Prevertebral calcific tendinitis is an uncommon cause of acute neck pain characterised by the identification of calcifications at C1–C2 level and the presence of a liquid collection at the prevertebral space which causes the displacement of the prevertebral radiographic line in imaging studies. It is very important to identify this rare, benign and self-limiting pathology, in order not to confuse it with other diseases that could erroneously lead to inappropriate treatment.
La tendinitis calcificante prevertebral es una causa poco frecuente de cervicalgia aguda, caracterizada por la identificación de calcificaciones a nivel de C1-C2 y, la presencia de una colección líquida en el espacio prevertebral, que ocasiona un desplazamiento de la línea radiográfica prevertebral en los estudios de imagen. Resulta de gran importancia identificar esta rara entidad, benigna y autolimitada, y no confundirla con otros procesos que erróneamente propiciasen actitudes terapéuticas inadecuadas.
Prevertebral calcific tendinitis, also known as retropharyngeal calcifying tendinitis or longus colli muscle tendinitis, is an uncommon and underdiagnosed cause of acute cervical pain. This rare condition is characterised by the presence of amorphous calcifications at the C1–C2 level and the presence of fluid collection in the retropharyngeal space, causing neck pain and odynophagia. The differential diagnosis should include retropharyngeal abscesses, infectious spondylitis and traumatic lesions. Knowledge of the clinical and radiographic findings of this benign and self-limiting condition is of great importance in order to avoid diagnostic errors which could lead to erroneous therapeutic, medical and surgical approaches.1
Case reportWe present the case of a 48-year-old female patient, who attended the ER due to neck pain of approximately 15 days duration, with progressive worsening in the last 2 days and odynophagia upon swallowing both solids and liquids. The patient reported no previous trauma or known trigger, presented no fever and no upper respiratory tract infections, either concurrent with or prior to this process. She had consulted at the ER 2 days before due to neck pain which did not improve with the anti-inflammatory treatment prescribed.
Upon examination, the patient presented a very limited range of cervical motion, especially in extension, with pain upon left paratracheal palpation which increased with swallowing and contraction of the cervical paravertebral musculature. No lymphadenopathy was detected upon palpation and the oropharyngeal examination was completely normal.
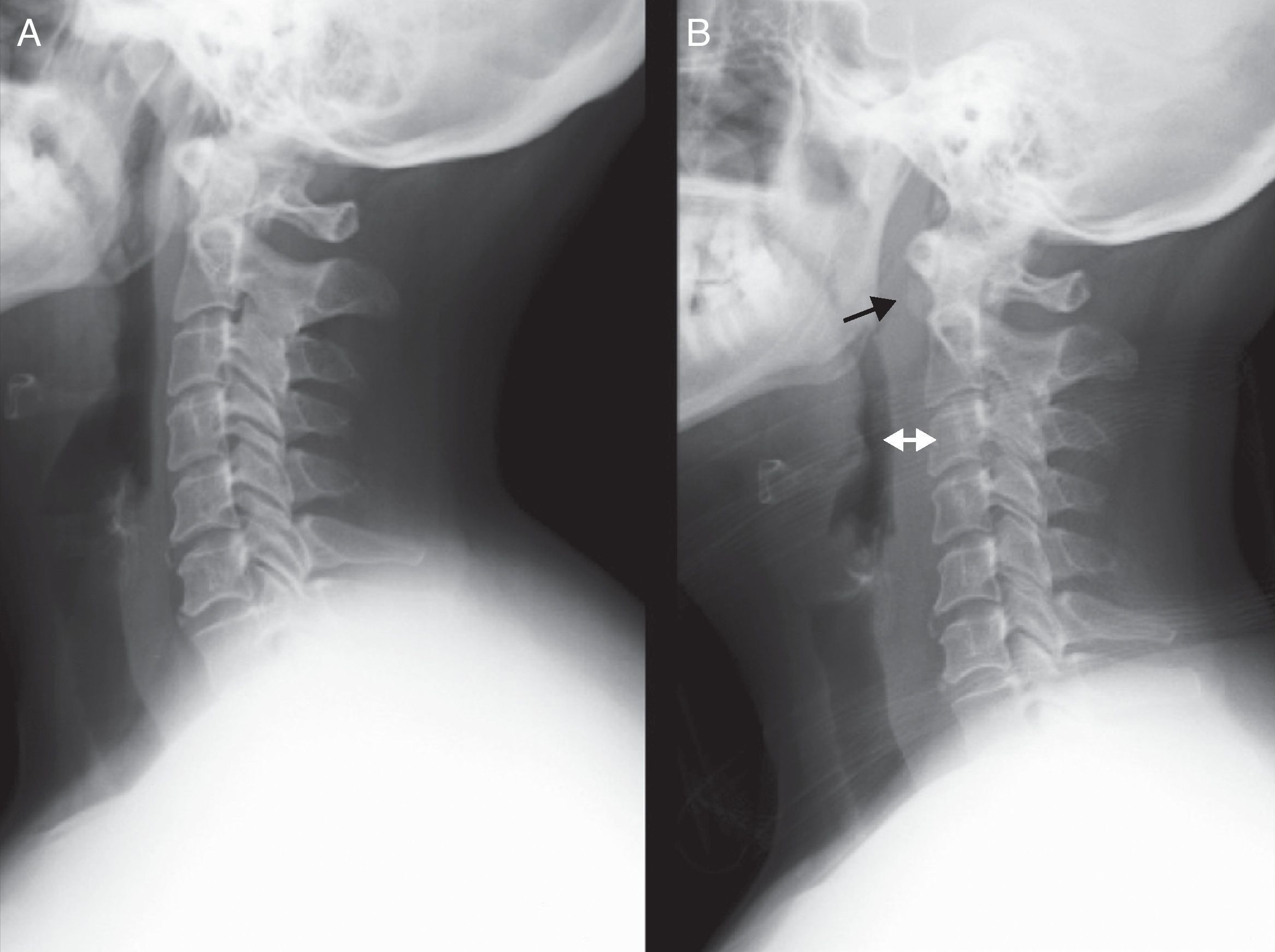
After performing a lateral cervical radiograph and comparing it with the study performed 2 days earlier at the ER, we observed a correction of cervical lordosis associated to a marked increase of the prevertebral space. We also observed calcification in the anterior C1–C2 region and anterior osteophytosis at the C5 and C6 levels (Fig. 1).
(A) Lateral radiographic projection showing a normal prevertebral space (about 7mm at the C3 level and 3cm at the C7 level). (B) Anterior displacement of the airway due to a marked increase of the prevertebral space, mainly from C1 to C4. A radiodense image can be seen at the C1–C2 level. The time interval between both radiographs was 2 days.
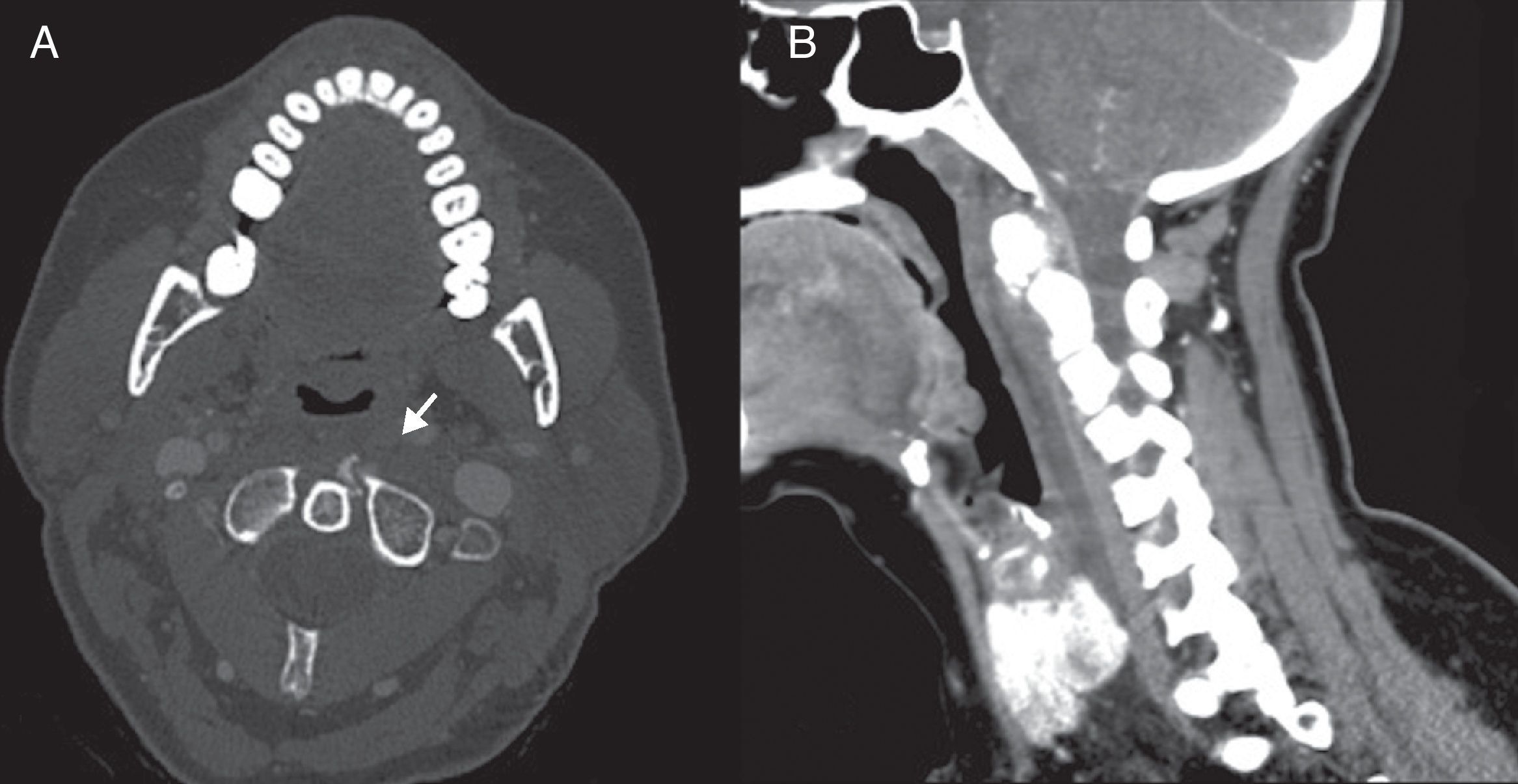
We requested an urgent computed tomography (CT) study which revealed an increased prevertebral space in relation to a fusiform, hypodense, homogeneous liquid collection, measuring 5mm×40mm×100mm and extending from the anterior arch of the atlas to the C6 vertebral body. The absence of gas and enhancement in the walls of the collection oriented against an abscess, whilst a coarse calcification of about 7mm, anterior and discreetly lateralised towards the left at the base of the odontoid process, provided diagnostic confirmation of prevertebral calcific tendinitis (Fig. 2).
(A) Axial CT section showing calcification in a ventral location to the odontoid process and lateralised towards the left. (B) Sagittal CT reconstruction with contrast in soft tissue window which shows fluid collection in the prevertebral and retropharyngeal spaces. The absence of peripheral enhancement and adaptation to the space occupied are radiographic findings that help to differentiate it from an abscess.
Since the patient presented disabling symptoms, she was admitted for intravenous corticosteroid therapy for 3 days, followed by oral corticosteroid therapy at home for a further 7 days. This treatment completely resolved the process and the calcification disappeared from the radiographs.
DiscussionThe prevertebral space is the anterior cervical space delimited ventrally by the deep cervical fascia, which separate it from the retropharyngeal space, and also by the spine, extending from the base of the skull to the mediastinum. This space contains the prevertebral muscles (longus colli, longus capitis, anterior rectus capitis and rectus) as well as the vertebral vessels, scalene muscles, phrenic nerve and part of the brachial plexus. The most important prevertebral muscle, the longus colli, is the neck rotator and flexor, and consists of 3 fascicles: superior oblique, vertical and inferior oblique. The superior oblique fibres originate from the anterior tubercles of the C3–C5 transverse processes and become inserted by a tendon into the anterior tubercle of the ventral arch of the atlas. The vertical fibres emerge from the C5–T7 vertebral bodies and become inserted into the C2–C4 bodies. The inferior oblique fibres originate from the T1–T3 bodies and become inserted into the anterior tubercles of the C5–C6 transverse processes.1
Calcific prevertebral tendinitis was first described by Hartley2 in 1964. Little is known about the aetiopathogenesis of this entity, although in a series of pathological studies conducted in 1994, Ring et al.3 demonstrated the deposition of calcium hydroxyapatite crystals in the longus colli muscle. Therefore, it has been hypothesised that repeated trauma, tissue necrosis phenomena and ischemia may all play a role in the deposition of these crystals, as is the case in other calcific tendinopathies in other locations.4 The breakage of these hydroxyapatite crystals would cause a painful, inflammatory response to foreign bodies in the longus colli muscle, leading to the formation of reactive fluid in the prevertebral space enveloping the muscle.5
Although it has been described as retropharyngeal tendinitis, a more accurate name would be prevertebral tendinitis or longus colli myositis, since it is the swelling of this muscle that causes the radiographic changes observable between C1 and C4.6
Although this condition is rare, its true incidence is probably higher, given that it often goes undiagnosed due to unawareness of many physicians, misinterpretation and confusion with other entities. The increasing accessibility of CT by emergency services will probably enable more new cases to be documented. From an epidemiological standpoint, it primarily affects patients aged between 30 and 60 years and is more frequent among women.
Patients usually present symptoms of acute cervical pain associated with reflex muscle contraction, decreased cervical range of motion, especially extension, and varying degrees of odynophagia and dysphagia.7 Dyspnoea is not usually present. Patients may also refer previous trivial trauma or recent upper respiratory tract infection, which can confuse the diagnosis, but a lack of trigger factors is very common.8 Patients may present fever, as well as discreet alteration of the leukocyte count and erythrocyte sedimentation rate. All these signs may erroneously guide towards retropharyngeal infection.1 However, in the latter entity, patients usually present a poorer condition with marked fever and clear alterations in their leukocyte count and acute phase reactants.
A thorough clinical history and examination are essential in order to identify this condition, as some subtle clinical findings may orient the differential diagnosis. Thus, cervical sprains, contracture and pain are greater in the paravertebral muscles of the neck radiating towards the shoulders, occiput and interscapular region, whilst pain in prevertebral tendinitis mainly appears in the anterior cervical region, usually lateralised, and with a scarce contraction component of the posterior paravertebral musculature, without radiation. As in acute cervical discopathy, pain increases with movement, which is very limited. However, whilst discopathy symptoms worsen with head flexion, pain in prevertebral tendinitis increases with extension and improves with neck flexion. Patients may present some degree of analgesic torticollis to relax the longus colli muscle.
Oropharyngeal inspection is normal in these patients, unlike in pharyngotonsillar infections which show hyperaemic changes and swelling of the tonsillar pillars or pultaceous plates. Odynophagia referred by these patients is typically lateralised and not linked to the midline of the anterior cervical region, as it would be in true oropharyngeal processes.
In terms of radiography, a characteristic sign is the presence of amorphous calcifications in the superior insertion of the longus colli muscle tendon at the C1–C2 level in the lateral projection of the cervical spine, as well as a variable increase in prevertebral soft tissues, typically from C1 to C4, although it may extend inferiorly up to C6, with anterior displacement of the airway. The radiographic identification of these deposits may not be evident. Small degrees of rotation or overlapping anatomical structures such as the earlobe or calcification of the stylohyoid ligament may be misleading. Therefore, good penetration and correct radiographic alignment are essential to locate these calcifications.1
The literature also contains reports of the same symptoms due to calcification deposition anterior to C5–C6, related to the origin of fibres of the vertical portion of the longus colli muscle.9
It can be difficult to differentiate lymphadenitis with abscessification from calcific tendinitis based only on clinical history and laboratory findings, because both can include fever, odynophagia, abnormal leukocyte count and acute phase reactants. Thus, CT is the key test to differentiate both entities.9 Identifying them correctly is essential since their treatment is radically different. Whilst retropharyngeal abscesses require surgical drainage and antibiotics, calcific tendinitis responds favourably to conservative treatment with anti-inflammatory drugs.
There are certain features in a CT scan which enable us to differentiate this entity from other conditions: (1) the fluid gently expands the retropharyngeal space in all directions; (2) absence of wall enhancement around the fluid, which would appear in the case of a retropharyngeal abscess; (3) absence of lymphadenopathy, and (4) pathognomonic tendinous calcifications in the longus colli muscle.10
Magnetic resonance imaging (MRI) is not as useful as CT because it does not reveal calcifications as reliably. In addition, it is not usually accessible by emergency services. However, an MRI scan would show an increased T2 signal corresponding to oedema in the retropharyngeal space and may also, sometimes, show bone oedema in the adjacent vertebrae.10
Prevertebral tendinitis generally responds favourably to non-steroidal anti-inflammatory drugs and cervical immobilisation, as well as a soft or crushed diet in cases of associated dysphagia. In severe cases, intravenous corticosteroid therapy provides rapid clinical improvement. It is usually resolved completely in the course of 1 or 2 weeks.
Since the condition is benign and self-limited, it is not usually unnecessary to conduct prolonged follow-up of patients. Lateral radiographs showing the resolution of the calcification, which usually disappears during the symptomatic phase, are often sufficient.
Ethical responsibilitiesProtection of people and animalsThe authors declare that this investigation did not require experiments on humans or animals.
Confidentiality of dataThe authors declare that they have followed the protocols of their workplace on the publication of patient data and that all patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consentThe authors declare having obtained written informed consent from patients and/or subjects referred to in the work. This document is held by the corresponding author.
Level of evidenceLevel of evidence IV.
Please cite this article as: Pellicer García V, et al. Tendinitis calcificante prevertebral aguda: a propósito de un caso y revisión de la literatura. Rev Esp Cir Ortop Traumatol. 2012;56;389–92.