
Distribution of frequencies of the location of uveitis according to sex, etiology, and laterality at the time of diagnosis.
| Variable | Categories | Location | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Anterior | Intermediate | Panuveitis | Posterior | p* | ||||||
| n | % | n | % | n | % | n | % | |||
| Sex | Male | 12 | 26.7 | 17 | 37.8 | 11 | 24.4 | 5 | 11.1 | 0.75 |
| Female | 10 | 25.6 | 15 | 38.5 | 12 | 30.8 | 2 | 5.1 | ||
| Etiology | Idiopathic | 8 | 25.8 | 13 | 41.9 | 9 | 29 | 1 | 3.2 | 0.53 |
| Infectious | 4 | 16.7 | 10 | 41.7 | 8 | 33.3 | 2 | 8.3 | ||
| Autoimmune | 9 | 33.3 | 9 | 33.3 | 5 | 18.5 | 4 | 14.8 | ||
| Laterality | Bilateral | 11 | 19.6 | 26 | 46.4 | 17 | 30.4 | 2 | 3.6 | 0.07 |
| Unilateral | 8 | 38.1 | 5 | 23.8 | 5 | 23.8 | 3 | 14.3 | ||
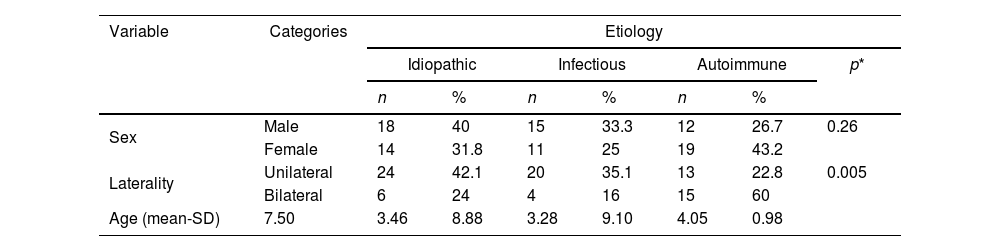
Table 3 shows the distribution of uveitis according to etiology; it is found that infectious etiology was more frequent in boys and autoimmune cause in girls. Unilateral involvement was more frequent in idiopathic etiology (42.1%), while bilateral affection predominates in autoimmune etiology (60%), with statistically significant differences (p=0.005). The earliest age of presentation was recorded in idiopathic origin with a mean of 7.50 years (SD=3.46).
Distribution of frequencies of the etiology of uveitis according to sex, laterality, and age at the time of diagnosis.
| Variable | Categories | Etiology | ||||||
|---|---|---|---|---|---|---|---|---|
| Idiopathic | Infectious | Autoimmune | p* | |||||
| n | % | n | % | n | % | |||
| Sex | Male | 18 | 40 | 15 | 33.3 | 12 | 26.7 | 0.26 |
| Female | 14 | 31.8 | 11 | 25 | 19 | 43.2 | ||
| Laterality | Unilateral | 24 | 42.1 | 20 | 35.1 | 13 | 22.8 | 0.005 |
| Bilateral | 6 | 24 | 4 | 16 | 15 | 60 | ||
| Age (mean-SD) | 7.50 | 3.46 | 8.88 | 3.28 | 9.10 | 4.05 | 0.98 | |
In the case of autoimmune uveitis, defined as those subjects with diagnoses of autoimmune disease or antibody positivity, 45.2% (n=14) were associated with JIA. The most frequent subtype was oligoarticular (65%), where 78% were female and 40% had positive antinuclear antibodies (ANA). The other subtypes found were HLA-B27 enthesitis-related arthritis (positive in 22%), systemic (ANA-negative), and psoriatic (ANA-positive) arthritis (one case each).
In the remaining 54.8% of the cases of autoimmune etiology, 47% were ANA-positive, 37.5% were HLA-B27 positive, and 6.5% were positive for both. None of the individuals had positive rheumatoid factor; there was one patient with Behcet’s disease and another with sarcoidosis.
Regarding the infectious etiology (29.21%), it was observed that the most frequent cause was tuberculosis (44%); all patients were assessed by pediatric infectious diseases, which confirmed the diagnosis and initiated anti-tuberculosis therapy (Table 4).
When evaluating the complications, it was found that 25.7% (23 patients) were diagnosed with any complication on admission. Complications at diagnosis were more frequent in girls (74.4%). When analyzing the number of complications in the last evaluation, 48% had one, 39% had 2, and 13% had 3. The most frequent were synechiae (69.5%), retinal detachment (30.5%), and glaucoma (26%). Complications were more frequent when the etiology was autoimmune, as well as in intermediate uveitis. There were no differences in age (Table 5).
Distribution of complications at diagnosis according to sex, etiology, location, and age.
| Variable | Categories | Complications on admission to the rheumatology clinic | ||||
|---|---|---|---|---|---|---|
| Yes | No | p | ||||
| no | % | no | % | |||
| Sex | Male | 27 | 67.5 | 13 | 32.5 | 0.50* |
| Female | 29 | 74.4 | 10 | 25.6 | ||
| Etiology | Idiopathic | 20 | 64.5 | 11 | 35.5 | 0.09* |
| Infectious | 12 | 60 | 8 | 40 | ||
| Autoimmune | 24 | 85.7 | 4 | 14.3 | ||
| Location | Anterior | 16 | 80 | 4 | 20 | 0.43* |
| Intermediate | 20 | 71.4 | 8 | 28.6 | ||
| Panuveitis | 11 | 57.9 | 8 | 42.1 | ||
| Posterior | 4 | 57.1 | 3 | 42.9 | ||
| Age (mean/SD) | 8.76 | 3.61 | 7.69 | 3.86 | 0.24** | |
Five subjects were blind at the last assessment, 4 had bilateral involvement, and 3 were women. The etiology of these patients was idiopathic (3) and infectious (2), none of which was autoimmune.
The treatment received was topical in 65% of the individuals, 55% required systemic corticosteroids, and 43% were under immunosuppressive treatment. Patients with infectious causes were referred to the infectious disease clinic and were managed according to the etiology.
At the end of the follow-up, it was documented that 24% continued with topical management, 44% used oral corticosteroids, 64% had non-biological immunosuppressive management: 80% methotrexate (65.2% in monotherapy and 34.7% associated with biologics), 15.5%, azathioprine, 5% mycophenolate mofetil), and 30% (n=27) of the patients received biological therapy.
Of the subjects under biologic therapy, at the time of the last assessment, 41% were on monotherapy and 59% were following combined therapy (40% biologic+methotrexate+oral prednisolone and 19% biologic+methotrexate). The most widely used biologic was anti-TNF alpha (adalimumab) (88%), followed by anti-interleukin 6 (7.4%), and anti-CD20 (3.7%). In these individuals, 33.3% (9/27) required one biologic, 29.6% (8/27) 2, and 3.3% (1/27) more than 2.
Finally, concerning the behavior of the disease, in the last assessment, it was shown that 48% of the patients were in remission with medication.
DiscussionUveitis in children is a disease that requires early diagnosis and management to avoid major visual complications with lifelong disability. This study did not find differences with that reported by other publications in terms of distribution by sex and age at diagnosis.1–3
The anatomical location most frequently reported in international cohorts is anterior1,4,5; in a Colombian cohort of pediatric patients in 2016, the predominant location was posterior.6 In the present study, the most frequent location was intermediate, similar to that described in a 2005 study carried out in Jerusalem.7
It was also found that the “non-infectious” etiology (idiopathic and autoimmune) was more prevalent, a difference that can be explained because the assessment was performed within the pediatric rheumatology clinic, assuming that infectious uveitis had been studied and treated by other specialties and did not reach this consultation.
Concerning the laterality of ocular involvement, data agree with those of the Colombian cohort of Salazar,6 in which, in patients with panuveitis and intermediate uveitis, bilateral involvement predominates, while in those with posterior uveitis, the predominance is unilateral.
It was found that autoimmune uveitis associated with JIA constituted 15% of all uveitis, like that reported in studies carried out in the United States,8 Europe,3,9 and Asia,10 unlike what was described by Lonngi et al.8 for Colombia, where JIA-associated uveitis did not reach 2%. The reason for this difference may be secondary to the specialist who makes the diagnosis and the type of patients treated, or to the fact that there is currently greater knowledge of the disease and a more exhaustive search for its autoimmune causes, in cooperation with the team of pediatric rheumatology.
The percentage of patients with uveitis secondary to tuberculosis is striking, since it was higher than that reported by other cohorts, in which the prevalences varied between less than 1% in reference clinics in North America, and 10% or more in highly endemic regions.11,12 This result may be important for the worldwide discussion13 on the discrepancies in the reports of tuberculous uveitis, which suggests that criteria should be established in its definition, especially in endemic areas.
According to a study in Turkey, every year 67 million children are diagnosed with latent tuberculosis14; it is expected that up to a third or more of all patients with uveitis have some evidence of previous exposure to tuberculosis.12,13 Hence, ocular tuberculosis infection must be sought in those subjects for whom other causes had been excluded, and who present at least one suggestive clinical sign such as extensive posterior synechiae, retinal perivasculitis with or without choroiditis, multifocal serpiginous choroiditis, optic disc granuloma, or optic neuropathy, and necessary microbiological confirmation of Mycobacterium tuberculosis (M. tuberculosis) in ocular fluids or tissues,12 to determine the real prevalence of M. tuberculosis as a cause of uveitis.
The number of complications observed in this study is comparable to that reported in other publications; the quantity of patients with severe complications at diagnosis and some degree of disability is striking, which reflects that in many cases the disease is not suspected, and this leads to a late diagnosis and a delayed referral to specialists in charge of the study and treatment initiation.
Regarding the treatment of patients, in this population the behavior was like that described in the literature: the most frequently used non-biological modifying antirheumatic drug was methotrexate, according to management recommendations, and 30% of the patients were refractory to these medications.15,16
This study has limitations due to its retrospective observational design, such as the absence of some missing data in the secondary registry and in the capture through the pediatric rheumatology clinic, and these limitations may bias the behavior of the entire Colombian pediatric population. However, given the significant number of patients analyzed, it is an approximation that allows characterizing uveitis in the country's pediatric population.
ConclusionUveitis is an intraocular inflammatory process that affects the pediatric population. This study found a higher frequency of idiopathic etiology, followed by autoimmune and infectious, as described in the literature. Nearly half of the subjects present complications with important implications for quality of life.
Conflict of interestsThe authors declare that they have no conflict of interest.