To evaluate the role of intra-operative hydrocortisone and post-operative dexamethasone on reducing post-operative complications following major surgeries involving oral cavity as in oral and maxillofacial surgeries performed under general anesthesia.
MethodologyThe post-surgical stress induces changes in metabolic and endocrinal pathways and also results in activation of inflammatory pathways. Post-operative administration of steroids helps in blocking all the stages of inflammatory process. This study was conducted on a group of 20 patients undergoing major surgical procedures. These patients were administered a combination of intra-operative hydrocortisone and post-operative dexamethasone therapy. Efficacy of these drugs in reducing post-operative complications was evaluated, using parameters like post-operative pain, number of analgesic injections, edema, sore throat, nausea and vomiting.
ResultsA 70% mean reduction in pain was seen on 2nd post-operative day and a drastic 97% pain reduction was noted on 4th post-operative day. An overall 12mm reduction in swelling was noted over the span of 4 days of hospital stay. Post-operative administration of dexamethasone helped in reduction of sore throat up to 95% on 2nd post-operative day. A remarkable finding noted was, that, none of the patients developed nausea and vomiting post-operatively.
ConclusionSurgeries done in and around the oral cavity are mostly prone to contamination as presence of saliva, bacteria, contaminants from stomach flora through acid reflux and post-operative events like vomiting, pollute the surgical site. A single intra-operative dose of hydrocortisone followed by post-operative tapered administration of dexamethasone helps in combating almost all of the post-operative complications after major oral and maxillofacial surgical procedures and hence hastens healing of surgical site.
Evaluar el papel de la administración intraoperatoria de hidrocortisona, y postoperatoria de dexametasona, para reducir las complicaciones postoperatorias tras las cirugías mayores de la cavidad oral y la cirugía oral y maxilofacial realizadas bajo anestesia general.
MetodologíaEl estrés postquirúrgico induce cambios en las vías metabólica y endocrina, y origina también la activación de las vías inflamatorias. La administración postoperatoria de esteroides ayuda a bloquear todas las etapas del proceso inflamatorio. Este estudio se realizó en un grupo de 20 pacientes sometidos a intervenciones quirúrgicas mayores. A dichos pacientes se les administró una combinación de hidrocortisona intra-operatoria y dexametasona postoperatoria. Se evaluó la eficacia de dichos fármacos para reducir las complicaciones postoperatorias, utilizando parámetros tales como dolor postoperatorio, número de inyecciones analgésicas, edema, dolor de garganta, náuseas y vómitos.
ResultadosSe observó un 70% de reducción media del dolor al segundo día postoperatorio y un 97% de reducción drástica del dolor al cuarto día postoperatorio. Se observó una reducción general de 12mm del edema durante el transcurso de la estancia hospitalaria de 4 días. La administración postoperatoria de dexametasona ayudó a reducir el dolor de garganta en un 95% durante el segundo día postoperatorio. Un hallazgo destacable fue que ninguno de los pacientes desarrolló náuseas ni vómitos a nivel postoperatorio.
ConclusiónLas cirugías practicadas en y alrededor de la cavidad oral son más propensas a la contaminación, ya que la presencia de saliva, bacterias, contaminantes de la flora estomacal a través del reflujo ácido, y los acontecimientos post-operatorios tales como vómitos, contaminan el sitio quirúrgico. La administración de una única dosis intra-operatoria de hidrocortisona y postoperatoria de dexametasona ajustada ayuda a combatir la mayoría de las complicaciones postoperatorias tras las intervenciones quirúrgicas mayores orales y maxilofaciales y, por tanto, contribuye a la curación del sitio quirúrgico.
The foremost factor in post-operative morbidity, excluding failures of surgical and anesthetic technique, is the surgical stress response. This surgical stress entails increased demands on organ function. These changes in organ functioning are interceded by endocrinal and metabolic changes and activation of many biological cascade systems (cytokines, complement, arachidonic acid metabolites, nitric oxide, free oxygen radicals, etc.). Activation of these biological systems is a result of the inevitable post-operative inflammation.
Corticosteroids have proved to be a boon for being the most efficacious anti-inflammatory agents. Its anti-inflammatory action has been put to test in many different studies and has stood the test of time.1–10 Most surgeons employ this property to control operative outcomes and provide a comfortable post-operative recovery.1–5,9,10 Corticosteroids have various applications; it is principally used as a replacement therapy in patients with adrenal insufficiency, in immunosuppressive therapy and as an anti-inflammatory agent.2,9,11–13 Its use as a life saving drug in cases of anaphylatic shock, Ludwig's angina and auto-immune diseases is a well proven fact.
Corticosteroids induce the synthesis of endogenous proteins, which block the enzymatic activation of phospholipase A2 which in turn inhibits arachidonicacid release. This leads to inhibition of the synthesis of prostaglandins, leukotrienes or substances related to thromboxane which are responsible for inflammation and pain.
The side effects of corticosteroids due to adrenocorticoid suppression are well known and depend on dose and duration of treatment.11,13 Such suppression can be observed when the physiological levels are elevated for more than 5 days, or when corticosteroids are administered for over 1–2 weeks.14 In our study, patients were administered with steroids for a period of four days and the dose was gradually tapered over the 4 day period to prevent suppression.
A study showed 19% of all patients to have experienced adverse reactions after the postoperative administration of 0.5mg of betamethasone via the oral route.15 Such reactions are not recorded with use of dexamethasone.
In a study that compared and tabularized the significance of efficacy of steroids in pain reduction, only the studies that used methylprednisolone, dexamethasone and betamethasone showed significant values.14
Dexamethasone seems to be the most suitable because it has the highest anti-inflammatory activity, no mineralocorticoid activity and a longest available half-life of 36–54h making it a drug of choice for its peri-operative use in the case of major surgeries.5–7,10 Hydrocortisone being a short acting steroid was used as a single dose to cover the anti-inflammatory action during the intra-operative period.
Oral and maxillofacial region is a unique and vital anatomic area considering that a well functioning oral cavity is required for proper nutrition. The surgeries carried out in this area get invariably contaminated by the salivary flora. Yet it is the most neglected region. All the above-mentioned properties of hydrocortisone and dexamethasone, support their compulsory use in peri-operative phase of major oral surgeries. The objective of this pilot study was to observe and provide evidence of the advantages of using peri-operative steroids and to stress the need for addition of peri-operative steroids to the protocols followed in hospitals treating oral and maxillofacial surgeries for a successful healthy post-operative healing.
Materials and methodsThe study was conducted with the appropriate institutional approval, and written informed consent was obtained from all patients. The protocols of the study were set in accordance to The Code of Ethics of the World Medical Association (Declaration of Helsinki). A total of 20 American society of anesthesiologists [ASA] physical status I and II patients, aged in the range of 25–65 years, undergoing major surgical procedure under general anesthesia were selected through a randomized controlled method. Surgical time of one and half hours was considered as a criteria for patients to be included in the study.
Although the total duration of all the twenty surgeries was two and half hours, it included intubation, patient preparation and extubation, hence limiting the surgical time to one and half hours.
The various major procedures included were trauma [maxillary, mandibular and zygomatico-maxillary complex fractures] and surgeries carried out to treat pathologies like keratocystic odontogenic tumor.
Exclusion criteria:
- •
Patients who had received pre-operative steroids/anti-emetics.
- •
Patients with history of immune-suppression.
- •
Patients with history of upper respiratory tract infection.
- •
Patients with metabolic disorders like diabetes mellitus.
Agents used for induction and maintenance of anesthesia and the operator surgeon were similar for all patients. Patients were premedicated with midazolam, and fentanyl. For induction propofol was used. Endotracheal intubation was facilitated with inj atracurium (0.5kg/bodywt) which was maintained with nitrous oxide in oxygen and supplemented with isoflurane. Oro-tracheal and naso-tracheal routes were used for intubation and duration of the surgical time was recorded. The tracheo-bronchial secretions were suctioned time to time to avoid the need of glycopyrolate or atropine. All patients received 100mg of hydrocortisone intra-operatively, half an hour post-commencement of incision to combat the immediate inflammatory response to surgical trauma. Post-operatively all patients received a tapering dose of dexamethasone for a period of four days, i.e. 8mg thrice in a day—8mg twice in a day—4mg twice in a day—4mg once in a day.
During the post-operative period, parameters like pain, swelling, number of diclofenac injections, sore throat, nausea and vomiting were recorded till the day of discharge; which on an average was fourth post-operative day. Number of diclofenac injections needed in the post-operative period was a more definitive indicator of pain which is why it was added to supplement the recordings of the more descriptive results of the visual analog scale. Pain, sore throat, nausea and vomiting were subjective parameters which were tabulated based on patient's feedback, whereas swelling and number of analgesic injections were evaluated by the post-graduate trainee.
Pain scores were measured using a 10cm visual analog scale (VAS; 0=no pain, 1–2=mild annoying pain, 3–4=nagging uncomfortable troublesome pain, 5–6=distressing miserable pain, 7–8=intense dreadful horrible pain, 9–10=worst possible, unbearable excrutiating pain). Nausea was evaluated as a subjective sensation of unease and discomfort in the upper gastro-intestinal tract with an involuntary urge to vomit. Vomiting was considered as the involuntary emptying (“throwing up”) of stomach contents through the mouth. Both nausea and vomiting parameters were assessed on each post-operative day based on symptoms and requirement of anti-emetic administration. Sore throat was assessed as pain, itchiness or irritation of the throat. Sore throat was evaluated on a scale of 1–10 (1–3=mild, 4–7=moderate, 8–10=severe) on a regular interval. Percentage reduction in nausea, vomiting and sore throat were recorded. Post-operative reduction in swelling of mid third or lower third of face was computed using a caliper like device by measuring the medio-lateral dimensions at the most prominent area. The percentage reduction was tabulated based on comparisons with values recorded on each post-operative day in the same patient. The device was movable only in horizontal plane. A long metallic scale was moved in a plane parallel to sagittal plane and the first point of contact of the swelling was marked externally on the face. The outer limb of the device was placed on this mark and patient was asked to open mouth 2cm wide to accommodate the internal limb of the device which was placed to locate corresponding intra-oral fixed point in relation to upper and lower second molars; according to area of interest.16 Number of analgesic injections administered during the 4 days follow up period was also kept in account to evaluate the analgesic property of dexamethasone.
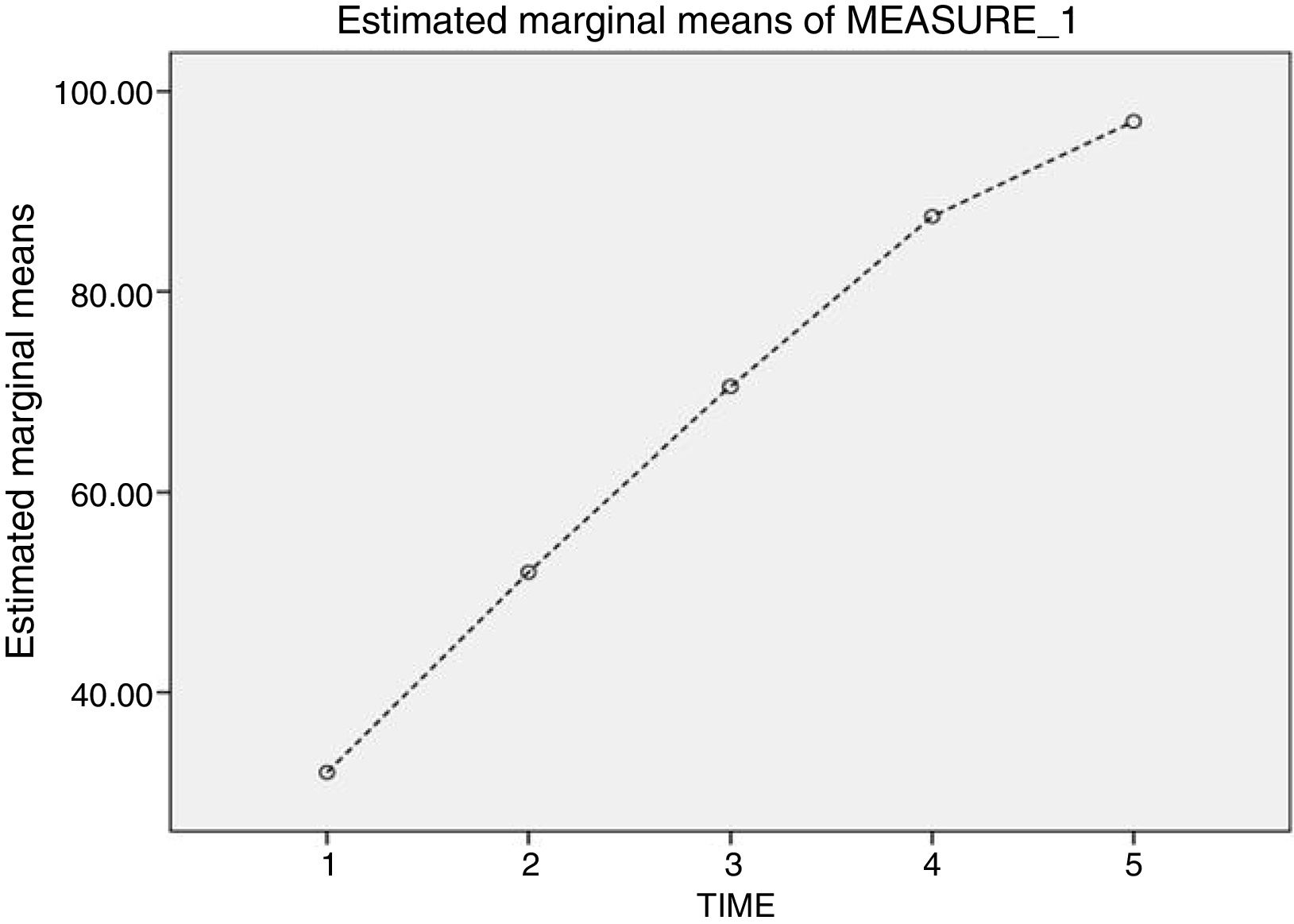
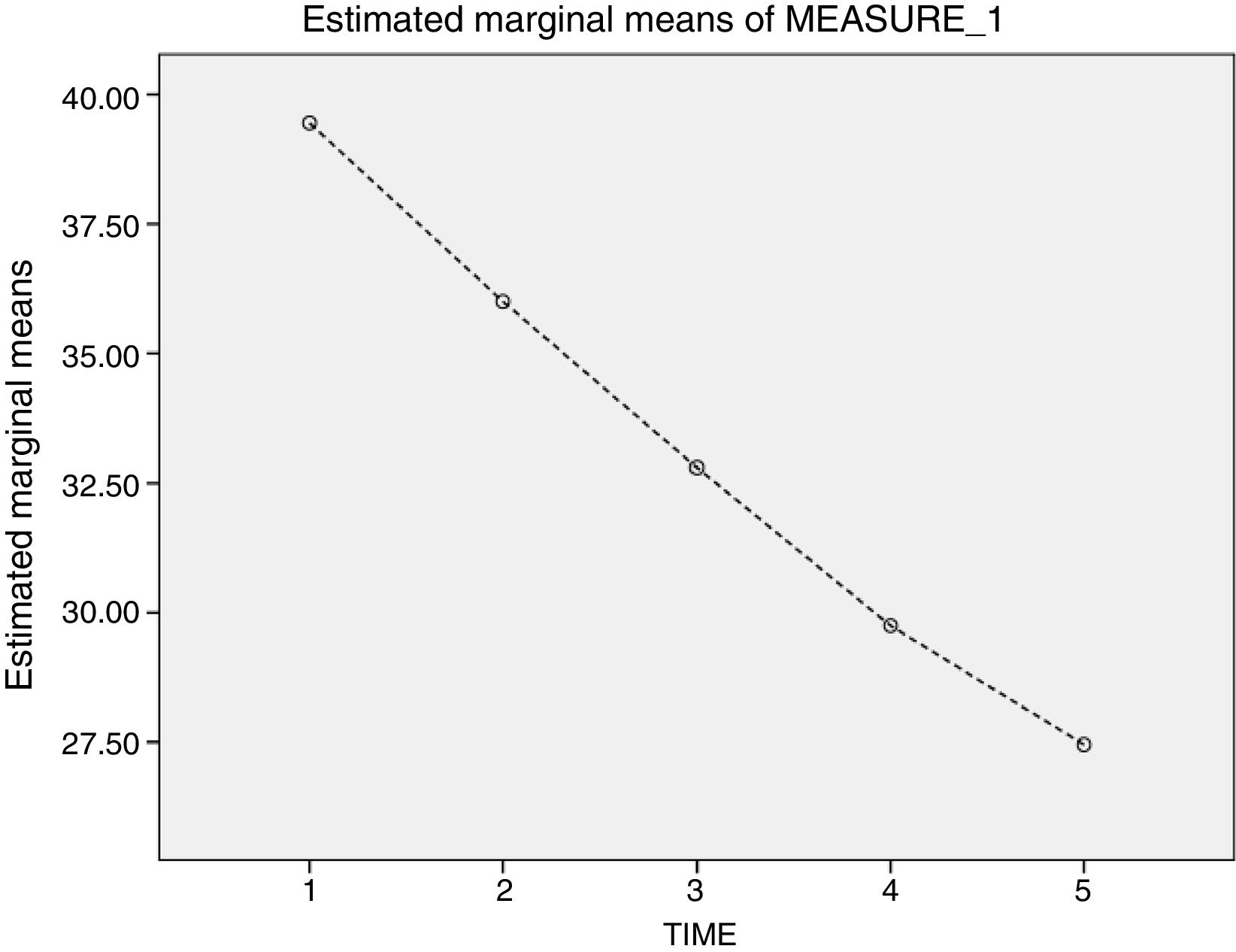
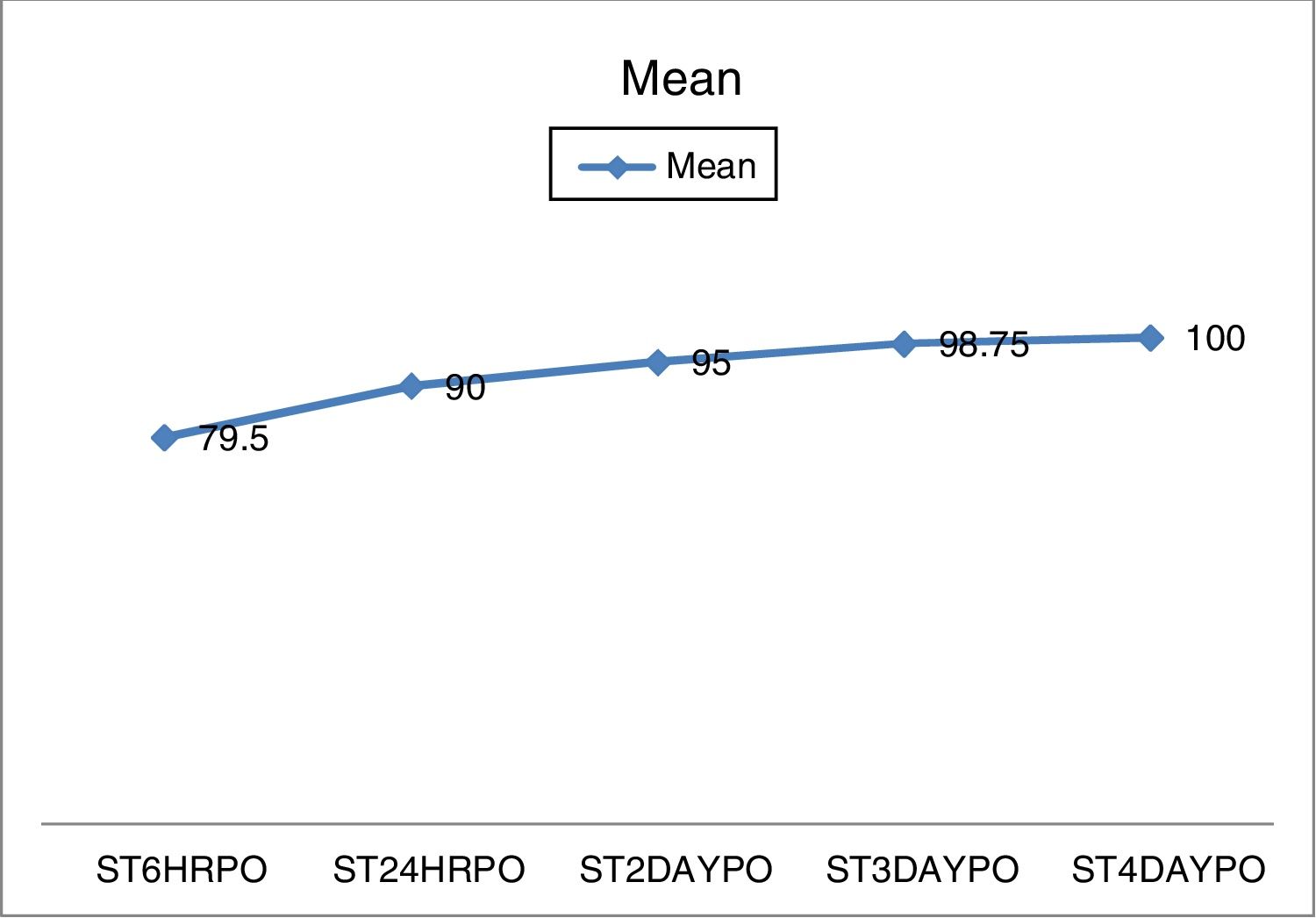
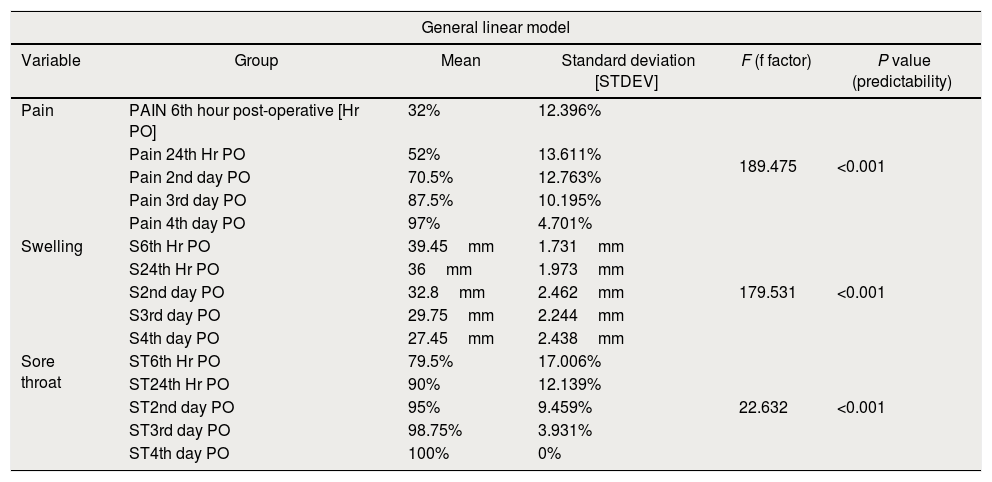
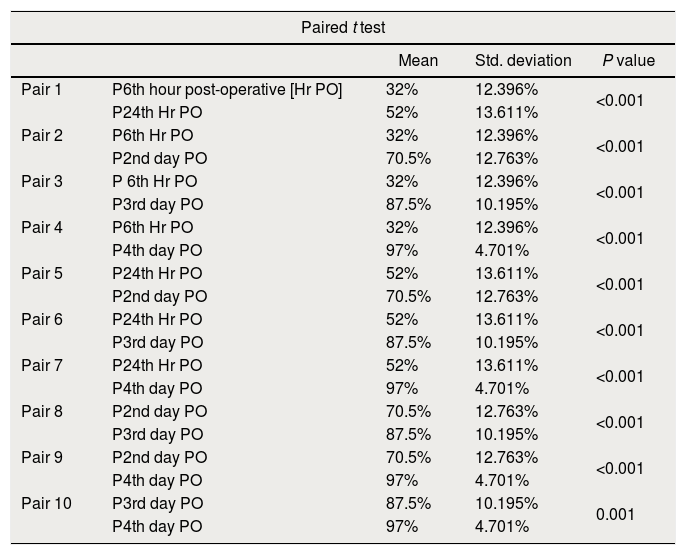
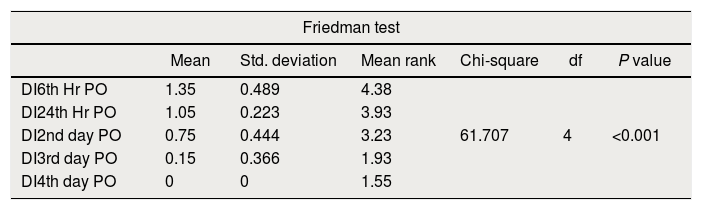
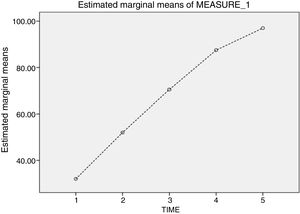
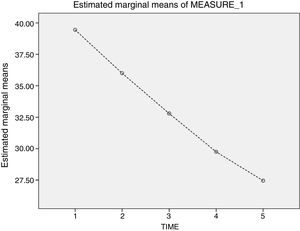
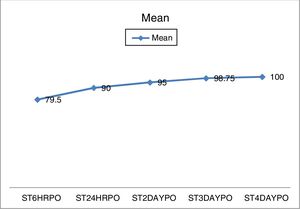
ResultsTable 1 shows that there was about 70% mean reduction in pain on 2nd post-op day and 97% mean reduction in pain on the 4th post-op day. Fig. 1 shows a linear increase in the percentage reduction of pain from 6th hour post-operatively to 4th day post-operatively following administration of intra-venous dexamethasone. The paired t-test (Table 2) carried out to evaluate the efficacy of dexamethasone in pain reduction on subsequent days showed significant values indicating that the drug is effective in reducing the pain till the 4th day. Table 1 is indicative that there was a 12mm mean reduction in swelling noted on 4th day post-operatively from the maximum swelling seen on 6th hour post-operatively. This is also evident from Fig. 2 which shows a linear graph model with a steep fall in the swelling over the span of 4 days. Paired t-test carried out for swelling showed significant reduction till 4th day as seen in case of pain. Table 1 clearly depicts that there was 95% mean reduction in sore throat noted on 2nd post-operative day and a 100% reduction on 4th day post-operatively. The significant reduction in sore throat has also been depicted on Fig. 3. Also results obtained on paired t-test for sore throat were significant till the 4th day as seen in former mentioned parameters. A remarkable finding noted was; none of the patients developed post-operative nausea and vomiting even at the 6th post-operative hour. Hence, none of the patients who were included in the study were administered anti-emetics post-operatively during their hospital stay. As already noted dexamethasone brings about drastic reduction in post-operative pain; number of diclofenac injections required post-operatively was reduced enormously which can be seen in Table 3. None of the patients who were on dexamethasone therapy required parenteral analgesics on 4th day.
Table depicting mean reduction in pain, swelling and sore throat.
| General linear model | |||||
|---|---|---|---|---|---|
| Variable | Group | Mean | Standard deviation [STDEV] | F (f factor) | P value (predictability) |
| Pain | PAIN 6th hour post-operative [Hr PO] | 32% | 12.396% | 189.475 | <0.001 |
| Pain 24th Hr PO | 52% | 13.611% | |||
| Pain 2nd day PO | 70.5% | 12.763% | |||
| Pain 3rd day PO | 87.5% | 10.195% | |||
| Pain 4th day PO | 97% | 4.701% | |||
| Swelling | S6th Hr PO | 39.45mm | 1.731mm | 179.531 | <0.001 |
| S24th Hr PO | 36mm | 1.973mm | |||
| S2nd day PO | 32.8mm | 2.462mm | |||
| S3rd day PO | 29.75mm | 2.244mm | |||
| S4th day PO | 27.45mm | 2.438mm | |||
| Sore throat | ST6th Hr PO | 79.5% | 17.006% | 22.632 | <0.001 |
| ST24th Hr PO | 90% | 12.139% | |||
| ST2nd day PO | 95% | 9.459% | |||
| ST3rd day PO | 98.75% | 3.931% | |||
| ST4th day PO | 100% | 0% | |||
Depicting table on paired t-test for drug efficacy.
| Paired t test | ||||
|---|---|---|---|---|
| Mean | Std. deviation | P value | ||
| Pair 1 | P6th hour post-operative [Hr PO] | 32% | 12.396% | <0.001 |
| P24th Hr PO | 52% | 13.611% | ||
| Pair 2 | P6th Hr PO | 32% | 12.396% | <0.001 |
| P2nd day PO | 70.5% | 12.763% | ||
| Pair 3 | P 6th Hr PO | 32% | 12.396% | <0.001 |
| P3rd day PO | 87.5% | 10.195% | ||
| Pair 4 | P6th Hr PO | 32% | 12.396% | <0.001 |
| P4th day PO | 97% | 4.701% | ||
| Pair 5 | P24th Hr PO | 52% | 13.611% | <0.001 |
| P2nd day PO | 70.5% | 12.763% | ||
| Pair 6 | P24th Hr PO | 52% | 13.611% | <0.001 |
| P3rd day PO | 87.5% | 10.195% | ||
| Pair 7 | P24th Hr PO | 52% | 13.611% | <0.001 |
| P4th day PO | 97% | 4.701% | ||
| Pair 8 | P2nd day PO | 70.5% | 12.763% | <0.001 |
| P3rd day PO | 87.5% | 10.195% | ||
| Pair 9 | P2nd day PO | 70.5% | 12.763% | <0.001 |
| P4th day PO | 97% | 4.701% | ||
| Pair 10 | P3rd day PO | 87.5% | 10.195% | 0.001 |
| P4th day PO | 97% | 4.701% | ||
Depicting table on mean and standard deviation for number of diclofenac injection required per day post-operatively.
| Friedman test | ||||||
|---|---|---|---|---|---|---|
| Mean | Std. deviation | Mean rank | Chi-square | df | P value | |
| DI6th Hr PO | 1.35 | 0.489 | 4.38 | 61.707 | 4 | <0.001 |
| DI24th Hr PO | 1.05 | 0.223 | 3.93 | |||
| DI2nd day PO | 0.75 | 0.444 | 3.23 | |||
| DI3rd day PO | 0.15 | 0.366 | 1.93 | |||
| DI4th day PO | 0 | 0 | 1.55 | |||
Out of the many factors that affect wound healing, a lesser known culprit is edema. With the onset of edema, pain, stiffness of skin, and trismus or limitation of mouth opening, ensues. This in turn affects nutrition which is a very important factor needed for good wound healing. Edema also increases risk of infection due to decreased blood circulation to the wound site. Compression of arterioles and capillaries creates dead tissue over a period of time that might result in a pressure ulcer. Edema can then lead to maceration, resulting in breakdown of the epidermal layers, further slowing the healing process. Our study showed a significant reduction of post-operative edema following administration of intravenous dexamethasone.
Pain can contribute to stressful states like anxiety, fear, depression which further delay wound healing. Anxiety in turn can lead to decreased pain threshold, reduced pain tolerance and can negatively influence the immune system.12,17,18 Steroids have analgesic property and patients in our study on dexamethasone required less rescue analgesia/opioid consumption during post-operative period.
Sore throat in the post-operative period is a common symptom which is secondary to intubation. Dexamethasone reduces sore throat symptom20 and this was supported by the findings of our study.
Oral and maxillofacial surgeries mostly involve procedures that require access through the oral cavity. The oral cavity houses a plethora of bacteria and this contamination is worsened with post-operative vomiting. To conduct a clean uninfected healing of surgical sites, it is imperative for the oral surgeon to prevent contamination of oral cavity by food or vomitus. This necessitates measures like administration of antacids, anti-emetics. Corticosteroids have a potent anti-emetic action that precludes administration of antacids and anti-emetics during the post-operative period.6,19–21 None of the patients in our study suffered from symptoms of nausea and vomiting in the post-operative period.
Psychological stress weakens cell-mediated immunity at the wound site, drastically delaying the healing process.17,18 The significance of an uneventful/smooth recovery period is imperative for a healthy healing. The modification of stress response has some great potential benefits on surgical outcome. Dexamethasone as seen through our study proved to be an excellent drug of choice for reduction of stress component and ensure a healthy recovery by diminution of post-operative symptoms like edema, pain, nausea, vomiting and sore throat.
Although steroids are the norm in the post-operative period, their use in oral and maxillofacial surgeries is not a part of the protocol. We recommend a single intra-operative hydrocortisone dose followed by dexamethasone administration in a tapering dose fashion during the post-operative period for hastening healthy recovery process. As observed on the basis of our study, the drug dexamethasone did not cause any untoward complication following its controlled intra-venous administration post-operatively.
To appreciate and corroborate the results of this article, we recommend a study comparing the post-operative healing with a control group. Also the combination of different glucocorticosteroids with different pharmacological profiles, as used in our study [intra-operative hydrocortisone followed by post-operative dexamethasone administration] merits further research.
FundingNone.
Conflict of interestThe authors declare that there are no conflicts of interest.