In maxillary defects with a significant vertical component, the reconstruction of the alveolar process is advisable in order to avoid disproportionate long implant supported crowns. This article evaluates the safety and efficacy of the treatment of the atrophic posterior maxilla with the three-dimensional reconstruction technique with autologous bone graft associated to the sinus lift technique in the same procedure. The unique approach for the recipient site was a sub-periosteal mucosal tunnel made through a single vestibular vertical incision. This approach avoids exposure and resorption, the main complications in on-lay grafting.
Materials and methodsThis retrospective study included 12 cases of atrophic posterior maxilla treated consecutively with this combined technique between January 2011 and July 2012. The alveolar crest was reconstructed to a minimum width of 6mm, increasing its height and decreasing the interocclusal distance to achieve the established success criteria of accurate insertion of implants equal or larger than 3.8mm diameter and 11mm length.
ResultsThe average gain in bone height was 4.54mm. Implant surgery was carried out 4 months after augmentation. A total of 25 implants were inserted with a 96% success. Patients were followed-up for an average of 18 months after grafting.
ConclusionsTreatment of atrophic posterior maxilla with three-dimensional reconstruction, sinus lift and “tunnel” approach, is an effective technique that provides reliable and stable results, enabling dental rehabilitation with suitable implant supported crowns.
En defectos maxilares con importante componente vertical, es necesaria la reconstrucción del proceso alveolar previamente a la rehabilitación con implantes para evitar una longitud desproporcionada de las coronas protésicas. En este artículo se revisa el tratamiento del maxilar posterior atrófico mediante elevación de seno y técnica de reconstrucción alveolar tridimensional simultánea con autoinjerto óseo. Se utilizó como vía de abordaje un túnel mucoso subperióstico a través de una incisión vertical única para prevenir los principales problemas de los injertos en aposición: la exposición y la reabsorción.
Material y métodoSe han evaluado retrospectivamente 12 atrofias maxilares posteriores tratadas con esta técnica de forma consecutiva entre enero de 2011 y julio de 2012. El reborde alveolar se reconstruyó hasta un mínimo de 6mm de anchura a nivel crestal, incrementando su altura y disminuyendo la distancia interoclusal, para alcanzar el criterio de éxito establecido de fijación segura de implantes de, al menos, 3,8 y 11mm de diámetro y longitud respectivamente.
ResultadosLa ganancia media ósea en altura fue de 4,54mm. La cirugía de implantes se realizó hacia los 4 meses. Se colocaron 25 implantes con un 96% de éxito. El tiempo medio de seguimiento fue de 18 meses.
ConclusionesEl tratamiento del sector posterior maxilar atrófico mediante reconstrucción tridimensional con autoinjerto óseo, elevación sinusal y abordaje por tunelización es una técnica que proporciona resultados predecibles y estables, permitiendo la rehabilitación con coronas sobre implantes dentales de dimensiones adecuadas.
Sinus lift is a surgical technique indicated for rehabilitation treatment with implants of atrophic posterior maxilla. Long-term studies show a success rate of implants inserted by means of this technique, which is similar to that of non-augmented bone.1–3 When, after the loss of posterior maxillary teeth, besides hyperpneumatisation of the sinus, there has been an atrophy of the alveolar process leaving a defect with a significant vertical component, it is necessary to associate sinus lift with the reconstruction of the bone crest to restore the anatomy that has been lost and to avoid disproportionate long implant supported crowns.
Multiple techniques have been described for reconstruction of the atrophic maxillary ridge: corticocancellous on-lay and interposition block bone graft; guided bone regeneration with titanium mesh or membranes; distraction osteogenesis, etc. There is consensus among the authors on the preference for the use of autologous bone, either combined or not with any type of biomaterial, for this augmentation surgery.4 Donor areas may be extraoral (mainly the iliac crest and the calvarium) or intraoral (chin and mandibular retromolar area).
The main short-term problem of bone height alveolar reconstruction with block grafting is wound dehiscence, which results in bone exposure, its contamination, and partial or total graft loss.5 A way of reducing the incidence of this complication is to avoid crestal incisions that imply surgical wound closure over the bone graft. The approach consisting of a subperiosteal tunnel through a vertical vestibular incision away from the area subject to reconstruction preserves the mucoperiosteum, which will cover the whole graft intact. Through this single incision, the conventional sinus lift technique may be simultaneously applied.
Another important problem of alveolar reconstruction with on-lay grafting is the high incidence of mid-to-long-term resorption. The larger and more cortical the graft structure is, the slower and more difficult the complete revascularization process of the graft becomes, which causes necrosis of the central areas and its resorption over time.6 In the case of the iliac crest, besides, the factor of its endochondral origin leads to a higher resorption rate.7
Structurally, the ideal graft would have a thin, though resistant, outer cortical layer and a dominant inner cancellous layer. The three-dimensional (3D) reconstruction technique described by Khoury consists in creating a graft having these characteristics and adapted to each particular case.6
In this article, a retrospective evaluation of the treatment of atrophic posterior maxilla with a significant vertical component is made by simultaneously performing sinus lift and alveolar process reconstruction with the 3D technique. For the latter, block bone autologous grafts cut in thin cortical slices and arranged in the shape of a box with particulate bone inside were used. The donor zones used were the mandibular retromolar area and the calvarium, as appropriate. As an approach to atrophic maxilla, the subperiosteal tunnel made through a single vestibular vertical incision was used.
Materials and methodsPatient screeningFor this study, 12 cases of atrophic posterior maxilla reconstruction treated consecutively by the authors through sinus lift and 3D reconstruction with a tunnel approach were retrospectively evaluated between January 2011 and July 2012. This study included patients with a combined defect of both height and width of maxillary alveolar ridge, behind the canine, of any aetiology whatsoever, and where autologous bone was used for both 3D reconstruction and infrasinusal filling.
The success criterion was established on accurate insertion and subsequent osseointegration of dental implants in the reconstructed zone to a minimum width of 3.8mm by 11mm in length. This implant diameter requires a minimum crest width of 6mm, with no vestibular reduction, so that fixation may have stable bone coverage of, at least, 1mm considering its whole surface. Therefore, the purpose of augmentation surgery is to achieve a properly sized alveolar ridge to safely accommodate the planned implants avoiding excessive interocclusal distances.
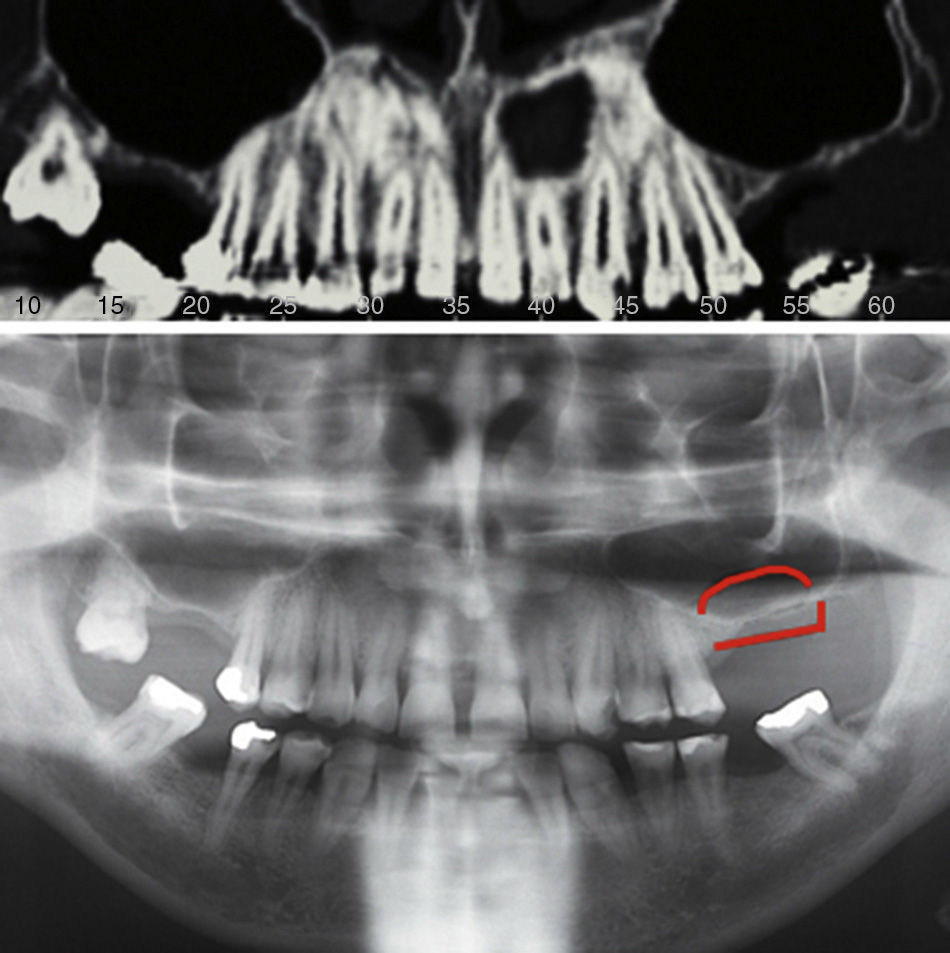
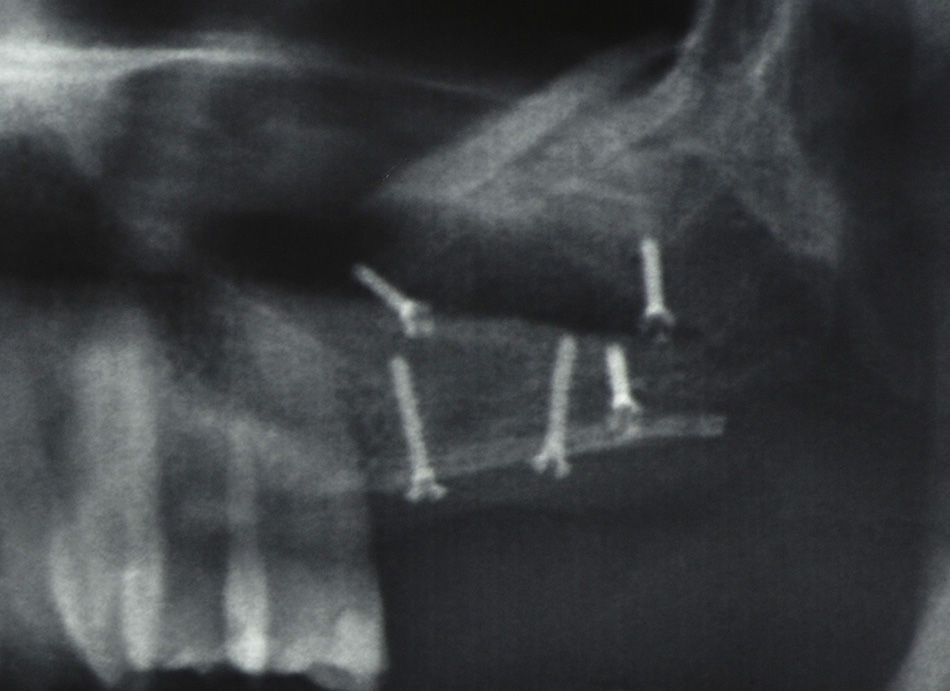
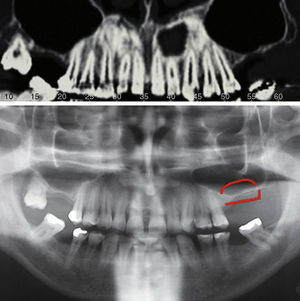
For diagnosis and treatment planning, orthopantomography (OPG) and cone beam computed tomography (CBCT) were performed in all cases prior to surgery (Fig. 1). At that moment, the procedure was contraindicated in patients with sinus infection and heavy smokers. Patients were informed about the procedure and signed the corresponding Informed Consent Form.
Surgical techniqueAntibiotic prophylaxis was performed with amoxicillin-clavulanic acid 1g/250mg PO every 12h, starting 1h before the surgical intervention and continuing for 7 days. Interventions were conducted under general anaesthesia and nasotracheal intubation or under local anaesthesia and conscious intravenous sedation. In all cases, both the donor zone and the recipient zone were infiltrated with local anaesthesia using a vasoconstrictive drug (articaine hydrochloride with adrenaline with a concentration of 1:100,000).
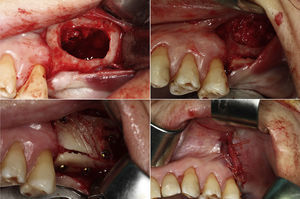
The approach used in the recipient zone consisted of a single vestibular vertical mucoperiosteal incision away from the defect. A wide subperiosteal tunnel was made through it, detaching the anterior wall from the maxillary sinus and including the alveolar defect at vestibular and crestal level. Subsequently, sinus lift was performed in a conventional way, opening a bone window on the anterior sinus wall with a tungsten carbide bur for a hand piece, which was extracted and preserved for later use. Then, the Schneiderian membrane was lifted and its integrity was verified.
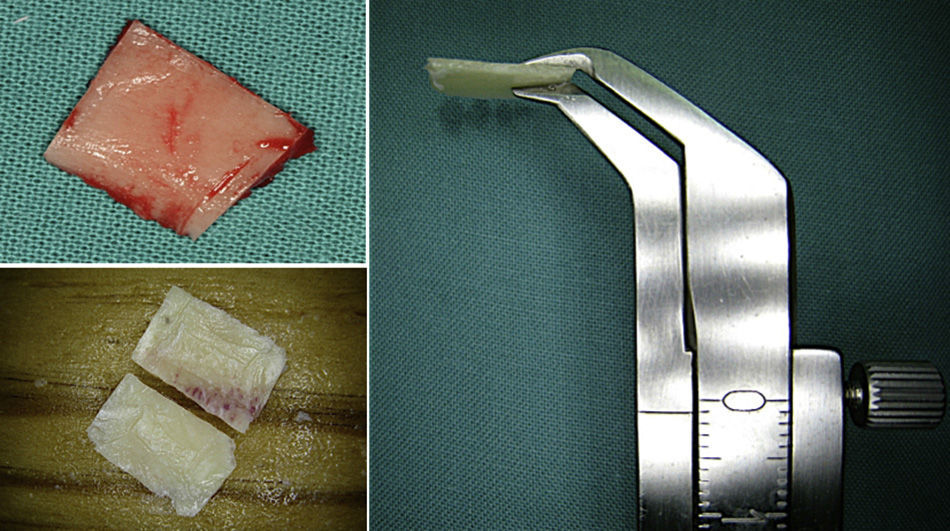
The approach used in the mandibular donor zone consisted of a mucoperiosteal incision on the lateral ridge at the second molar level towards the anterior edge of the external oblique ridge. After subperiosteal detachment, the retromolar vestibular area was exposed. With a microsaw disc of 0.25mm thick (Frios Microsaw, Dentsply), two vertical linear cuts were made at cortical level, at a distance based on the defect to be treated, joined on their inferior edge by another longitudinal cut. Upper edges were joined by means of linear cortical microperforations made with a thin lancet bur. Using a thin chisel, a mandibular branch vestibular corticocancellous fragment measuring about 4mm thick was obtained. In those cases where the calvarium was used as donor zone, access thereto was achieved through a parasagittal longitudinal incision in the scalp, by sub-pericranial detachment at the non-dominant parietal bone. From the external diploe, a corticocancellous block graft was equally obtained using a microsaw disc. The graft obtained from any of the areas was sagittally divided into two thin slices of about 1mm thick (Fig. 2).
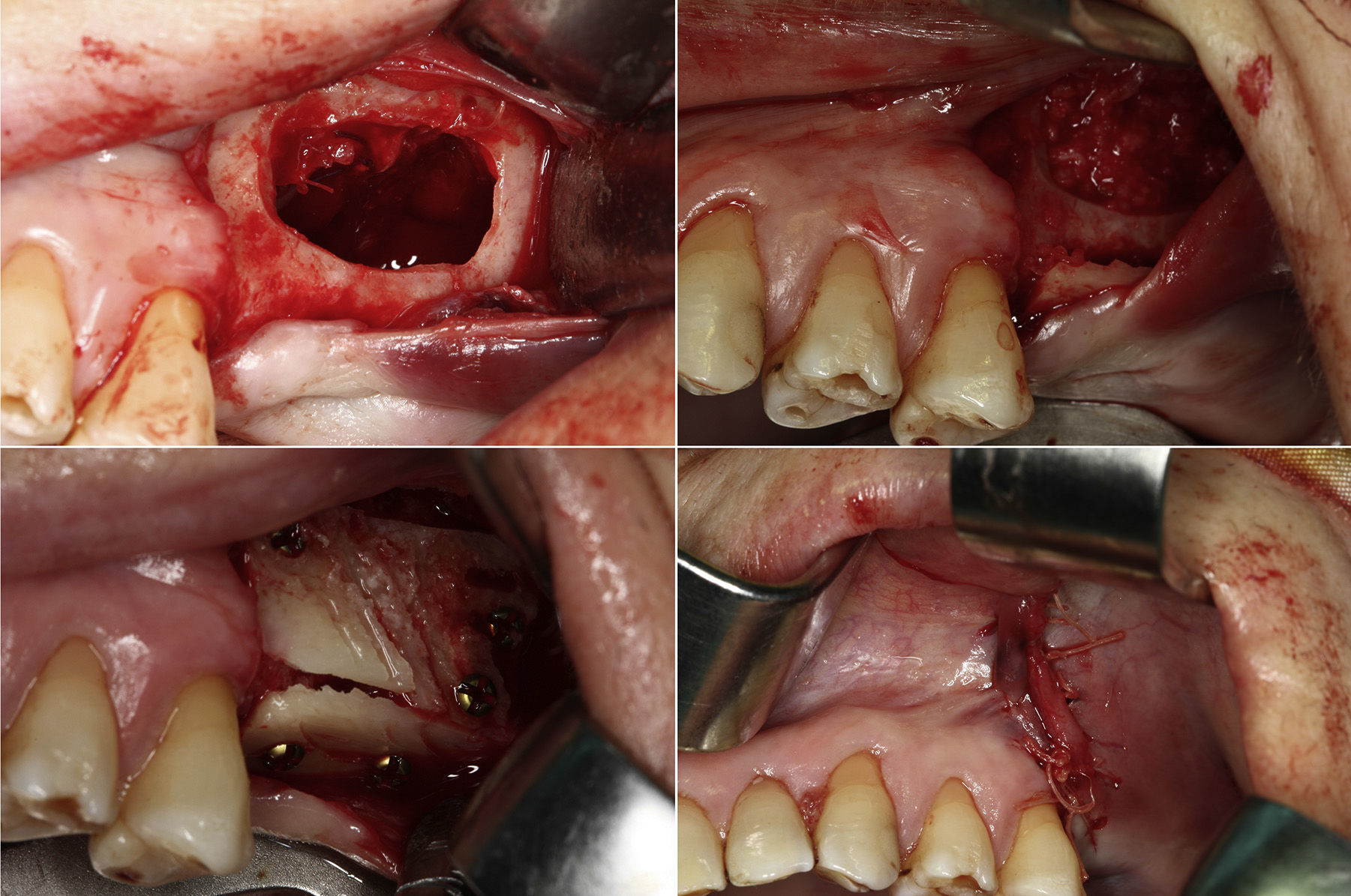
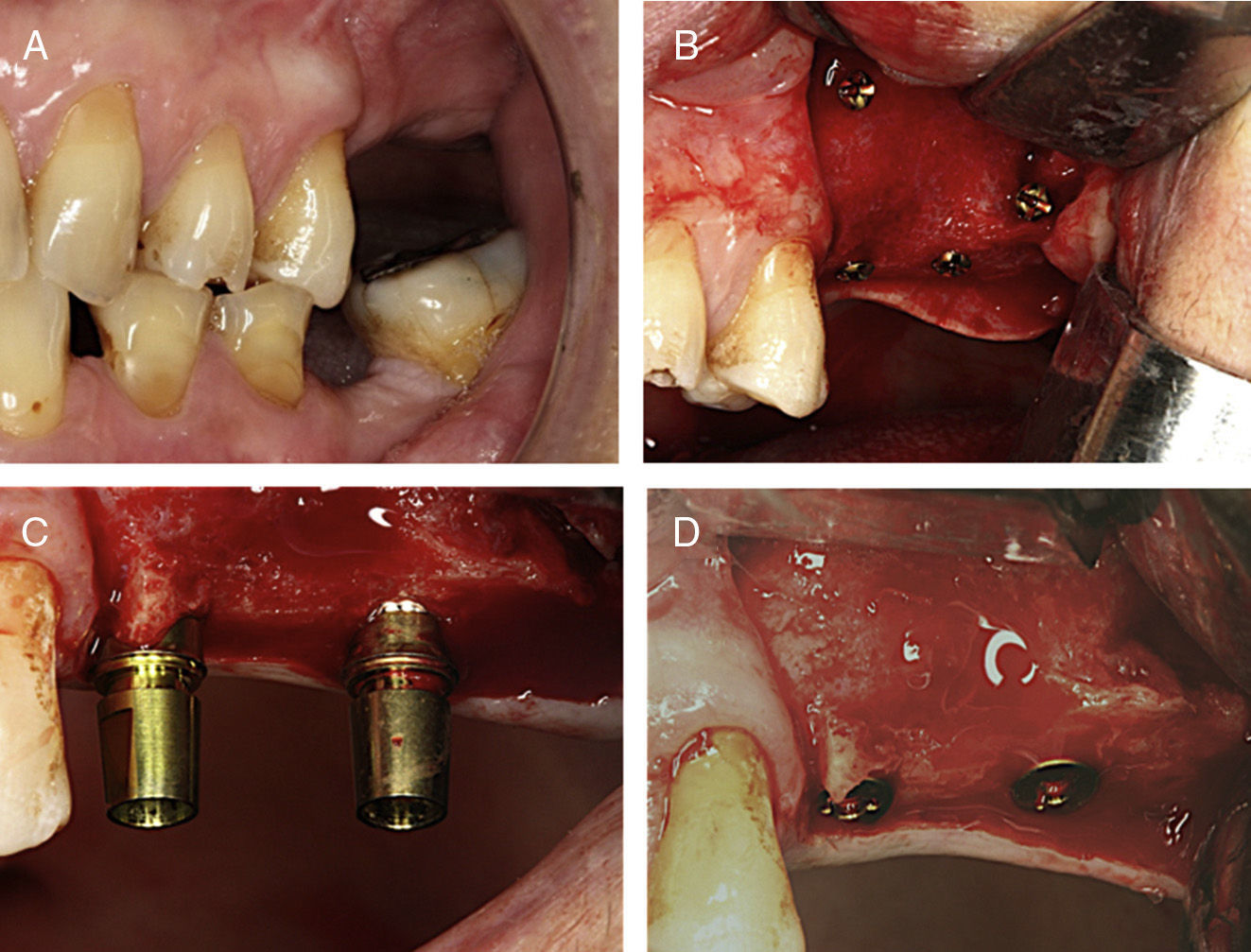
Part of the graft was particulate in small fragments and inserted in the subantral space created after sinus membrane lift. As a roof of this new cavity, the bone window of the maxillary wall extracted for sinus access was placed in contact with the lifted Schneiderian membrane. Through the tunnel, one of the monocortical graft slices was inserted after being carved, placing it in the crest position and fixing it with osteosynthesis microscrews of 1.2mm (Stryker, Leibinger, Germany). The other cortical slice was placed in vestibular position and fixed with two microscrews, thus completing the three-dimensional reconstruction of the defect. In the cases where this slice did not cover the whole sinus window, a titanium micro mesh (Stryker) or a collagen reticulated reabsorbable membrane (Collagene AT, CDOO S.R.L.) was used to complete the closure. The incision was closed with a single-plane absorbable polyglactin 4/0 suture (Vicryl rapide, Ethicon) (Fig. 3).
(A) Single vestibular vertical mucosal incision and subperiosteal tunnel. Left sinus lift. Schneiderian membrane perforation repair with absorbable suture 6/0. (B) Crest graft slice positioned and fixed with two microscrews through the tunnel. Subsinusal filling with particulate autologous bone. (C) Cortical graft slice fixed in vestibular position with three microscrews. (D) Single-plane mucoperiosteal closure.
To protect the cranial donor zone and to avoid sinking thereof, the generated defect was covered with a malleable titanium dynamic mesh (Stryker) fixed with microscrews and, on top of it, the scalp itself and other scalp planes were sutured.
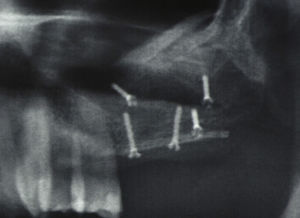
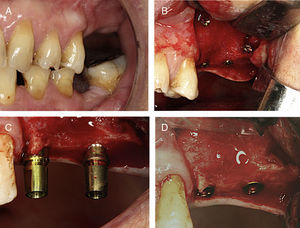
Between months 4 and 6, a control OPG, a vertical gain measurement, and implant phase planning (Fig. 4) were performed. The osteosynthesis screws and dental implant fixation (Dentsply Implants, Xive model, with Cell Plus original surface, Manheim, Germany) were conventionally removed under local anaesthesia. The approach used in this surgery consisted of a pure crestal incision or a palatine paracrestal incision with vestibular displacement based on keratinised gum arrangement (Fig. 5).
After about four months of osseointegration, implants were exposed, gingiva formers were placed, and the prosthetic phase was started (Fig. 6).
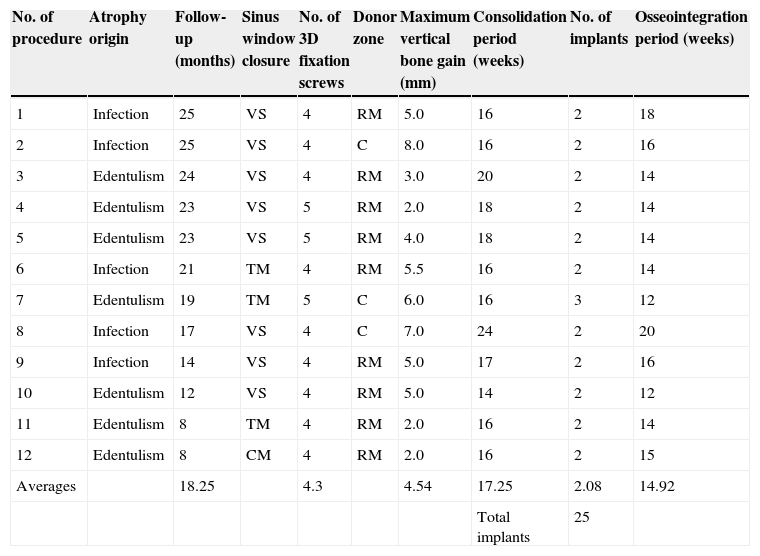
ResultsThe results of augmentation surgery are summarised in Table 1. Twelve atrophic posterior maxilla reconstructions were performed in 11 patients (six male and five female subjects; one female patient was subject to a bilateral surgery). The mean age of the patients was 47.3 years, within a range of 26–57. In six patients, the procedure was performed under local anaesthesia and conscious intravenous sedation. In the remaining five, where any type of associated surgery was conducted, the calvarium was used as graft donor area or a bilateral procedure was performed – the reconstruction was performed under general anaesthesia.
Clinical data: implant and augmentation surgery.
| No. of procedure | Atrophy origin | Follow-up (months) | Sinus window closure | No. of 3D fixation screws | Donor zone | Maximum vertical bone gain (mm) | Consolidation period (weeks) | No. of implants | Osseointegration period (weeks) |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Infection | 25 | VS | 4 | RM | 5.0 | 16 | 2 | 18 |
| 2 | Infection | 25 | VS | 4 | C | 8.0 | 16 | 2 | 16 |
| 3 | Edentulism | 24 | VS | 4 | RM | 3.0 | 20 | 2 | 14 |
| 4 | Edentulism | 23 | VS | 5 | RM | 2.0 | 18 | 2 | 14 |
| 5 | Edentulism | 23 | VS | 5 | RM | 4.0 | 18 | 2 | 14 |
| 6 | Infection | 21 | TM | 4 | RM | 5.5 | 16 | 2 | 14 |
| 7 | Edentulism | 19 | TM | 5 | C | 6.0 | 16 | 3 | 12 |
| 8 | Infection | 17 | VS | 4 | C | 7.0 | 24 | 2 | 20 |
| 9 | Infection | 14 | VS | 4 | RM | 5.0 | 17 | 2 | 16 |
| 10 | Edentulism | 12 | VS | 4 | RM | 5.0 | 14 | 2 | 12 |
| 11 | Edentulism | 8 | TM | 4 | RM | 2.0 | 16 | 2 | 14 |
| 12 | Edentulism | 8 | CM | 4 | RM | 2.0 | 16 | 2 | 15 |
| Averages | 18.25 | 4.3 | 4.54 | 17.25 | 2.08 | 14.92 | |||
| Total implants | 25 |
C: calvarium; VS: vestibular slice; CM: collagen membrane; TM: titanium mesh; RM: retromolar area.
The mandibular retromolar area was used as bone graft donor zone in eight patients, including the bilateral case, which required reconstruction in both sides of the mandible. In the other three cases, the calvarium was used as donor zone.
The average gain in bone height was 4.54mm, within a range of 2–8mm. A minimum of two microscrews was used to fix each cortical bone slice; three cases required the use of an additional screw. The average of microscrews required for complete reconstruction was 4.25.
The sinus access window was closed with a cortical graft slice. In three cases, this closure was completed with a titanium micro mesh fixed with microscrews and, in another case, with a collagen membrane and membrane nails.
As intraoperative incidents, three sinus membrane perforations were reported upon lift thereof. Two of them were sutured, and the other was repaired by folding it and placing a collagen sponge. In one case, there was a mucosal laceration at the tunnel access upon distal fixation of bone grafts. Access achieved by a single vertical mucoperiosteal incision was enough in all cases to perform sinus lift and alveolar reconstruction simultaneously, maintaining a closure under no strain.
Mean follow-up time was 18 months, within a range of 8–25 months. As a complication related to obtaining the graft in the mandibular retromolar area, three temporary lip hypoaesthesias were reported in the mentonian nerve region. All resolved spontaneously and completely within a maximum period of 6 months. At the recipient zone level, there were two crest graft fractures that led to movement of the mesial fragment, which was prematurely removed. In one of the cases, sinusitis was reported; it was managed with medical treatment, but it caused a partial graft loss, which was verified upon implant surgery. In the case of the closure of the sinus access window with a collagen membrane, premature extrusion of part of the filling particulate bone occurred, causing discomfort at the bottom of the patient's labial vestibule. As minor complications, a minimum bone graft exposure on the palatal side, which resolved by milling, and a small wound dehiscence away from the graft with no consequences whatsoever were recorded.
Implant surgery was carried out between weeks 14 and 24, with an average of 17.25 weeks. A total of 25 implants were inserted. In all cases, two implants of 11 or 13mm in length were fixed, except for one case where three implants were inserted. A total of 23 implants had a diameter of 3.8mm; one of 4.5mm and another one of 3.4mm. A 96% success was achieved in relation to augmentation surgery in our series, according to established criteria (fixation of dental implants equal to or larger than 3.4mm×11mm). Implant osseointegration success was 100% after a mean period of 14.92 weeks (range 12–20).
DiscussionThe two major problems of surgical reconstruction of the maxilla with on-lay bone grafting are the high short-to-mid-term resorption rate and the high incidence of dehiscence of the surgical wound.8–10 As far as resorption is concerned, some authors point to 41.5% bone height loss in the first 6 months after the insertion of bone grafts obtained from intraoral areas, such as the chin or the mandibular branch.11 When using bone of endochondral origin, as in the case of the iliac crest, this resorption occurs quickly during the bone remodelling process.7 Even when an external approach is used for graft placement and fixation, its vertical resorption will be high. Bell et al.12 report 23% resorption, within 6 months, of corticocancellous iliac crest block grafts inserted extraorally for the treatment of severe mandibular atrophy.
The graft neovascularisation process, which occurs after its fixation in the recipient bed, is essential for long-term feasibility thereof. According to other authors,6,13 this revascularisation, which should be fast and complete, is unlikely to be fully achieved in the case of cortical bone blocks. Before vessels neoformed from the soft tissue coverage and the recipient bed reach the inner part of the graft, necrosis phenomena have already taken place at this level, and it has received macrophage activity, which eventually results in its posterior resorption.
The so-called 3D reconstruction technique developed by Khoury consists in generating a graft whose structure combines a thin cortical bone outer layer, which provides consistency while enabling vascular penetration, with particulate bone filling, thus favouring fast revascularisation and a lower resorption.6 This characteristic is clinically evident upon implant surgery, where bone reconstruction volume is practically equal to baseline volume 4 months earlier (there is no resorption around the osteosynthesis screws), which enables an efficient osseointegration of the fixing elements.
The biological behaviour of the calvarium bone is similar to that of the mandibular branch, since they share structural characteristics and an embryological origin. The mandibular donor zone reacts with more inflammation and pain and implies a potential complication of nerve injury, usually temporary, in the inferior alveolar nerve, which sometimes gets exposed when removing the graft block. The advantages of the use of cranial bone as a donor zone include an almost asymptomatic postoperative period and the absence of significant complications when a careful technique is implemented.14 Its main disadvantages are the use of a second extraoral operative field and the need for general anaesthesia. If there is no additional surgery, local anaesthesia with conscious intravenous sedation monitored by an anaesthetist is usually enough when the mandibular retromolar area is used. Level of consciousness monitoring using the bispectral index provides good results.15
Bone graft immobilisation is one of the basic requirements for its correct neovascularisation. In our series, there were two crestal layer fractures that led to movement of the mesial fragment, which demanded extraction thereof. It is worth mentioning that the crest graft lies on its anterior margin over the inferior edge of the vestibular slice. Therefore, proper fixation of the vestibular graft is essential. In most cases, two screws for each slice are enough for a proper graft fixation.
Early bone graft exposure leads to its contamination and, in most cases, to the total or partial loss thereof.16,17 The subperiosteal tunnel approach enables the wound to remain wide apart from the bone graft. There is no wound strain and, therefore, a lower possibility of dehiscence. This circumstance is essential, mainly in cases of vertical augmentation. On the other hand, this approach does not alter the continuity of the periosteum that covers the grafts, maintaining its osteoregenerative capacities intact. Initially, this approach was described for preprosthetic surgery for mandibular alveolar ridge augmentation with hydroxyapatite.18 A single vestibular vertical incision provides enough access for 3D reconstruction of posterior maxilla with simultaneous sinus lift.
Another atrophic posterior maxilla reconstruction technique may be tissue regeneration guided with different biomaterials. The potential implementation of these procedures with approaches that would prevent crestal incision could reduce the high incidence of exposure of the membranes or meshes used in the technique.19,20
The treatment alternative to alveolar bone reconstruction in atrophic posterior maxilla is sinus lift with implant fixation in the subsinus cavity and rehabilitation by means of proportionally long crowns with the possibility of support on pterygoid implants. In scientific literature, there is more and more evidence of treatment efficacy with short implants in the upper maxilla, which may justify, from a strictly functional point of view, the choice of this procedure, avoiding reconstructive surgery.21–23
ConclusionsAtrophic posterior maxilla reconstruction with a significant vertical component by the combination of 3D reconstruction, sinus lift, and a single tunnel approach offers predictable and stable outcomes regarding rehabilitation with proportionately sized dental implants and prosthetic crowns.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors declare that they do not have any conflicts of interest.
To professor Pedro Infante Cossío for his work, dedication, and teaching regarding review of this article and other publications.
Please cite this article as: Restoy A, Pizarro VL, Ordóñez V, Lara J, Doussinague BR, Domínguez-Mompell JL. Tratamiento del maxilar posterior atrófico mediante técnica de reconstrucción tridimensional con elevación de seno y abordaje «en tunel». Rev Esp Cir Oral Maxilofac. 2015;37:7–14.