Acanthocytes, when≥5% of urinary erythrocytes examined, are considered as the most reliable marker of glomerular haematuria. However, some uncertainties still exist in the literature about their morphological definition. The aim of this paper is to discuss this topic and to suggest a univocal definition of acanthocytes as erythrocytes with the shape of a ring with one or more protrusions.
Los acantocitos, cuando son≥5% de los eritrocitos urinarios examinados, se consideran el marcador más fiable de la hematuria glomerular. Sin embargo, todavía existen algunas incertidumbres en la literatura acerca de su definición morfológica. El objetivo de este artículo es discutir este tema y proponer una definición unívoca de los acantocitos como eritrocitos con la forma de un anillo con una o más protuberancias.
In 1982, Fairley and Birch described dysmorphic red blood cells and proposed their use to distinguish glomerular from non-glomerular haematuria.1 In 1991 Köhler et al described a specific type of dysmorphic red blood cell, i.e., the “acanthocyte”, as a marker of glomerular bleeding,2 an approach which has subsequently been validated by different authors. However, in spite of this, a univocal definition of acanthocyte is still missing.
The aims of this paper are 1. to review the different definitions which have been proposed of the term acanthocyte and 2. to suggest a univocal definition of this special subtype of dysmorphic urinary erythrocyte.
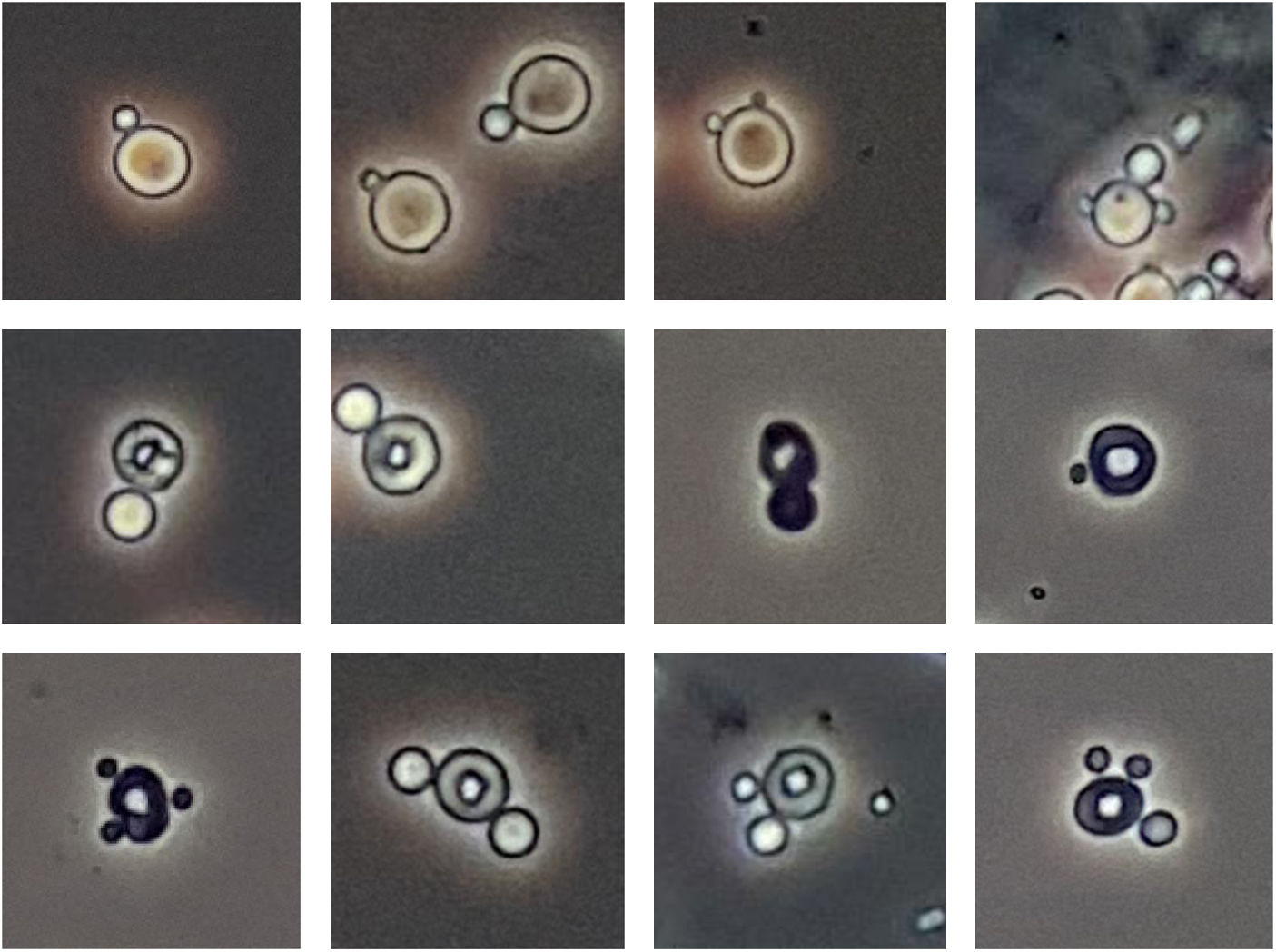
Definition of the term acanthocyteIn 1991 Köhler et al described acanthocytes as “ringforms with vesicle-shaped protrusions”.2 Chu et al in 19903 and Tomita et al in 19924 produced an exhaustive classification of dysmorphic erythrocytes, in which acanthocytes were included and defined as “G1 cells”. However, Chu et al described G1 cells as “doughnuts with more than one bleb” while Tomita et al described G1 cells as “doughnut-like cells with one or more blebs”. In addition, Tomita et al pointed out that G1 cells had “two kinds of deformity, i.e., bleb formation and a deeper concave formation”. In a later article by Kitamoto et al,5 it was clearly stated that G1 cells also included ring forms with a single bleb. This criterion was also adopted by Lettgen and Wohlmut in a paper published in 1995.6
Quite interestingly, this criterion of two deformities or anomalies to make an acanthocyte or a G1 cell was already supported in a Dalet's et al article of 1987.7 The authors noted that the monodiverticular erythrocytes (a single kind of deformity), considered by Tomita et al as G4 cells,4 could be generated in the laboratory as a consequence of an excessive centrifugation speed of the urine. They also demonstrated that the erythrocytes with a ring and one diverticulum (= with two kinds of deformity) were not associated with urine osmolarity changes and/or different centrifugation conditions, for which reason they considered them as real dysmorphic erythrocytes, with a glomerular origin. These annular and monodiverticular erythrocytes fully coincided with the definition of G1 cells supplied by Tomita et al4 and Kitamoto et al.5
Therefore, monodiverticular or polydiverticular erythrocytes (Figure 1, top) and monodiverticular or polydiverticular ring-shaped erythrocytes (G1 cells) (Figure 1, middle and bottom) should not be confused, since only the latter can be considered acanthocytes.
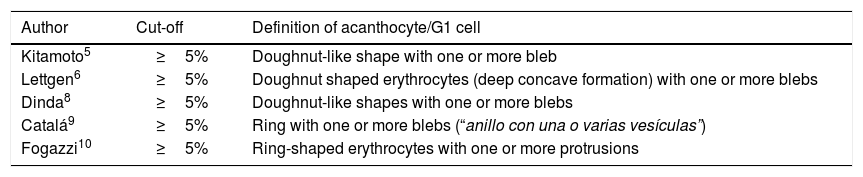
Differentiation of glomerular and non-glomerular haematuriaDifferent authors have carried out studies to establish a cut-off that could allow a differentiation between glomerular and non-glomerular haematuria using acanthocytes or G1 cells as criterion (Table 1).
Definition of acanthocyte/G1 cell used by different authors to establish the cut-off for glomerular haematuria.
| Author | Cut-off | Definition of acanthocyte/G1 cell |
|---|---|---|
| Kitamoto5 | ≥5% | Doughnut-like shape with one or more bleb |
| Lettgen6 | ≥5% | Doughnut shaped erythrocytes (deep concave formation) with one or more blebs |
| Dinda8 | ≥5% | Doughnut-like shapes with one or more blebs |
| Catalá9 | ≥5% | Ring with one or more blebs (“anillo con una o varias vesículas”) |
| Fogazzi10 | ≥5% | Ring-shaped erythrocytes with one or more protrusions |
All of them agreed that haematuria was of glomerular origin when acanthocytes/G1 cells represented≥5% of erythrocytes, with a specificity of 100% and sensitivities between 73% and 100%.
All the considered authors also agreed in defining the acanthocyte or G1 cell as a ring with one or more blebs.
ConclusionsAs we have seen, the cut-off of 5% has been calculated taking into account mono and polydiverticular acanthocytes. Both forms are considered specific for glomerular haematuria. The use of only polydiverticular acanthocytes in the calculation of acanthocyturia would decrease the total count of acanthocytes in the sample. This would entail a loss of sensitivity of the technique, which could be very important, bearing in mind that the cut-off is a low value.
We therefore, emphasize the importance of counting both the monodiverticular and the polydiverticular acanthocytes to identify glomerular haematuria, using the cut-off validated by the cited authors.
Conflict of interestThe Authors declare that they do not have any conflict of interest.