Leiomyosarcomas is rare tumour that arises from smooth muscle cells.1,2 They account for 7% of soft tissue sarcomas.1–3 Leiomyosarcoma in the head and neck region account for only 3–10%,2,4 and less than 0.1% develops in the oral cavity.2 It has been reported that oral leiomyosarcoma shows a bimodal peak in the third, sixth and seventh decades of life.4 Although a possible association with trauma, estrogenic stimulation, ionizing radiation and Epstein–Barr virus has been suggested, its underlying aetiology remains uncertain.4,5,9,10 This article describes an additional case of oral leiomyosarcoma affecting the tongue related to ionizing radiation.
Case presentationA 41-year-old male patient who two years previously had undergone radiotherapy and chemotherapy because of a Cavum Carcinoma, the patient was referred to the maxillofacial department on October of 2014 because a rapidly increasing lesion on the on the right side of the tongue was noticed at the follow-up. Clinical examination showed a well-circumscribed firm, submucosal mass on the right side of the tongue (Fig. 1). No cervical lymphadenopathy was palpable. As control of his Cavum Carcinoma the patient had a PET/CT scan that only reports a focal uptake on right side of the tongue.
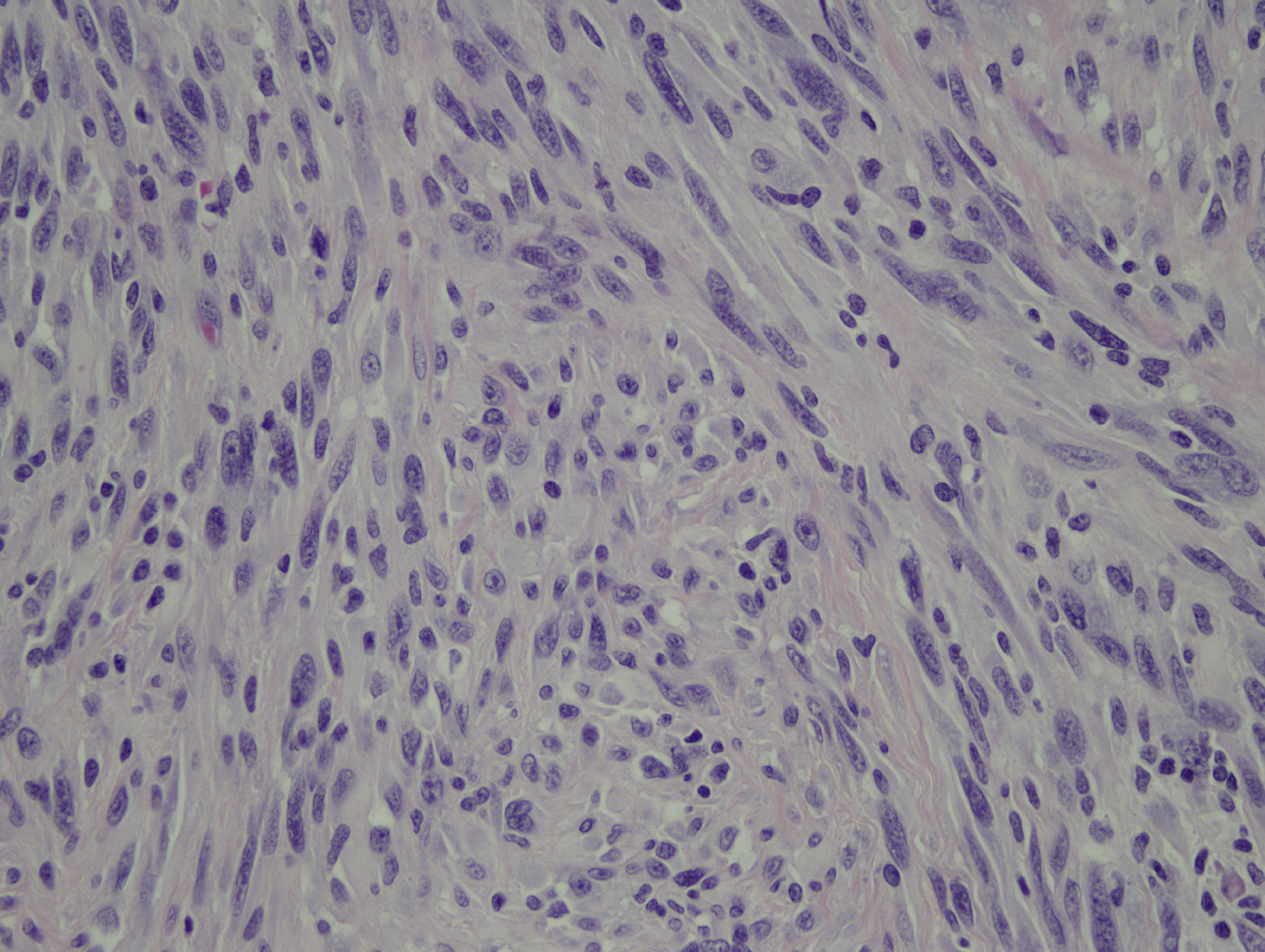
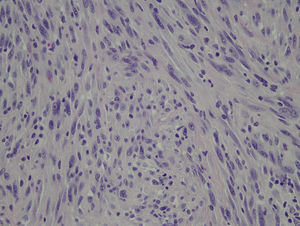
An incisional biopsy was repeated on January 2015 after a first negative result; the histopathology showed an infiltrating spindle cell tumour that stained for smooth muscle actin. The immunohistochemistry stained positively with smooth muscle actin, desmin, and caldesmon (Fig. 2).
He was treated with hemiglossectomy. It was reconstructed with a medial sural perforator flap, and no neck dissection was performed on March of 2015 (Fig. 3a–c). The patient had a good functional and cosmetic result with no signs of recurrence in subsequent follow-ups, last one on July 2016.
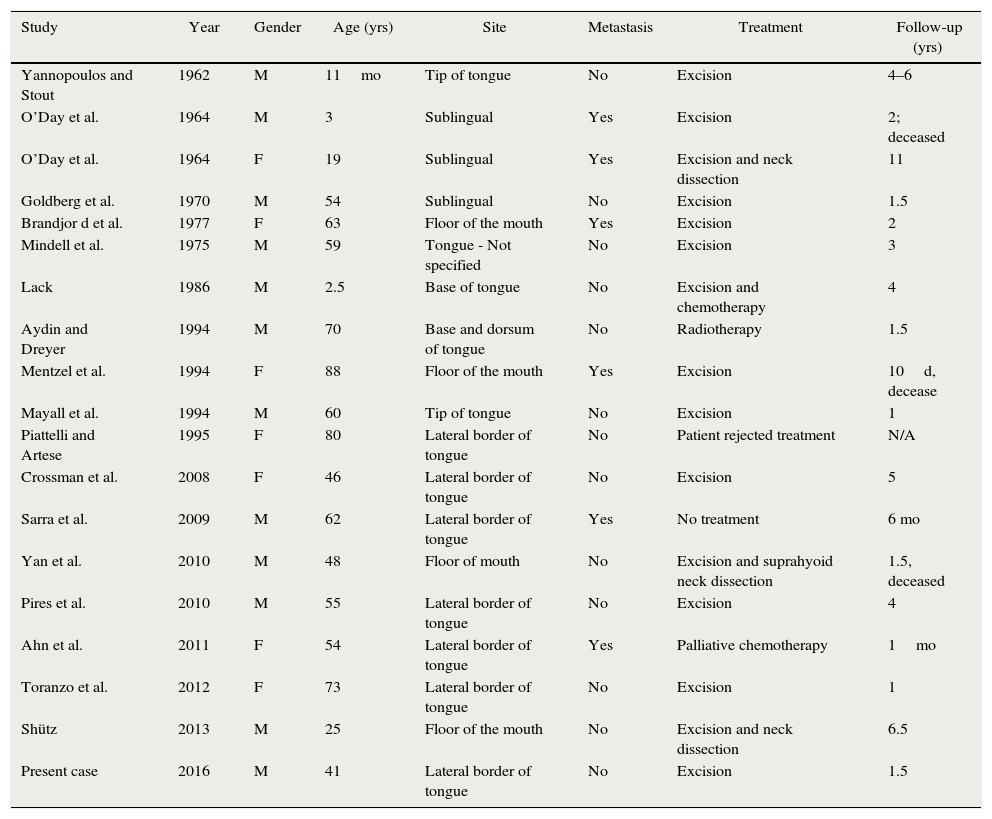
The cases reported in the literature are summarized in Table 1. We included Oral LMS that only affected the tongue; publish in the English and Spanish literature with all the variables included in the table. The exclusion criteria were LMS not affecting the tongue and publication with incomplete medical reports.
Reported cases of primary leiomyosarcoma arising from the tongue.
| Study | Year | Gender | Age (yrs) | Site | Metastasis | Treatment | Follow-up (yrs) |
|---|---|---|---|---|---|---|---|
| Yannopoulos and Stout | 1962 | M | 11mo | Tip of tongue | No | Excision | 4–6 |
| O’Day et al. | 1964 | M | 3 | Sublingual | Yes | Excision | 2; deceased |
| O’Day et al. | 1964 | F | 19 | Sublingual | Yes | Excision and neck dissection | 11 |
| Goldberg et al. | 1970 | M | 54 | Sublingual | No | Excision | 1.5 |
| Brandjor d et al. | 1977 | F | 63 | Floor of the mouth | Yes | Excision | 2 |
| Mindell et al. | 1975 | M | 59 | Tongue - Not specified | No | Excision | 3 |
| Lack | 1986 | M | 2.5 | Base of tongue | No | Excision and chemotherapy | 4 |
| Aydin and Dreyer | 1994 | M | 70 | Base and dorsum of tongue | No | Radiotherapy | 1.5 |
| Mentzel et al. | 1994 | F | 88 | Floor of the mouth | Yes | Excision | 10d, decease |
| Mayall et al. | 1994 | M | 60 | Tip of tongue | No | Excision | 1 |
| Piattelli and Artese | 1995 | F | 80 | Lateral border of tongue | No | Patient rejected treatment | N/A |
| Crossman et al. | 2008 | F | 46 | Lateral border of tongue | No | Excision | 5 |
| Sarra et al. | 2009 | M | 62 | Lateral border of tongue | Yes | No treatment | 6 mo |
| Yan et al. | 2010 | M | 48 | Floor of mouth | No | Excision and suprahyoid neck dissection | 1.5, deceased |
| Pires et al. | 2010 | M | 55 | Lateral border of tongue | No | Excision | 4 |
| Ahn et al. | 2011 | F | 54 | Lateral border of tongue | Yes | Palliative chemotherapy | 1mo |
| Toranzo et al. | 2012 | F | 73 | Lateral border of tongue | No | Excision | 1 |
| Shütz | 2013 | M | 25 | Floor of the mouth | No | Excision and neck dissection | 6.5 |
| Present case | 2016 | M | 41 | Lateral border of tongue | No | Excision | 1.5 |
Intraoral leiomyosarcoma, particularly in the tongue are extreme rare. They arise from smooth muscle cells.1,2,5–11 Intraoral leiomyosarcoma occurs more frequently in males.4 Clinically the tumour presents as a well-circumscribed painless mass. The correct diagnosis is only made following a definitive histological examination and confirmed by immunohistochemistry.3,6,8,10,11 Immunohistochemical staining has consistently shown positive for desmine, vimentin, and smooth muscle actine, whereas a negative response to S100 protein and the cytokeratins is usually found.1–7
Leiomyosarcoma behaves as an aggressive tumour, and has a tendency to infiltrate surrounding tissues. The more frequent distant metastases of leiomyosarcoma are the head and neck region,2–5 in 15% of the cases.2,3 Metastases can also spread to the regional lymph nodes, and the lung and the liver are prediction sites for distant metastases.2–5
The cause of leiomyosarcoma remains unknown, although cases associated with trauma, estrogenic stimulation, ionizing radiation and Epstein–Barr virus have been suggested.4,5,9,10
The treatment consists of wide surgical excision with regional lymph node dissection as required, with the goal of histologically clear margins. This determines the true course of the disease and the long-term prognosis.2–5,7–11
Chemotherapy is generally reserved for palliative cases, such as inoperable tumours or metastatic spread.2,8,10
The case that we report of a primary intraoral leiomyosarcoma it could be induced by ionizing radiation. It is essential that the clinician be familiar with the lesion, and anticipates the possible presence of this disease and makes early diagnosis. Treatment of primary leiomyosarcoma is radical tumour resection with histologically clear margins.
Ethical disclosuresProtection of human and animal subjectsThe authors state that no experiments were performed on human beings or animals as part of this investigation.
Confidentiality of dataAuthors state they have followed the protocols of their workplace about the data publication of patients.
Right to privacy and informed consentAuthors have obtained the informed consent from the patients or subjects referred to in the article. This document is in possession of the corresponding author.
Conflict of interestThe authors declare that there are no conflicts of interest.