To assess the radiological and functional outcome of arthrodesis of the 4th and 5th finger using the APEX™ (Extremity Medical, Parsippany, NJ) intermedullary interlocking screw system in patients with severe recurrence of Dupuytren's disease.
Materials and methodThe DASH questionnaire and the VAS scale were used to assess the clinical outcomes. The angle of arthrodesis, fusion time and implant fixation were evaluated on X-rays. The patients were monitored for complications during surgery and the follow-up period.
ResultsThe sample comprised 6 patients. Mean follow up was 19.6 months. All of the patients presented clinical and radiological evidence of fusion at 8 weeks, with fusion angles of 30° (3) and 45° (3). There were no complications and none of the implants had to be removed. The functional outcomes in these patients were poor.
ConclusionThe system offers a reliable method for IPJ arthrodesis at a precise angle. It promotes stable fixation that does not require prolonged immobilisation. It can be used together with other procedures on the hand with severe recurrence of DD. The functional outcomes for this group of patients using this device were poor.
Valorar el resultado radiológico y funcional de la artrodesis de la articulación IFP del 4.° o 5.° dedo de la mano mediante el sistema intramedular de tornillos entrelazados a compresión APEX™ (Extremity Medical, Parsippany, NJ) en pacientes afectos de recidiva grave de la enfermedad de Dupuytren.
Material y métodoLos resultados clínicos se valoraron mediante el cuestionario DASH y la escala EVA. En las radiografías se evaluó el ángulo de artrodesis, el tiempo de fusión ósea y la fijación del implante. Se observó cualquier complicación encontrada durante la cirugía o en el periodo de seguimiento.
ResultadosLa muestra estuvo representada por 6 pacientes. El seguimiento medio fue de 19,6 meses. Todos presentaron evidencia clínica y radiológica de fusión en 8 semanas, con un ángulo de fusión de 30° (3) y 45° (3). No se presentaron complicaciones y no se tuvo que retirar ningún implante. Los resultados funcionales en este tipo de pacientes fueron pobres.
ConclusiónEl sistema proporciona un método fiable para la artrodesis de la IFP en un ángulo preciso. Promueve una fijación estable que no requiere inmovilización prolongada. Puede usarse junto con otros procedimientos en la mano afecta por recidiva grave de ED. Los resultados funcionales con el uso de este dispositivo en este grupo de pacientes fueron pobres.
The relapse rate following surgery for Dupuytren's disease (DD) may stand at from 12% to 39% for fasciectomy, 50%–58% for needle fasciotomy and from 10% to 31% for Clostridium histolyticum colagenase injection.1 This relapse rate has been associated with bilateral involvement, family history, ectopic involvement and a young age.2 Although in the first surgical operation the metacarpo-phalangeal contracture is almost always corrected, it is very common for the correction to be lost at the level of the proximal interphalangeal joint (PIJ), and this may arise in up to 70% of cases.3
There are several options for the treatment of relapses in this disease. These include the use of local flaps, skin grafts, arthroplasty, osteotomy and arthrodesis, all of which are valid alternatives to avoid amputation of the affected finger. However, there is currently no agreement on which treatment is optimum in case of relapse.4 Arthrodesis of the proximal interphalangeal joint may create a stable joint in a functional position from the time surgery takes place.4
The aim of this study is to evaluate the radiological and functional results of arthrodesis of the PIJ of the 4th or 5th finger of the hand by means of the intramedullary system of interlocking APEX™ (Extremity Medical, Parsippany, NJ) screws under compression in patients with severe relapse of Dupuytren's disease.
Materials and methodA descriptive retrospective study was undertaken of a series of patients with the clinical diagnosis of severe relapse of Dupuytren's disease. They had been operated from 2013 to 2016 by arthrodesis of the PIJ using the compression interlocked system of APEX™ screws, with at least 6 months follow-up. All of the patients had been operated at least once using fasciectomy.
We define relapsing Dupuytren's disease as the situation in which at least 3 months after the last operation prior to arthrodesis (moment “0”), the patient has an increased deficit of passive extension of at least 20° in one of the operated joints, measured using a goniometer and with the presence of a palpable band of tissue.5
The severity of the relapse in the finger subjected to arthrodesis was quantified using Tubiana's system.6
Demographic data were recorded, together with clinical characteristics, family history of DD, the number of previous operations and the passive extension deficit of the finger before and after the last surgical operation prior to arthrodesis. In connection with the arthrodesis the indication for surgery was recorded, as well as the finger subjected to arthrodesis, any additional associated procedures and follow-up duration.
All of the patients were followed-up using posteroanterior, oblique and lateral X-rays of the finger at 4, 8 and 12 weeks, then at 6 months and one year. The consolidation time was evaluated together with the PIJ angle of fusion. An arthrodesis was considered to be consolidated when bridges in both ends of the bone were observed, as well as the absence of pain at the centre and few signs of inflammation.
The final clinical result of the operated hand was evaluated using the Disabilities of the Arm, Shoulder, and Hand-questionnaire (DASH)7 and the Analogue visual scale (AVS). The following questions were included to evaluate the degree of patient satisfaction: “Are you satisfied with the surgery?” and “Would you accept another operation?”. All surgery-associated complications were recorded.
Data analysis was performed using version 21.0 of the social sciences statistical package (SPSS), and in all cases the level of statistical significance was set at 95% (P<.05). Qualitative variables were expressed as numbers and percentages. Averages and standard deviation were used for quantitative variables. The Wilcoxon test was used to compare the quantitative results before and after surgery.
Surgical techniqueThe APEX™ implant is available in a range of sizes at two different angles, 30° and 45°. 30° implants were preferred for the 4th finger. In patients whose 5th finger was involved the decision to use one angle or the other was based on the mobility of the metacarpo-phalangeal (MP) joint at the time of surgery. In those cases where hyperextension of the MP was not possible, arthrodesis at 30° was preferred to achieve greater opening of the hand.
The procedure takes place under local anaesthesia and ischaemia of the limb by means of a pressure cuff on the arm. The time taken varies depending on the procedures, from 45min for PIJ arthrodesis of a single radius up to 135min for more complicated hands.
A dorsal longitudinal incision is made at the level of the PIJ. The central band of the extensor tendon, the joint capsule and the periostium are angled and reflected at the radial and ulnar, respectively. The collateral ligaments are freed from the condyles of the phalanx to crate flexion and completely expose the joint surfaces.
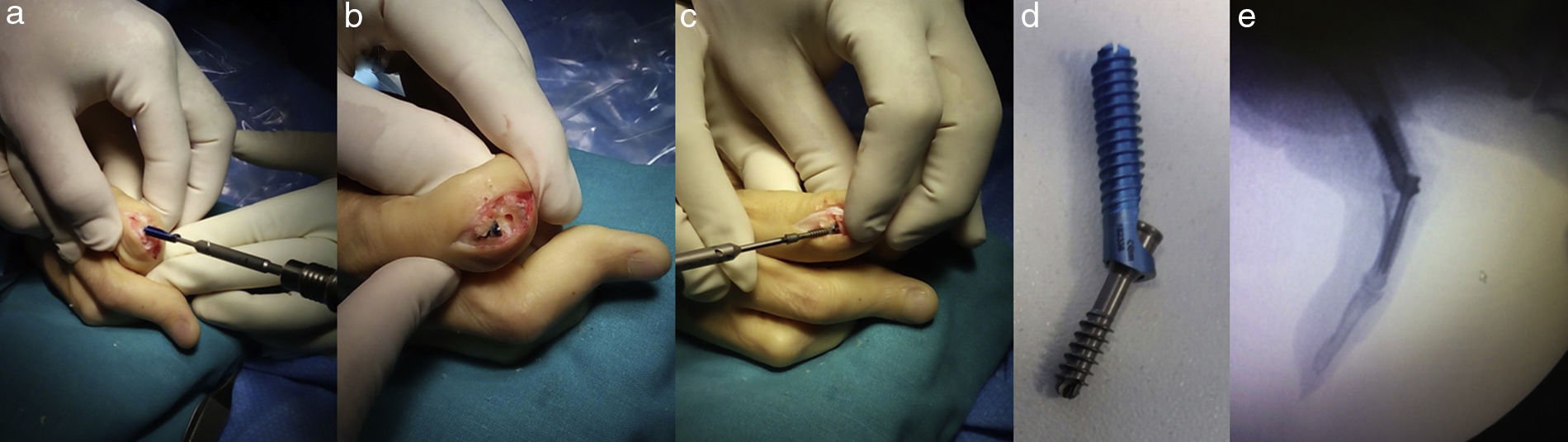
Guided by fluoroscopy a guide needle is inserted into the centre of the medullary canal of the proximal phalanx. A cannulated rasp is used to prepare the phalangeal canal. The (X-post™) implant is inserted into the proximal phalanx at the appropriate depth and rotation (Fig. 1a and b). A reamer and rasp are passed from the palm to the back of the hand through the implant, creating a dorsal hole in the neck of the proximal phalanx. The phalanx condyles are flattened, exposing spongy bone with a nominal angle of 30° or 45°.
A guide needle is then inserted into the centre of the base of the mid phalanx and a bit and reamer are used to open the medullary canal and expose spongy bone at the base of the phalanx. The length of the compression screw is determined using a cannulated rule and it is inserted through the dorsal window of the X-post™ and threaded into the mid phalanx, keeping the finger at the appropriate rotation (Fig. 1c and d). The coupling mechanism between the 2 components is a Morse cone (Fig. 1e). The capsule and extensor mechanism are closed sequentially using absorbable 4/0 sutures. At the end of the procedure a cushioned bandage is put into position without tension. Mobilisation of the hand commences immediately.
ResultsThe sample was composed of 6 men (100%) with an average age of 60 years old (range: 48–78). Three right hands and three left hands were operated. 83.33% of the patients had bilateral DD. No patient had associated ectopic diseases or first-degree family members affected by DD. All of the fingers subjected to arthrodesis had been operated on at least twice beforehand (range 2–3). The average duration of the follow-up was 19.6 months (range: 7–33 months).
100% of the patients had undergone an increase of the PIJ extension deficit that averaged 32.5° (range 20°–45°) after moment “0”. The severity of the relapse measured on Tubiana's scale was stage iv in 100% of the patients.
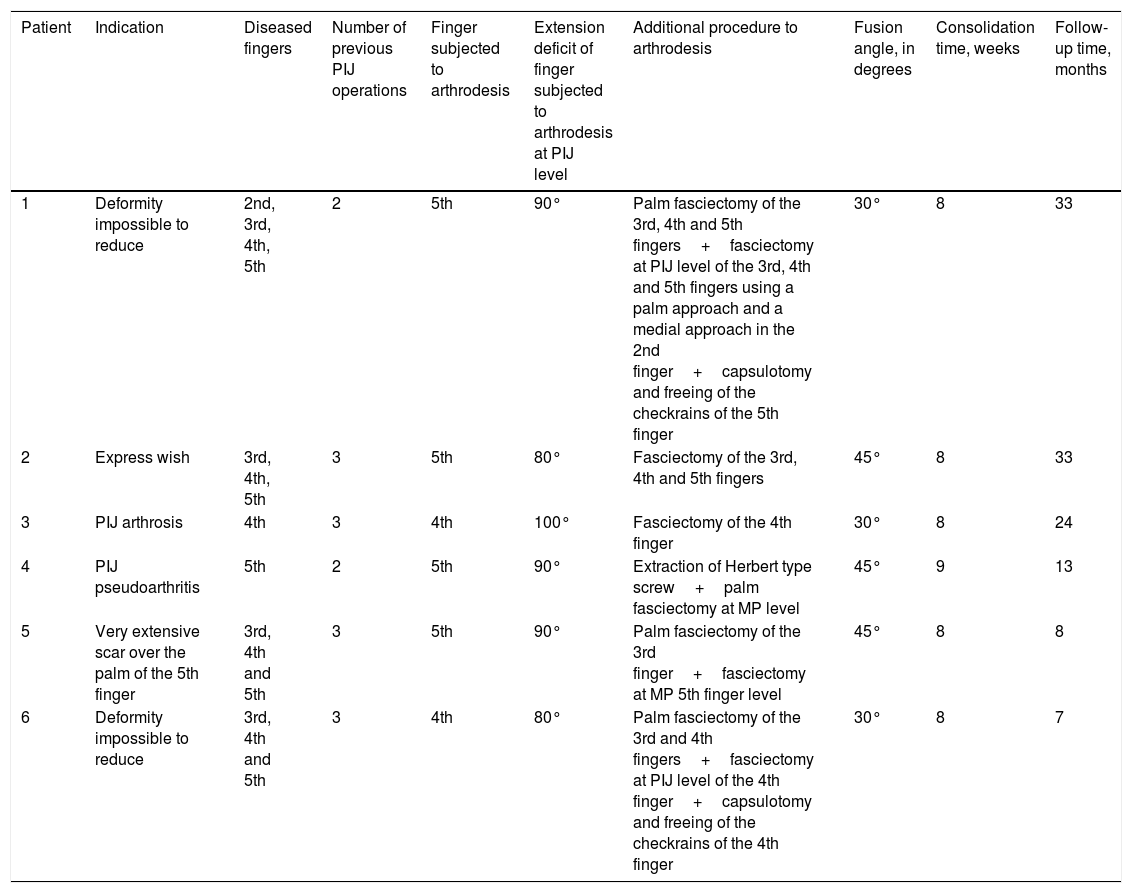
The indication for arthrodesis and the additional procedures performed are shown in Table 1.
Surgical indication, associated procedures and radiological results.
| Patient | Indication | Diseased fingers | Number of previous PIJ operations | Finger subjected to arthrodesis | Extension deficit of finger subjected to arthrodesis at PIJ level | Additional procedure to arthrodesis | Fusion angle, in degrees | Consolidation time, weeks | Follow-up time, months |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Deformity impossible to reduce | 2nd, 3rd, 4th, 5th | 2 | 5th | 90° | Palm fasciectomy of the 3rd, 4th and 5th fingers+fasciectomy at PIJ level of the 3rd, 4th and 5th fingers using a palm approach and a medial approach in the 2nd finger+capsulotomy and freeing of the checkrains of the 5th finger | 30° | 8 | 33 |
| 2 | Express wish | 3rd, 4th, 5th | 3 | 5th | 80° | Fasciectomy of the 3rd, 4th and 5th fingers | 45° | 8 | 33 |
| 3 | PIJ arthrosis | 4th | 3 | 4th | 100° | Fasciectomy of the 4th finger | 30° | 8 | 24 |
| 4 | PIJ pseudoarthritis | 5th | 2 | 5th | 90° | Extraction of Herbert type screw+palm fasciectomy at MP level | 45° | 9 | 13 |
| 5 | Very extensive scar over the palm of the 5th finger | 3rd, 4th and 5th | 3 | 5th | 90° | Palm fasciectomy of the 3rd finger+fasciectomy at MP 5th finger level | 45° | 8 | 8 |
| 6 | Deformity impossible to reduce | 3rd, 4th and 5th | 3 | 4th | 80° | Palm fasciectomy of the 3rd and 4th fingers+fasciectomy at PIJ level of the 4th finger+capsulotomy and freeing of the checkrains of the 4th finger | 30° | 8 | 7 |
PIJ: proximal interphalangeal joint; MP: metacarpo-phalangeal joint.
100% consolidation of the arthrodesis was achieved in an average of 8 weeks, with a fusion angle of 30° in 3 patients and 45° in 3 patients, corresponding to the nominal angle of the device (Table 1).
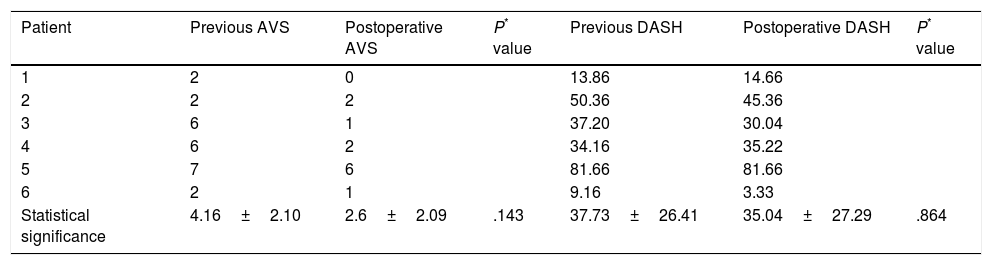
In all of the patients the pain level calculated using the AVS fell from 4.5 points to 2.6 points, although this was not statistically significant (P=.143). When the DASH questionnaire was used to evaluate the functionality of the operated hand the result was hardly favourable, falling from 37.73 points to 35.04 points (P=.864) (Table 2). When the clinical relevance of the changes was evaluated, no patient showed a relevant reduction in their DASH score,8 and only 50% of the patients experienced a relevant reduction in pain.9
Results in terms of pain and functionality.
| Patient | Previous AVS | Postoperative AVS | P* value | Previous DASH | Postoperative DASH | P* value |
|---|---|---|---|---|---|---|
| 1 | 2 | 0 | 13.86 | 14.66 | ||
| 2 | 2 | 2 | 50.36 | 45.36 | ||
| 3 | 6 | 1 | 37.20 | 30.04 | ||
| 4 | 6 | 2 | 34.16 | 35.22 | ||
| 5 | 7 | 6 | 81.66 | 81.66 | ||
| 6 | 2 | 1 | 9.16 | 3.33 | ||
| Statistical significance | 4.16±2.10 | 2.6±2.09 | .143 | 37.73±26.41 | 35.04±27.29 | .864 |
Average±standard deviation.
AVS: analogue visual scale; DASH: disabilities of arm, shoulder and hand questionnaire, Spanish version.
All of the patients were satisfied with the surgery and would accept it again.
No complications arose in connection with the PIJ arthrodesis, and there were no cases of implant migration or breakage, and no irritation of the soft tissues around the implant occurred.
DiscussionArthrodesis is a rescue procedure for patients with relapsing DD.10 There is very little in the bibliography on the clinical and functional results of arthrodesis procedures in the treatment of this condition.4,10,11 This procedure is not recommended for the routine treatment of Dupuytren's contracture.10
The arthrodesis consolidated in 100% of the cases in our series. This occurred in an average of 8 weeks, and these data are similar to those in previous publications.10,11 The position of the arthrodesis varied depending on the finger that was involved as well as the needs of the patient. In PIJ arthrodesis of the fingers it is generally recommended that the second finger be fused at 20°, the third finger at 30°, the fourth at 40° and the fifth at 45°.12 In three of our patients the arthrodesis was at an angle of 30° and in the other 3 it was at an angle of 45°. Fourth fingers were set an angle of 30° in arthrodesis, as the system does not allow other angles. One 5th finger was set at an angle of 30° in arthrodesis due to restriction of its MP hyperextension. The other fifth fingers were subjected to arthrodesis according to the recommendations described above.12
The functional results measured using the DASH scale were poor (Table 2). Few works in the literature specifically describe the functional results of PIJ arthrodesis of the fourth and fifth fingers in the case of relapsing DD, so that it is difficult for us to make comparisons. In their series of 16 patients operated using PIJ arthrodesis by shortening of the F1, Watson and Lovallo10 reported their results in terms of the total range of active movement and hand grasping force, and we do not have the corresponding data for our series. Honecker et al.13 reported on 7 cases of PIJ arthrodesis of the fifth finger with resection of the intermediate phalanx and stabilisation using a needle. Four of their cases were subsequent to repeat operations for DD, although they do not clearly describe the reason for the operations. They achieved 75% of good results in their series, measured by QuickDASH. A contradictory finding in our series is that in spite of the not very satisfactory results, 100% of the patients expressed their subjective satisfaction. In general it is hard to measure the results following treatment for Dupuytren's disease.14 The results were measured from the patient's viewpoint (PROM), such as arm, shoulder and hand disability (DASH), the Unité Rhumatologique des Affections de la Main scale and the Southampton Dupuytren Scoring Scheme, as well as the Michigan Hand Questionnaire. However, in practice these scales do not seem to function well, including the ones specifically designed for Dupuytren's disease.15
Pain is rarely reported in works on DD.16 In their evaluation of pain prior to surgery 3 patients had a high AVS score. One patient had arthrosis of the PIJ and another had the sequela of a previous arthrodesis; both of these patients underwent a significant reduction in pain after surgery (patients 3 and 4, Table 2). The other patient had neuropathic pain after surgery prior to the arthrodesis (patient 5). The incidence of neuropathic pain after fasciectomy stands at 3.4% (ranging from 0% to 7.7%) for primary surgery, and it may reach from 4.2% to 27% in the case of repeat surgery.17 Revision surgery may be contraindicated in these cases, and amputation of the finger becomes an option.18 This, together with not achieving the minimum improvement in terms of clinical relevance,9 may explain the poor result in this patient.
As far as we know this is the only published series in which severe relapse of DD is treated by an interlocking screws device. The general bibliography on the use of these new devices is very limited and almost inexistent. Vanderzanden et al.19 published a series of 17 patients treated using an interlocking device for metacarpo-phalangeal arthrosis of the thumb. They obtained 100% consolidation in an average of 7.9 weeks after surgery, with a fusion angle of 24.4° and an average follow-up of 4.9 months. They did not report any complications. Novoa et al. reported similar results in a series of 9 patients.20 In general, arthrodesis is not a procedure that is used very often in patients with DD, and only 2.8% of patients will require it.10 In the series reported by Watson and Lovallo10 there was 100% consolidation at 6 weeks, with an average fusion angle of 30° in the fourth finger and 37° in the fifth finger. Moberg21 recommends resecting the PIJ and using a square nail of bone from the proximal cubitus to leave the finger at 25° flexion. Watson and Fong11 describe a concave-convex arthrodesis technique as a rescue procedure. Izadpanah and Rizzo4 prefer the use of needles and a tension band. The majority of these works are about series of patients treated with primary surgery for Dupuytren's disease, in which isolated cases have occurred that required arthrodesis. It should be pointed out that our series, in spite of the fact that it is small, is one of the few to specifically focus on arthrodesis in case of severe relapse of DD.
The weakness of our study lies in the size of its sample, which is relatively small with a short follow-up. We are therefore unable to rule out the possibility that longer-term studies with large samples may detect complications with implants of this type and the possible bone defects that may be created if they are removed, if this were necessary. Another problem that should be evaluated but which did not occur in our series would be the treatment of relapse at MP level following the implantation of the APEX™ if the disease were in active phase, and the possible risk of infection around the implant in case of extensive incisions. The strength of this study lies in the fact that as it involves a single centre its internal validity is greater due to the uniformity of the patient treatment protocol and test evaluation. Likewise, although patient data was recorded retrospectively, they were evaluated by a specialist prospectively.
ConclusionIn our series the APEX™ system proved to be a reliable method of PIJ arthrodesis in patients with severe relapse of DD. Bone fusion was achieved in an average of 8 weeks at a consistent angle of fixation. It may be used together with other procedures in hands affected by severe relapse of DD. The functional results with use of this device in this group of patients were poor.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Novoa-Parra CD, Montaner-Alonso D, Pérez-Correa JI, Morales-Rodríguez J, Rodrigo-Pérez JL, Morales-Suarez-Varela M. Artrodesis de la articulación Interfalángica proximal del 4.° y 5.° dedo utilizando un dispositivo de tornillos entrelazados a compresión en el tratamiento de la recidiva grave de la enfermedad de Dupuytren. Rev Esp Cir Ortop Traumatol. 2018;62:216–221.