Dental-skeletal anomalies are treated by combining orthodontic treatment with orthognathic surgery. This mainly involves performing sagittal osteotomy of the mandibular branch. This technique offers many advantages, but its main disadvantage is paraesthesia of the inferior alveolar nerve. There are several treatments focused on promoting neurological recovery, one of which is low intensity laser. The aim of this study was to make a clinical evaluation of the efficacy of low intensity laser therapy in the neurosensory recovery of tissues after sagittal osteotomy of the mandible.
A group of twelve patients with the need of surgical correction of their dental-skeletal anomaly underwent orthognathic surgery with bilateral mandibular sagittal osteotomy. Patients were treated unilaterally and blinded with a low intensity infrared GaAlAs laser of 808nm, and compared with the contralateral site as a control group, following the course of the inferior dental nerve. The parameters used were of 100mW of power, irradiation of 3.6W/cm2, 2.8J of energy per point, an energy density of 100J/cm2, to 28s in each point with a distance of 1cm between points. The treatment included two sessions per week with a minimum of 10 sessions, starting 48h after surgery. Mechanical and thermal evaluations were performed in the first, fourth, seventh and tenth sessions. A significant improvement was observed in the subjective response of the patients on the treated side. The treatment of neurosensory disorders with low-intensity infrared laser has been shown to be effective in accelerating recovery, providing greater patient comfort, and presenting advantages over other existing methods.
Las anomalías dentoesqueléticas son tratadas combinando el tratamiento de ortodoncia con la cirugía ortognática, principalmente, mediante la osteotomía sagital de rama mandibular. Esta técnica ofrece muchas ventajas, pero dentro de sus principales desventajas se encuentra la parestesia del nervio dentario inferior. Existen varios tratamientos enfocados a promover la recuperación neurológica y uno de ellos es el tratamiento con láser de baja intensidad. Esta investigación tuvo como objetivo hacer una evaluación clínica de la eficacia de la terapia con láser de baja intensidad en la recuperación neurosensorial de los tejidos tras la osteotomía sagital de la mandíbula.
Un grupo de 12 pacientes con necesidad de corrección de su anomalía dentoesquelética fueron intervenidos con cirugía ortognática mediante la osteotomía sagital de rama mandibular bilateral. Los pacientes fueron tratados en el postoperatorio de manera unilateral y ciega con láser infrarrojo de baja intensidad de 808nm, medio activo de gaaias, y comparados con el lado contralateral como control, siguiendo el recorrido del nervio dentario inferior. Los parámetros utilizados fueron de 100 mW de potencia, irradiación de 3,6 W/cm2, 2,8 J de energía por punto, una densidad de energía de 100 J/cm2, a 28 s en cada punto con una distancia de 1cm entre puntos, 2 sesiones por semana, con un mínimo de 10 sesiones a partir de las 48 horas después de la cirugía. Se realizaron evaluaciones mecánicas y térmicas en la primera, cuarta, séptima y décima sesión. Se observó una mejora significativa en la respuesta subjetiva de los pacientes en el lado tratado. El tratamiento de los trastornos neurosensoriales con el láser de baja intensidad de infrarrojos ha demostrado ser eficaz en la aceleración de la recuperación, proporciona una mayor comodidad al paciente y presenta ventajas sobre otros métodos existentes.
Dentofacial deformities result from deficiencies in the craniofacial complex's growth and development, in the maxilla, the mandible or both. In each case, deformities can be symmetric or asymmetric, passed down genetically or acquired. Orthognathic surgery is an alternative in the correction of maxillomandibular deformities. This treatment is performed after an initial orthodontic treatment, aiming for a better position between the dental elements and the alveolar ridge. Then, the surgery is thoroughly planned based on esthetics and functionality, and carried out by osteotomies.1
The most common mandibular surgery technique is the Sagittal Split Osteotomy (SSO), which is used in prognathic, retrognathic treatments for mandibular asymmetry. Schuchardt started the studies on Sagittal Split Osteotomy in 1942, then Obwergeser and Trauner in 1957, Dal Pont in 1961, Hunsuck in 1968 and Epker in 1977, which made it a secure procedure, stale and versatile. Among its advantages are the advancement of mandibular retraction, correcting asymmetries, intraoral access with little or no external scaring, and allowing vertical rotations.2,3
One of the most common SSO complications is neurosensory disturbances, resulting from manipulating the neurovascular bundle, usually a temporary disturbance of the mental and the inferior alveolar nerve. Regardless of the lesion being in the mandibular foramen, the length of the inferior alveolar nerve or the mental foramen, the symptoms of a neural lesion are observed through different degrees of sensibility loss in the lower lip area, chin, labial mucosa, and skin of the mandibular area and that of the lower teeth.4–9
Trauma to the peripheral nerve may result in deficiency that varies from complete sensibility loss to a subtle change in tactile sensibility, which may continue for days, weeks, or even become permanent. The spontaneous reversion depends mainly on the injury degree, location, and individual capacity of recovery.1
There are several therapies that accelerate nerve lesion recovery, reducing the sensibility recovery time, such as administering systemic medications, local physiotherapy, electric stimulation, nerve repair surgery, low intensity laser treatment, and other therapies such as homeopathy and acupuncture.1,10–12
The use of low intensity lasers has been mentioned in literature due to its special characteristics, which provide important therapeutic effects, bio-modulators, analgesia, lymphatic drainage, bone regeneration, tissue and neuro-sensitive fiber repair.11–14
Low intensity laser helps in neural repair, increasing the neurons’ metabolism and improving the ability to produce myelin, inducing the spread of Schwann cells and reducing the synthesis of inflammation mediators.12,14,15 This treatment is being considered promising due to its non-invasive nature and its ability to regenerate wounded nerves without surgery, being a bio-modulator of signs and symptoms of these disorders.15
The use of aluminum gallium arsenide (AlxGa1-xAs) laser has been proposed as auxiliary treatment for the trigeminal nerve paresthesias resulting from Sagittal Split Osteotomy.12,15–19
Several clinical protocols with different irradiation parameters have been established; however they are still insufficient to standardize the treatment for neurosensory disturbances.20–23
This research aimed to make a clinical evaluation of the effectiveness of the low intensity laser therapy in the recovery of neurosensorial tissues after sagittal osteotomy of the mandible during orthognathic surgery.
Patients and methodsAfter the approval of the Ethics Research Committee of the IGESP Hospital (1310-2011), a group of 12 patients in need of surgical correction of their dento-skeletal deformity was selected. We performed a total of 12 bilateral sagittal split osteotomies; were immediate post-operatory bilateral nerve paresthesia was diagnosed (12 cases).
All surgeries were performed by the same surgeon. The patients were evaluated in order to determine the degree of the bilateral mandible paresthesia and underwent unilateral mandible laser therapy to determine the improvement degree on the wound, compared to the side that did not receive laser treatment. In this research the patients did not use any other therapy for neurosensory recovery.
Inclusion criteria were:
- •
Patients that had undergone orthognathic surgery including the bilateral sagittal split osteotomy technique.
- •
Patients with post-operatory paresthesia in the bilateral inferior alveolar nerve.
- •
Patients with inferior teeth, making thermal testing feasible.
Excluding criteria were:
- •
Slicing or breaking of the inferior alveolar nerve during the surgical procedure.
- •
Patients that decline their participation after being explained the study and understanding what it was about.
- •
Patients that did not follow the established protocol of consults.
The test side were the laser was applied was chosen with the application of a randomizer program (True Generator – ramdom.org) randomized (obtaining a total of 12 test and 12 control sides, 1 of each in every patient's mandible). The 12 patients were irradiated unilaterally with low intensity laser on 808nm (infrared), using the other side as a control with blindfolded patients. The control side received the application of a placebo heat light to replicate the feeling of the laser application of the test site.
All patients filled out the forms stating their medical records and the Informed Consent Form.
Two types of tests were used to evaluate neurosensorial disturbances: the mechanoreceptor tests, through a brush, and the nociceptors tests through thermal tests with hot gutta-percha and endo-frost. With a brush, applied on the skin of the posterior and middle mandible area, labial commissure, inferior lip, chin area skin, vestibular gum and labial mucosa, always comparing one side with its opposite. This test was used to evaluate sensibility presence or absence when being brushed, as well as having pain or shocks, or any other feeling described by the patient.
The initial evaluation methods as well as the periodical ones were identical and aimed to map the different conditions before, during, and after the proposed treatment.
A thermal test was performed through gutta-percha and cotton balls drawn in Endo-frost, applied to the molar, pre-molar and incisor crowns on both sides. Thermal tests were made in isolation, heat on all treated teeth, and then cold. The thermal tests were carried out to observe the presence or absence of pain related to temperatures. We took great care to evaluate teeth, which had received endodontic treatment or showing lack of vitality, in advanced, eliminating the possibility of a false negative. Frontal teeth from each segment were always evaluated, in order to know the best recovery condition, since usually improvement occurs from the back to the front.
Touching, temperature, and brushing tests we performed with blindfolded patients.
The 12 patients chosen with recommendations for orthognathic surgery with Sagittal Split Osteotomy, started laser therapy 48h after their surgical interventions, being the treated area, right or left side, chosen by means of a draw.
Radiation numbers were stipulated to be at least 10 sessions and there was no estimations regarding the maximum number of sessions, depending on the individual recovery capacity of each patient.
The test and control side skin was cleaned with cotton soaked in alcohol before each session, in order to avoid interferences of sweat and chemicals that could affect laser irradiation absorption. Regarding the oral tissue, contact with saliva was avoided, since it could cause absorption deflection.
To keep the patient from knowing on which side the treatment was being performed, an eye protector was used (blindfold) in order not to see the laser, as well as an iPod with earphones in order to make perception difficult.
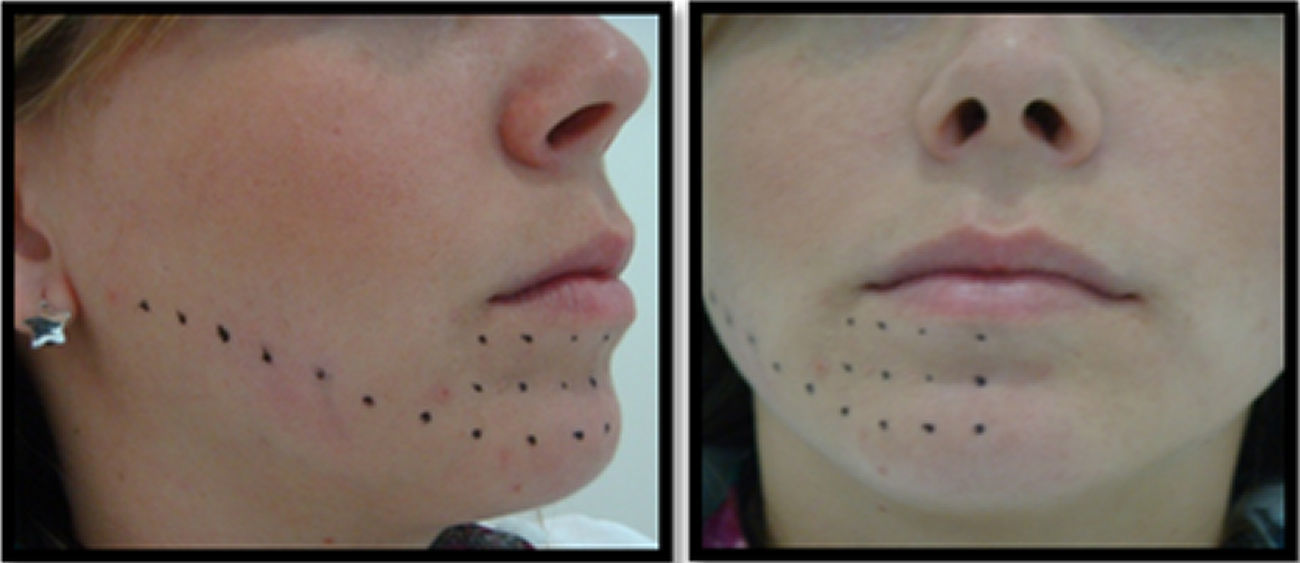
A W. Laser II DMC – São Carlos – SP/Brazil was used with an active means of AlxGa1-xAs, infrared emission of λ=808nm and power of 100mW. The spot area of the tip is of 0.0028cm2, however a teeth spacer was used 2mm from the irradiated tissue, thus resulting in an area of 0.028cm2. Irradiation time per point was of 28s, which resulted on an energy density of 100J/cm2 per point. The application was done from the back to the front, following the length of the inferior alveolar nerve starting at its entrance in the mandible foramen to the chin area and the external lip, and the oral area before the molars to the internal side of the lip, with an average of 25 points per patient (on one side) (Fig. 2).
Irradiation was always done on the same points, with the help of a millimetric endodontic guide, two to three sessions per week with an interval of 48–72h with at least 10 sessions, or until the complete recovery of the neurosensory disturbance (Fig. 1).
All patients received a sensitivity (mechanoreceptors and nociceptors) test at three during the laser application sessions. Those were performed at the first, sixth, and tenth laser treatments, considering that the evaluator testing the areas did not know where the laser treatment was being applied, and gathering. The information of the dichotomous variable as (yes/no) presents sensitivity during the test.
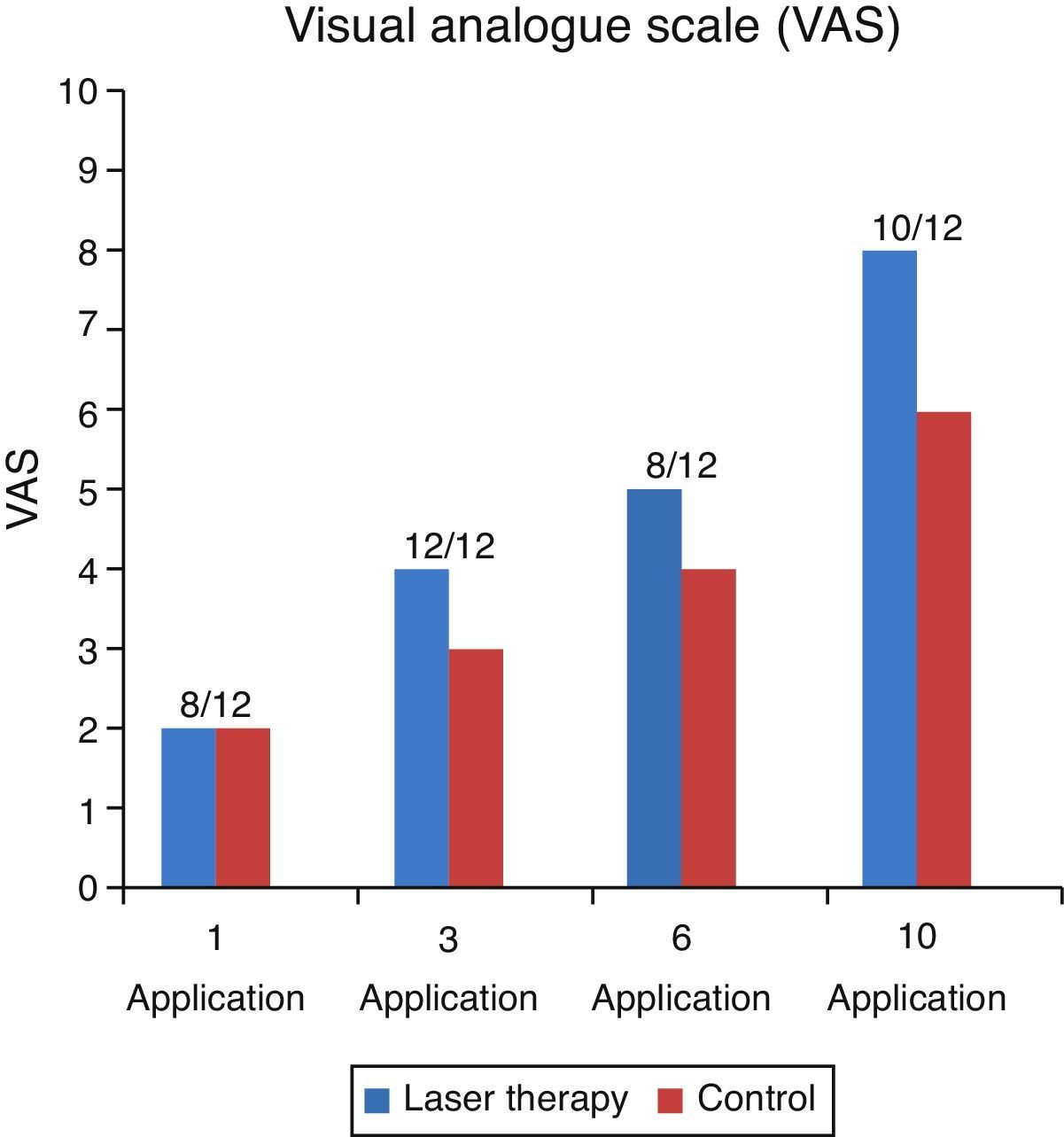
The results of the subjective interpretation of the pain were measured by the analogous visual scale of pain (VAS scale) which was performed by the patients in each control on a line of 10cm identifying the pain level from zero (0) or absence of the pain up to ten (10) maximum pain experienced and whose results were interpreted as, 0: absence of pain, 1–3: mild pain, >3–6: moderate pain, >6–10: severe pain. All the information collected was analyzed by means of dispersion measures for the quantitative variables (age), frequency description measures (proportions) for the gender variable, and the pain assessed by the VAS scale as an ordinal variable was analyzed by means of tests of non-parametric statistics (Kruskal–Wallis) with a level of statistical significance p<0.05.
ResultsFrom the patients evaluated, 6 of them were male and 6 female. Average age was of 30, and went from 18 to 54 years.
No patient described pain or temperature increase on the irradiated area during the treatment. There were mentions of symptoms such as burning, itching, jabbing, tingling, and temperature changes without stimuli, after the irradiation treatment.
No patient mentioned irritations, lip bites or salivation decrease. The skin from the commissure was the first area to show sensibility return in almost all patients. In general, patients showed signs of subjective improvement even before having it objectively tested.
We used Shapiro Wilk's test-analysis with a void normal hypothesis of the data obtained from the patients determining the type of elements that will be used for the analysis.
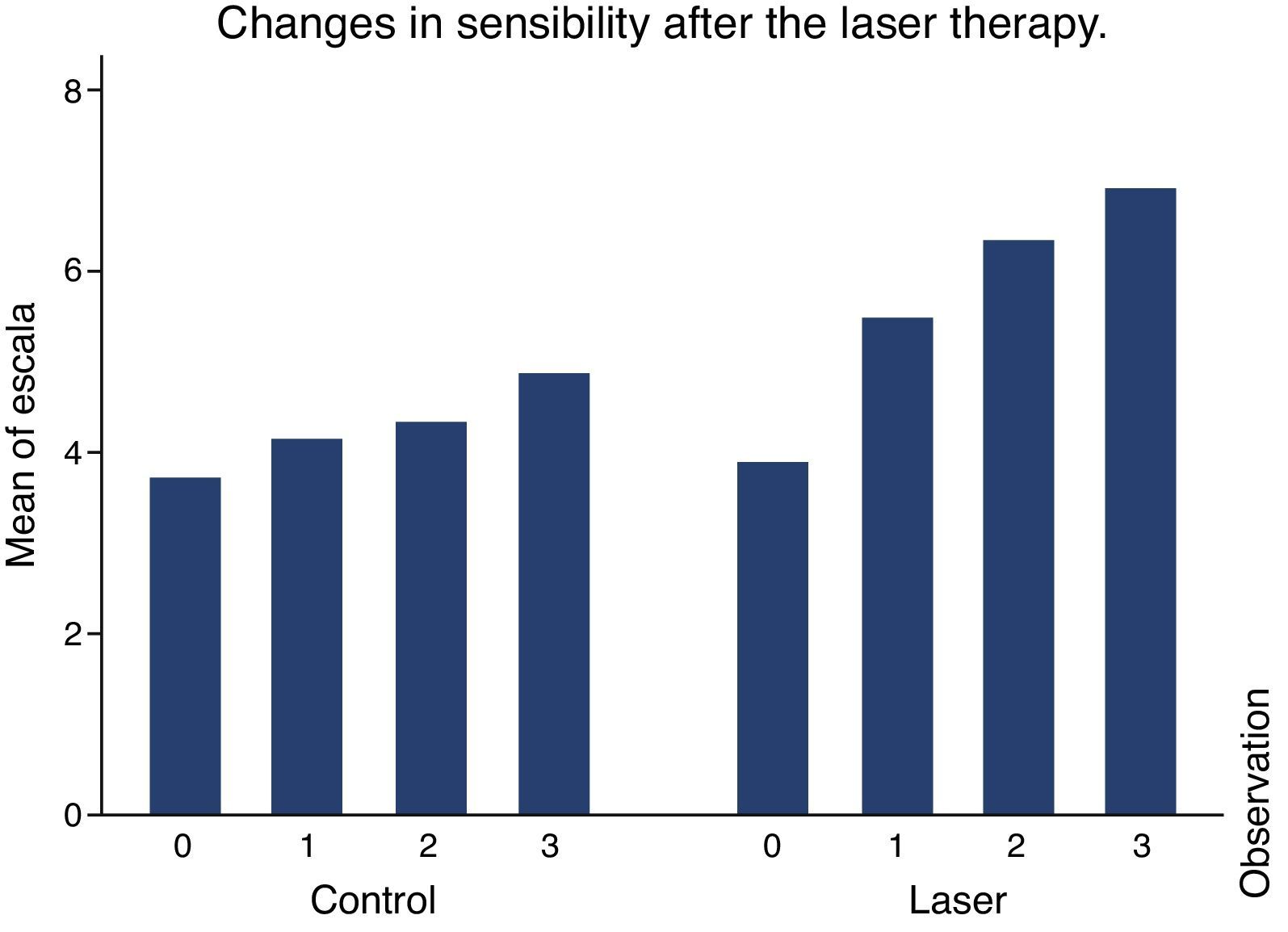
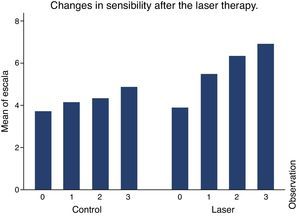
Comparing the behavior among the variables between the intervention group and the control group (Kruskal–Wallis test), we prove statistically significant differences p<0.0001 as of the second observation, showing that the group studied had a similar behavior to the control group, only at the initial observation.
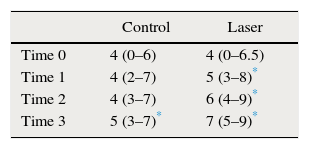
The group studied had a base sensitivity of 4, the same as the control group. As of the second observation it was verified that the group studied had less sensibility than the control group. On average, sensibility on the control group was 4 and on the group studied it was 6 (Table 1).
The control group had a statistically significant sensibility increase only on the fourth observation, p<0.001 for all the observed regions, with all the stimuli compared to the initial observation. It also had more sensibility on the second, third, and forth observation p<0.0001 for all the regions and stimuli used.
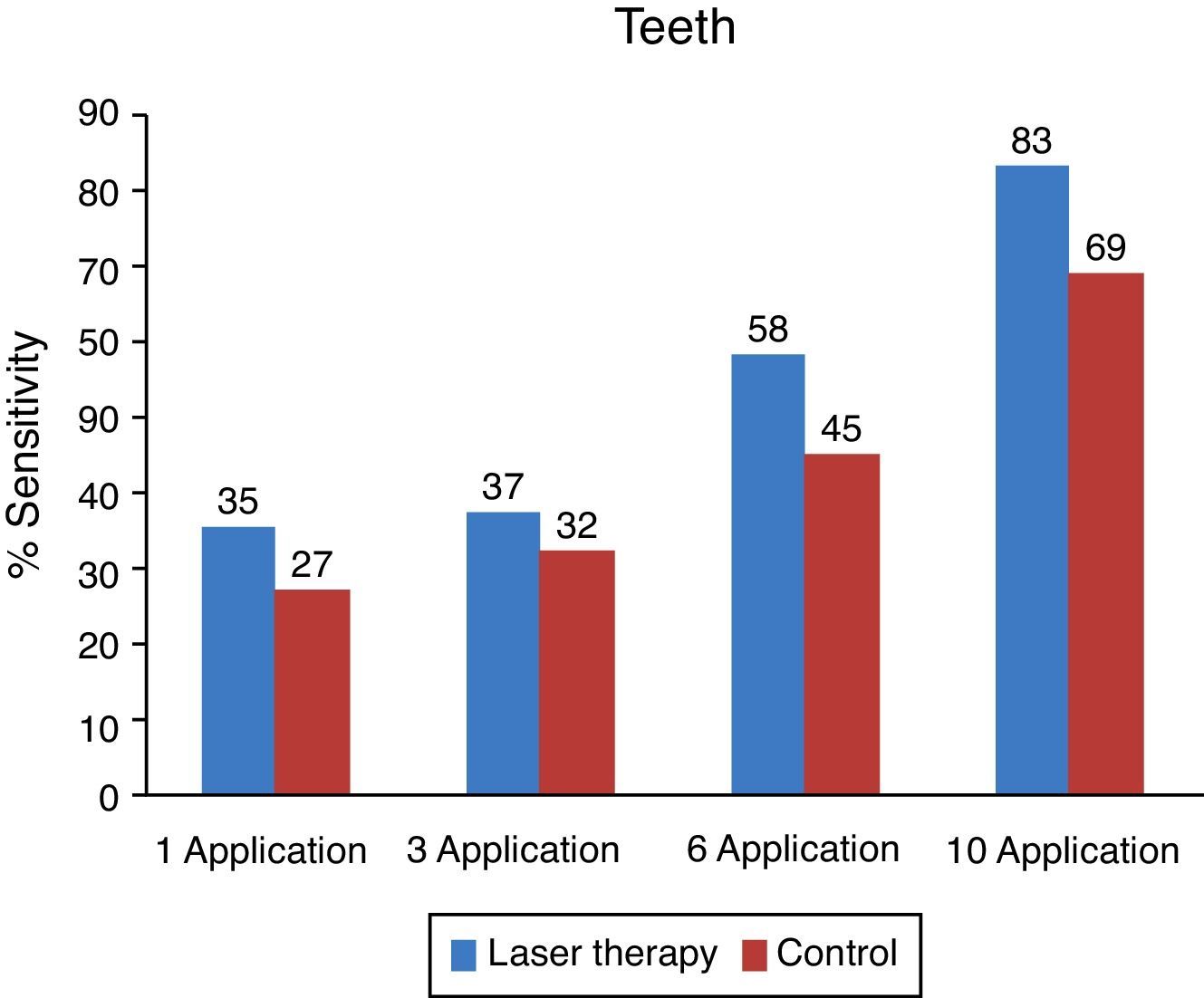
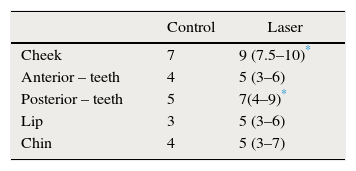
In the control group, all anatomic evaluated areas showed sensibility recovery with a similar pattern, without showing any statistically significant differences. On the group studied, the face and tongue area of the teeth significantly recovered sensibility after received laser therapy of p<0.0001 and average sensibility of 9 and 7, respectively, for all stimuli used (Table 2).
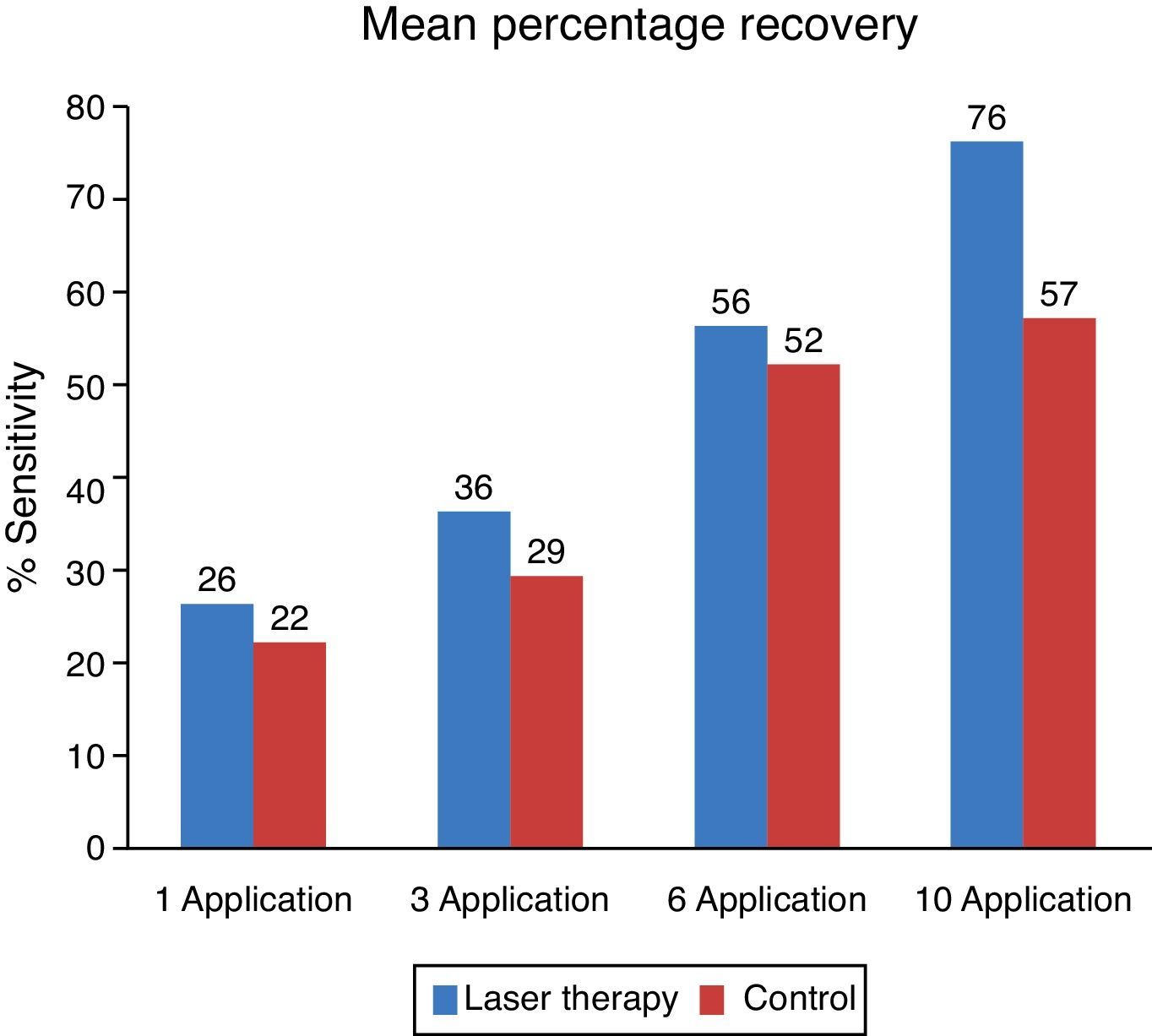
No group showed a significant sensibility difference based on the type of stimuli. All stimuli showed similar effects (Fig. 2).
The control group and the one studied showed similar sensibility results on the initial observation. The group studied shows improvement and sensibility increase for all stimuli while the control group does not show any significant improvement (Fig. 2).
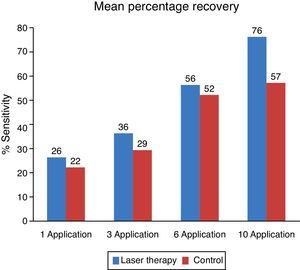
Results from the subjective analysis using the VAS sensibility scale showed that the majority of the patients presented a clinically valuable decrease in the perception of pain to the thermal stimulus (2/10 VAS) and that the majority of the patients had a higher perception. From pain to thermal stimulation on the side treated with laser therapy which was clinically identifiable from the third laser therapy session (Fig. 3).
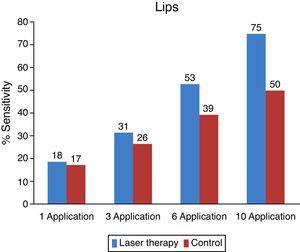
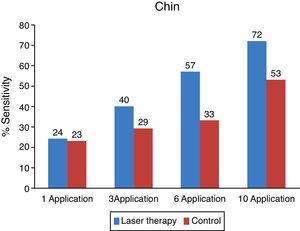
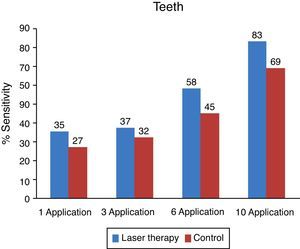
For the objective analysis, brush, endo-frost and gutta-percha tests were used in order to have a proportion of sensitive, partially sensitive or no sensitive responses for each patient, thus presenting all the evaluated matters. Statistics for these proportions are presented (Fig. 4).
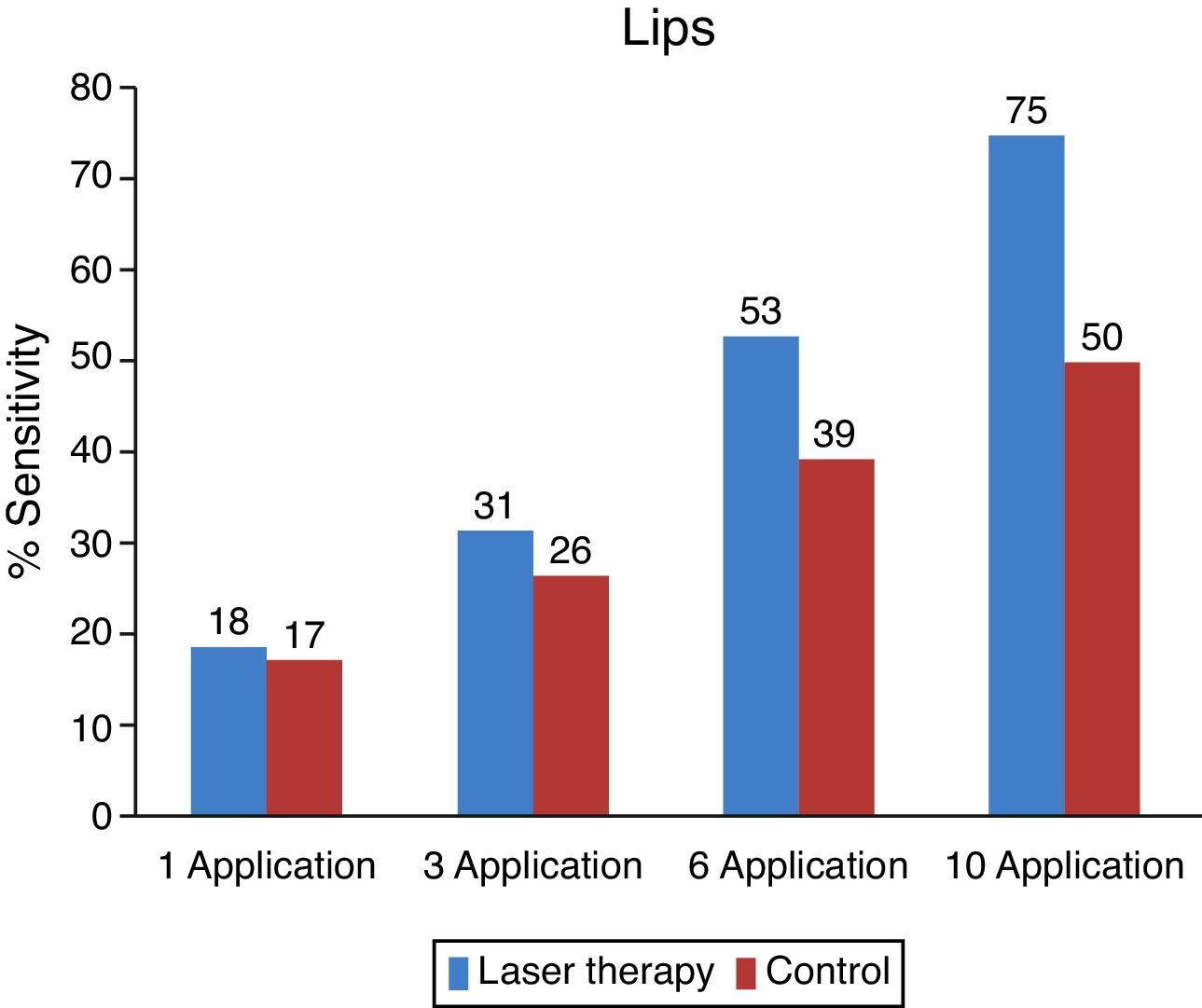
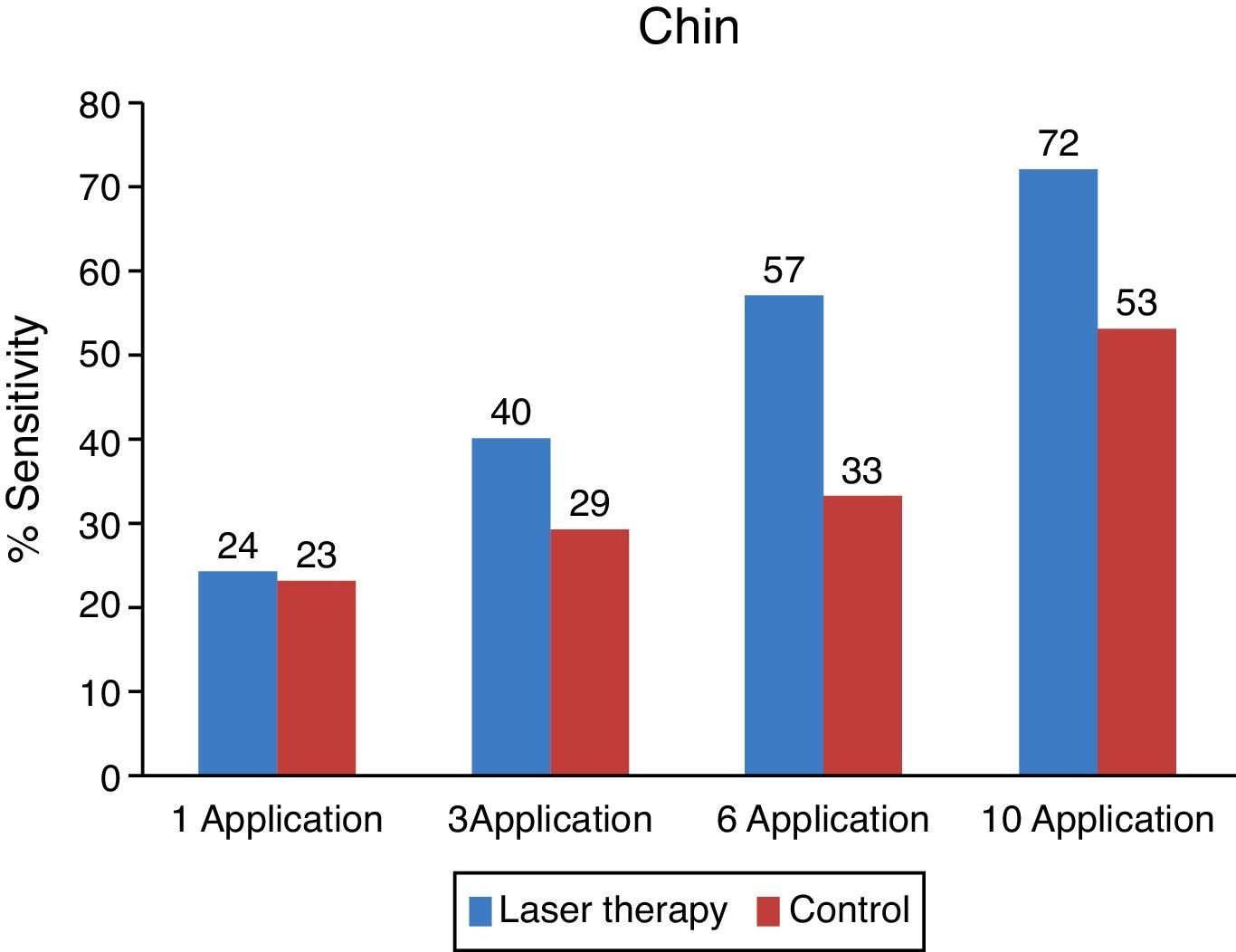
The objective analysis per area was performed on the same way than the general objective analysis, thus observing separate areas to evaluate the improvement on each one (Figs. 5–7).
The area of the cheeks was also evaluated and treated. Post-operatory and pre-operatory paresthesia in this region did not show any significant change.
On the side treated with low intensity laser, a faster recovery can be observed compared to that of the control side. From the evaluated areas, teeth and lips had better recovery index. The chin was the area with more paresthesia both on the objective and subjective evaluations.
Only one patient expressed having a more significant improvement on the control side than on the one treated with laser.
DiscussionThe sagittal split osteotomy technique originally described by Schuchardt in 1942 was modified and published by Obwegeser and Trauner in 1957, and it continued being modified. Nowadays, it is the most used technique for correcting bone mandible deformities.24 All patients considered in this study were surgically treated with this technique.
Despite the many advantages offered by the sagittal split osteotomy there are also some disadvantages or complications resulting from this technique. One of those complications is the neurosensory alteration of the inferior alveolar nerve.24-27
Published studies describe that females are more at risk from developing post-operatory complications as well as neuro-sensitive disturbances.28 Older people have more severe neurosensory deficiencies. This studied considered an equal number of male and female patients, and the average age was of 30, going from 18 to 54, and neurosensory recovery was more affected on older patients regardless of the sex.
Several types of treatment are mentioned to accelerate the recovery of the inferior alveolar nerve, such as systemic medication, local physiotherapy, electric stimulation, homeopathy, acupuncture and laser, and in more severe cases, neurosensory repair surgery.29 On all studies performed there is no protocol that has been sufficiently tested in order to completely treat paresthesia. In this study, patients had low intensity laser therapy as the only therapy to increase the recovery of a neurosensory disturbance.
Treatment of neurosensory deficiencies with low intensity lasers has been studied with positive results. Considering that the protocol of the treatment that includes irradiation on the length of the affected nerves, with fixed distances among the points, diode laser (AlxGa1-xAs), with point irradiation and infrared wave length, show better results, which is why we chose to use it.19,20
Opposite to some studies, our patients did not experience any pain, shocks or dysesthesia in response to the applied dosage. Treatment protocol was twice a week, which contributed in the periodical return of the stimulation, and it was clinically feasible for professionals.
Despite the laser having an output power of 100mW and irradiations used in this study may be considered high compared to other studies mentioned in the literature, the irradiation of 3.5W/cm2 used, is within the possible limits of the non-thermal effect. Therefore, the low intensity laser therapy proposed in this study, the energy of the photons absorbed is not transformed in heat, but it does result in the desired photochemical, photo-physic and/or photo-biological effects in the cells and tissue.20,30 In this study, there was no testimonial of thermal sensation during low intensity laser irradiation.
The mechanical and thermal objective tests used for this study were considered accurate and efficient for their clinical use. Their application is easy, and may be used on all regions, both oral and external, considering the treatment protocol for patients with similar characteristics may be uncomfortable for the patients. Our work used a variation of the method developed by Epelbaum.18
Main testimonials before the treatment consisted of tingling, jabbing, shocks, numbness, sensitivity loss, dryness, burning, inflammation, difficulty when speaking, and uncomfortable sensation, biting, being afraid of anesthesia or having another surgery, embarrassment, pressure, difficulty when putting lipstick on and when brushing the teeth. It is important to consider that what motivates patients to seek help is not only sensibility loss, but the disturbances created by it.30–33
After a month of treatment, only tingling, shocks, numbness and being afraid of other surgical event were the fears describe by the patients; the areas that still showed signs of disturbances generally were the lip and the chin. Overall, patients showed signs of subjective improvement before confirming the objective improvement with the tests. Proven results from previous studies show that neurosensory recovery may be sped, both in regards to the recovery time and to the degree of the lesion. It is believed that neurosensory return occurs faster when low intensity laser irradiation is performed right after the surgery, thus controlling edema, modulating inflammation and reducing the oxidant stress of the neurovascular bundle.12,15,34,35
We recommend further studies and follow up, increasing observations to evaluate the maximal function of low intensity laser treatment and knowing number of sessions required for this therapy.
The use of low intensity laser is effective in the treatment of post-operatory paresthesias from the first session, also low intensity laser therapy in post-operatory procedures (sagittal split osteotomy) for the treatment of paresthesias is efficient both on soft and dental tissue. The low intensity laser with a, infrared wavelength of 808nm is efficient in accelerating the recovery of nerve fibers, thus providing more comfort to the patient and presenting advantages such as reducing signs of inflammation, better tissue repair and therefore less uncomfortable pain, accelerating bone remodeling and repair, compared to other existing methods for the treatment of paresthesias like systemic medication, physiotherapy and repair surgery.
Ethical responsibilitiesProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Ethical approvalThis research received de ethical approval of the Bioethics Committee of the IGESP Hospital in Sao Paulo, Brazil (1310-2011).
FundingNone.
Conflicts of interestThe authors have no conflicts of interest to declare.