Complications related to anterior cruciate ligament (ACL) graft are common. Change in height, especially patella baja, can be a cause of anterior knee pain. Several studies have related ACL reconstruction with bone-tendon-bone graft to patella baja.
MethodsForty-three patients with ACL reconstruction using a with bone-tendon-bone graft were included in this study. All patients underwent the same surgery, with closure of the paratenon of the patellar tendon. A radiological study was performed before surgery and 2 years after surgery. The Insall-Salvati index, axial view and patellar tilt were analysed in all patients. The healthy contralateral knees were used as the control group.
ResultsNo significant differences were observed from the preoperative measurements or at the 2-year follow-up.
ConclusionsThe use of patellar tendon with closure of the paratenon in ACL reconstruction was not shown to modify patellar height within the radiological follow-up of two years.
Las complicaciones asociadas al uso de injertos del ligamento cruzado anterior (LCA) son frecuentes. Los cambios en la altura, sobre todo de la patela baja, pueden ser la razón de la aparición de dolor en la zona anterior de la rodilla. Diversos estudios han asociado la reconstrucción del LCA mediante la técnica de injerto hueso-tendón-hueso con patela baja.
MétodosCuarenta y tres pacientes con reconstrucción del LCA mediante injerto hueso-tendón-hueso fueron incluidos en el presente estudio. Todos los pacientes fueron sometidos a la misma cirugía, con el cierre del paratendón del tendón rotuliano. Se realizó un estudio radiológico antes de la cirugía y 2 años después de la misma. En todos los casos se estudió el índice Insall-Salvati, el corte axial y la inclinación patelar. Como control se utilizó la rodilla sana contralateral del paciente.
ResultadosNo se encontraron diferencias significativas entre el estudio preoperatorio y el realizado tras 2 años de la cirugía.
ConclusionesEl uso del tendón patelar con cierre del paratendón en la reconstrucción del LCA no ha demostrado modificar la altura patelar en estudios radiológicos a los 2 años de seguimiento.
Central third bone-tendon-bone (BTB) (patellar tendon graft), is one of the most commonly used grafts in the world.3 Since it was first described by Jones in 1963, several authors have considered this graft the gold standard.3–6 The BTB donor site can suffer various complications, such as anterior knee pain with a frequency ranging from 6% to 40%, according to previous studies.7 Radiological studies of the donor site have occasionally associated the use of BTB with the onset of patella infera,8–10 and thus associated with anterior knee pain.9
Other situations such as fracture of the patella, patellar tendon rupture, joint stiffness, and arthrofibrosis have been widely associated by various authors with patella baja syndrome.11–14 Patella infera is characterised by permanent shortening of the patellar ligament and is associated with limited articular balance at the level of the knee. It is associated with patellar tendon shortening, soft tissue contractures, quadriceps weakness, restriction of joint motion and femoropatellar incongruence. Patella baja is a multifactorial complication that can be induced acutely through trauma to the knee, iatrogenically in ligamentoplasties, osteotomies and arthroplasties, or can be chronic, secondary to inflammatory processes of the knee.1
Patella baja has been associated with knee pain after this operation, as well as the use of this graft, indicating that closure of the patellar tendon after removal of the graft might induce patella baja.7,15
This paper aims to assess whether reconstruction of the anterior cruciate ligament (ACL) with a patellar tendon graft and closure of the paratenon change the height of the patellar tendon, and thus we aim to highlight this as a possible cause of anterior knee pain. We hypothesise that paratenon defect and closure can cause a change at the height of the patella that induces patella infera.
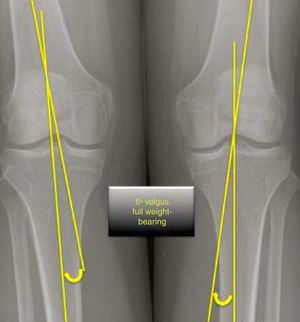
Materials and methodsA consecutive series of patients with complete ACL rupture were studied prospectively that underwent surgical reconstruction in our centre, using BTB autograft, between January and December 2009. A radiological study was performed before the surgery and at the 2 months postoperative follow-up, including weight-bearing anteroposterior and lateral X-rays, at 45° flexion, and axial view of both knees at 30°.
The contralateral knee was used as the control, in the same times as the operated knees. All the patients agreed to participate in the study and we sought the approval of the Ethics Committee with file number 09/45.
The inclusion criteria were to be aged over 18 years, having a primary ACL rupture and having undergone reconstruction with a patellar tendon graft. The exclusion criteria included having undergone prior surgery to the injured knee, prior ACL injury and patients who had not completed radiological follow-up preoperatively or at 2 years after the operation.
The surgery was performed under spinal anaesthesia and a preventive ischaemic tourniquet was used. First an arthroscopic revision of the knee was undertaken to confirm rupture of the ACL. Then the patellar graft was harvested from the central third of the patellar tendon, with bone blocks 25mm in length and 9mm thick (the patellar and the tibial blocks were the same). The grafts were of a constant size regardless of the anatomy of the subject. The ACL reconstruction was performed using the anatomical single bundle technique. The donor site was closed by suturing the paratenon with single sutures of absorbable material (Vycril 1) with the knee in extension or slight flexion of less than 20°. In no case was the defect filled. All the patients followed the same standard physiotherapy for the anterior cruciate ligament and the same subsequent follow-up protocol.
Radiological studies were performed before the surgery by analogue: lateral X-ray at 45° of flexion (bilateral) non weight-bearing, and a further study at 2 years follow-up, and an axial view of the patella to measure the distance between the edge of the patella and the femur of both sides to assess the degree of subluxation.
The data were gathered prospectively through an observational study in relation to the radiological variable.
Hypotheses/calculationsIn order to calculate the sample size, a group of 40 patients were selected to detect with 80% power and an odds ratio of 3.5, using the Chi-square test and an estimation of 5% to achieve statistical significance. Ten percent of patients were added since the patients were chosen taking possible losses to follow-up into account. In the end, only one patient was excluded from the study for failing to complete the subsequent follow up (due to a change of address). The study was completed with 43 patients.
All the patients were diagnosed, operated and followed up by the same surgeon.
The radiological study was performed before and 2 years after the surgery with lateral radiographs of both knees at 45° femorotibial flexion. The radiological measurements were performed manually by 2 independent surgeons using a graduated ruler.
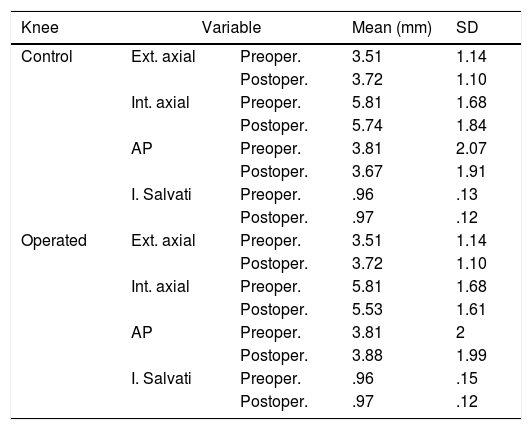
The radiological results of the measurements before and 2 years after the surgery were compared to validate the measurements. The statistical analysis was performed with descriptive analysis (Table 1). The concordance correlation coefficient and the total deviation index were estimated to confirm the reliability of the measurements, as shown in Table 2.
Description of control measurements and operated knees.
| Knee | Variable | Mean (mm) | SD | |
|---|---|---|---|---|
| Control | Ext. axial | Preoper. | 3.51 | 1.14 |
| Postoper. | 3.72 | 1.10 | ||
| Int. axial | Preoper. | 5.81 | 1.68 | |
| Postoper. | 5.74 | 1.84 | ||
| AP | Preoper. | 3.81 | 2.07 | |
| Postoper. | 3.67 | 1.91 | ||
| I. Salvati | Preoper. | .96 | .13 | |
| Postoper. | .97 | .12 | ||
| Operated | Ext. axial | Preoper. | 3.51 | 1.14 |
| Postoper. | 3.72 | 1.10 | ||
| Int. axial | Preoper. | 5.81 | 1.68 | |
| Postoper. | 5.53 | 1.61 | ||
| AP | Preoper. | 3.81 | 2 | |
| Postoper. | 3.88 | 1.99 | ||
| I. Salvati | Preoper. | .96 | .15 | |
| Postoper. | .97 | .12 | ||
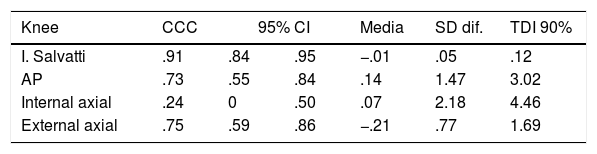
Concordance correlation coefficient (CCC) and confidence interval (95% CI) between preoperative and postoperative values. Mean difference and standard deviation, as well as the total deviation index (TDI 90%) that represents the lowest values where 90% of the differences between preoperative and postoperative knees are included.
| Knee | CCC | 95% CI | Media | SD dif. | TDI 90% | |
|---|---|---|---|---|---|---|
| I. Salvatti | .91 | .84 | .95 | −.01 | .05 | .12 |
| AP | .73 | .55 | .84 | .14 | 1.47 | 3.02 |
| Internal axial | .24 | 0 | .50 | .07 | 2.18 | 4.46 |
| External axial | .75 | .59 | .86 | −.21 | .77 | 1.69 |
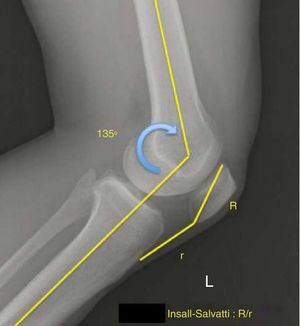
The measurements of each patient's control knee were used for this analysis. The study focused on evaluating the differences between the measurements obtained preoperatively and those obtained postoperatively. Figs. 1–3 show the different measurements performed. The preoperative Insall-Salvati index was used to compare with the contralateral knee. Then, the variation of the Insall-Salvati index was studied comparing the postoperative results.
The intervariable consistency was the first parameter studied to validate our measurements, using the preoperative and postoperative variables of the healthy knee.
Both the estimation of the concordance correlation coefficient (=.91) and the lower limit of its CI (.84) showed a high degree of concordance between the preoperative and postoperative values for the Insall-Salvati variable. We estimate that 90% of the differences are less than .12 (total deviation index=.12).
Thus, we can see that the Insall-Salvati ratio is a highly reliable measure. The Student's t-test for independent variables was used to measure the preoperative Insall-Salvati ratio compared to the contralateral knee, obtaining a p>.05, concluding that there were no significant differences before the surgery.
Then, the variation of the Insall-Salvati ration before and after the surgery was compared with the Student's t-test for paired samples. The p>.05, therefore we can conclude that there were no significant differences measured using the Insall-salvati index between the preoperative and the postoperative periods.
DiscussionThis study found no significant differences in the Insall-Salvati indices between the operated knees compared to their unoperated contralateral knees, in line with previous studies.15 However, there are other studies that have confirmed a change in the position of the patella.16
The postoperative onset of patella baja after closure of the patellar tendon has been associated with removal of the BTB graft,16 although there are other publications where no differences have been demonstrated comparing groups where the ligament defect was sutured with others where it was not closed.
This study has the limitation of being retrospective and therefore the level of scientific evidence is limited, although it might be useful to generate hypotheses for further studies that confirm the hypothesis we put forward in this paper. Furthermore, there was no control group to compare, although to resolve this issue we took the other knee as the control which we found useful to evaluate the intrapersonal differences.
Wang et al.10 described changes in patellar length in relation to radiological studies. However, both patella alta and baja were observed with no clear relationship with pain symptoms.
In a previous study by Mast et al.3 patients who had undergone patellar tendon surgery were followed up for 2 years, and had no anterior knee pain. They found that their clinical assessments were identical in both knees and that the radiological and ultrasound studies showed no significant differences, other than a 10% increase in the thickness of the operated tendon.17
Tria et al.22 observed that using the central middle of the patellar tendon could induce patella infera. These radiological findings also correlated with increased femoropatellar pain. Krosser et al.12 compared 2 groups of patients, half had a closed tendon defect, whereas it had been left open in the rest (only closing the paratenon).18 The authors found a non-significant tendency towards shortening of patellar tendon length in the first group.18
In our study we did not observe this fact that was detailed in the previous study. The radiological indices showed no postoperative variation (2 years after surgery) in patellar height. On the same lines, the study group of Adriani et al. observed no changes between groups after closing the donor site defect.9
Another study demonstrated that patients with ACL injuries had a higher rate of patella baja which was considered a risk factor for rupture of ACL plasty. The authors recommend not using patellar tendon when these 2 factors are present. In this study, the patients showed no symptoms of patella baja, either postoperatively or preoperatively.
Several authors have highlighted that the donor site should be closed by closing the paratenon instead of the tendon directly to prevent possible changes to the height of the patella.19
Hantes et al.6 compared the length of the patellar donor site in patients with BTB or hamstring grafts.20 They found no significant differences in terms of patella baja or anterior knee pain. A different study group compared 2 groups of 40 patients with and without patellar closure and found no significant differences in patellar height.
The study group of Shelbourne et al.14 found no variation in patellar tendon height in their series, and started early rehabilitation therapy.21
Muellner et al.20 observed an important tendency towards shortening in women that concluded after 6 months. The same study observed that ACL surgery using BTB graft caused significant changes in the patellofemoral angle, which might lead to problems of femoropatellar alignment, and therefore femoropatellar pain.9 Along the same lines, other authors have found that using the BTB autograft shortens the length of the remaining patellar tendon by an average of 1.6mm.8 However, this shortening is does not reflect any clinical result without greater pain or functional variation.
In this study we observed no significant changes in patellar height (measured using the Insall-Salvati index), with no evidence of significant differences among the groups studied (before/after surgery). Therefore, the technique used did not alter the patellar height or regeneration of the donor site.
With respect to the studies that indicate that anterior knee pain might be associated with patellar height, we can conclude in our series that there were no significant differences in height and therefore anterior knee pain would not be associated with patellar height.
The progress of donor site regeneration has been studied by various authors. Moebius et al.16 observed that their donor sites had regenerated at 30 months postoperatively, although some patients did not achieve full regeneration.22 Patellar height reduced less than 10% compared to the healthy contra lateral knee.
A study by Wang et al.10 concluded that 9.1% of patients had significant patellar height shortening.23 Franck et al.15 conducted a systematic review of 4 randomised clinical trials where they observed no significant differences in the results in patients who had undergone ligamentoplasties with BTB compared to patellar tendon closure in the donor site.
In our study, as mentioned in the previous study, no significant evidence was found that would imply a variation in patellar height after ligamentoplasty with BTB.
ConclusionThe use of the patellar tendon with closure of the paratenon in ACL reconstruction was not demonstrated to modify patellar height in radiological studies at 2 years’ follow-up.
Level of evidenceLevel of evidence III.
Ethical responsibilitiesProtection of people and animalsThe authors declare that no experiments were performed on humans or animals for this study.
Data confidentialityThe authors declare that they have followed the protocols of their centre of work regarding the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestsThe authors have no conflict of interests to declare and have not received funding of any type.
Please cite this article as: Seijas R, Sallent A, Pons A, Cusco X, Catala J, Cugat R, et al. Modificaciones en la altura patelar por el uso del injerto hueso-tendón-hueso. Rev Esp Cir Ortop Traumatol. 2018;62:337–342.