Arthroscopic stabilisation is a well-recognised surgical technique with a variable rate of failure reported between 0–35%. The aim of this study was to evaluate the outcome of this technique and our second aim was to identify risk factors that could be associated to recurrence rate.
Material and methods41 patients that underwent arthroscopic shoulder stabilisation for glenohumeral instability between 2001–2015 were included. Different items such as epidemiologic, recurrence, age at first dislocation, preoperative sport practice, and number of fixation devices used were collected. The results were evaluated using functional scales (WOSI, Rowe y Walch-Duplay) and radiological study was assessed using the Samilson-Prieto score. Data from the medical history were recognised in order to assess possible risk factors.
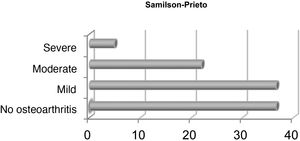
ResultsThe overall redislocation rate was 9.4%. The average follow-up was 83 months. The 54.3% of the patients achieved excellent/good results in the functional assessment scales. The range of motion was complete in 90% of the cases. On the radiographs, only 4.88% of the patients present advanced osteoarthritis. It was not possible to identify risk factors related to a worse outcome after surgery.
ConclusionThe arthroscopic Bankart repair with suture anchors is considered the gold standard for treatment of anterior glenohumeral instability. The long-term follow-up shows a favourable outcome, with a redislocation rate of 9% and low complication rate.
La estabilización artroscópica de la lesión de Bankart es una técnica ampliamente utilizada en la inestabilidad glenohumeral anterior con una tasa de recurrencia que puede variar, según la literatura, entre el cero y el 35%. El objetivo principal de este estudio es evaluar los resultados a medio-largo plazo de esta técnica, el objetivo secundario es identificar los posibles factores de riesgo asociados con la recidiva de la inestabilidad.
Material y métodosSe incluyeron 41 pacientes diagnosticados con inestabilidad glenohumeral anterior e intervenidos mediante cirugía artroscópica entre los años 2001 y 2015. Se evaluaron diferentes variables como los datos epidemiológicos, la recidiva de la luxación (subluxación o luxación), la edad del primer episodio, el tipo de actividad deportiva previa a la primera luxación y el número de implantes empleados en la cirugía. Los resultados funcionales fueron evaluados mediante las escalas.
Índice de inestabilidad de hombro de Western Ontario (WOSI), Rowe y Walch-Duplay y los resultados radiológicos a través de la escala de Samilson-Prieto. Se recogieron datos de la historia clínica con el fin de evaluar los posibles factores de riesgo.
ResultadosEn el studio, se observó una tasa de reluxación del 9,4% con un seguimiento medio de 83 meses. El 54,3% de los pacientes alcanzó resultados excelentes/buenos en las escalas de valoración funcional. El rango de movilidad fue completo en el 90% de los casos. En un 4,88% se apreció artrosis avanzada en los estudios radiológicos. No se identificaron factores de riesgo relacionados con un peor resultado tras la cirugía.
ConclusiónConsideramos que la estabilización artroscópica de la lesión de Bankart mediante anclajes de sutura es la técnica de elección en el tratamiento de la inestabilidad glenohumeral anterior primaria ya que consigue unos índices de recidiva razonables a medio-largo plazo (9%), con un índice de complicaciones bajo.
Anterior chronic glenohumeral instability is a common problem, which affects 1.7% of the population.1 The main therapeutic aim is to avoid a relapse of subluxation or luxation episodes with a reproducible technique which presents with a low rate of complications. To do this, many surgical techniques have been described, with different outcomes regarding the stability provided, rate of relapse, associated complications and functional outcome.
When treating this pathology, we may divide the surgical techniques into anatomical and non anatomical. The anatomical techniques try to restore the natural position of the labrum and the appropriate tensions of the capsuloligamintous complex, whilst the non anatomical ones seek to stabilise the shoulder, compensating the capsulolabral lesions or bony lesions with additional reinforcements.
Arthroscopic Bankart capsulolabral repair is the most used anatomic technique.2 Recent studies show that between the years 2006 and 2008, 87.7% of surgical treatments for shoulder instability consisted in repair of the Bankart lesión.3,4 Short term results of this technique are widely demonstrated with a recurrence rate of between 8% and 11%, equal to or better than rates for open surgery.4
Few studies have been published on the long-term outcomes of arthroscopic repair using suture anchors, with a recurrent rate of between 23% and 35% being recorded4,5 in series of more than 10 years evolution.
Among non-anatomic repair methods the Bristow-Latarjet procedure is outstanding. This technique presents with the lowest rate of long-term relapses,6 but with postoperative complications7 both in the mid to long term, a later return to sports activity with more limitation for external rotation8 and a higher risk of joint degeneration compared with anatomic repair.
The main aim of the study was to assess the mid-long term results of arthroscopic Bankart repair, using suture anchors in patients with anterior shoulder instability who underwent surgery in our centre. Our secondary aim was to assess the possible risk factors which could have been associated with an unsatisfactory result after surgery.
Materials and methodsThis study was approved by the ethics committee of the hospital (Protocol P.I: 175/16). The patients gave their written consent to participate in the study which was designed in keeping with the statute of Helsinki.
DesignA longitudinal, observational, retrospective study of a consecutive case series where we took a sample of patients who had been operated on using capsulolabral stabilisation through arthroscopy in our centre between the years 2001 and 2015.
Inclusion criteria were: patients over 18 years of age, who were operated on in our centre with arthroscopic capsulolabral stabilisation by two expert shoulder unit surgeons.
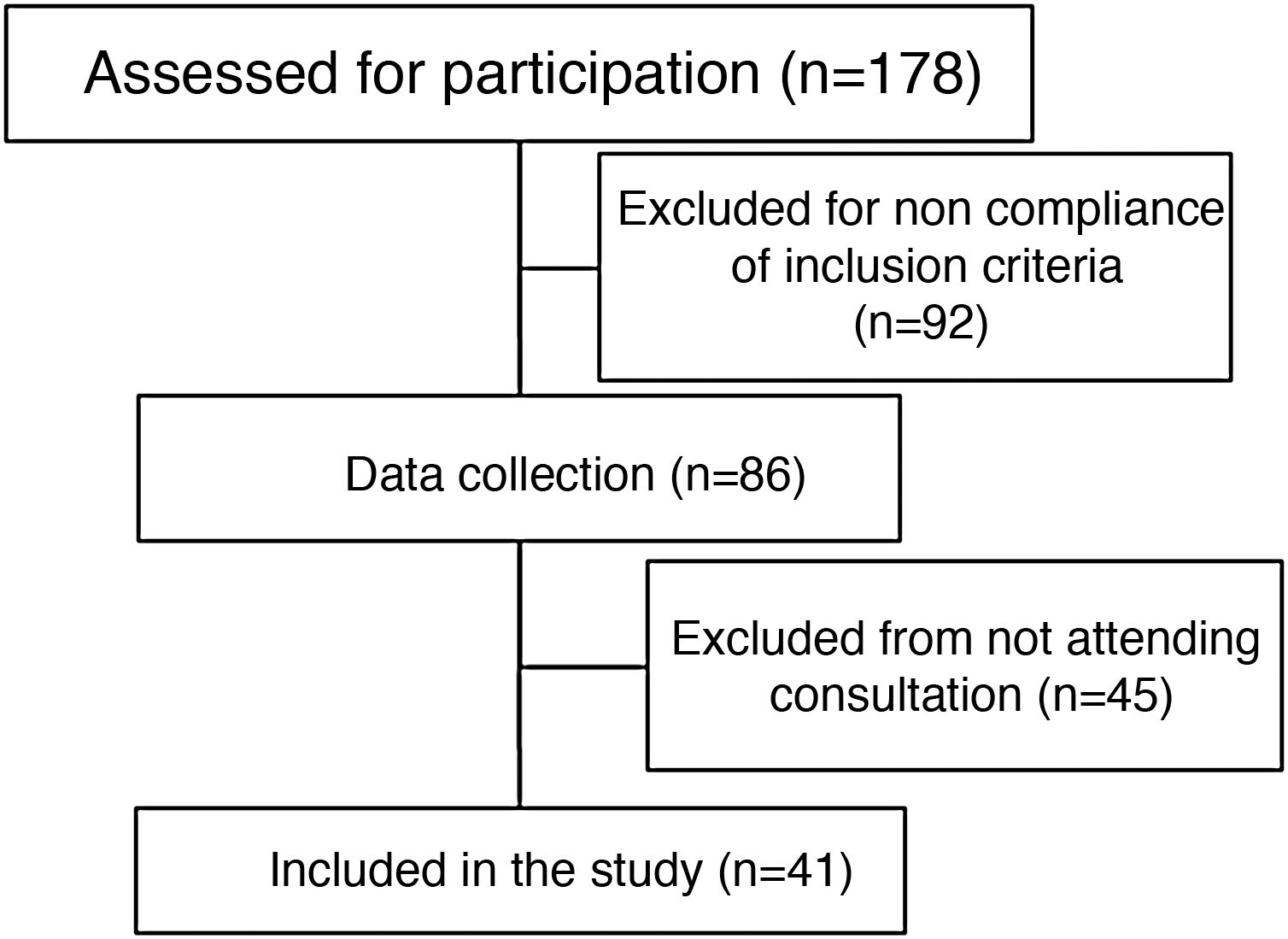
One hundred and seventy eight shoulder instabilities which were operated on were assessed. Patients under 19 years of age were excluded, along with those who had glenoid defects above 20% or who referred to previous surgery of the shoulder and for whom posterior follow-up had taken place. Those individuals who were not operated on with arthroscopic capsulolabral stabilisation were excluded.
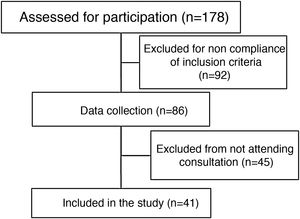
From our initial sample of 178 patients operated on for glenohumeral instability, we selected 86 who met all the criteria previously described. Taking this second sample as reference, we only accepted individuals who had attended consultation and who had a control shoulder X-ray at the time of the study. As a result the final sample comprised 41 patients (Fig. 1).
Outcome measurementsThe primary result of this study was recurrent instability, defined as luxation or subluxation experienced by the patient.
Secondary results were subjective shoulder instability, shoulder function and quality of life perceived by the patient. This was assessed with three functional scales: The Western Ontario shoulder instability scale (WOSI), the Rowe scale and the Walch-Dupla scale. The questionnaires of the different scales include data regarding sport and type of sport practiced, relapses, pain, weakness, apprehension, range of movement and feelings such as worry or fear. The questionnaires were completed in the medical practice and for the Rowe and Walch-Duplay9,10 scales, patients were classified into different categories according to the function of the numerical value obtained: “excellent” (90 to 100), “good”(75 to 89), “medium” (51 to 74) and “poor” (<50). The WOSI scale was expressed in the percentage obtained.
Data from the medical file were collected to assess possible risk factors in recurrent shoulder instability, such as age at time of surgery, number of previous luxations to this one, hyperlaxitude, age at first luxation, sport practised, presence of Bankart or Hill-Sachs lesion and number of implants used.
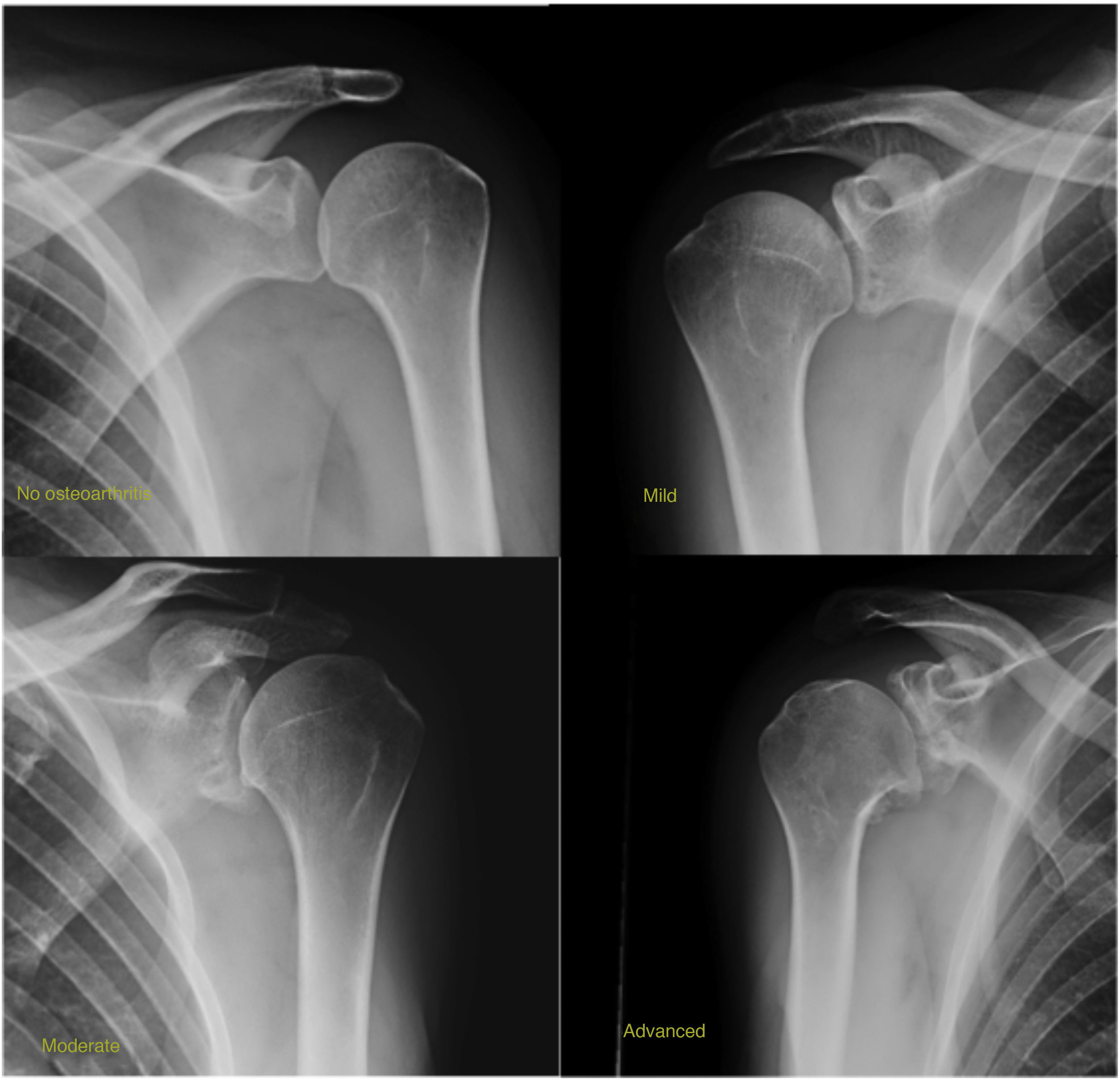
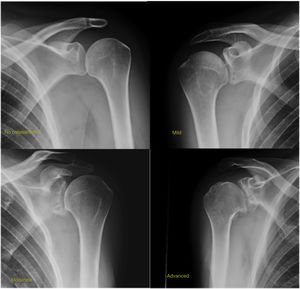
Radiological analysisThe shoulder X-rays (true anteroposterior, axilliary and anteroposterior projections in internal and external rotation) performed in the medical practice were examined by a trauma surgeon with experience in shoulder surgery and also a radiologist. They were classified according to the Samilson and Prieto scale: no osteoarthritis, mild osteoarthritis (presence of humeral osteophyte or glenoid under 3mm), moderate osteoarthritis (osteophyte between 3 and 7mm with slight reduction of joint space) and severe osteoarthritis (osteophyte over 7mm with frank reduction of joint space) (Fig. 2).
Statistical analysisPatient characteristics are described as mean and standard deviation (SD) or median and interquartile range (IQR) depending on whether the distribution can be accepted or not as normal. The categorical variables were presented using absolute and relative frequencies. The main result, recurrent instability, was expressed as a percentage of patients who experienced frequent instability after arthroscopic Bankart stabilisation. Univariate analysis was performed of the possible association between the independent variables with recurrent instability. The categorical variables were analysed using the Fisher exact test. For secondary results, a Mann–Whitney U test was used to assess the differences in the WOSI, Rowe and Walch scores between the recurrence group and the non recurrence group. The possible association with osteoarthritis was analysed using the Kruskar-Wallis test. A subanalysis was made which assessed the impact of several risk factors in recurrent instability after arthroscopic Bankart repair, extracted from patient's medical records. Statistical analysis was performed with the STATA 15 software and p values of <.05 were considered significant.
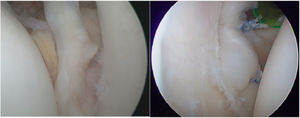
SurgicalArthroscopic repair was carried out in all cases under general anaesthesia and interescalenic block with the patient in beach chair position. To confirm the pattern of instability, examination under general anaesthesia was made prior to the beginning of surgery. Three arthroscopic portals were used to carry out the procedure (posterior, anterior and anterosuperior).
A complete diagnostic arthroscopy was performed, seeking joint lesions, such as the disinsertion of the anteroinferior glenoid labrum, the distention of the joint capsule and the state of the glenohumeral ligaments. The Hill-Sachs humeral lesion was identified and quantified as was the anteroinferior lesion of the bony glenoid surface. Chrondral lesions and the integrity of the rotator cuffs were also assessed.
Labrum reinsertion linked to anterior capsular plication was performed using suture anchors. When there was posterior instability posterior stabilisation was added (Fig. 3).
The postoperative period consisted of shoulder immobilisation for three weeks. External rotation was limited and at night a sling was worn for six weeks. After three weeks, the patient began with passive and assisted active exercises. At six weeks they began active exercises and after three months muscle strengthening.
ResultsMean age of the 41 patients included was 34.9 years. Of them, 32 (78%) were men and nine (22%) women. The mean age of the first luxation was 27 years and the median of episodes prior to surgery was 6.5. Sixty five point eight per cent of men were right-handed and in 75% this was the dominant shoulder. Almost 22% of people were hyperlax, defined according to the Beighton11 criteria as external rotation above 90° in abduction, extension of the fifth metacarpophalange of 90°, hyperextension of the elbow of over 10° and distance of the thumb to volar surface of the forearm of under 21mm.
Out of the total sample, 10 patients (24.3%) did not practice sport, 30 (73.1%) did so for leisure and one (2.4%) practiced competitive sport. Of those who practised sport, 10 (32.2%) were activities with no risk (athletics, rowing, swimming backstroke or breaststroke, diving, physical education, cross-country skiing, sailing), nine (29.0%) performed contact sports (martial arts, cycling, motorcycling, football, water skiing, alpine skiing, skydiving and riding) 11 (35.4%) sports with arm raising (weight lifting, swimming butterfly stroke and crawl, skating, golf, hockey, tennis, baseball) and one (3.2%) risk sports (basketball, handball, volleyball, water polo and kayak).
After surgery, 23 patients (74.2%) were able to return to the sport they practised before and eight (25.8%) had to change activity.
A Hill-Sachslesion presented in 43.9% of cases, a Bankart lesion in 85% and a glenoid bony defect (under 20%) in 15% of patients. As a mean, 2.52 implants (one to six) were used. The anterior anchors were used in all cases and the posterior ones in 25%. Data from four patients were collected (9.4%) who again had episodes of luxation, and one of them required further surgery (Latarjet procedure). These four individuals were operated on between 2001 and 2004, and they all relapsed over five years after intervention. Regarding the number of implants used, three patients had two anchors and one had three. No complications arose during surgery.
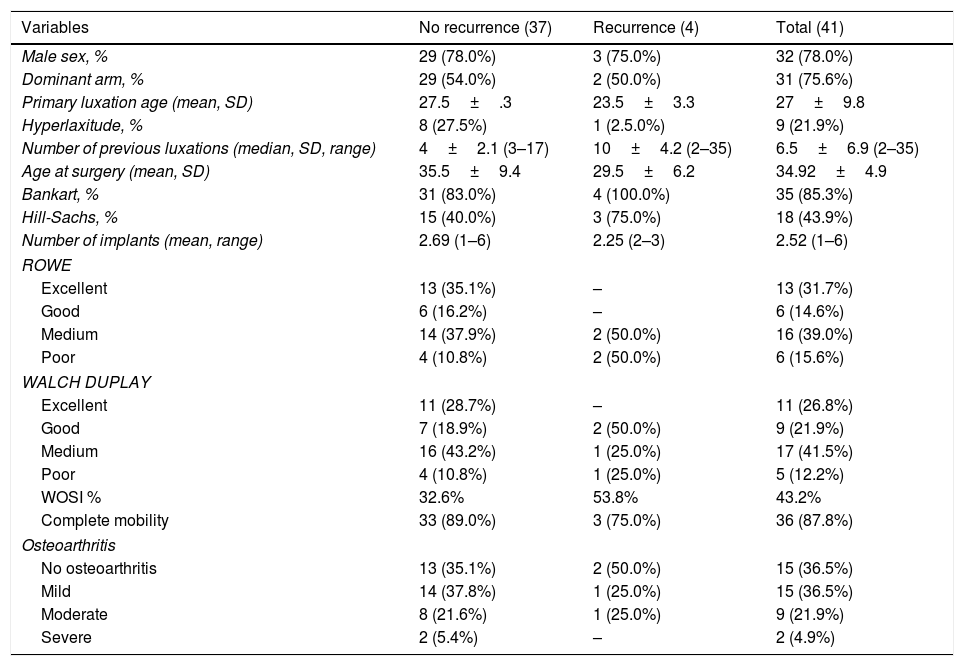
In 54.3% of cases good or excellent results were obtained in the functional scales and a complete mobility range was achieved in 36 patients (87.8%). In those with over five years of follow-up, the results in the functional scales were good or excellent in 60% (Table 1).
Variables studied based on recurrence.
| Variables | No recurrence (37) | Recurrence (4) | Total (41) |
|---|---|---|---|
| Male sex, % | 29 (78.0%) | 3 (75.0%) | 32 (78.0%) |
| Dominant arm, % | 29 (54.0%) | 2 (50.0%) | 31 (75.6%) |
| Primary luxation age (mean, SD) | 27.5±.3 | 23.5±3.3 | 27±9.8 |
| Hyperlaxitude, % | 8 (27.5%) | 1 (2.5.0%) | 9 (21.9%) |
| Number of previous luxations (median, SD, range) | 4±2.1 (3–17) | 10±4.2 (2–35) | 6.5±6.9 (2–35) |
| Age at surgery (mean, SD) | 35.5±9.4 | 29.5±6.2 | 34.92±4.9 |
| Bankart, % | 31 (83.0%) | 4 (100.0%) | 35 (85.3%) |
| Hill-Sachs, % | 15 (40.0%) | 3 (75.0%) | 18 (43.9%) |
| Number of implants (mean, range) | 2.69 (1–6) | 2.25 (2–3) | 2.52 (1–6) |
| ROWE | |||
| Excellent | 13 (35.1%) | – | 13 (31.7%) |
| Good | 6 (16.2%) | – | 6 (14.6%) |
| Medium | 14 (37.9%) | 2 (50.0%) | 16 (39.0%) |
| Poor | 4 (10.8%) | 2 (50.0%) | 6 (15.6%) |
| WALCH DUPLAY | |||
| Excellent | 11 (28.7%) | – | 11 (26.8%) |
| Good | 7 (18.9%) | 2 (50.0%) | 9 (21.9%) |
| Medium | 16 (43.2%) | 1 (25.0%) | 17 (41.5%) |
| Poor | 4 (10.8%) | 1 (25.0%) | 5 (12.2%) |
| WOSI % | 32.6% | 53.8% | 43.2% |
| Complete mobility | 33 (89.0%) | 3 (75.0%) | 36 (87.8%) |
| Osteoarthritis | |||
| No osteoarthritis | 13 (35.1%) | 2 (50.0%) | 15 (36.5%) |
| Mild | 14 (37.8%) | 1 (25.0%) | 15 (36.5%) |
| Moderate | 8 (21.6%) | 1 (25.0%) | 9 (21.9%) |
| Severe | 2 (5.4%) | – | 2 (4.9%) |
SD: Standard Deviation calculated; WOSI: Western Ontario shoulder instability index.
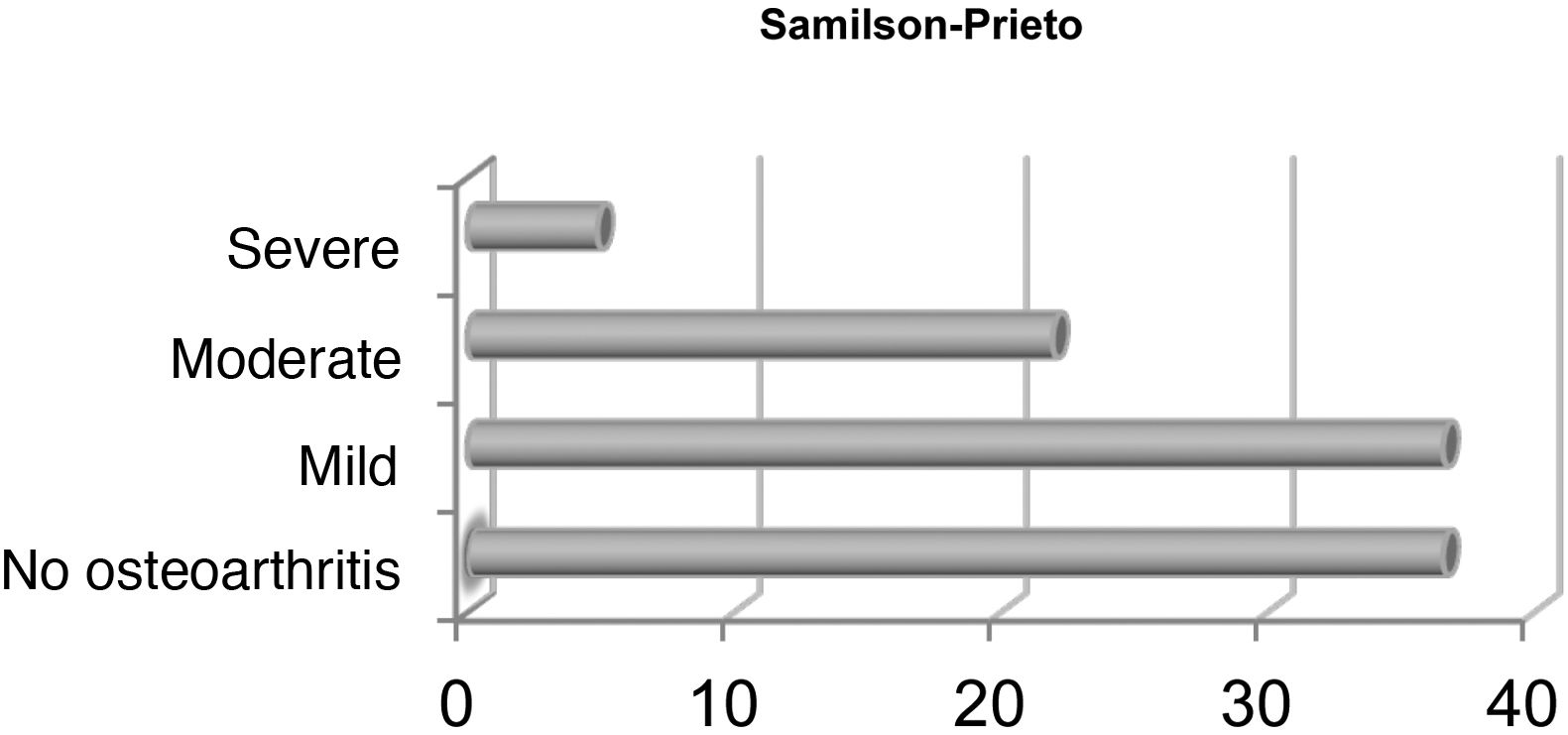
Seventy-three per cent of participants did not present with osteoarthritis o it was mild (humeral or glenoid osteophyte under 3mm with no reduction in joint space) (Fig. 4).
The appearance of osteoarthritis was not statistically significantly linked with sex, age of first luxation or number of presurigcal luxations but a tendency was observed that the higher the number of luxations, the greater the rate of postoperative osteoarthritis. It was also confirmed that the case of reluxation after intervention had had numerous previous episodes with a median of 10 luxations, without this being statistically significant. No relationship was found between the number of a anchors and osteoarthritis or relapse of luxation.
Eighty-seven point eight per cent of patients achieved complete mobility and those who did not obtain it did not have osteoarthritis or this was mild. Those classified as having severe osteoarthritis had no limitations of movement.
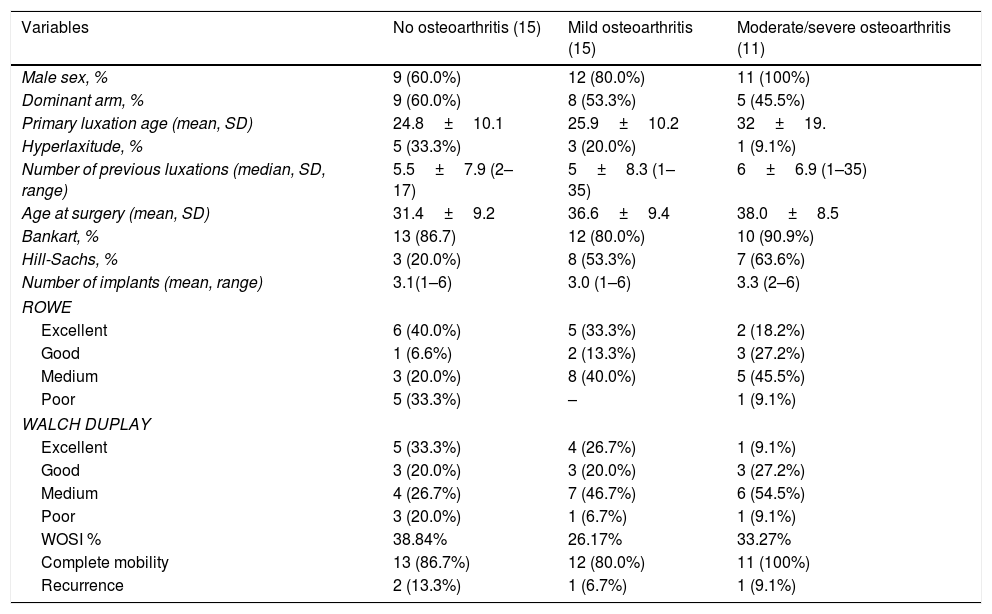
Of the individuals who suffered from reluxations, two did not have osteoarthritis, one had mild osteoarthritis and the other moderate (Table 2).
Variables studied based on osteoarthritis.
| Variables | No osteoarthritis (15) | Mild osteoarthritis (15) | Moderate/severe osteoarthritis (11) |
|---|---|---|---|
| Male sex, % | 9 (60.0%) | 12 (80.0%) | 11 (100%) |
| Dominant arm, % | 9 (60.0%) | 8 (53.3%) | 5 (45.5%) |
| Primary luxation age (mean, SD) | 24.8±10.1 | 25.9±10.2 | 32±19. |
| Hyperlaxitude, % | 5 (33.3%) | 3 (20.0%) | 1 (9.1%) |
| Number of previous luxations (median, SD, range) | 5.5±7.9 (2–17) | 5±8.3 (1–35) | 6±6.9 (1–35) |
| Age at surgery (mean, SD) | 31.4±9.2 | 36.6±9.4 | 38.0±8.5 |
| Bankart, % | 13 (86.7) | 12 (80.0%) | 10 (90.9%) |
| Hill-Sachs, % | 3 (20.0%) | 8 (53.3%) | 7 (63.6%) |
| Number of implants (mean, range) | 3.1(1–6) | 3.0 (1–6) | 3.3 (2–6) |
| ROWE | |||
| Excellent | 6 (40.0%) | 5 (33.3%) | 2 (18.2%) |
| Good | 1 (6.6%) | 2 (13.3%) | 3 (27.2%) |
| Medium | 3 (20.0%) | 8 (40.0%) | 5 (45.5%) |
| Poor | 5 (33.3%) | – | 1 (9.1%) |
| WALCH DUPLAY | |||
| Excellent | 5 (33.3%) | 4 (26.7%) | 1 (9.1%) |
| Good | 3 (20.0%) | 3 (20.0%) | 3 (27.2%) |
| Medium | 4 (26.7%) | 7 (46.7%) | 6 (54.5%) |
| Poor | 3 (20.0%) | 1 (6.7%) | 1 (9.1%) |
| WOSI % | 38.84% | 26.17% | 33.27% |
| Complete mobility | 13 (86.7%) | 12 (80.0%) | 11 (100%) |
| Recurrence | 2 (13.3%) | 1 (6.7%) | 1 (9.1%) |
SD: Standard Deviation calculated; WOSI: Western Ontario shoulder instability index.
No risk factors were determined which could have been significantly related to reluxation. The people who had reluxatio were between 20 and 28 years of age when they suffered from the first episode. No statistical significance was found with hyperlaxitude or with the sport practised. One patient did not practise a sport, another practised a physical activity with no risk, another a contact sport and the last, a high risk sport. The person who practiced competitive sport went back to their regular practice and had no further episodes of instability.
DiscussionThe posterior effects of shoulder stabilisation may be assessed using subjective and objective variables. In this study, relapse is highly valued (subluxation or luxation) and glenohumeral osteoarthritis in plain X-ray as objectives means of failure and the functional status of the pattern using the result of different scales as the subjective measurement.
Recurrence of instabilityOur study included 41 patients with a mean follow-up of 83 months. A relapse rate (reluxation) of 9.4% was reported. These results are comparable with other studies found in the literature. Carreira reported a 10% recurrence of instability in 85 patients with 24 months follow-up.12
There are few long-term studies where arthroscopic Bankart repair results have been assessed. Castagna5,13 obtained a recurrent rate of 16% with a follow-up of 130 months and Aboalata14 18% with follow-up of 156 months. Other studies refer to rates ranging between 23% and 35% of relapse.12,15 it is possible that the rate of relapse of luxation increased over follow-up time. In our study, the four patients had reulxations after five years and this may be confirmed by research studies such as that of Zimmerman,16 suggesting that time after surgery is one of the main factors concerning relapse.17–19
Glenohumeral osteoarthritisThe natural history of glenohumeral instability, as described by Hovelius,1 is the progression towards osteoarthritis in 55% of cases in 10 years, even in a single episode of luxation. The appearance of postoperative osteoarthritis after capsulolabral repair varies 21.8%20 to 69%21 in published studies. Recent studies such as that of Bock22 outline that, despite carrying out good repair of the capsulolabral complex, progression of osteoarthritis is independent from surgery when compared with the healthy side and concludes that there is a predisposition to develop osteoarthritis in the shoulders which have been dislocated. In our study, 73% of patients did not present with osteoarthritis or it was mild. These results are similar to those found in the literature.23 Only 4.88% of individuals suffered from advanced osteoarthritis which is a better result fromthat of studies such as Privitera18 where there was 40% osteoarthritis, albeit at 10 years.
We believe that it is clinically relevant to have found that the patients who presented with the most osteoarthritis are those who have suffered more preoperative luxations. These data lead us to recommend carrying out early surgery15,24 and not wait for multiple luxations, particularly in young, active patients.25 No statistically significant cut-off value was found for the number or preoperative luxations.
In our study we found there was a statistically significant relationship between the ROWE and osteoarthritis, with the result that the higher the score in it, the lower the appearance of this disease. We believe this finding may bring us to no conclusion, given the small sample size and few variables included in this scale, some of which are subjective.
Functional evaluationThere were few long-term studies where the arthroscopic surgical results were assessed using subjective functional scales. Seventy five per cent of patients considered their status as excellent and/or good according to the WOSI scale. The patients who presented with relapse of instability had poorer scores without this finding being statistically significant. Furthermore, we were able to observe that, the better the WOSI scale result, the lower the degree of osteoarthritis (although this association was not statistically significant). We found results were similar in other studies.15
Regarding the Walch Duplay scale, we observed 18 cases (almost 50%) of excellent or good results in patients without reluxation. In those who suffered form reluxation, two showed good results, one medium and the rest, poor. In the Tordjman26 study 31 people who underwent the same technique were evaluated, obtaining good results in 75% of them, but with a higher rate of reluxation after five years of follow-up (25%) than in our study. This study concluded that, despite the good results, this scale did not correlate with any risk of recurrence.
The results assessed were excellent or good according to the ROWE scale in 19 patients (over half of the individuals without recurrence) and medium or poor in all those who suffered from relapse. However, these results were not statistically significant.
Prognostic factorsMany studies identified early age as a separate risk factor for failure after arthroscopic Bankart repair.19,27 This may be due to the participation of young patients practising high risk sports or an inappropriate postoperative protocol from these patients due to non compliance.
The Arciero28 study assessed 36 patients with a mean age of 20 years. The rate of reluxation in individuals treated conservatively was 80% vs.14% of patients who underwent capsulolabral repair. Robinson29 studied the rate of reluxation in 88 people with a mean age of 24.8 years and a follow-up of two years after intervention. These people had suffered from a single episode of luxation and were operated on during the first month with capsulolabral repair compared with plain arthroscopy and lavage. The rate of reluxation was 14% in the first group and 38% in the second. These results are comparable to our study, where patients who relapsed had a mean age of 23.5 years the first time they suffered an episode of luxation.
The number of luxations prior to surgery was identified as a risk factor for the development of osteoarthritis.20,21 In the Plath study we found there was a positive correlation between the number of luxations prior to surgery and the appearance of osteoarthritis. In this study (with 100 patients assessed) the mean of preoperative luxations was six. In our study, the individuals who presented with more osteoarthritis also had a median of six luxations.
Equally, in several studies,20,21,27 the number of implants has been regarded as a risk factor for the development of osteoarthritis, with a mean of four implants (two to seven) in the patients who suffered from greater osteoarthritis. This is similar to what we found in our study, where 3.3. Implants were used on average (two to six).
Strengths and limitationsOur study had several strengths. It is one of the few studies where three different evaluation scales were used, where a control X-ray was provided to assess postoperative osteoarthritis and the minimum follow-up of patients was two years. All the subjects were operated on by two surgeons experienced in shoulder surgery. However, this was a retrospective study with inherent limitations. In the first place, we were only able to include 41 of our 86 patients due to lack of follow-up. Also, most preoperative X-rays were not available and neither did we have the three functional scales prior to surgery and they could therefore not be compared. Furthermore, the small sample size prevented us from reaching conclusions that provided outcome predictions. Lastly, we did not have a group which used a different technique with which to compare it, since the Bankart repair is, in our experience, the optimum treatment to use in this group.
All of this led us to conclude that, given the diversity among studies in current literature, it is essential to carry out a prospective study that includes preoperative e data (scales, X-rays, sport practised, mobility, etc.) comparing them with the postoperative results in the different follow-up controls.
ConclusionWe consider that arthroscopic stabilisation of the Bankart lesion using suture anchors is the treatment of choice for primary anterior glenohumeral instability since we obtained reasonable mid- to long-term rates of relapse (9%), with a low rate of complications.
Level of evidenceLevel of evidence III.
FinancingThe authors of this study declared they had not received any financing for conducting it.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: García-Vega M, De La Cuadra-Virgil P, Jiménez-Cristobal J, Occhi-Gómez B, Boserman-Pérez-de Villaamil M. Reparación capsulolabral artroscópica en la inestabilidad glenohumeral anterior. Resultados a medio y largo plazo. Rev Esp Cir Ortop Traumatol. 2021;65:255–263.