Recurrent sub-maxillary gland disorders are relatively common. They are mainly caused by obstructive gland diseases. Other aetiologies are malignancies, autoimmune, or degenerative diseases. The traditional treatment of the submandibular gland is the surgical excision by a cervical approach. The advantages of this approach are: its simplicity, direct surgical vision, and speed of the procedure. The most important disadvantages are: unsightly cervical scar, and injury risk of the marginal branch of the facial nerve.
This paper presents and discusses the intraoral approach to the submandibular gland. The advantages over the conventional approach are: the elimination of the scar and the risk of injury to the marginal branch. The main disadvantages are: the technical difficulty, reduced vision, the longer surgical time, and the possibility of lingual nerve injury.
A total of 6 patients, 4 women and 2 men aged 25–60 years, underwent a sub-maxillectomy by intraoral approach in the Hospital Universitario de Canarias (Tenerife, Spain). In all cases, the aesthetic and functional results were very satisfactory, with only mild self-limited lingual nerve dysesthesia being observed at two months.
We present an alternative to the cervical approach for the submandibular glands; the intraoral approach. The major advantage of this technique is to eliminate the cervical scar.
Las alteraciones recurrentes de las glándulas submaxilares son unos trastornos relativamente frecuentes que se deben, generalmente, a una enfermedad obstructiva de la glándula, entre otras menos frecuentes, como la presencia de neoplasias, enfermedades autoinmunes o degenerativas. El tratamiento quirúrgico habitual consiste en la exéresis de la glándula submaxilar a través de un abordaje cervical. Las ventajas de este abordaje cervical son su sencillez, la visión directa del campo quirúrgico y la rapidez del procedimiento. Las desventajas más relevantes son la cicatriz cervical y la posibilidad de lesión de la rama marginal del nervio facial.
Se presenta y discute el abordaje intraoral como acceso a la glándula submaxilar. Su ventaja respecto al abordaje convencional es la eliminación de la cicatriz cervical y el riesgo de lesión de la rama marginal. Sus desventajas fundamentales son la dificultad técnica, la visión reducida, el mayor tiempo quirúrgico empleado y la posibilidad de lesión del nervio lingual.
En el Hospital Universitario de Canarias (Tenerife, España), a un total de 6 pacientes, 4 mujeres y 2 varones entre 25 y 60 años, se les realizó una submaxilectomía por abordaje intraoral. En todos los casos los resultados estéticos y funcionales fueron muy satisfactorios, tan solo leves disestesias del nervio lingual autolimitadas en 2 meses.
Se presenta una alternativa por vía intraoral al abordaje cervical para la realización de submaxilectomía, con la ventaja principal de eliminar la cicatriz cervical.
There are multiple processes and diseases that cause chronic symptoms in the submaxillary glands resulting in gland excision. The most common conditions for which gland removal is indicated include sialolithiasis, chronic sialadenitis, and benign and/or malignant tumour processes. The traditional technique to perform a submaxillectomy is via a cervical approach using a small submaxillary cervical skin incision, above the gland location, and 2–3cm away from the mandibular angle/body. The main advantages of this type of approach are: shortness, simplicity, and a large operative field. It provides a good view of the adjacent cervical structures and few complications of interest. Among them, we should mention potential damage to the marginal branch of cranial nerve VII, ranging from 1% to 7.7%1 based on the medical literature, or damage to the lingual or hypoglossal nerves, with an incidence ranging from 1.4% to 2.9%1,2. The only disadvantage of this approach is the scar produced in the patient's neck, particularly in the case of young patients.
The surgical alternatives we find in the medical literature to avoid this kind of approach and the neck scar are the face-lift or rhytidectomy approach, the endoscopic and/or robotic approach, and the intraoral approach.
We present our experience with the intraoral/transoral approach for submaxillectomies, and their advantages and disadvantages.
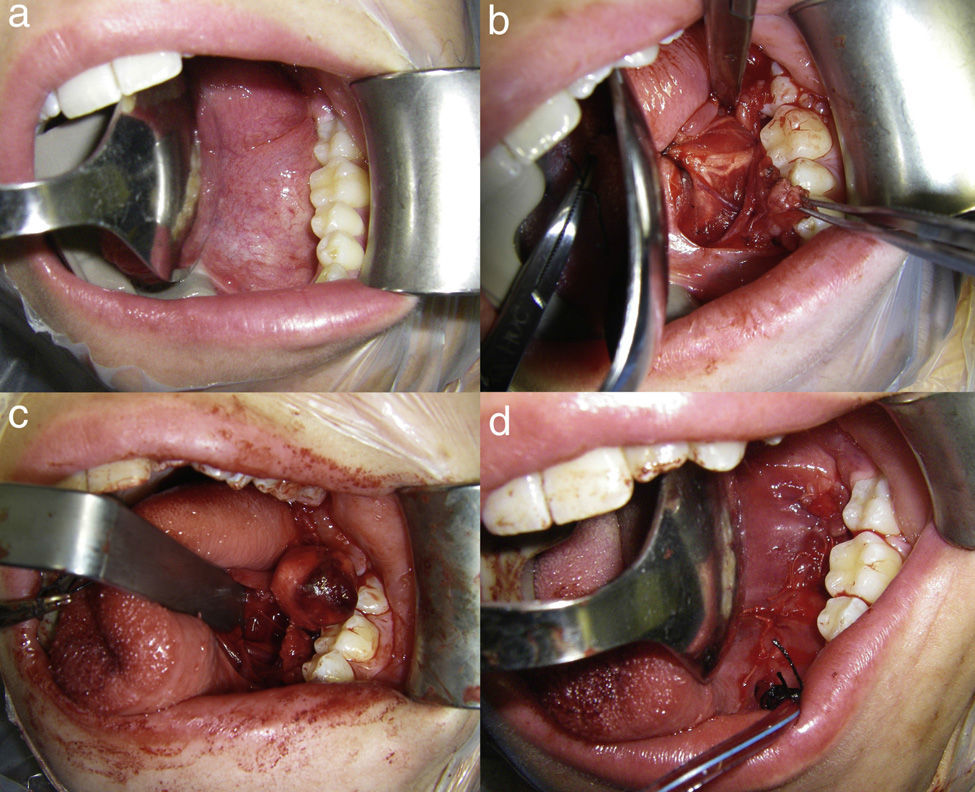
Surgical techniqueFollowing patient nasotracheal intubation and placement of a mouth-opener on the contralateral side, lidocaine with epinephrine with a concentration of 1:100,000 are injected into the floor/lateral base of the tongue. An approximately 4–5cm long incision is made along the lateral floor of the mouth, from the drainage orifice of the Wharton's duct up to the retromolar region (Fig. 1a). At first, the incision is superficial to avoid damaging the lingual nerve. When dissecting the anterior region of the mouth floor, the sublingual gland is found, and rejected to the medial side. The Wharton's duct and the lingual nerve are identified. The dissection is guided by the course of the Wharton's duct until reaching the submaxillary gland (Fig. 1b). Once the cranial pole of the gland has been identified, the gland is dissected along its entire perimeter. In this dissection phase, manual pressure by the assistant is required from the cervical area, in the submaxillary region, in a direction that allows him to lift the submaxillary gland to the mouth floor. In order to see the operative field clearly, the muscles of the mouth floor are separated, especially the mylohyoid muscle, and Allis tissue forceps are used for gland traction. The gland dissection over its entire perimeter is completed with haemostasis and ligation, if applicable, of the vascular structures. This dissection is performed surrounding the fascia encompassing the gland, thus minimising the risk of damaging the hypoglossal nerve and the marginal branch of the facial nerve.
(a) Preparation of the lateral floor of the mouth for the intraoral approach with mouth-opener and tongue retractor. (b) Incision in the mouth floor showing the lingual nerve, Wharton's duct, and sublingual gland. (c) Image showing the submaxillary gland on the mouth floor just about to be removed. (d) Access closure with absorbable suture in two planes, with the drain fixed to patient's canine tooth.
Once the gland has been released from its adhesions in the submaxillary area, it is removed to the oral cavity, and ligation of the Wharton's duct close to its drainage orifice is made to avoid leaving potential stones in the duct (Fig. 1c). Haemostasis of the surgical bed is made, and an intraoral Redon-type suction drain is placed and fixed to the lower canine tooth with 3/0 silk suture for the first 24h following surgery. To close the intraoral access, suture in two planes is used to prevent the passage of saliva onto the surgical bed and the loss of vacuum from the drain (Fig. 1d). Postoperative antibiotic therapy is necessary for the first five days after the surgery. In general, drain removal and hospital discharge occur 24h after the surgery with patient follow-up in an outpatient setting.
Materials and methodsA retrospective study of the submaxillectomies performed via intraoral approach between November 2008 and September 2012 at the Oral and Maxillofacial Surgery Department of Hospital Universitario de Canarias [Canarias University Hospital] (Tenerife, Spain) was conducted. In the study, the following variables were analysed: age, sex, diagnosis, surgical time, hospital stay, postoperative complications, sequelae, clinical follow-up, and aesthetic outcome. Patients who had submaxillary stones removed by intraoral approach without gland excision were excluded from this study.
ResultsA total of six submaxillectomies were conducted in six patients through an intraoral approach. Two of the patients were male and four were female, aged from 25 to 60 years. Four patients had been diagnosed with treatment-naïve chronic sialadenitis by sialendoscopy and two patients with pleomorphic adenoma of the submaxillary gland. The choice of this approach was based on the patients’ aesthetic demands, age, and presence of an associated medical condition. The cervical approach was chosen for patients who did not care about the scar, were older than 65 years, or had a condition being treated with antiplatelet or anticoagulant drugs.
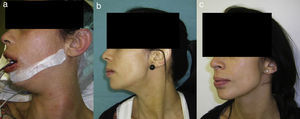
The mean surgical time was 103 (90–115)min, and the mean hospital stay from admission to hospital discharge was 2.5 days (2–3 days) (Table 1). Two patients had an infectious complication in the immediate postoperative period, which resolved with outpatient oral antibiotic therapy. Four patients experienced dysesthesia in the operated hemi-tongue, which disappeared spontaneously by the third month following surgery. Four patients also had mild self-limited haematoma in the submaxillary region that did not require any kind of additional treatment (Fig. 2). No patient developed long-term sensory or motor sequelae, wound retraction, or recurrence of their respective diseases. All the patients achieved an exceptional aesthetic outcome, without neck scar, only a scar line on the lateral floor of the mouth (Fig. 3).
Table of patients undergoing intraoral submaxillectomy.
| Age | Sex | Diagnosis | Size (cm) | Surgery time (min) | Hospital stay | Follow-up (months) | Complications | Sequelae | Nerve alterations |
|---|---|---|---|---|---|---|---|---|---|
| 58 | Male | Chronic sialadenitis | 3.3×2.2 | 115 | 3 | 30 | Infection | No | No |
| 54 | Male | Chronic sialadenitis | 3×2 | 90 | 3 | 28 | No | No | Mild dysaesthesiaLingual nerve 1 month |
| 45 | Female | Chronic sialadenitis | 3×3 | 110 | 3 | 26 | No | No | No |
| 60 | Female | Chronic sialadenitis | 4×3 | 92 | 2 | 24 | Infection | No | Mild dysaesthesiaLingual nerve 2 months |
| 29 | Female | Pleomorphic adenoma | 2×3 | 100 | 2 | 21 | No | No | Mild dysaesthesiaLingual nerve 1 month |
| 25 | Female | Pleomorphic adenoma | 2×1.5 | 115 | 2 | 18 | No | No | Mild dysaesthesia Lingual nerve 2 months |
The intraoral or transoral excision of the submaxillary gland was described by Miloro in 19993 and by Hong and Kim in 2000.4 In medical literature, many authors state that they have used the intraoral route for removing stones lodged in the Wharton's duct since the early 20th century, but it was De Martini who first published a submaxillectomy by transoral route in 19565. Other authors published similar approaches to the gland by intraoral route around that time.6,7 So far, in medical literature, there are few articles on series of submaxillectomies by intraoral route.2,8–16
Based on my experience and the opinion of all the authors in the specialised literature, the greatest difficulties with this technique are the limited operative field, poor visibility, and the potential risk of damaging nerve structures, particularly the lingual nerve. These circumstances require a laborious and careful dissection of the gland, especially the posterior and lower pole.
The risk of damaging the lingual nerve may be avoided with its adequate identification after the superficial incision of the mucosa and with a meticulous dissection. The 360° dissection should not be performed in the lingual nerve, except for the intersection with the Wharton's duct, for the purpose of maintaining its vascularisation and avoiding unnecessary manipulations. It is not advisable to place a locator, such as vessel-loops, to avoid accidental tractions of the nerve and thus its potential damage. During the immediate postoperative period, four patients from our series experienced dysesthesia in the operated hemi-tongue, possibly in relation to the manipulation of the lingual nerve. These cases of dysesthesia resolved spontaneously within the first two months following surgery; this circumstance is also mentioned by other authors in their respective papers.15,16
The potential injury of the facial vessels and hard-to-stop bleeding may be avoided by a sub-facial dissection of the gland and the ligation of its vasa vasorum, located at the posterior pole of the gland. Ligation of the facial artery and vein is not required for this technique and, if possible, should be avoided. Strict haemostasis of the surgical bed with placement of a Penrose drain is essential in these patients to avoid the development of haematoma in the region. In our experience, placing an intraoral drain, fixed to a canine tooth with 3/0 silk suture, has proved to be very useful and well-tolerated by patients, thus avoiding the small skin scar from the duct opening.
One of the technique disadvantages is surgical time, which is much longer if compared to the conventional cervical approach.2 As explained above, this is due to the greater technical difficulty and the poor visibility resulting from a small operative field; the learning curve of this technique will condition the reduction of the surgical time.
The obvious advantage of the intraoral approach, mentioned by every author, is the absence of scar in the neck area. In adult or elderly patients, an attempt may be made to hide the scar in the neck wrinkles, but the scar is especially evident in young patients, particularly in geographical areas with heavy sun exposure, such as Tenerife, and in races that tend to develop keloid scars. The advantage of avoiding a neck scar and achieving an excellent aesthetic outcome with identical functional results as the ones obtained with the conventional approaches is, in my view, the direction to follow and one of the targets that should guide our efforts in the future development of our specialty.
Other authors have used endoscopic techniques for the dissection of the submaxillary gland by intraoral route,10 while others have opted for robotic surgery17,18 through the face-lift or supraclavicular approaches. The use of the intraoral approach for conducting a submaxillectomy does not require any special equipment or technology. It is technically more complicated and laborious if we compare it to the traditional cervical approach. The clear advantage of avoiding a neck scar, especially in young patients, is a reason that warrants the use of this technique. Its use in benign cancers is questioned by some authors,15 but, in our opinion, this technique has been used in two patients with good results and without signs of recurrence in the long term. This approach is contraindicated in cases of malignant cancer or suspected malignancy.
A thorough analysis of each case and proper patient selection are essential in the use of this technique. In cases of infiltration into the fascia, large-sized lesions, or the presence of other complicating factors, it is advisable to use the traditional cervical approach.
ConclusionSix cases of intraoral approach for a submaxillectomy are reported as an alternative to the cervical approach. The clear advantages of this technique are the elimination of the unsightly neck scar and the possibility of damaging the marginal branch of the facial nerve. The most important disadvantages of this approach are the technical difficulty, the poor visibility, and the potential damage to the lingual nerve.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors declare that they do not have any conflicts of interest.
Please cite this article as: Arribas-García I, Gómez-Oliveira G, Martínez Pérez F, Serrano-Álvarez A, Sánchez Burgos R, Álvarez-Florez M. Abordaje intraoral de la glándula submaxilar. Presentación de un abordaje estético poco utilizado. Rev Esp Cir Oral Maxilofac. 2015;37:1–6.