Impacted mandibular third molars can be located in close proximity to the mandibular canal. This creates a risk for the nerve or artery injury. These are contained in the canal. However, the impacted third molar can be moved coronally by orthodontic means, after removal of overlying bone, and safely extracted. The orthodontic intervention slowly moves the tooth apex away from the mandibular canal and reduces the potential for a neural injury. This method may be useful for older patients with root apices that approximate or are actually located in the mandibular canal. This technique needs further study. There is a theoretical potential for neural or arterial injury from physical contact of the tooth apex as it moves by or through the mandibular canal.
Los terceros molares inferiores impactados pueden localizarse muy cerca del canal mandibular. Esto constituye un riesgo de lesión del nervio o la arteria, que se localizan dentro del canal. No obstante, el tercer molar impactado puede desplazarse en dirección coronal con ortodoncia, tras ostectomía del hueso suprayacente, y extraerse sin riesgos. La intervención ortodóncica desplaza lentamente el ápice del diente fuera del canal mandibular y reduce la posibilidad de lesión neural. Este método puede ser útil para pacientes de edad avanzada con ápices dentales que se aproximan o en realidad se localizan en el canal mandibular. La técnica necesita un estudio adicional. Hay la posibilidad teórica de lesión neural o arterial a partir del contacto físico del ápice del diente a medida que se desplaza a través del canal mandibular.
Third molars, wisdom teeth, can be anatomically superfluous in the human anatomy and be considered for extraction.1 In some patients the tooth apex may be located in close proximity, or actually in, the mandibular canal. The canal contains the inferior alveolar nerve, artery and vein and thus may incur damage during the removal of such a located molar. The actual occurrence of nerve injury is low but this can be the cause of neural sequelae and lawsuits against the surgeon.2,3 Third molar removal is controversial because of the question of physiologic necessity for removal of these teeth. There are also economic and quality of life issues for patients and society. These issues should be discussed with the patient before third molar surgery. Diagnoses that may indicate third molar removal include recurrent pericoronitis and angular impaction against the cementoenamel junction of the second molar. The classifications of third molar impactions are based on radiographic appearance: vertical, horizontal mesio angular, distoangular, buccolingual.4,5 Mesioangular position may be the most common impacted position.6 Advanced age, increased operative time and distoangular and horizontal preoperative impaction position are associated with mandibular third molar surgery post operative morbidities.7
Surgical removal of third molars is associated with postoperative pain, swelling, and trismus. Parameters associated with complications are age, gender, significant medical history, oral contraceptives, pericoronitis, poor oral hygiene, smoking, position of impaction, relationship of third molar apex to the mandibular canal, increased surgical time, surgical technique used, surgeon's experience, perioperative antibiotics, topical antiseptics, intra-socket medications, and anesthetic technique, a localized alveolar osteitis, postoperative infection, hemorrhage, oro-antral communication, damage to the adjacent teeth, displaced teeth, and bone fracture.8
The positions of third molar apices in relation to the mandibular canal on plane film radiography are: superimposition of the apex on the canal, apical radiolucency, incomplete radiographic canal border, bend in the radiographic canal and a narrowing of the canal.9 These descriptions may not portray the actual apical position that can be seen on cone beam computerized tomograms. The risk for nerve injury may be lower if the third molar is removed when the root apex is immature. Later, it can develop and approach or enter the mandibular canal then there may be a higher risk for inferior alveolar nerve damage. Third molar removal is the most common reason for post-operative altered nerve sensation of the inferior alveolar nerve.10 Neural sequelae include anesthesia, paresthesia, pain or a combination of these (Renton). Neural sequelae may occur for several reasons, physical damage from the tooth removal, infection, inflammation and instrument trauma.10 The removal of a third molar in close proximity to the mandibular canal can expose the inferior alveolar nerve and produce an altered sensation of the inferior alveolar nerve that may be permanent.10 Microsurgical repair can be done successfully in many cases when performed by a trained and experienced surgeon soon after the injury.11
The radiographic preoperative assessment parameters of surgical difficulty are the spatial relationship, depth of the impaction, the relationship/space of the ramus, the positioning of the impaction, the number and shape of the roots, the shape root apex, and the proximity of the root to the mandibular canal. Radiographic assessment is useful but not completely predictive of an adverse outcome.5
There needs to be enough space from the distal of the second molar to the anterior border of the ramus for the third mandibular molar can erupt into the occlusal plane.10 There is a consensus that third molars do play some undetermined role in lower anterior tooth crowding.10
When the root apex is close to the mandibular canal an alternative procedure to surgical extraction may be appropriate, such as coronotomy or orthodontic distraction.10,12–14 If the inferior alveolar nerve is exposed during the surgical extraction, about 50% of these patients will recover neural function spontaneously but 50% may not. A surgical neural repair intervention may be indicated. 4.5–7 months after such repair most will improve.10,11 Cone beam computerized tomograms (CBCT) can aid in diagnosis and treatment planning but may not prevent an adverse outcome.10
Optimal time for third molar removal may be when the root apices are immature with little or bone covering and before age 24.14,15 Third molar removal before the age of 23 may not result in distal periodontal defects and may improve the periodontal condition in this area.16 However, an incision design that leaves the second molar distal gingiva intact may result in better periodontal healing.17
The clinical decision to remove symptomatic third molars is not particularly difficult. However, the removal of asymptomatic third molars may be complex. There is accumulating data that support the removal of these impacted teeth to prevent other conditions from developing.18 Many asymptomatic third molars do not require removal. However, some third molars may be subclinically infected.10 Clinically evident pericoronal infections can develop around these teeth later in life. Also, caries can occur at the distal aspect of the adjacent second molar especially where the mesial marginal ridge of the mesio-angular impacted third molar contacts the cement-enamel junction. Caries here can advance quickly and endanger the pulp of the second molar.
Generally, distal second molar caries occur in about 20% of patients when there is no third molar present.8 When there is an impacted third molar at a mesio-angulation of 31–70° distal second molar caries occurred in 47% of the patients and when there is an impaction at 71–90° the caries prevalence is 43%. A 90° impaction is a horizontal impaction. There is a significant effect of increased caries when there is distal interproximal contact at the cement-enamel junction of the second molar and this risk increases with the patient's age.19
CBCT can be used to demonstrate the position of the mandibular canal and the relationship of the third molar apex. CBCT may not predict an inferior nerve surgical exposure any more accurately than a panoramic plane film.20 A lingually positioned mandibular canal demonstrated on the CBCT is associated with a higher incidence inferior alveolar nerve injury.20 When there is apparent contact of the apex of the mandibular third molar with the mandibular canal on CBCT there is a 49% risk of nerve exposure. There is 23% risk for postoperative altered sensation of those cases where there was CBCT apex–canal contact. If there is an exposure of the mandibular canal in apex–canal contact cases there is a 37% risk for postoperative altered sensation.21 Although a surgical nerve exposure cannot be accurately predicted, the radiographic evidence of apex–canal contact demonstrated a higher risk for postoperative nerve involvement.
Postoperative complications from third molar removal are localized osteitis (dry socket), infection and nerve damage to the inferior alveolar and lingual nerves.22–24 Preoperative oral antibiotic administration does not appear to significantly reduce the incidence of dry socket. More unusual sequelae are severe hemorrhage, epidural abscess, subdural hematoma, benign positional vertigo, tissue emphysema, fracture and hematoma related asphyxiation.22–24
Preoperatively, a 2mg oral dose of amoxicillin may reduce postoperative pain in younger third molar surgery patients aged 12–19.25
Recurrent pericoronitis infections are an indication for third molar extraction. Informed consent should be obtained. Included in this discussion is the potential for a temporary or permanent altered sensation of the distribution of the inferior alveolar nerve. A neural disturbance of the innervation may occur of the region of the ipsilateral half of the lower lip. The patient should understand the risks.
Other treatment options beside extraction are available. An impacted mandibular third molar that has root apices in close proximity to the mandibular canal can be decoronated and the roots are left in the mandible. The contact to the second molar is relieved and the potential for nerve damage is not an issue.26 However, careful monitoring is key to prevent caries from entering the pulp, forming an infection complicating the situation. The potential for infection and caries remains.
Another solution for removal of dangerously impacted teeth is orthodontic forced extrusion that moves the apices away from the mandibular canal for subsequent extraction.12–14 This procedure may relieve the potential for neural damage.
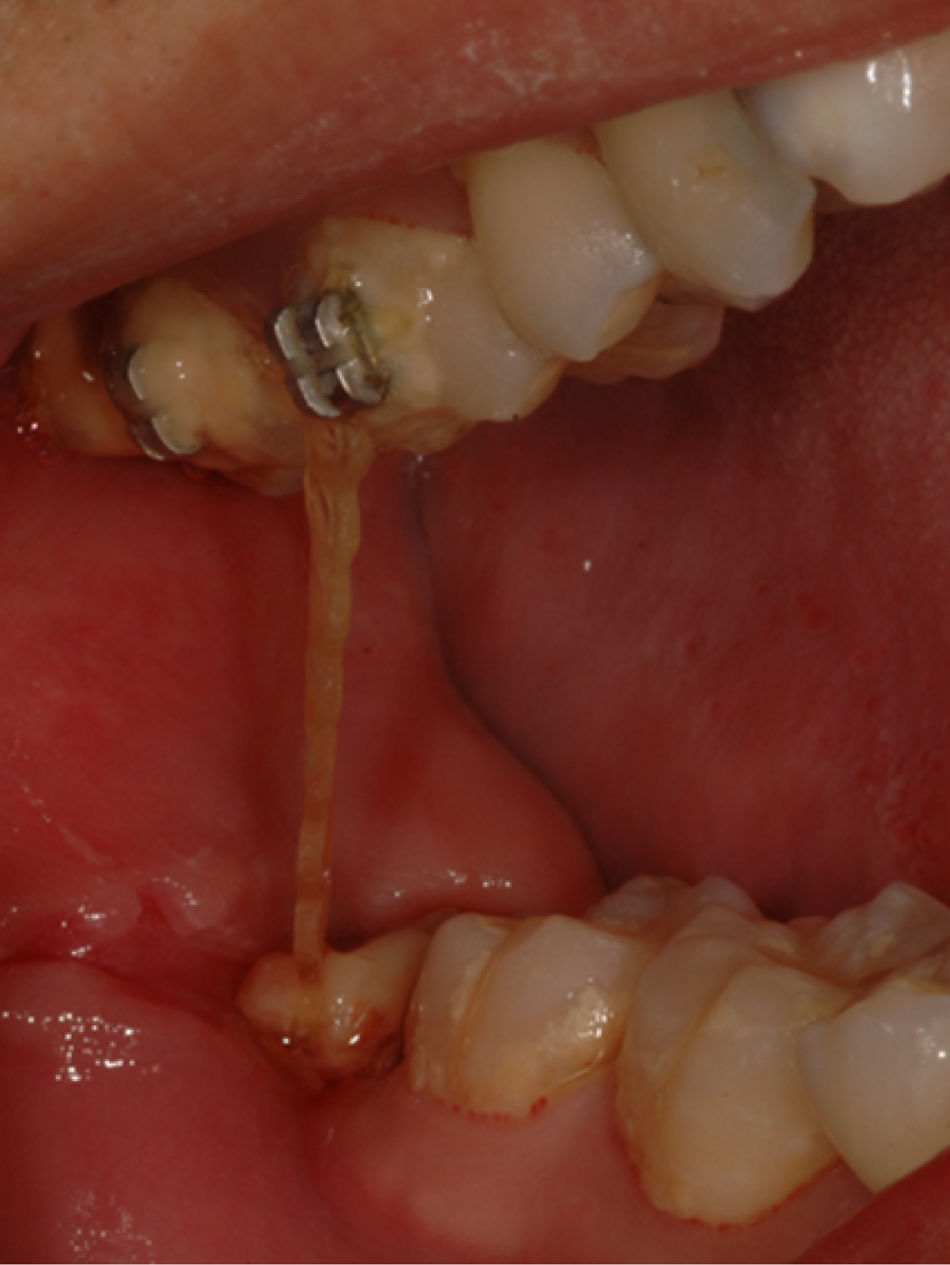
The procedureWhen a third molar is deemed a high risk for neural damage during third molar extraction options are discussed and informed consent obtained (Figs. 1 and 2). If the patient consents to an orthodontic forced extrusion the protracted treatment time and sequence should be explained. The removal is composed of two phases the orthodontic phase and the extraction phase. The orthodontic/surgical phase entails a surgical exposure of the tooth corona and removal of any osseous covering and mesial tooth structure that may impair occlusal movement of the tooth. Bleeding control is important for bracket placement so the patient may need reappointing to insure that the brackets can be securely placed in a relatively dry field. The tooth enamel is acid etched and an orthodontic button is bonded in the same directional plane of prospective occlusal movement. At least two maxillary molars are then acid etched and two edgewise brackets are bonded on the facial of each molar to provide anchorage (Fig. 3). A short piece of round wire may be attached to link the molars. An elastic linked chain is then attached one end to the button on the impacted third molar and the other end on maxillary bonded brackets. The elastic chain should be under tension only when the jaws are in repose and freeway space is at maximum. The elastic chain would be flaccid in maximum intercuspation. The patient is encouraged to cyclically depress the mandible to place tension on the elastic chain. A landmark measurement is taken to enable measurement of the occlusal progress of the third molar as it arises from the bone. Generally, the distal marginal ridge of the second molar can serve as this landmark. Follow up visits are done every 2–3 weeks to monitor movement and replace the elastic chain as it loses elasticity. Appropriate extrusion time is approximately 4–12 weeks. A prescribed chlorhexidine oral rinse (Peridex) may be appropriate to maintain oral hygiene. When the landmark measurement is found to be approximately 2mm a periapical radiograph can be done to demonstrate the position of the apex in relation to the mandibular canal. When the root apex is approximately 2mm away from the radiographic mandibular canal the extraction phase is begun and the third molar is easily removed under local anesthesia (Fig. 4).
The patient over the age of 24 with a recurrently symptomatic third molar with the apex in close proximity to the mandibular canal, that requires removal, is a surgical concern. The patient wants relief from the episodes of pain and infection but the potential for post operative morbidity is a serious consideration when the tooth apex is located near the mandibular canal.
Furthermore, patients over the age of thirty years may not have appropriate healing of the epithelial attachment at the distal of the second molar after third molar removal.10,27 This may create a periodontal issue at the distal of the second molar. There may be a poor healing of the attachment that can result in a periodontal pocket. The pocket may require periodic scaling and root planning or barrier membrane tissue guided regeneration.27–29
Predicting the difficulty of a third molar extraction is an uncertain process. The Pederson index is a method for predicting surgical difficulty. While this index is useful it cannot be the sole predictor determinant and by itself is considered unreliable.30
If the third molar is not removed, distal caries may develop at the distal of the second molar.8 Thus, the risk of postoperative neural sensory alteration and periodontal loss of distal attachment should be weighed against the benefits of relief of pain, distal caries prevention and relief of recurrent pericoronitis.
Crestal bone covering of the ridge is removed to facilitate the extrusion of the tooth and to induce a regional acceleratory phenomenon that increases bone remodeling.31 Wilcko and coworkers have demonstrated that removal of the local cortical bone can facilitate and speed orthodontic movement.32 The orthodontic forces must be applied immediately after the osseous surgery to take full advantage of the cellular activities. After two to three weeks the physiologic cellular mechanisms may be past prime time.
When the CBCT demonstrates that the mandibular canal is located to the facial aspect of the third molar root apex, this may not be associated with a dramatically increased risk for surgical nerve exposure.20,21 However, the close proximity of the apex to the canal may indicate a potential for neural surgical trauma.
The forced extrusion of the impacted third molar may not completely relieve the potential for sequelae. There is no evidence that the orthodontic movement of the root apex away from the canal will indeed prevent neural damage. If the tooth apex moves through the canal theer may be physical contact with the nerve or artery. Contact with the nerve may induce an altered sensation or arterial bleeding may produce a hematoma that with degradation produce an altered sensation from ferrous free radicals.33 Thus the movement of the tooth apex itself may potentially produce a neural event where the apex is located actually inside the mandibular canal or if the apex moves through the canal.33–35 Tooth movement may occur too quickly to allow for the neural sheath to accommodate and so produce an altered sensation.
The incidence of permanent postoperative altered sensation is low but a concern. This technique is not new and has been prior reported in the oral surgical literature.
ConclusionsImpacted mandibular third molar apices can be located in or in close proximity to the mandibular canal. CBCT or panoramic plane films can demonstrate the positioning. These impacted molars can be extruded by orthodontic force mesio-coronally using maxillary molars for anchorage. This moves the apices away from the canal and may relieve the potential for adverse sequelae. The mesial marginal ridge of the impacted molar is removed to facilitate the extrusion. The overlying osseous covering is removed to induce the regional acceleratory phenomenon to increase bone remodeling. Extraction of the extruded tooth can be easily accomplished due to the poorly calcified bone. An older patient with an apex that approximates or is actually located in the mandibular canal may benefit from this technique. There remains a potential for neural or arterial damage from the apical movement through the mandibular canal.
Conflict of interestThe authors have no conflict of interest to declare.