Temporomandibular-ankylosis brings extensive limitations on the patient quality of life. Surgical treatment is frequently necessary associated with a continuous rehabilitation. The anatomy of this region and potential complications of this surgery must be thoroughly known to avoid iatrogenic injuries.
Case presentationA young patient underwent surgical treatment of congenital bilateral ankylosis with disastrous consequences such as facial palsy, deafness and cerebrospinal leaks on the right side related to intraoperative trauma involving structures of the external, middle and inner ear.
ConclusionSince there is no corrective treatment for this type of injuries, the craniomaxillofacial surgeon and other professionals who carry out interventions of this nature need perfect knowledge of the anatomy of the temporal bone and lateral skull base, taking into account the risk of surgical disasters like the one here reported.
La anquilosis temporomandibular se asocia a importantes limitaciones de la calidad de vida del paciente. Con frecuencia, es necesario un tratamiento quirúrgico asociado a una rehabilitación continua. Para evitar las lesiones yatrogénicas, se requieren conocimientos exhaustivos de la anatomía de esta región y de las complicaciones potenciales de la cirugía.
Presentación del casoUn paciente joven se sometió a tratamiento quirúrgico de una anquilosis bilateral congénita con consecuencias catastróficas, como parálisis facial, sordera y extravasación de líquido cefalorraquídeo en el lado derecho relacionada con el traumatismo intraoperatorio, que afectó a las estructuras del oído externo, medio e interno.
ConclusiónPuesto que no se dispone de un tratamiento corrector para este tipo de lesiones, tanto el cirujano experto en cabeza y cuello como otros profesionales que efectúan intervenciones de esta naturaleza necesitan unos conocimientos óptimos sobre la anatomía del hueso temporal y la base del cráneo, y deben tener en cuenta el riesgo de una catástrofe quirúrgica como la descrita en este paciente.
The temporomandibular joint (TMJ), essential for normal function of the mouth, chewing, speech and nutrition, is synovial and composed of hard cartilage, which allows correct connection and sliding of the involved bone. The fibrocartilaginous tissue is avascular and has high regenerative capacity.1
This structure is formed by the temporal bone (glenoid fossa and articular eminence) and mandibular condyle; the main muscles implicated in the control of TMJ are the temporal and masseter. There are a lot of TMJ disorders, like ankylosis and the most common dislocation of the joint.2,3
The extent of mouth opening is an important parameter for assessing the functionality of this joint.4 The opening considered normal ranges 35–40mm and can be done by specific measurement instruments.5,6
TMJ ankylosis causes great discomfort and the patient often requires multidisciplinary care to soften the impact of this condition on their quality of life. Treatment often involves surgery with greater or lesser degree of difficulty and requiring great anatomical knowledge not only of TMJ, but also of all related structures.7,8 The risks of iatrogenic injuries and sequelae increase, often deteriorating the patient condition, when this complex region is approached without the proper preparation.9
We report the case of a young woman who underwent surgery for correction of bilateral TMJ ankylosis, which resulted in a complete disaster, causing unacceptable otological and neurological sequelae.
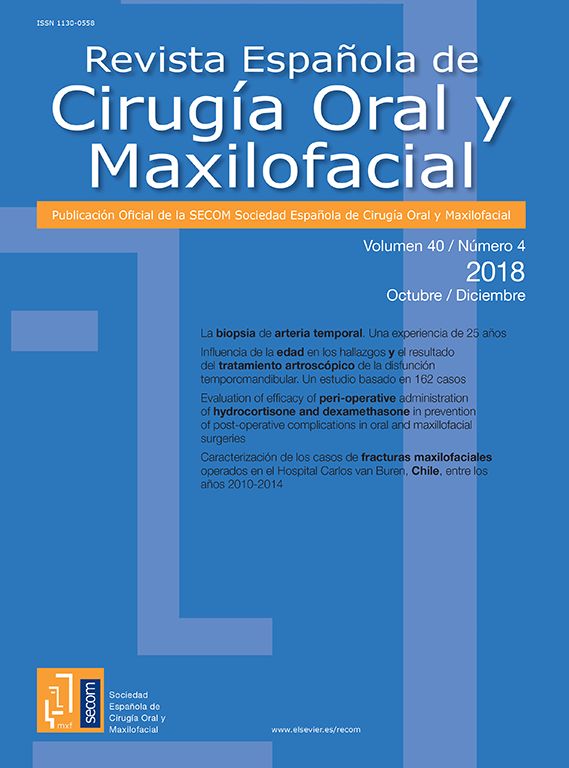
Case presentationA Brazilian female patient aged 22years old was referred to our clinic three months after undergoing surgery in another service to correct congenital bilateral TMJ ankylosis with placement of acrylic spheres, titanium condylar screws and plates in both joints (Fig. 1).
This illustration shows the TMJ reconstruction. Note the close relationship between the external auditory meatus and the TMJ and that the right side is more damaged than the left side. White arrow=external auditory meatus; black arrow=TMJ (prosthesis=acrylic ball has been placed in position); yellow arrow=titanium material. (For interpretation of the references to color in this figure legend, the reader is referred to the web version of the article.)
A pre tragal approach was taken to perform this surgery with subfascial dissection by planes (subfascial). The TMJ ankylosis was removed and placed a prosthesis made of acrylic, in ball format, to fill the empty space created by this procedure. The condyles became fractured during the surgery and it needed a further fixation with titanium plates and screws.
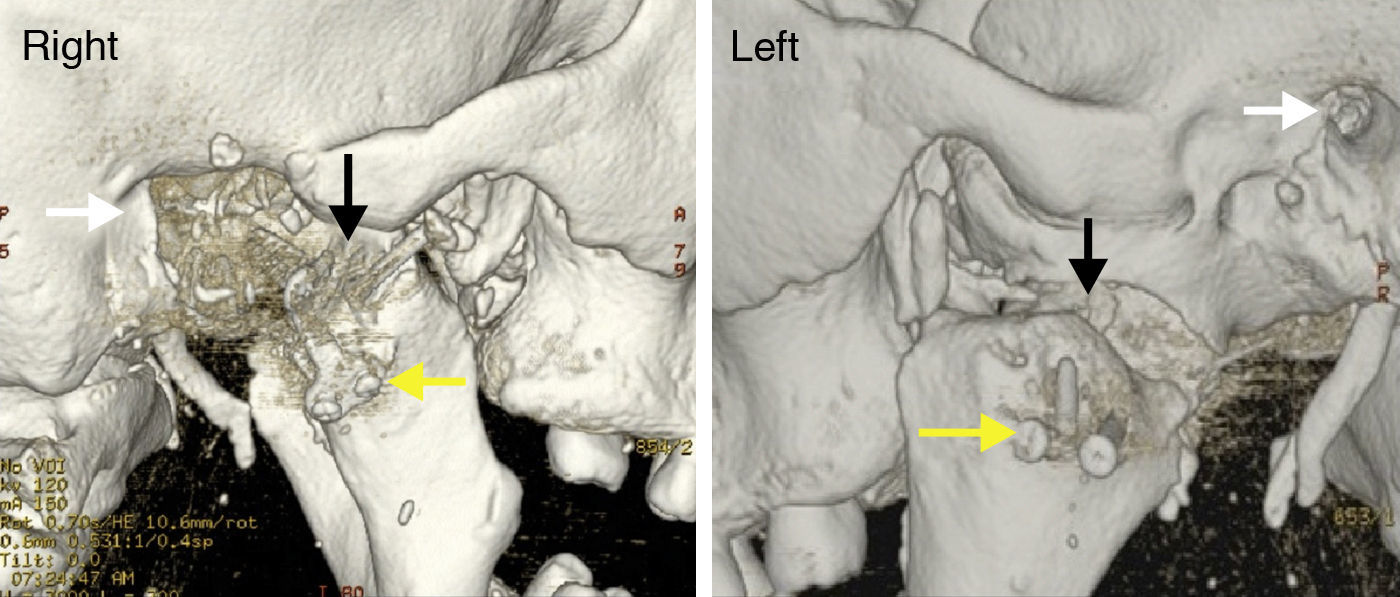
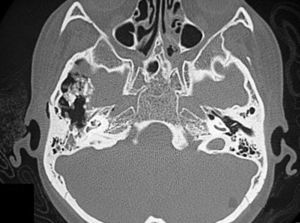
In addition to complaining of the lack of facial movement and hearing loss on right side, immediately after surgery, she reported having developed a cerebrospinal leak in the right ear, treated with lumbar shunt, which closed spontaneously during the first month. During physical examination, she showed right peripheral facial palsy grade IV (House-Brackmann scale) (Fig. 2). Otoscopy showed right prosthetic joint covered by soft tissue protruding and blocking the entire external auditory canal. The audiometric test resulted in deafness on the right side and normal hearing on the left side. Previous electromyography revealed complete impairment in the right facial nerve without reinnervation signs. Finally, CT scan showed extensive destruction in the lateral skull base region, involving middle and inner ear and the middle fossa floor (Fig. 3).
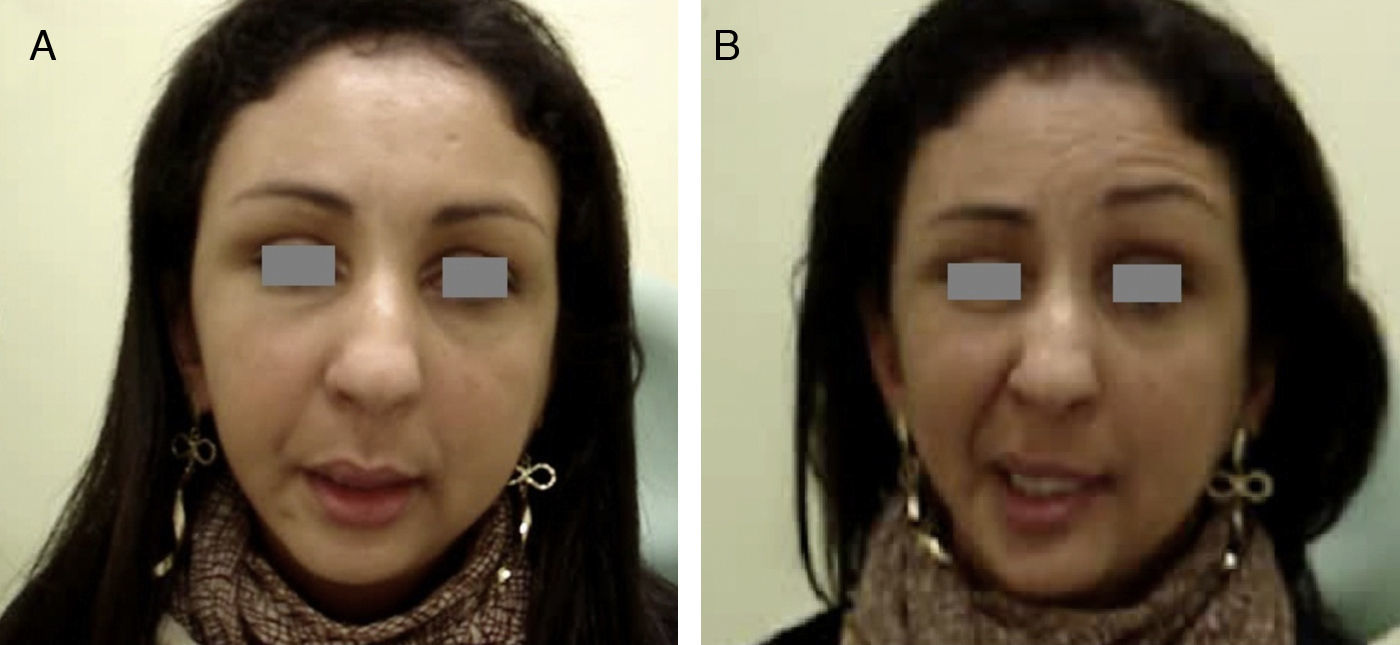
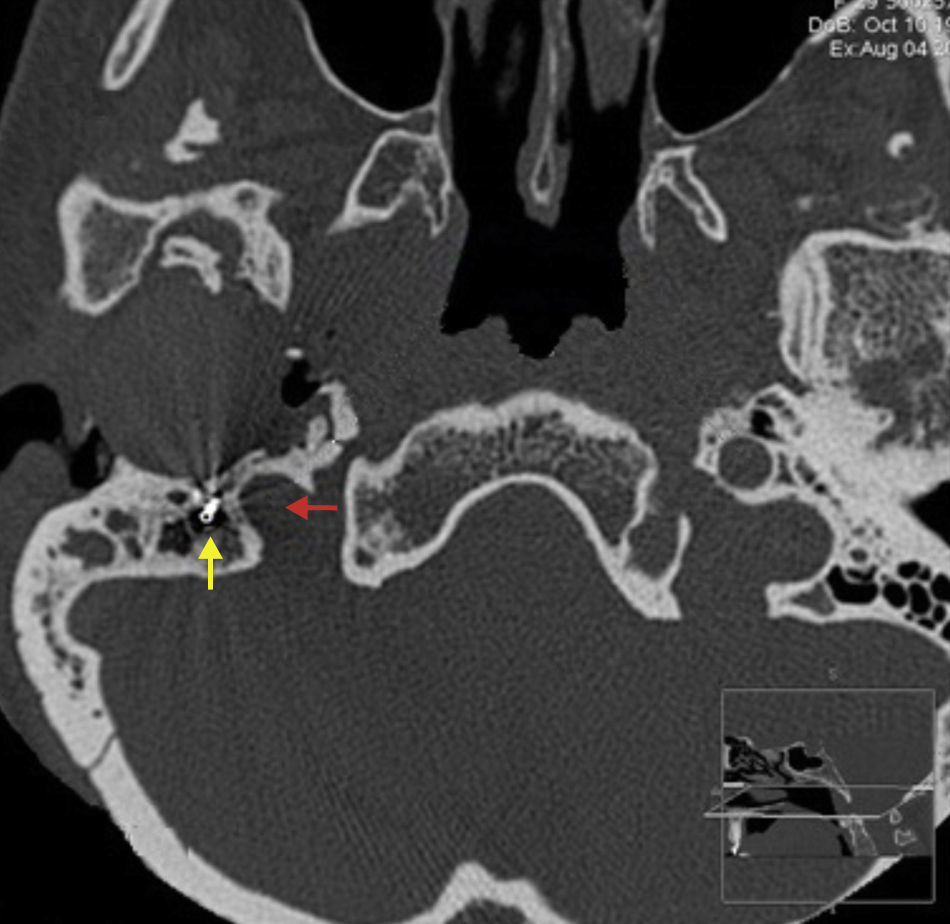
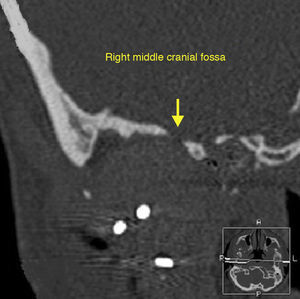
After a careful evaluation of the temporal bone, using a high-resolution computed tomography, the following situations were observed: discontinuity along the top edge of the right temporal bone, which suggests an area of continuity between the middle fossa floor and the surgical site (Fig. 4). Signs of calcification were observed around the right cochlea, mainly in the basal turn, compatible with labyrinthitis ossificans. There was also a hyperdense material projected next to the vestibule and oval window, which may correspond to materials used during surgery or residual calcifications.
This illustration shows the proximity of the middle fossa with the middle ear (right side). Note the destruction in the region of the lateral skull base structures and the involvement of the middle fossa floor. Yellow arrow: Area of discontinuous bone of middle fossa floor. (For interpretation of the references to color in this figure legend, the reader is referred to the web version of the article.)
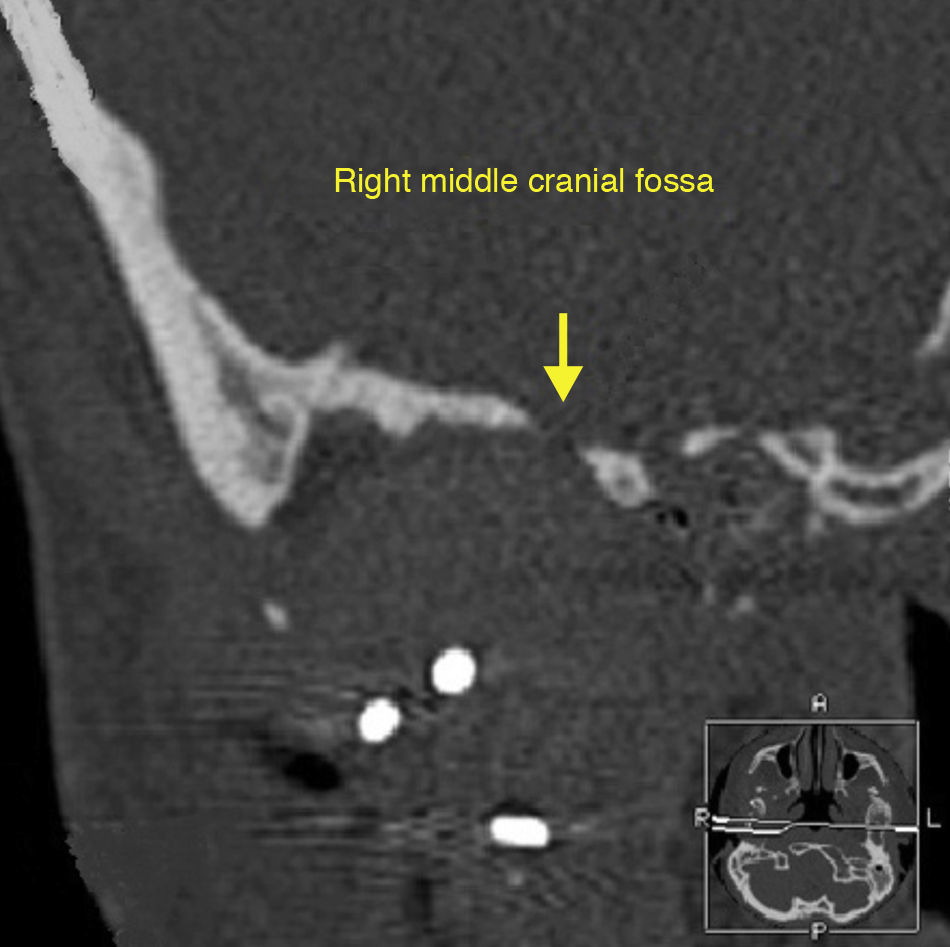
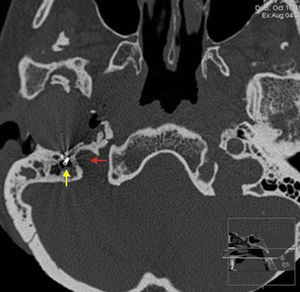
Postsurgical changes extending to the proximal portion of the right carotid canal (in the topography of the first segment of the petrous portion of the carotid artery), which is tightened, can be observed on the CT scan (Fig. 5). It should be noted, however that there is also a slight narrowing of the rest of the right carotid canal (compared with the contralateral side), which corresponds to a patient constitutional change (anatomic variant). An intracranial carotid angiography would be necessary to confirm possible iatrogenic injury of the right carotid artery.
This illustration shows the proximity of the titanium material with the internal carotid artery (right side). Note that a fatal result could happen if this prosthesis had been inserted a few millimeters medially. Yellow arrow: titanium material; red arrow: internal carotid artery. (For interpretation of the references to color in this figure legend, the reader is referred to the web version of the article.)
Eustachian tubes were unchanged during the radiological evaluation. Gross calcifications were also observed adjacent to the ossicular chain, at the right ear, compatible with tympanosclerosis.
A surgical repair of the facial nerve was offered to the patient; however, because of the possibility of losing the prosthesis in this procedure, she refused the surgery. During an 8-year follow-up, she maintained deafness in the right ear, mouth opening of 2.5cm and right facial palsy grade III (House-Brackmann scale), with multiple synkinesis and muscle orolabial spasticity.
So after conclusion of clinical evaluation (mouth opening of 2.5cm, no pain) and considering the patient decision we decided to do only clinical follow-up, with no exchange of prosthesis or any other surgical approach of TMJ ankylosis. The patient is 8years postoperatively and has a good functional outcome regarding their TMJ ankylosis, so apparently there will be no need to exchange her prosthesis.
DiscussionIn medical literature there are few statistics on complications of surgery ATM, with descriptions ranging from 17 to 25%.10,11
The TMJ has a close relationship with the lateral skull base and structures in this area. The middle ear and its ossicles, the inner ear and its sensorineural components, the facial nerve and the carotid artery in its intratemporal pathway are among the most important elements at risk in the surgical procedures performed in the TMJ. The anatomical knowledge has demonstrated the close embryological, anatomical and functional relationship between the TMJ and the middle ear.4 The TMJ superior stratum is attached posteriorly to the cartilaginous auditory meatus, the parotid gland fascia and the bony auditory meatus with anatomical variations.12,13 In addition, the superior attachment of the capsule is bounded to the temporal bone. The posterior part of the middle fossa formed by the squamous portion of the temporal bone and which forms the upper surface of the TMJ and the posterior surface of the mandibular condyle rests against the tympanic part of the temporal bone.14
In the medical literature, extratemporal-bone complications are reported in the TMJ surgery such as cervicomediastinal abscess,15 pneumomediastinum,16 subcutaneous emphysema and parotid fistula.17 Among the greatest potential risks of this procedure, complications of vascular lesions in the superficial temporal, internal maxillary and middle meningeal arteries may be serious or even fatal.9,18
The use of hemiarthroplasty by substitution of one articular surface is not a good choice for handling temporomandibular ankylosis.19,20 Several studies have shown that it can cause erosion of the fossa as a complication in these cases.19,21
It is increasingly accepted that the best treatment for ankylosis joint replacement with a prosthetic total, with both components, branch and fossa. However, this is an issue still under discussion and still there is no evidence to indicate what is the best option.
A variety of techniques have been cited in the literature for the treatment of this pathology, such as simple arthroplasty,22 interposition and joint reconstruction with alloplastic or autogenous materials.23,24 The variety of techniques used throughout the years, show how difficult it has been to find a satisfactory method for the reconstruction of the TMJ.
Most reports in the literature show isolated cases and reports with few cases. Usually the type of surgery and materials used vary from country to country, however, we can say that the purpose is always the same: (1) A successful resection of the ossified segment, (2) Use of an interpositional spacer, when required, (3) Physiotherapy and early postoperative intensive.25
Even less invasive, interventions such as TMJ arthroscopy may cause ear involvement. However, although similar complications have been described, circumstances with cerebrospinal fluid leak, facial paralysis and profound hearing loss were not found in the literature. Extensive lesions secondary to surgery in this case suggest an anatomical dissection performed without references.
After reduction surgery for condylar fracture, Lim reported the presence of a Kirschner wire in the middle fossa.8 By proximity, it is not uncommon intracranial penetration of the mandibular condyle after impact of trauma. Considering these anatomical relationships, in the presence of ankylosis, careful dissection and use of drill are necessary because the limits of the dura mater and cerebral content are not evident.
According to Yu,26 the use of computer-assisted navigation guidance allows safe excision of extensive new bone formation within the complex anatomy of the skull base, distorted by the disease, in cases of TMJ ankylosis. A navigation-guided resection of the ankylosed bone is recommended in these types of surgeries to reduce potential risks of the procedure.26
Aesthetic, functional and psychological repercussions of facial palsy can be as much as disabling, even more than those caused by ankylosis. In this procedure, the risk of damage of the extratemporal portion of the facial nerve is higher than the portions in the Fallopian canal, which has a constant location and easier identification. In extreme situations, as a proper preventive action, we recommend identifying the course of the facial nerve in the middle ear to the parotid.
Sensorineural hearing loss evidenced as a result of destruction of the basal cochlear turn completes the catastrophic outcome in this procedure. In our opinion, there is no justification for injuries of the otic capsule like this. Deep and comprehensive knowledge of these structures, surgical approaches, physiology and pathology are necessary to obtain satisfactory treatment results,27 and all clinicians of the various specialties involved in the care of these patients should be aware of this acute condition.
The reconstruction of the TMJ, which remains a major challenge in head and neck surgery, may be performed using a great variety of techniques with autogenous or alloplastic materials. According to Ebrahimi,28 there is no gold standard set for this surgery, and the results of ramus-condyle reconstruction with distraction osteogenesis suggest that this could become a standard technique in selected patients. Although results show less predictable, the costochondral grafting is the method of choice in children.29
The functional result and the reduction of pain in patients with TMJ ankylosis treated using total prosthetic or gap arthroplasty would be similar, according to Loveless.30 The good functional results provided by prosthetic reconstructions reflect the advances made in materials and surgical techniques.
Although the use of reconstruction plates with isolated metallic condyle in the glenoid fossa with natural disc has demonstrated stability in TMJ destructions caused by tumors or trauma,31 it is recommended the use of a total prosthesis (glenoid fossa and condyle) for alloplastic TMJ reconstruction, in cases of ankylosis, as well as in patients with advanced degenerative diseases, post-traumatic condylar destruction or multiple surgeries.32
The lack of studies comparing long-term functional results of various types of prosthesis available determines the choice of system to be used for personal experience of each surgeon.33
ConclusionThe craniomaxillofacial surgeon and other professionals who carry out interventions of this nature should have perfect knowledge of the anatomy of the temporal bone and lateral skull base, taking into account the risk of committing surgical disasters like the one here reported.
FundingAn unfunded project.
Conflict of interestThe author(s) declare that they have no conflict of interest.
We would like to thank the patient who allowed us to publish this case, and the Otolaryngology (ORL) staff for all their help and support.