Bisphosphonates are currently considered first choice treatment of osteoporotic disease. Its proven anti-fracture effect in all types of osteoporosis and its presence on the market for many years make them the most widely used drugs for the treatment of this disease. A number of adverse effects associated with this medication that have appeared over the past 10 years or so have caused concern on whether or not to maintain a continued treatment with these drugs over a long period of time. These side effects include a series of fractures, considered atypical because of their location and radiological appearance, which occur in patients treated long-term with bisphosphonates. These fractures that share a number of common clinical features, do not meet the classic profile of osteoporotic fragility fractures. Prolonged inhibition of bone remodelling could be the pathophysiological basis for this explanation, although this causal relationship is not yet clearly established. The objective of this paper is two-fold, on the one hand to present four clinical cases of atypical fractures related with long-term administration of these drugs and, on the other, to perform a literature review of this pathological entity, in an attempt to clarify what is the real status of this problem and whether it is necessary to establish both surgical and non-surgical therapeutic recommendations for these types of fractures.
Los bifosfonatos son considerados actualmente un tratamiento de primera elección de la enfermedad osteoporótica. Su reconocida eficacia antifractura en todos los tipos de osteoporosis y su presencia en el mercado desde hace varios años, hacen que sean los fármacos de uso más extendido para el tratamiento de la enfermedad. En la última década han aparecido una serie de efectos adversos relacionados con esta medicación que han encendido la voz de alarma sobre la conveniencia o no de mantener el tratamiento continuado con estos fármacos durante un largo período de tiempo. Entre estos efectos se encuentra la aparición de una serie de fracturas consideradas atípicas por su localización y apariencia radiológica que se manifiestan en pacientes tratados de forma crónica con bifosfonatos. Estas fracturas que comparten una serie de características clínicas comunes, no cumplen el clásico perfil de la fractura por fragilidad osteoporótica. La prolongada inhibición del remodelado óseo podría ser el sustento fisiopatológico para su explicación, aunque todavía no está claramente establecida esta relación causal. El objetivo del presente trabajo es doble, por un lado presentar cuatro casos clínicos propios de fracturas atípicas relacionadas con la administración de estos fármacos y, por otro, realizar en base a ellos una revisión bibliográfica de esta entidad patológica, para intentar esclarecer cuál es la situación real del problema y determinar si es necesario establecer algún tipo de recomendaciones terapéuticas, tanto quirúrgicas como no quirúrgicas, ante este tipo de fracturas.
Bisphosphonates are considered to be the standard of care for osteoporosis, with alendronate and risedronate as first-line drugs.1 Both drugs have proven efficacy in reducing vertebral, as well as non-vertebral and hip fractures in women with osteoporosis. Furthermore, they are indicated as drugs of choice in osteoporosis in males and in steroid-induced osteoporosis.1,2
A debate has risen in the last several years as to whether the profound suppression of bone remodelling that these drugs induce might have a negative effect on the mechanical resistance of bone, especially after 4 years of continuous treatment.3 In 2005, the first case reports on a fracture series were published; these fractures were defined as atypical because they failed to meet the classical profile of osteoporotic fragility fracture that end up being catalogued as a complication associated with the hypersuppression of remodelling caused by prolonged therapy with alendronate.4 Since then, numerous items, generally in the form of case reports,5–18 have been published relating this type of fracture, generally in the subtrochanteric region or in the femoral diaphysis, with prolonged treatment with bisphosphonates. A recent review of the cases published in the literature identifies 141 cases that would meet the characteristics set forth to define this type of “atypical fracture”.19 Despite the fact that a very low incidence of this type of fracture is seen in the post hoc analysis of the leading long-term follow-up studies with bisphosphonates and a causal relationship cannot therefore be established between the prolonged administration of these drugs and the appearance of these fractures,20 an alarm has been sounded among health professionals regarding the possible risk to patients receiving this medication over prolonged periods of time.
Thus, the aim of the present work is twofold: on the one hand, it seeks to present four case reports of atypical fractures associated with the administration of these drugs and use these to conduct an updating of the disease entity, since, bearing in mind that bisphosphonates are the most widely used drugs for the treatment of osteoporosis, we perceive a need to calibrate this risk accurately and to determine whether some type of treatment recommendations are needed, both surgical and non-surgical, when facing this type of fracture.
Case reportsCase number 1Seventy-four year old female with a history of high blood pressure and type II diabetes under outpatient treatment with enalapril maleate-hydrochlorothiazide and metformin, diagnosed with postmenopausal osteoporosis 10 years ago and treated since then with alendronate (5mg/day for 4 years and 35mg/week for 6 years), with good treatment compliance and without any noticeable side effects; she comes to the Emergency Room due to pain and deformity in the thigh after a casual fall down some stairs. The patient reported having suffered bilateral pain in the groin-femoral region prior to this fall for the previous 7 months without any history of trauma and for which she had been under treatment with NSAID by her general practitioner without any significant improvement.
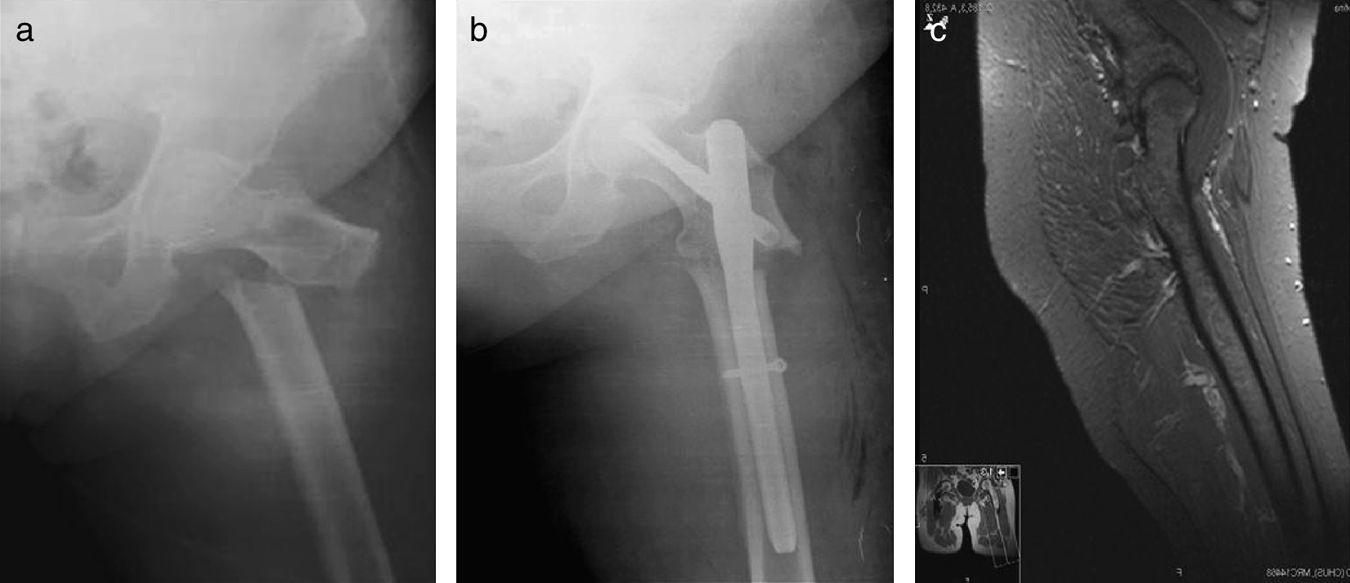
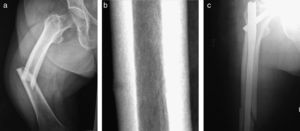
On admission, radiological tests show a transverse, slightly oblique subtrochanteric fracture of the femur with a medial spicule and thickening of the lateral cortical bone (Fig. 1a) that had been diagnosed as an atypical subtrochanteric fracture of the femur associated with the prolonged use of bisphosphonates, and said treatment was discontinued at that time. Having carried out the proper preoperative tests, screening for secondary osteoporosis (haemogram, blood count, blood formula, ions, BUN, Cr, albumin, proteins, proteinogram, calcium, phosphorus, 25-OH vitamin D, PTH, FAL, osteocalcin, TSH, and calcium in urine, all within normal limits) and an X-ray of the contralateral femur that did not reveal any significant pathological alterations, she was treated surgically by means of dynamic locking endomedullary nailing with reaming of the medullary canal with a TFN long nail (Synthex) (Fig. 1b). During the immediate postoperative period, a DEXA was performed (total BMD of the femoral neck with 0.734g/cm2, T score −1.7, Z score 0.0), as was an MRI of the contralateral hip-femur that did not show evidence of periosteal oedema or diaphyseal stress fractures (Fig. 1c). The patient's follow-up to date is satisfactory and she is currently being treated with 1-34 PTH.
Case number 2Seventy-nine year old female, without any clinical history of interest who has been following treatment with alendronate for more than 10 years (5mg/day for 3 years and 35mg/week for 7 years) and oral calcium supplements for osteoporosis (BMD L1–L4 with 0.528g/cm2, T total −4.72, Z total −2.99). Total BMD of the femoral neck with 0.750g/cm2, T score −1.87, Z score −0.55. Adherence to treatment over the course of these years had been correct, maintaining the said treatment uninterruptedly. For the last three years, steroid treatment has been associated at a dose of 6mg per day of deflazacort due to non-specific, generalized joint pain.
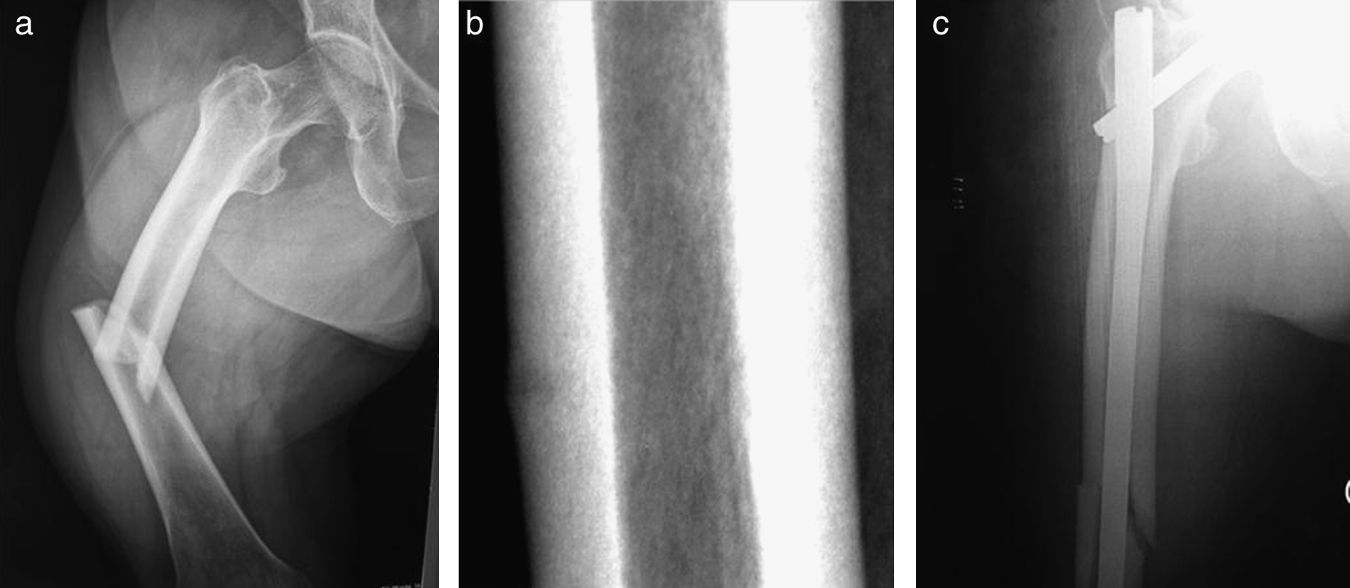
Prior to admission, the patient reported non-specific pain in her right thigh, without prior trauma over the preceding 1 month that was assessed by her general practitioner and treated symptomatically. Since her pain continued despite treatment, the patient went to the Emergency Room where a series of radiological studies were performed and failed to reveal any kind of pathological alteration; the patient was therefore referred for evaluation to the ordinary trauma clinic. While leaving to home, the patient suddenly suffered a sharp pain in the medial area of the thigh that was accompanied by a snapping sound and subsequent fall to the ground. She was readmitted to the same department and diagnosed with a diaphyseal fracture of the right femur. Radiologically, a fracture of middle third of the femur is seen, with a transversal line, medial spicule, and thickening of the lateral cortical bone (Fig. 2a). On reviewing the X-ray previously performed on the patient, an area of external cortical thickening is seen in the mid-diaphyseal area, with a faint fracture line (Fig. 2b). In light of the patient's clinical history and given the radiological characteristics of the fracture, she was diagnosed with an atypical diaphyseal fracture of the femur associated with prolonged use of bisphosphonates, and was admitted for surgical treatment of the fracture. Osteosynthesis was performed with a long, reamed, intramedullary Gamma® nail (Stryker Corporation) (Fig. 2c). The patient's analyses conducted to screen for secondary osteoporosis were within normal limits and the radiological analysis of the contralateral femur did not yield any significant radiological alterations.
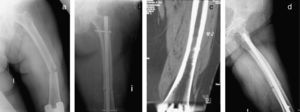
Case number 3Sixty-three year old female who presents at the Emergency Room after spontaneous fracture of the proximal diaphysis of the left femur with a transversal fracture line, thickening of lateral cortical bone, and medial spicule (Fig. 3a). The patient had been receiving treatment with oral alendronate (5mg/day for 3 years and 35mg/week for 7 years) for more than 10 years for osteoporotic disease with good adherence to treatment and without any noticeable side effects, although three years ago the patient had been diagnosed with a stress fracture in her right tibia which consolidated completely (Fig. 3b). Diagnosed with an atypical fracture of the femoral diaphysis associated with the prolonged use of bisphosphonates, the patient was admitted for study and surgical treatment. The appropriate preoperative testing is performed, as well as screening for secondary osteoporosis, which revealed an associated deficit of vitamin D, and the patient was treated surgically by means of a long, reamed, Gamma® endomedullary nail (Stryker Corporation) (Fig. 3c). The radiological study of the contralateral femur was normal.
Case number 4Seventy-nine year old female with a history of high blood pressure and hyperlipidaemia under outpatient treatment with candesartan cilexetil and atorvastatin, diagnosed 11 years ago with postmenopausal osteoporosis; since then, she has been receiving treatment with alendronate (5mg/day for 4 years and 35mg/week for 7 years) with good adherence to treatment and without any noticeable side effects.
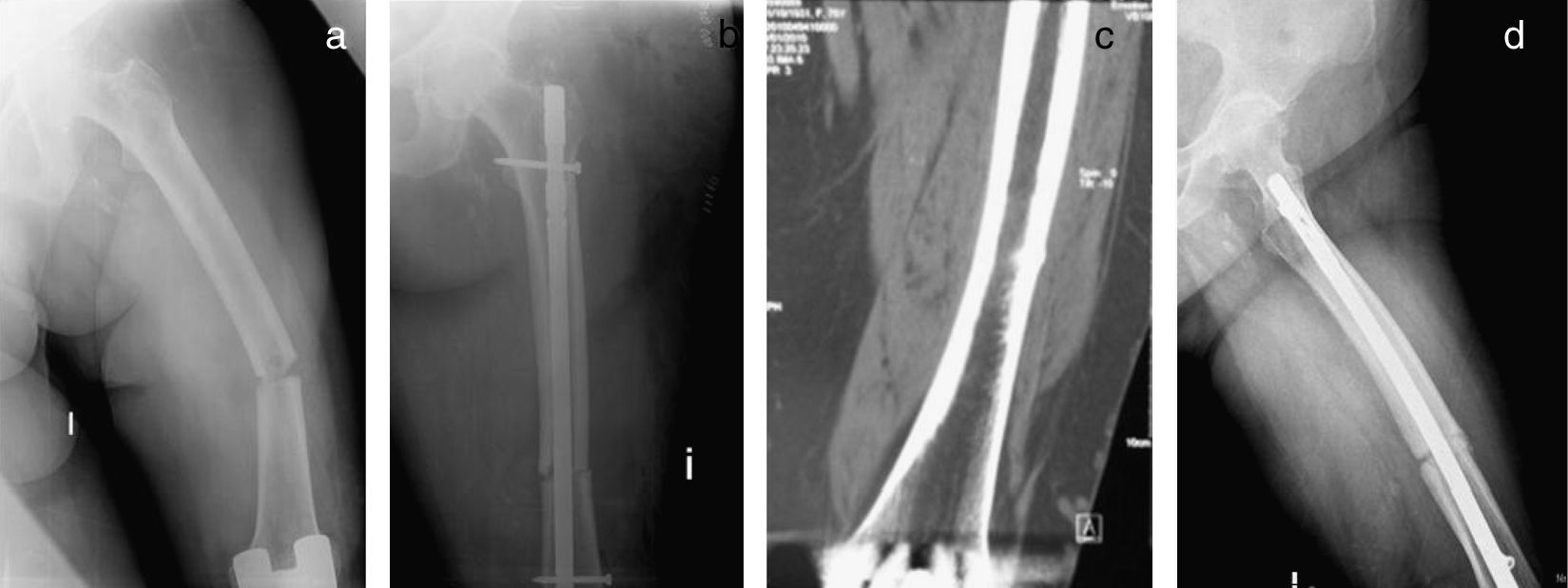
The patient presented at the Emergency Room after having suffered trauma from a fall from standing height with pain, deformity, and functional impediment for standing and walking. Radiologically, a transverse fracture of the femoral medio-diaphysis with a medial spicule and thickening of the lateral cortical bone (Fig. 4). At that time the patient was not diagnosed with an atypical fracture and was treated with an unreamed, static, UFN endomedullary nail (Synthex) (Fig. 4b), with discontinuation of treatment with bisphosphonates deferred until 4 months after surgery.
In light of the fact that the patient reported having undergone a total arthroplasty of the knee on the same side 36 months earlier and from which she was still being seen at the outpatient clinic for thigh pain that had gotten worse in the previous 6 months and failed to improve with analgesic treatment or with NSAIDs, the imaging studies are reviewed in order to assess said painful arthroplasty and a prior CT reveals monocortical thickening with stress fracture (Fig. 4c) that went undetected at the time. With these data, the patient was diagnosed with an atypical fracture of the femoral medio-diaphysis associated with prolonged use of bisphosphonates and admitted for evaluation and screening for secondary osteoporosis (without evidence of any significant alteration), an X-ray of the contralateral femur (no relevant pathological alterations), and a DEXA of the contralateral hip that showed discreet osteopenia (total BMD of the femoral neck 0.816g/cm2, T score −1.0, Z score 1.0). At present, 12 months after the surgery, fracture consolidation is delayed (Fig. 4d) and the patient is awaiting dynamization of the nail and treatment with 1-34 PTH.
State of the artConcept of atypical fractureAtypical fractures associated with the prolonged use of bisphosphonates tend to be fractures located in the proximal third of the femoral diaphysis, although they can appear at any other point of this diaphysis, from the distal portion of the lesser trochanter to the proximal portion of the supracondylar prominence of the distal femoral metaphysis.21
In terms of the causative mechanism, they normally appear following low energy trauma, equivalent to a fall from the person's own height or less, although they may occur spontaneously.21
Pathologically speaking, the fractures may be complete or incomplete; in either case, they may be bilateral. Complete fractures affect the entire diaphysis; they usually have a transversal or slightly oblique course, accompanied by a characteristic medial spicule, and are not comminute (Fig. 5). Incomplete fractures, on the other hand, only affect one of the diaphyseal cortices, normally the lateral cortex, and, in pathological terms, they behave like a stress fracture and radiologically appear in the form of a radiolucent transverse line located on said cortical bone. Macroscopically, both types, complete and incomplete, associate a periosteal reaction and thickening of the lateral cortical bone at the level of the fracture focus (Fig. 5), both characteristics indicative of stress fracture. On occasion, cortical thickening is more generalized and affects both cortices.21
Clinically speaking, atypical fractures associated with the prolonged use of bisphosphonates are characterized by the fact that they are sometimes associated with different types of co-morbid situations (insufficiency-deficiency of vitamin D, hypophosphataemia, rheumatoid arthritis, etc.), and various types of pharmacological treatments (glucocorticoids, proton bomb inhibitors, other osteoporosis drug treatments, etc.). Moreover, they very often present with prodromal pain in the groin or thigh,21 requiring the exclusion of other possible causes of low energy fractures, such as pathological fractures related to primary or metastatic bone tumours, for a definitive diagnosis to be reached.
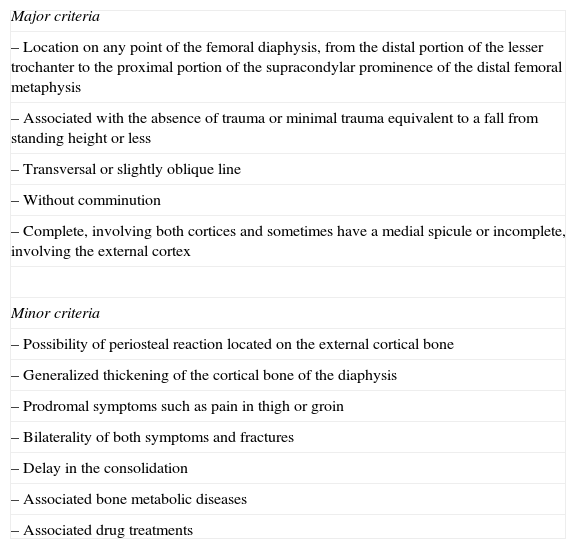
To facilitate the identification and typification of this type of fracture, a series of major and minor criteria have recently been established (Table 1).21 For a fracture to be classified as an atypical fracture associated with the prolonged use of bisphosphonates, it must meet all the major criteria. The minor criteria, although often associated with the fracture, may not present in all patients.
Atypical femoral fractures associated with the prolonged use of bisphosphonates.
| Major criteria |
| – Location on any point of the femoral diaphysis, from the distal portion of the lesser trochanter to the proximal portion of the supracondylar prominence of the distal femoral metaphysis |
| – Associated with the absence of trauma or minimal trauma equivalent to a fall from standing height or less |
| – Transversal or slightly oblique line |
| – Without comminution |
| – Complete, involving both cortices and sometimes have a medial spicule or incomplete, involving the external cortex |
| Minor criteria |
| – Possibility of periosteal reaction located on the external cortical bone |
| – Generalized thickening of the cortical bone of the diaphysis |
| – Prodromal symptoms such as pain in thigh or groin |
| – Bilaterality of both symptoms and fractures |
| – Delay in the consolidation |
| – Associated bone metabolic diseases |
| – Associated drug treatments |
At present, the overall incidence of subtrochanteric fractures of the femur is estimated to be low, accounting for 2–4% of all hip fractures.22 Three quarters of this type of fracture would normally be related with high-energy trauma, for instance, motor vehicle accidents.23 Their repercussion on morbi-mortality is similar to that of fractures of the proximal end of the femur, with mortality rates of 14% at 12 months and 25% at 24 months, and with functional repercussions that keep most patients (71%) from returning to basic activities of daily living in similar conditions to the ones they had prior to fracture.24
Upon closer examination of the epidemiology of subtrochanteric fractures due to insufficiency or stress occurring in a given bone metabolic conditions due to insufficient elastic–plastic resistance of the bone,25 we find a prevalence rate of close to 1% for this type of fracture.26
The incidence of subtrochanteric fractures in general appears to remain stable over time, with fewer than 30 cases per 100,000 inhabitants per year, in contrast to that of fractures of the femoral neck and pertrochanteric fracture that, in women, decreased in incidence from 600 to 400 cases per 100,000 inhabitants per year between 1996 and 2006.27 These data would confirm the fact that the incidence of osteoporotic hip fractures has fallen overall since the marketing of bisphosphonates, whereas the incidence of subtrochanteric and diaphyseal fractures has not varied.
Nevertheless, it must be remembered that the general incidence of subtrochanteric fractures remaining stable may obscure the presence of a greater number of atypical fractures, since, although the use of bisphosphonates might lower the number of “typical” osteoporotic fractures, their prolonged use might increase the number of atypical ones, offsetting in a sense, the final statistical outcome, above all considering that many epidemiological studies do not collect the distinctive radiological criteria of this type of fracture.28
It is estimated that approximately 25% (17–29%) of all subtrochanteric and diaphyseal fractures of the femur present characteristics that can allow them to be defined as atypical fractures associated with the prolonged use of bisphosphonates.29
More specifically, in the pivotal bisphosphonate studies, the risk of suffering a subtrochanteric or diaphyseal fracture of the femur has been established as 6 cases per 10,000 patients/year,20 a figure that falls significantly if the diagnosis is restricted to radiologically atypical subtrochanteric fractures. Thus, the general incidence of this possible complication of treatment with bisphosphonates might be estimated in 7.8 cases per 100,000 personas/year for individuals over the age of 60 years. Nevertheless, a recent study has demonstrated that this incidence of atypical femoral fractures increases with the time of exposure to the drug, going from 2 per 100,000 cases per year for every two years of use of bisphosphonates up to 78 per 100,000 cases per year for every 8 years of use of these drugs.30
Therefore, the incidence of atypical fractures associated with the prolonged use of bisphosphonates appears to be very low, both in head-to-head comparison with the number of subtrochanteric or diaphyseal fractures of the femur in general, as well as when indirectly related to the number of vertebral, non-vertebral, and hip fractures prevented by this drug class.21
Pathophysiology of the atypical fractures associated with bisphosphonatesAlthough the relation between bisphosphonates and atypical femoral fractures is consistent, a causal relation per se has yet to be demonstrated, with atypical femoral fractures being reported in patients not exposed to this type of drug.21
Nevertheless, in the vast majority of cases of atypical femoral fractures published, alendronate is the drug related to these fractures, although there are also case reports in people treated with pamidronate, risedronate, and zoledronate.7,18,31 Consequently, no conclusive relationship is considered to exist between alendronate and the increased risk of this type of fracture, but rather there is possibly a kind of “class effect” association for all bisphosphonates. It might be true that the higher affinity for osseous hydroxyapatite of the aminobisphosphonates in general, and alendronate in particular, might be reflected in a greater degree of absorption, greater anti-resorptive potency, and greater persistence of the drug in the bone,32 circumstances that would favour prolonged inhibition of bone remodelling over time.
For most authors, this would constitute the pathophysiological substrate underlying this association. The conspicuous, maintained suppression of bone remodelling that these anti-osteoporotic drugs produce would foster, on the one hand, the appearance of altered mineralization (increased mineral apposition with decreased mineral heterogeneity) and, consequently, an accumulation of microfractures that would increase the fragility of the bone, despite the increased bone mineral density. These microfractures would tend to be located in highly mineralized areas of the cortical bone33 and, hence, the subtrochanteric and diaphyseal areas of the femur would be especially susceptible to this type of fracture. Other possible pathophysiological alterations induced by bisphosphonates and that might also be associated with this type of atypical fracture would be the changes in the normal pattern of collagen fibre cross-linking and alterations in the proportions of collagen maturing induced by these drugs, as well as the reduction in local neovascularization due to the anti-angiogenic effect of bisphosphonates, a circumstance that accounts for the existence of less periosteal vascularization and, consequently, poorer repair response to the stress fracture.21
The striking inhibition of bone remodelling might also have an additive effect over time, especially if the bisphosphonates continue to accumulate in the bone tissue, which, pathophysiologically, might be highly relevant in the appearance of atypical femoral fractures. In this regard, various works have indicated that the accumulative effect of bisphosphonates, and as a result, the possibility of hypersuppression of bone remodelling, could occur after treatment periods of 5 or 7 years.19,29
Nevertheless, the data derived from the histological analyses published to date are not conclusive when establishing maintained bone remodelling inhibition as a single aetiopathogenic factor.19 In this sense, it must be pointed out that altered bone resorption has not been found in all patients with atypical fracture associated with the prolonged use of bisphosphonates,31 and that when post-fracture histological analyses have been performed on the subtrochanteric region, osteoclasts with normal morphological characteristics have been found,9 as well as normal trabecular structural patterns. Hence, some authors consider that this hypersuppression of bone remodelling does not have to be a direct consequence of prolonged treatment with bisphosphonates, but rather a pre-existing clinical condition, subsequently aggravated by said treatment.31
It is therefore considered that in this type of fracture, other general alterations must be involved—alterations associated with the maintained inhibition of bone remodelling and, in a multifactorial context, contributing to its appearance.
From a general perspective, the fact that many patients who have suffered this type of fracture associate a series of co-morbidities that have repercussions on normal bone metabolism, such as hyperparathyroidism secondary to vitamin D deficiency (which would increase bone resorption), diabetes mellitus (which would lead to an accumulation of advanced glycation end products, and hence, greater bone fragility and increased risk of fracture), steroid treatment (which would increase osteoclastic and decrease osteoblastic activity), proton bomb inhibitor treatment (per se associated with hip fracture) or multiple anti-resorptive therapy,21 means that it would be particularly useful to establish a series of sub-groups that are at high risk for suffering this type of fracture.20
Consequently, it can be concluded that, to date, the ultimate pathophysiological mechanism by means of which atypical fractures associated with the prolonged use of bisphosphonates are triggered remains unknown. These drugs are likely to play a role in the development of said fractures, although it is not possible that they are the sole trigger necessary for them to develop.
Diagnostic considerations of atypical fracturesWhereas osteoporotic fractures are, for the most part, secondary to a fall, atypical fractures sometimes occur spontaneously, preceded by minimal trauma or simply while walking.21 Atypical fractures affecting the femur, the ones most commonly reported, appear in the subtrochanteric region (≥5cm distal to the lesser trochanter) or in the femoral diaphysis.34,35 Nevertheless, atypical fractures have been reported in other less common locations such as the humerus, the sacrum, the ischium, the pubic branches, the tibia, and the metatarsals.17,18,36
From a clinical point of view, patients with atypical fractures associated with the prolonged use of bisphosphonates on occasion associate various types of co-morbid situations, such as vitamin D insufficiency-deficiency, hypophosphataemia, and rheumatoid arthritis and/or different types of drug treatments (glucocorticoids, proton bomb inhibitors, other anti-osteoporotic agents, etc.), with prodromal symptoms present in most cases, such as pain in the groin or thigh of varying duration and intensity, or weakness and discomfort attributable to other causes.22,37
When they occur, these fractures may be uni- or bilateral,21,38 complete or incomplete; in the case of complete fractures, they generally follow a transverse or slightly oblique course; they tend not to be comminute and present a characteristic medial spicule, normally with the distal fragment displaced superiorly and fracture angulation toward varus. In most cases, there is lateral cortical thickening that may be the only finding in the event of incomplete or radiologically relatively inexpressive fractures, a circumstance suggesting not only the presence of an alteration in the response to load transfer at that level but also that the process is chronic. Cortical thickening is sometimes more widespread and may affect both cortices.21
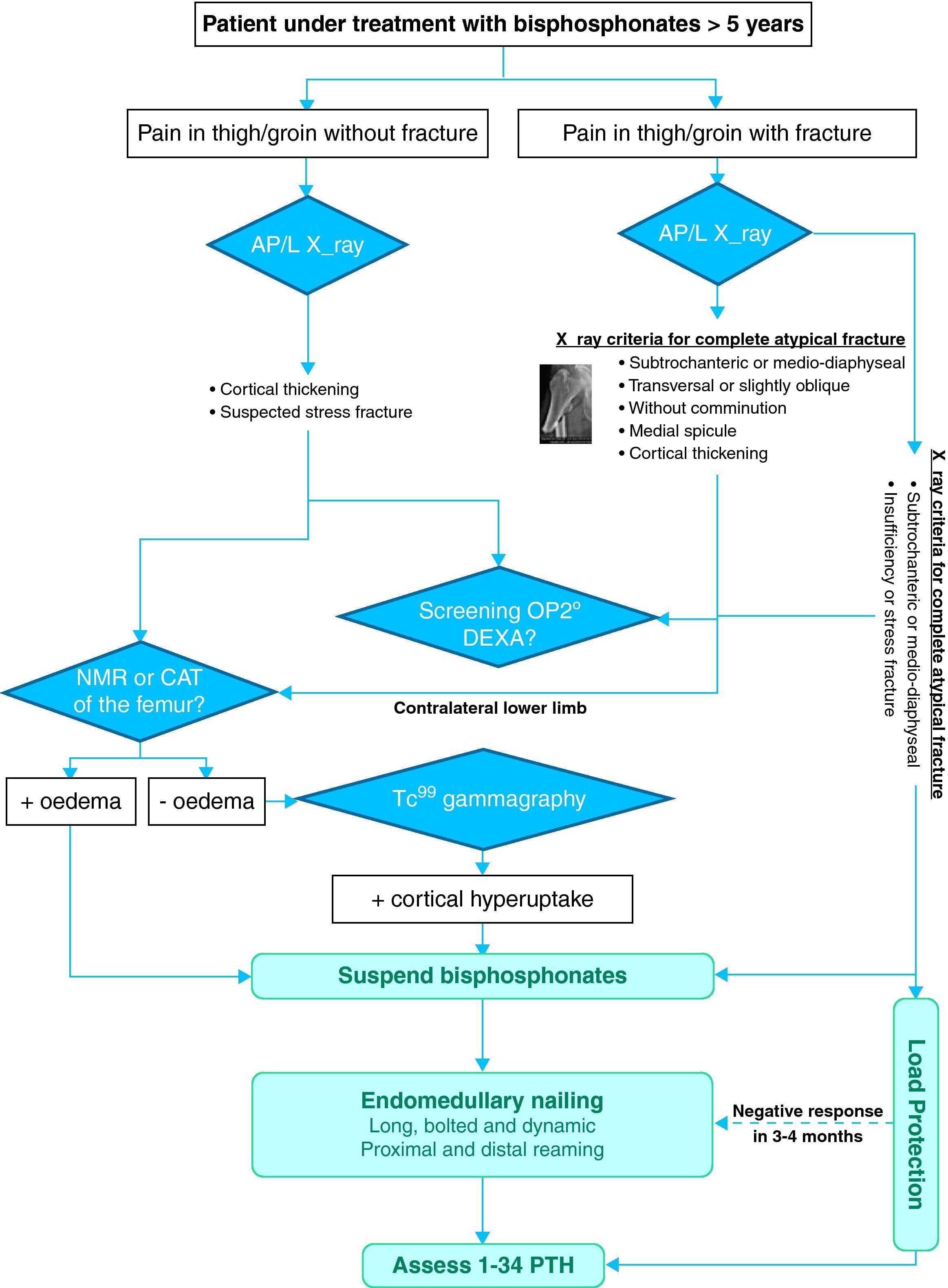
This increased cortical thickness should be considered predictive of an imminent atypical fracture,39 for which reason a simple AP/L X-ray of the contralateral femur that includes the entire diaphysis is recommended in the case of a unilateral atypical fracture. If this test is not wholly conclusive and there is a high degree of clinical suspicion, a CT, MRI, or gammagraphy of the contralateral femur would be indicated in search of predictive signs of the presence of fracture due to developing insufficiency or stress21,36 (Fig. 6). In these cases, CT scanning would make it possible to confirm focal cortical thickening, neoformation of periosteal bone and/or the presence of a faint radiolucent line indicative of focal intracortical resorption or a stress fracture in development.21 The MRI would typically reveal oedema in T1, reactive hyperaemia in T2, and neoformation of periosteal bone in the case that a fracture due to insufficiency or stress is developing.21 The gammagraphy would indicate a unilateral or bilateral area of diffuse enhanced uptake with a central area of maximum uptake, normally located on the lateral cortical, unlike primary or secondary infectious or tumoural pathologies of the bone that appear centred in the endomedullary space.21 Any of these three imaging techniques provide greater sensitivity and specificity than a simple X-ray for detecting the initial stages of insufficiency or stress fracture.21,31,32,40
Likewise, these tests would be indicated in the event that the patient presented prodromal symptoms with normal or doubtful X-rays21 (Fig. 6). In such cases, on occasion, DEXA images performed to monitor treatment enable the detection of periosteal bone neoformation indicative of a developing insufficiency or stress fracture.21
Treatment considerations of atypical fracturesAmong their characteristics, atypical fractures related to prolonged treatment with bisphosphonates present a certain tendency toward delayed consolidation (Table 1),21,33,36 which is why these fractures present a particularly high rate of morbidity. Hence, from a treatment perspective, it appears necessary to establish all medical and surgical procedures to decrease the possibility of this complication and foster its cure.
Considerations regarding surgical treatmentWhile it is true that there are as yet no controlled studies that have determined the type of surgical treatment to be applied in these fractures, a recent review21 suggests that, in the case of a complete subtrochanteric or femoral diaphyseal atypical fracture and due to the fact that bisphosphonates inhibit osteoclastic remodelling, the treatment used should foster healing by enchondral repair. In this type of fracture type, intramedullary nailing is therefore recommended with a long, reamed nail that protects the entire femoral diaphysis from re-fracture.21 Sliding screw plate-type devices, by not fostering enchondral repair and in the light of their high failure rate, would not be recommended as a method for osteosynthesis in this type of fracture.21
From a technical point of view, we believe it is extremely important for a correct initial reduction of the fracture to be guaranteed, often particularly difficult in the case of subtrochanteric fractures, due to both the muscle action as well as the course of the fracture itself. Correctly determining the point of entry for the nail and initiating the manual advance are likewise difficult given the strange hardness displayed by the bone. The endomedullary canal should be over-reamed by at least 2.5mm more than the nail's diameter, so as to avoid problems having to do with endosteal stenoses when present, to make it easier to insert the reconstruction nail, and to keep the diaphyseal remnant from fracturing.21 The proximal femoral fragment may require additional reaming to make it easier to insert the nail chosen and avoid poor alignment of the fracture.21
In the case of incomplete subtrochanteric or diaphyseal atypical fracture of the femur with pain in the thigh, prophylactic endomedullary nailing is advised.21 In those cases in which pain is minimal, it may be wise to try a prior period of conservative treatment, instructing the patient to have limited weight-bearing through the help of elbow crutches or a walking frame. Nevertheless, if reasonable clinical as well as radiological improvement is not seen after 2 or 3 months with this treatment, prophylactic endomedullary nailing is consistently recommended given that, in most cases, the fracture will evolve toward a complete fracture.21 In the remaining cases, protected weight-bearing and the reduction of physical activity should continue until the pain and bone oedema on the MRI disappear.21
As we have previously commented, in all cases of complete and incomplete atypical fractures, with or without symptoms, the contralateral femur should undergo imaging techniques for evaluation in search of indications of fracture due to development of an insufficiency or stress fracture21 (Fig. 6).
Likewise, no matter what type of atypical fracture it is and regardless of the surgical treatment chosen to manage it, the medical measures mentioned previously should always be established in order to foster healing and prevent, as far as possible, the appearance of complications that increase morbidity.
Considerations regarding medical treatmentFrom a medical perspective, we still have no controlled studies at the present time that define the strategies to follow for both the prevention and co-adjuvant treatment of atypical femoral fractures associated with the prolonged use of bisphosphonates.
The first thing to be considered if we are looking at the co-adjuvant treatment of atypical fractures from a medical perspective is the immediate discontinuation of anti-resorptive therapy in all patients presenting a complete or incomplete fracture or radiological images suggesting that an insufficiency or stress fracture is in the making.21 In addition to this treatment measure, a complete screening for secondary osteoporosis should be performed including phospho-calcium metabolism, with a special attention to vitamin D deficiency and its correction by means of appropriate supplementation. Due to the fact that, in some of the cases published, treatment with teriparatide (1-34 PTH) has been shown to improve fracture consolidation, reducing the risk of pseudoarthrosis, even in the absence of definitive scientific evidence to ratify such a decision, the administration of this drug would appear to be indicated in patients who have suffered this type of fracture, particularly when there is no evidence of radiological consolidation 4–6 weeks following surgery.21
With a view to the preventive treatment of atypical fractures, the first thing to be considered is, obviously that the decision on whether or not to begin treating osteoporosis with bisphosphonates should absolutely be made on a case-to-case basis and be founded on a proper evaluation of the risks/benefits entailed.
Once this is defined, the second thing to consider is the optimal duration of this intervention. Although it does appear clear that patients with osteoporosis being treated with bisphosphonates benefit from an important reduction in the risk of fracture for at least 5 years, the continued use of this treatment beyond this timepoint must be re-examined annually, using fracture risk rating scales, such as FRAX®, the patient's personal history of the appearance of fragility fractures, BMD evaluation (above all in the area of the hip) and/or the presence of underlying medical or pharmacological conditions affecting bone resistance.21 For those individuals in whom the risk of fracture continues to be moderately high, the continuation of treatment with bisphosphonates should be firmly considered. However, low-risk patients, in whom no recent fracture is seen or with densitometric osteoporosis (T score>−2.5) after the initial course of treatment, might benefit from a “treatment vacation” since, based on the cases and series of fractures published to date, the mean duration of treatment with bisphosphonates in patients with atypical fracture is 7 years. If the decision is made in favour of taking a temporary break from the medication, reinitiating anti-osteoporosis treatment with bisphosphonates or with a different drug class should be re-evaluated on the basis of the patient's clinical status, bone remodelling markers and BMD, considering the reintroduction of drug treatment in those patients at greater risk for fracture.21
Given that more than 50% of all patients with atypical femoral fractures associated with the prolonged use of bisphosphonates have suffered a prodrome of pain in the thigh or groin prior to the fracture, it is especially important to establish information measures targeting patients and physicians about this symptom. As previously commented, the presence of this type of prodrome would require an imaging study of both femurs in search of indications of fracture due to a developing insufficiency or stress fracture21 (Fig. 6).
Other considerationsAlthough the first alarm with respect to the influence that profound and prolonged suppression of bone remodelling induced by bisphosphonates might have on the mechanical resistance of bone was sounded by Ott in 2001,3 it was the work by Odvina et al. that truly called attention to the relationship between this pathophysiological alteration and the existence of a given type of subtrochanteric and medio-diaphyseal femoral fractures.4 Since then, there have been several isolated case reports and series taken from retrospective studies32,33,35,41 describing the clinical and radiological features of this type of fracture and its relation with the prolonged administration of aminobisphosphonates.
Setting aside the review of articles that merely offer case reports, we will briefly analyze the papers that we consider reflect and provide structural considerations, both pro and con, regarding said causal relationship.
Neviaser et al., in 2008, retrospectively analyzed the subtrochanteric and femoral diaphysis fractures produced by means of a low energy mechanism over a period of some 5 years and showed that 36% of these patients received prior therapy with alendronate and that 76% of them presented an atypical fracture pattern, with a simple horizontal course and a lateral peak in an area of cortical hypertrophy. The authors conclude that prolonged treatment with this drug might be related to the appearance of this type of fracture.41
One year later, Lenart et al. carried out a retrospective case–control study with the same cohort of patients from the Neviaser study, comparing them with patients who had suffered an intertrochanteric fracture or fracture of the femoral neck in the same period of time. The use of bisphosphonates was present in 15 of the 41 subtrochanteric fractures evaluated (37%) and in only 9 of the 82 patients who had suffered a pertrochanteric or femoral neck fracture (11%), for an odds ratio of 4.44 (CI 1.77–11.35). Ten of the 41 subtrochanteric fractures collected showed the characteristic atypical radiological pattern of a horizontal fracture course in the context of thickened cortical bone. Furthermore, the duration of the bisphosphonate therapy turned out to be significantly longer in the former group of fractures than in the latter. The authors conclude that in patients who take bisphosphonates, there is a greater percentage of low energy, subtrochanteric fractures than fractures in the pertrochanteric or femoral neck region.29
In 2010, Isaacs et al. published a comparative analysis of 100 patients with low energy fractures of the femoral diaphysis before and after the introduction of bisphosphonates (21 between 1995 and 1997 and 79 between 2007 and 2009). Of all these patients, those having fractures that could be considered as due to insufficiency were identified, and of these, the ones meeting those criteria received treatment with bisphosphonates, recording a total of 41 patients with fractures of these characteristics. Twenty-nine of these patients (71%) also exhibited painful prodromal symptoms and 18 (44%), bilateral fractures. The authors conclude that sustained therapy with bisphosphonates is associated with this type of insufficiency fracture.42
Park-Wyllie et al., in a very recently published work analyzing a cohort of 9723 women over the age of 68 years who initiated treatment with bisphosphonates between 2002 and 2008 establish that treatment with these drugs for more than 5 years effectively increases the risk of suffering an atypical subtrochanteric fracture or fracture of the femoral diaphysis, although the absolute risk is low. In the light of these results, the authors propose the need to establish the individual risk of atypical fracture for each patient, and bearing this risk in mind, reconsider or withdraw treatment (treatment vacation) in those patients in whom the risk of suffering an osteoporotic-type fracture is low.43
However, in contrast to these works in favour of the causal relation between the prolonged administration of bisphosphonates and atypical fractures, some well-structured scientific papers have recently appeared that do not make it possible to faithfully establish said association.
Thus, Abrahamsen et al., in a review of a large Danish cohort, point out that only 7% of the patients with fractures considered to be atypical were being treated with alendronate, the same percentage presented by patients who had suffered an osteoporotic hip fracture, concluding that this type of fracture can be considered as a mere consequence of the osteoporotic pathology and not as a complication stricto sensu of therapy with bisphosphonates.44
The same authors, in a recently published subsequent review,45 investigated the risk of suffering a subtrochanteric fracture or fracture of the femoral diaphysis in women who were on treatment with alendronate versus a control group, as well as evaluating the total time of treatment-accumulated doses and their relation with this type of fracture. In contrast to the 13 fractures per 10.000 patients/year in the group of untreated women, there were 31 fractures per 10.000 patients/year in the group of women who had received treatment, with a similar risk for those who had received treatment for a longer period of time (up to 9 years) as for those who had received a lower accumulated dose. Therefore, considering these results and slightly qualifying what has previously been published, they conclude that the risk of subtrochanteric fracture or fracture of the femoral diaphysis is greater in patients treated with bisphosphonates, but unrelated to the duration of therapy, thereby establishing that the most likely origin of this type of fracture lies in the osteoporosis itself more than in the treatment with these drugs.
Also very recently, Black et al., in a pooled post hoc analysis of the FIT, FLEX, and HORIZON clinical trials conclude that even after 10 years, the incidence of subtrochanteric fractures or fractures of the femoral diaphysis that can be associated to prolonged treatment with bisphosphonates is very low and did not observe a significant increase in the relative risk in any of the three studies. The authors therefore consider that there is no significant increase in the risk of suffering this type of fracture in these patients.20
In a systematic review of the main case series published in the literature, Giusti et al. conclude that although bisphosphonate therapy is present in the majority of the cases, it is not an indispensable circumstance for the development of this type of fracture; other conditions, such as steroid therapy or treatment with proton bomb inhibitors, are probably involved. These results lead the authors to conclude that, based on these factors, certain patients may have a special predisposition to develop this type of fracture, determinants that must be identified in the future by means of well-designed prospective studies.19
The outstanding review by the American Society for Bone and Mineral Research (ASBMR) task force, under the leadership of Elizabeth Shane,21 establishes that, on the basis of the data available to date, the incidence of this type of fracture can be considered very low, particularly with regards to the amount of osteoporotic fractures prevented with this kind of treatment. It also acknowledges the impossibility of establishing a causal relationship between bisphosphonates and atypical fractures, although it does point out that the risk of developing this type of fracture increases as exposure to the drug increases, appealing to the need for research models that determine the true scope of this pathology and the possible relationship between these fractures and prolonged treatment with these drugs.
In another recently published and very interesting review by the European Society on Clinical and Economic Aspects of Osteoporosis and Osteoarthritis (ESCEO) and the International Osteoporosis Foundation (IOF),46 the evidence of the relationship that exists between atypical fractures and the prolonged use of bisphosphonates is reviewed. In this review, although it acknowledges the existence of a relationship, not irrefutably demonstrated, with the prolonged use of alendronate that as yet, cannot be extrapolated to other bisphosphonates, it also establishes that the risk of atypical fracture–benefit relationship in protection against osteoporotic fracture is favourable to the use of these drugs, since the fractures that are avoided are far superior to those that could theoretically result from the continuous use of these drugs for more than 5 years.
ConclusionsDespite the fact that a very low incidence of atypical subtrochanteric fractures or diaphyseal fractures of the femur can be extrapolated from the leading studies of long-term follow-up with bisphosphonates and that very few case reports or reviews can be found in the literature published in this regard to prove a greater risk of this type of fracture among people taking this medication, the appearance of such fractures has undoubtedly generated a fair degree of alarm among health-care professionals dedicated to this type of pathology.
Consequently, bodies such as the ASBMR, ESCEO, or the IOF itself, in their consensus statements regarding atypical fractures associated with prolonged treatment with bisphosphonates21,44 consider that, while a clear, causal relation with bisphosphonate therapy cannot be established, further in-depth epidemiological research and more, well-designed studies are needed to characterize and define clearly the pathophysiology of this type of fracture, so as to be able to establish both its importance and all the risk factors that might be associated with these fractures.
In this same sense, although it is true that the suppression of bone remodelling brought about by prolonged treatment with bisphosphonates could have a certain influence on the appearance of atypical fractures in patients with prepathological bone condition that has not been clearly established and that probably coincides with that of patients at high risk for suffering osteoporotic fractures in general, we must not lose sight of the benefits that this treatment brings to patients with osteoporosis.
Therefore, and as a final recap, we, at the GEIOS group, would like to present a series of possible reflections and considerations regarding atypical fractures associated with the prolonged treatment with bisphosphonates.
Bisphosphonates are anti-osteoporosis drugs that are highly efficacious in preventing vertebral and non-vertebral fractures, including hip fractures. They are considered to be safe drugs with scant incidence of adverse effects.
The incidence of atypical fractures in patients treated with bisphosphonates is extremely low and does not affect the risk/benefit ratio of these drugs.
A causal relation cannot be established between prolonged treatment with bisphosphonates and the appearance of atypical fractures; these drugs probably play a role in the development of these fractures, but it is not possible for this type of therapy to be the only condition needed for their development.
The incidence of atypical femoral fractures increases as does the time of exposure to bisphosphonates. The mean duration of treatment with bisphosphonates in the patients with atypical femoral fracture is 7 years.
Atypical fractures associated with prolonged treatment with bisphosphonates may be uni- or bilateral, complete or incomplete. Radiologically, they are characterized by the display of a course that is usually transversal or slightly oblique, non-comminute, and with the formation of a characteristic medial spicule. Lateral cortical thickening can be observed in most cases. Among their features, they are prone to delayed consolidation.
When facing a patient with prolonged treatment with bisphosphonates who reports continuous pain in the groin or in the thigh and in all cases of complete and incomplete, unilateral, atypical fracture, whether they present symptoms or not, a simple, AP/L X-ray of the contralateral femur is recommended, including the entire diaphysis. If this test is not totally conclusive and the level of clinical suspicion is high, a CT, MRI, or gammagraphy should be performed on the contralateral femur in search of signs predicting for the presence of a developing insufficiency or stress fracture.
Complete atypical, subtrochanteric or diaphyseal femoral fractures require efficacious osteosynthesis by means of intramedullary nailing with a long, reamed nail that protects the entire femoral diaphysis from re-fracturing. In incomplete atypical fractures with pain in the thigh, above all if they have not responded to conservative treatment, prophylactic endomedullary nailing might be advisable.
Immediate supression of bisphosphonate treatment in all those patients with complete or incomplete fracture or radiological images that suggest a developing insufficiency or stress fracture, must be carried out.
Even in the absence of definitive scientific evidence to corroborate it, the administration of teriparatide (1-34 PTH) in patients who have suffered this type of fracture appears to be indicated, particularly when there is no evidence of radiological consolidation by 4–6 weeks following surgery.
Well-designed, prospective studies are needed to determine the true risk of suffering this type of fracture and its possible relationship with this treatment. Specific diagnostic codes must be created to facilitate their recording, promote their study, and to establish appropriate medical-surgical management.
At the present time, according to the bibliography available, bisphosphonates continue to be the standard of care for osteoporosis; hence, there are no grounds for alarm to justify their non-prescription or withdrawal for this cause in patients with osteoporosis or osteoporotic fracture.
The decision as to whether to initiate osteoporosis treatment with bisphosphonates must be strictly individualized and based on a proper evaluation of the risk/benefit ratio entailed. Though it appears clear that patients with osteoporosis on treatment with bisphosphonates benefit from an important reduction in their risk of fracture for at least 5 years, the continued use of this treatment beyond that should be re-evaluated yearly. For those patients in whom the risk of fracture continues to be moderately high, continued treatment with bisphosphonates should be seriously considered. However, low risk patients, without any recent fracture or densitometric osteoporosis (T score>−2.5) after the initial course of treatment might benefit from “treatment vacation”.
Level of evidenceExpert opinion. Level of evidence V.
Protection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of dataThe authors declare that they have followed the protocols of their work centre on the publication of patient data and that all the patients included in the study have received sufficient information and have given their informed consent in writing to participate in that study.
Right to privacy and informed consentThe authors must have obtained the informed consent of the patients and/or subjects mentioned in the article. The author for correspondence must be in possession of this document.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Caeiro-Rey JR, et al. Fracturas atípicas relacionadas con el uso prolongado de bifosfonatos. Estado de la situación. Rev esp cir ortop traumatol. 2011;55(5)392–404.