Osteoporosis is a metabolic and systemic disease characterised by alterations at the level of bone tissue with loss of bone mineral density, changes in microarchitecture, mineralisation and remodelling that determine greater bone fragility and risk of fracture.
Falls in the elderly are a risk factor closely related to fragility fractures and numerous studies demonstrate this relationship.
Vertebral fractures are a major cause of morbidity and mortality. The epidemiology differs from osteoporotic fractures at other skeletal sites, as only one-third are clinically recognised. In the elderly, the approach to osteoporotic vertebral fracture involves comprehensive evaluation of the patient, since it is both a cause and a consequence of multiple geriatric syndromes. This fracture, in its acute phase and subsequently, can lead to destabilisation of other organs and systems of the elderly, medical complications at different levels, functional deterioration, dependence, and even the need for institutionalisation.
Therefore, it is important to carry out a multiple assessment of patients with vertebral fractures, addressing not only the history and risk factors of osteoporosis, but also those factors that lead to falls, as well as a comprehensive geriatric assessment and the complications closely associated with it.
In this chapter we address each of these aspects that are necessary in the individual and multidimensional approach to the elderly patient with vertebral fracture due to bone fragility.
La osteoporosis es una enfermedad metabólica y sistémica caracterizada por alteraciones a nivel del tejido óseo con pérdida de densidad mineral ósea, cambios en la microarquitectura, mineralización y remodelado que determinan una mayor fragilidad del hueso y riesgo de fractura.
Las caídas en el adulto mayor son un factor de riesgo estrechamente relacionado con las fracturas por fragilidad, y numerosos estudios demuestran esta relación.
Las fracturas vertebrales son causa de morbimortalidad importante. En el adulto mayor, el abordaje de la fractura vertebral osteoporótica implica una evaluación integral del paciente, ya que es tanto causa como consecuencia de múltiples síndromes geriátricos. Esta fractura, en su fase aguda y posteriormente, puede suponer la desestabilización de otros órganos y sistemas del anciano, complicaciones médicas a distintos niveles, deterioro funcional, dependencia e incluso necesidad de institucionalización.
Es, por tanto, importante una valoración múltiple del paciente con fractura vertebral, abordando no solo los antecedentes y los factores de riesgo de osteoporosis, sino también aquellos factores condicionantes de caídas, además de una valoración geriátrica integral y de las complicaciones íntimamente asociadas a la misma.
Osteoporosis is a metabolic and systemic disease characterised by alterations at the level of bone tissue with loss of bone mineral density, changes in microarchitecture, mineralisation, and remodelling that lead to increased bone fragility and risk of fracture. However, osteoporosis is a silent disease, without clinical manifestation until fractures occur, at which point it has an enormous impact, especially in the elderly, as it causes pain, functional deterioration, disability, and dependence, and secondarily, loss of quality of life, risk of institutionalisation, and economic costs.1,2 A good example of this duality, due to its incidence, is vertebral fracture, a major complication of osteoporosis because it is an indicator of future risk of new fractures and associated negative consequences.
Falls in the elderly are a risk factor closely related to fragility fractures and numerous studies demonstrate this relationship.3,4
Therefore, multiple evaluation of the patient with vertebral fracture is necessary. Not only history and risk factors for osteoporosis need to be addressed, but also risk factors for falls, making a comprehensive geriatric assessment and assessing closely associated complications. In this chapter we address each of these aspects which are necessary for an individual and multidimensional approach to the elderly patient with a vertebral fracture due to bone fragility.
Evaluation of the risk factors for osteoporosis. Personal history and risk factors for osteoporosisThe prevalence of osteoporosis in women aged 60–69 years is estimated at around 22% and increases to 70% in those over 80 years of age. In addition, 70% of all fractures occur in women, although some studies have found a male to female ratio of 1:1 in vertebral factors.5 The prevalence of vertebral fracture varies according to age and geographical area, but it is estimated to reach 50% in the geriatric population6 and therefore osteoporosis is linked to the ageing process, with a strong relationship with the female sex.
Furthermore, in the natural history of the disease we see progressive occurrence of radius fractures at around 55–65 years of age, vertebral fractures with a peak incidence at 75–85 years of age, and later hip fractures in those over 80 years of age.7 This also corresponds to greater involvement of trabecular bone in the perimenopausal age, determined by hormonal changes, and the involvement of cortical and trabecular bone in the older adult, with less influence of hormonal changes, and where vitamin D deficit and secondary hyperparathyroidism play a more relevant role in the pathogenesis.
As we mention above, female sex and advanced age are intrinsic and non-modifiable risk factors for fractures, as is having had previous fractures. A woman with a vertebral fracture has double the risk of hip fracture and a 4-fold risk of suffering a new vertebral fracture; furthermore, 19% will present a new vertebral fracture in the following year.8,9
Older women, who are underweight, smokers, diabetics, or with low adherence to osteoporosis treatment are most at risk of refracture.10
Also, the presence of indirect indicators of vertebral fracture, such as kyphosis, loss of height of more than 2cm or a distance between hip and rib of 2cm or less, alert us to previous non-symptomatic fractures, which some studies warn may be up to 70% of all vertebral fractures.11
There is increasing evidence of the close relationship between bone and muscle, such that they function as a muscle-bone unit, and this has led to growing interest in entities such as sarcopenia and osteosarcopenia. Sarcopenia is a process in which there is a loss of muscle strength associated with changes in muscle quantity and quality, and osteosarcopenia is a confluence of both pathologies. An increase in serum markers of inflammatory activity such as interleukin 6 or tumour necrosis factor-α has been described in patients with osteoporosis and sarcopenia, which indicates damage at local and systemic level, determining an exponentially greater risk of bone fracture.12,13 The prevalence of osteosarcopenia is highly variable according to the studies, at between 5% and 37%, and more frequent in women.14
Both sarcopenia and osteosarcopenia have a close relationship with frailty, given that muscle plays a relevant role in the physiopathology of frailty and is therefore a key point in its intervention. For the same reason, sarcopenia and malnutrition are closely related and therefore malnutrition, low weight, sarcopenia, and frailty play a negative role in the development of osteoporosis and risk of fracture in the elderly.15,16
Low physical activity, sedentary lifestyle, or immobility are other factors influencing frailty, sarcopenia, and osteoporosis, and also mechanisms involved in the loss of muscle mass.
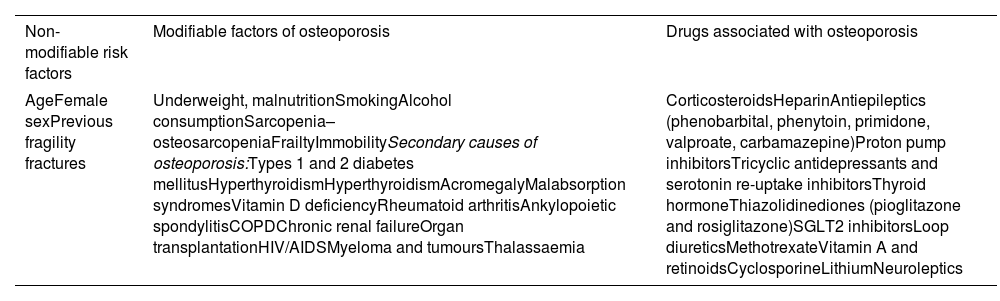
Many chronic diseases or pathologies increase the risk of osteoporosis and fracture, and are the cause of secondary osteoporosis. Of these diseases, the relationship between diabetes and osteoporosis or osteopenia and fracture is noteworthy,17 both diabetes type 1 and type 2. Metformin appears to have an osteogenic effect, reducing the risk of fracture, while sulphonylureas, SGLT2 inhibitors, or thiazolidinediones (pioglitazone and rosiglitazone) have been found to increase the risk for fracture.18 GLP-1 agonists and DPP4 inhibitors appear to have an anabolic effect on bone and the relationship with insulin is unclear as there are studies for and against any relationship.19
Other endocrine diseases associated with osteoporosis include hyperthyroidism, acromegaly, and hyperparathyroidism. Calcium or vitamin D deficiency, malabsorptive disorders, alcohol consumption, and smoking are also associated with osteoporosis. Chronic kidney disease and transplant patients are also at increased risk of fracture.
Autoimmune diseases such as ankylopoietic spondylitis, rheumatoid arthritis, and chronic pulmonary disease (COPD) also have a higher risk of bone fracture, as well as other chronic processes listed in Table 1.
Risk factors for osteoporosis.
| Non-modifiable risk factors | Modifiable factors of osteoporosis | Drugs associated with osteoporosis |
|---|---|---|
| AgeFemale sexPrevious fragility fractures | Underweight, malnutritionSmokingAlcohol consumptionSarcopenia–osteosarcopeniaFrailtyImmobilitySecondary causes of osteoporosis:Types 1 and 2 diabetes mellitusHyperthyroidismHyperthyroidismAcromegalyMalabsorption syndromesVitamin D deficiencyRheumatoid arthritisAnkylopoietic spondylitisCOPDChronic renal failureOrgan transplantationHIV/AIDSMyeloma and tumoursThalassaemia | CorticosteroidsHeparinAntiepileptics (phenobarbital, phenytoin, primidone, valproate, carbamazepine)Proton pump inhibitorsTricyclic antidepressants and serotonin re-uptake inhibitorsThyroid hormoneThiazolidinediones (pioglitazone and rosiglitazone)SGLT2 inhibitorsLoop diureticsMethotrexateVitamin A and retinoidsCyclosporineLithiumNeuroleptics |
Another essential aspect in assessing risk for fracture is the pharmacological review, given that numerous drugs are associated with a greater risk of osteoporosis, particularly anticonvulsants (phenobarbital, phenytoin, primidone, valproate, carbamazepine) which interfere with vitamin D metabolism. Other drugs, widely used in the elderly population, such as proton pump inhibitors or serotonin reuptake inhibitors, thyroid hormone, or heparin, also affect bone metabolism. Some authors have found a relationship between neuroleptics, sedatives, and lithium, although it seems that the effect is low and could be conditioned by the higher risk for falls that they entail.20
Corticosteroids have a direct and indirect effect on bone remodelling; on the one hand, they contribute to the development of sarcopenia with an effect on muscle tissue; on the other, they reduce sex hormones, which has an impact on bone and muscle. And finally, they have a direct effect on bone tissue by increasing osteoclastogenesis and reducing osteoblastogenesis and increasing bone apoptosis. Studies show that in those subjects receiving>7.5mg of prednisone daily on a chronic basis for more than 6 months, the risk of fracture increases by 15–20%.
Hormone deprivation therapy, aromatase inhibitors, and other drugs associated with risk of bone fracture are also shown in Table 1.
On the other hand, the discontinuation of previous treatment with denosumab has been seen to accelerate bone turnover and rapidly increase the risk of new vertebral fractures in the 6–18 months after last administration of the drug, especially in women with previous vertebral fractures.21,22
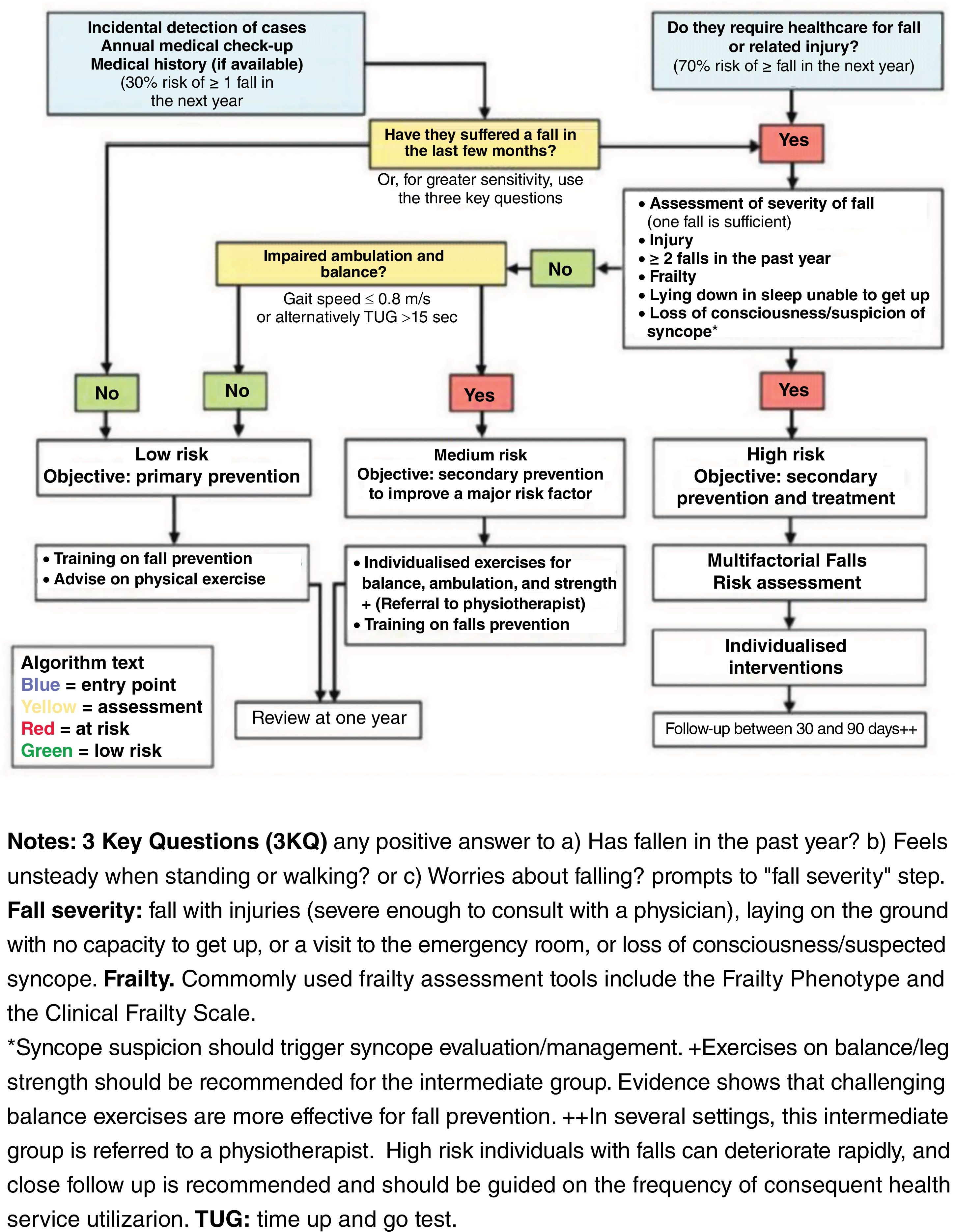
Assessment of risk factors for falls as a causal mechanism for vertebral fractureAlthough vertebral fractures are not systematically associated with a fall or trauma, and on many occasions are a chance finding in the examination of a patient presenting for another reason, falls are intimately associated with fractures in the elderly3,5 and we should always evaluate them in patients with vertebral fractures.
One third of older people living in the community and half of those living in nursing homes suffer falls each year, and a high percentage of these falls will occur repeatedly, increasing the risk of complications.23
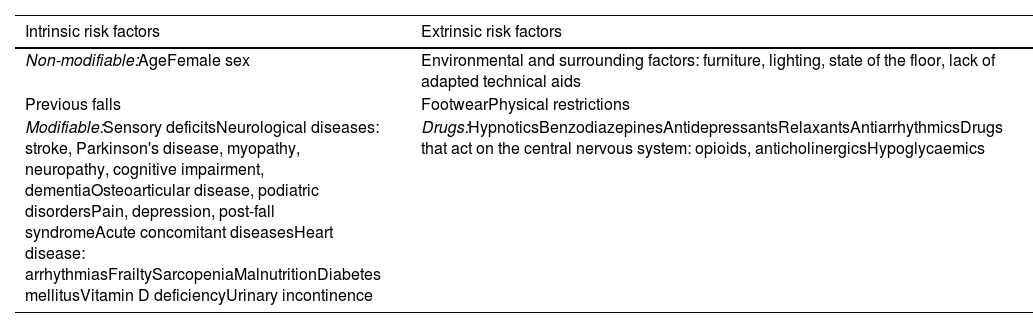
Falls are the result of a complex interaction between circumstances external to the individual (extrinsic factors) and internal factors or circumstances related to diseases and processes that determine this risk (intrinsic factors), which are listed in Table 2.
Risk factors for falls.
| Intrinsic risk factors | Extrinsic risk factors |
|---|---|
| Non-modifiable:AgeFemale sex | Environmental and surrounding factors: furniture, lighting, state of the floor, lack of adapted technical aids |
| Previous falls | FootwearPhysical restrictions |
| Modifiable:Sensory deficitsNeurological diseases: stroke, Parkinson's disease, myopathy, neuropathy, cognitive impairment, dementiaOsteoarticular disease, podiatric disordersPain, depression, post-fall syndromeAcute concomitant diseasesHeart disease: arrhythmiasFrailtySarcopeniaMalnutritionDiabetes mellitusVitamin D deficiencyUrinary incontinence | Drugs:HypnoticsBenzodiazepinesAntidepressantsRelaxantsAntiarrhythmicsDrugs that act on the central nervous system: opioids, anticholinergicsHypoglycaemics |
Generally, there will not be one single triggering factor, but multiple risk factors, which also offers us the opportunity to make multiple interventions.
Among the intrinsic risk factors, it is important to recognise all those diseases that interfere with balance and gait: sensory deficits, both visual and auditory, neurological pathology (dementia, Parkinson's disease, cerebral vascular disease, neuropathies, and myopathies),24 vestibular pathology, osteoarticular pathology of the lower limbs and podiatric disorders, and cardiovascular pathology such as arrhythmias and orthostatic hypotension.25,26 Disorders that reduce our functional reserve, such as frailty, sarcopenia, and malnutrition, and the diseases that favour them, such as diabetes, also increase the risk of falls and the need for technical aids, or functional deterioration in basic activities, all of which are indicative of this low functional reserve and risk for falls.27–30
Other problems associated with falls are depression, poor pain control, and post-fall syndrome, characterised by stress and fear of falling, which leads to functional impairment and increased risk of falls, and which occurs after having suffered a fall.31,32 There are also intrinsic factors that cannot be modified, such as age; falls are more frequent in the elderly, with a 4-fold increase in the risk in those over 85 years.33 Some authors also find a higher risk of falls among women and especially of falls with complications. One of the most important factors to consider when assessing the risk for falls is having had previous falls; specifically, patients with 2 or more falls in the last year are considered to be at high risk.33,34
An exhaustive pharmacological review is also essential in the assessment of falls, as many pharmacological groups are related to falls. The group of psychotropic drugs and especially benzodiazepines, hypnotics, antidepressants, and anticonvulsants are associated with a higher risk of falls. Also, some drugs with cardiovascular effects (antihypertensives and antiarrhythmics such as beta-blockers or digoxin), those that increase the risk of delirium or acute confusional syndrome (such as opioids or drugs with anticholinergic effects), and anti-inflammatory and hypoglycaemic drugs. There is consensus on the need to review all pharmacological prescriptions in patients with falls, especially in those who are polymedicated, have poor treatment adherence, or high consumption of psychotropic drugs, and inappropriate prescriptions should be discontinued given this risk.35–37
Finally, it is essential to assess other circumstances extrinsic to the individual, but which increase the risk of falls, including type of footwear, furniture, lighting, the characteristics of the floor, or the lack of adapted technical aids in the bathroom or bedroom. In the case of residential homes or hospitals, it is important to assess these adaptations in common areas, stairs, bathrooms, and bedrooms, and evaluate the use or involvement of physical restraint in these falls, recommending that it should not be used in these settings.
Given the complexity and great variety of risk factors that interact in the vertebral fragility fracture patient, different tools have been designed to help us quantify the risk of fracture in the older adult based on the presence of the risk factors mentioned above. Tools such as Q-Fracture and Garvan have been specifically developed for use in the older population, unlike FRAX, and also consider whether they have suffered a fall, previous fractures, and their number when stratifying risk.38–40
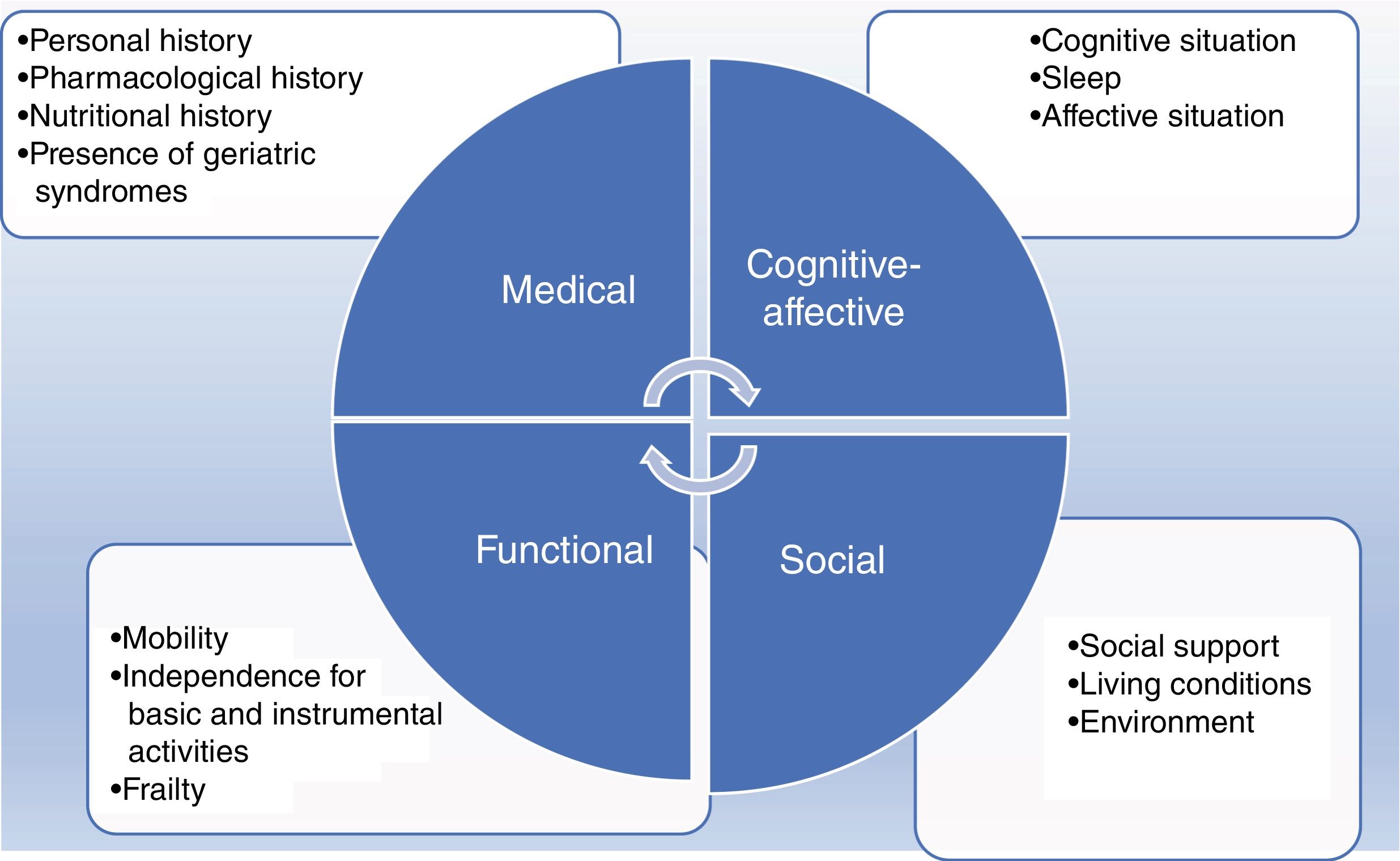
Comprehensive geriatric assessment as part of the approach to the elderly patient with vertebral fracture. Assessment of medical complicationsIn the older adult, the approach to osteoporotic vertebral fracture involves comprehensive assessment of the patient, because it is both a cause and consequence of multiple geriatric syndromes. This fracture, in its acute phase and later, can lead to destabilisation of other organs and systems in the elderly, medical complications at different levels, functional deterioration, dependence, and even the need for institutionalisation.41 Therefore, a comprehensive geriatric assessment is necessary, both to provide the most appropriate treatment for pain and potential medical complications in the acute phase and to select the most appropriate preventive pharmacological treatment for second osteoporotic fractures for each patient, in the context of specific recommendations for the prevention of falls.42,43
The appropriate approach to osteoporotic vertebral fracture is multidimensional and individualised treatment based on the mental, functional, and social situation of the patient prior to the fracture (Fig. 1).
Their previous capacity for ambulation, for carrying out basic self-care activities and independence for instrumental activities must be assessed, analysing the impact of the fracture on these areas.44 Pain and other complications of vertebral fracture can lead to immobilisation and dependence, which can be irreversible in some cases. Similarly, the selection of preventive treatment for new fractures should be based, among other factors, on the functional situation of the patient prior to the vertebral fracture, as this is a very important predictive factor for quality of life and life expectancy.
The presence of cognitive deterioration is a determinant of the risk of fracture-related confusional syndrome. Insomnia or the aggravation of behavioural disorders in the patient with dementia (for whom it is more difficult to manifest symptoms such as pain, difficulty in urination, or bowel movements) or loss of autonomy for ambulation is frequent. Similarly, the patient with cognitive impairment requires monitoring to ensure adherence to anti-osteoporotic treatment.
Similarly, it is essential to know the social environment of the patient, who often has a greater degree of dependence than before the fracture, to ensure adequate care at home or in a residential centre.
Osteoporotic vertebral fracture, being a sentinel disease of potential undetected clinical problems, and a high risk of deteriorated health status, makes a complete assessment of frailty recommendable, as a marker of risk of disease, hospitalisation, disability, and mortality. It is essential it is detected to implement specific diagnostic-therapeutic measures, and it is very relevant for estimating the type and efficacy of preventive treatment for new fractures.
The medical complications of osteoporotic vertebral fractures can manifest both in the acute phase and later. In the older adult, in addition to the characteristic girdle pain that can be very disabling, other complications are frequently observed.45,46 They should be assessed and treated early to minimise their consequences:
- •
Immobilisation, loss of muscle mass, and risk for pressure ulcers.
- •
Constipation and even paralytic ileus secondary to pain, drugs, and immobilisation.
- •
Increased risk of acute urinary retention and urinary tract infection related to pain, immobility, pharmacological side effects, and constipation.
- •
Insomnia, delirium, or aggravation of chronic behavioural disorders in cases of dementia, secondary to poor pain control.
- •
Respiratory complications, respiratory failure in relation to hypoventilation in immobilised patients. Shallow breathing and fear of coughing due to pain and adverse effect of analgesic medication on breathing may induce bronchial congestion and respiratory infection.
- •
Side effects of potent analgesic drugs that should be monitored, especially opioids and anti-inflammatory drugs.
- •
Risk of destabilisation of chronic cardiorespiratory disease.
- •
Hyporexia in relation to pain, constipation, side effects of analgesics.
- •
Thromboembolic complications, which should be anticipated by assessing the use of low molecular weight heparin.
- •
Electrolyte complications, requiring special monitoring of hyponatraemia secondary to SIAHD due to pain.
For all the above reasons, the older adult with an osteoporotic vertebral fracture should receive, on the one hand, treatment in the acute phase of pain and prevention of the abovementioned medical complications based on their comorbidity and, on the other, anti-osteoporotic treatment and fall prevention, tailored to their previous physical, mental, and social situation.42
Multidimensional approach to the older adult with vertebral fracture: acute fracture, subacute fracture, and incidental fractureVertebral fractures are a major cause of morbidity and mortality. The epidemiology of vertebral fractures differs from osteoporotic fractures in other skeletal sites, as only one third are recognised clinically (acute–subacute-symptomatic) and detected by appropriate imaging methodology, while another high percentage have asymptomatic or incidental vertebral fractures, which are not detected until a simple dorsolumbar spine X-ray is performed for another reason.
A vertebral fracture categorised as acute or chronic, benign, or malignant, osteoporotic, or secondary to another disease, leads the treating physician to different therapeutic strategies. It is essential to distinguish an osteoporotic vertebral fracture from a pathological vertebral fracture for correct diagnosis and therapeutic approach.
Vertebral fractures of secondary causes should be considered in:
- •
Young individuals, after low energy or spontaneous trauma. A secondary cause should be sought until proven otherwise, and should not be attributed to a decrease in bone mineral density, even when this is present.
- •
Coeliac disease, patients undergoing gastric bypass surgery, other pathologies such as myeloma, metastases, neoplasms, autoimmune diseases, deposit diseases such as Gaucher disease, rickets in children, or osteomalacia in adults should be considered on a case-by-case basis and should be ruled out frequently.
- •
Likewise, medication should be reviewed as explained above as a cause of secondary fracture and glucocorticoid use should always be looked for.
- •
Rheumatological diseases, as explained in another chapter, are also causes of secondary vertebral fractures, and screening should be conducted according to other clinical data associated with the patient.
- •
The fracture progression time indicates the relationship it may (or may not) have with the symptoms presented by a patient. The importance of imaging in this instance lies in defining an acute fracture or, in contrast, a chronic fracture.
- •
Asymptomatic, chronic, incidental fractures, with no associated clinical symptoms, require a study to rule out a possible secondary cause, in cases where this is suspected, and anti-osteoporotic treatment should also be considered.
Acute or subacute, symptomatic fractures are those carrying the most medical complications, some of which have already been mentioned above, and require a multidimensional approach at the acute stage, as they are frequently associated with pain and functional deterioration, with the complications that this entails for the elderly patient. Symptom control often requires the use of orthoses, analgesics, initial rest, and subsequent rehabilitation, and considering surgical treatment.
In general, in the elderly patient with an acute-symptomatic or chronic-asymptomatic vertebral fracture, both preventive measures for new fractures and treatment to control medical complications should be instituted, and this includes the following multidimensional approach:
- •
Physical exercise, as a measure to prevent functional deterioration, and many of the subsequent complications. Pain control in symptomatic vertebral fractures should be awaited before starting. It also helps in the prevention of falls.47,48
- •
Nutrition, a balanced diet, rich in protein, should be ensured given that an insufficient protein intake has deleterious effects on both bone mass and muscle mass. A daily intake of 1g/kg body weight is recommended for healthy elderly people, and may vary in other circumstances (renal or hepatic disease, or more acute situations). A diet rich in calcium is also important.
- •
Vitamin D supplementation if daily sun exposure is not adequate.
- •
Avoid alcohol and smoking as a preventive measure.
- •
Assess risk of falls, the approach is explained in Fig. 2.34
- •
Systematic review of medication both as a preventive mechanism for vertebral fractures and falls, and once they have occurred. The STOPPfall tool is a proposal for this.49
- •
Adequate pain control, using opioids with care if necessary.
- •
Identify and treat hydroelectrolyte disturbances (hypo-hyperkalaemia, hypo-hypernatraemia) and water balance disturbances (both due to depletion and overload) in the preoperative and postoperative periods to avoid greater morbidity and mortality. It is also important to detect anaemia, and to monitor haemoglobin levels and treat where necessary to optimise the patient.
- •
Preventive measures for delirium, and how to deal with it once it appears. Given that it is a secondary organic condition, it is important to assess all possible triggers so as to control it therapeutically (pain, constipation, medication, hydration, nutrition, etc.).50
- •
Avoid constipation, using laxatives preventively if necessary to avoid complications. In the elderly patient, it is advisable to combine them when opioids are started.
It should not be forgotten in the overall approach, to assess the need for specific drugs for osteoporosis: antiresorptives or osteoformers, as explained in another chapter.
In summary, vertebral fractures require multidisciplinary and multidimensional management in the same way as hip fractures, although there are currently no well-defined models.51 It is equally necessary to manage the complexity they involve in clinical practice, especially in the elderly patient, and to recognise the benefits of a comprehensive approach, along with creating clinical pathways and care maps that apply the recommendations of clinical practice guidelines.
Level of evidenceLevel of evidence i.
Ethical considerationsThere are no ethical considerations to note.
FundingNo funding was received for this manuscript.
Conflict of interestsThe authors have no conflict of interests to declare.