Radial head fractures represent 33–75% of elbow fractures (30 cases/100,000 population/year). "Terrible Triad’s Hotchkiss" is characterised by radial head fracture, coronoid fracture and elbow dislocation. Our principal goal is to compare our results on each type of prosthesis in the context of the triad.
Material and methodsWe conducted an observational, descriptive and retrospective study. Sample size was 47 patients. Variables analysed were affiliation, Mason’s classification, surgical aspects (moment of surgery, surgical time, prosthesis type, re-surgery), rehabilitation time, causes of prosthetic failure, complications, radiographic findings (according to Van Riet), Popovic’s loosening areas, M.E.P.S. and Cassebaum’s scales. We performed an inter-group study, on patients treated with monopolar or bipolar prosthesis, in order to see results.
ResultsAverage age was 43.5±8.9 years. 72.7% were in highly demanding jobs. Mason’s fracture type IV appeared in all the cases and Regan-Morrey’s type I was the most frequent coronoid fracture (42.6%). There were 22 bipolar prosthesis and 25 monopolar prosthesis. Surgery time was about 112.3±59.1min. External fixation was used in 6.4%. M.E.P.S. final: 85.9±15 points. Rehabilitation time was about 4.7±2.5 months. Of the patients, 76.6% returned to work. Cassebaum’s results were good-excellent in 74.5% of patients. There were 3 cases of prosthetic mobilization. Heterotopic ossification appeared in 29.8% of cases and 15.2% presented overstuffing. With regard to the inter-group study, we observed that there was less surgical time with monopolar prosthesis (p=.006), fewer second look surgeries (p=.05), less stiffness (p=.04), less heterotopic ossification (p=.004) and septic loosening (p=.005), without any influence on M.E.P.S. (p=.44).
ConclusionsResults obtained in terrible triads with prostheses in our experience are good. Prosthetic type influences results, because surgical time for implantation of a monopolar prosthesis was less than for a bipolar one, although rehabilitation time was longer. With bipolar prostheses, external fixation was required, with a higher rate of reinterventions, stiffness, prosthetic mobilization, heterotopic ossification and prosthetic loosening. However, there were no differences between the two prosthetic types in terms of clinical results, like M.E.P.S. or Cassebaum scores.
Las fracturas de cabeza radial representan el 33-75% de las fracturas del codo (30 casos/100000 habitantes/año). La “Triada terrible de Hotchkiss” se caracteriza por fractura de cúpula radial, coronoides y luxación del codo. Nuestro objetivo principal es comparar los resultados según el tipo de prótesis utilizada en el contexto de la tríada.
Material y métodosEstudio observacional, descriptivo y retrospectivo. Tamaño muestral de 47 pacientes. Variables analizadas: filiación, clasificación de Mason, aspectos quirúrgicos (demora, tiempo quirúrgico, tipo de prótesis, reintervenciones), tiempo rehabilitador, causas de fracaso protésico, complicaciones, hallazgos radiológicos (según Van-Riet), zonas de aflojamiento (Popovic), escalas M.E.P.S. y Cassebaum. Se realizó un estudio intergrupal entre los tipos protésicos monopolar y bipolar, para ver los resultados obtenidos.
ResultadosEdad media:43,5±8,9 años. 72,7% de profesionales de grandes esfuerzos. La fractura Mason IV apareció en todos los casos y la tipo I de Regan Morrey para coronoides (42.6%. 22 prótesis bipolares y 25 prótesis monopolares. Tiempo de intervención: 112,3±59,1minutos. Fijación externa en el 6,4%. M.E.P.S. final: 85,9±15 puntos. Tiempo rehabilitador: 4,7±2,5 meses. Alta por mejoría: 76,6%. Cassebaum bueno-excelente en el 74,5%. Hubo 3 casos de movilización protésica, 29,8% de osificaciones heterotópicas y sobredimensionado en el 15,2%. En el estudio intergrupal, objetivamos que con prótesis monopolares hubo menor tiempo quirúrgico (p=0,006), menores reintervenciones (p=0.,05), menor rigidez (p=0,04), osificación heterotópica (p=0,004) o aflojamiento protésico (p=0,005), sin influir en escala M.E.P.S. (p=0,44).
ConclusionesLos resultados obtenidos en tríadas terribles con prótesis en nuestra experiencia son favorables. El tipo protésico sí influye, ya que el tiempo quirúrgico para la implantación de una prótesis monopolar fue menor, aunque el tiempo de rehabilitación fue algo mayor. Con las prótesis bipolares se requirió más la fijación externa, siendo también mayor la tasa de reintervenciones, rigidez, movilización protésica, osificación heterotópica y aflojamiento protésico. Sin embargo, no hubo diferencias entre ambos tipos protésicos en cuanto a resultados clínicos, ya fuera M.E.P.S., o Cassebaum.
Hotchkiss’ terrible triad1,2 is characterised by dislocation of the elbow, with radial head fracture and coronoid fracture. The elbow is the second most dislocated joint in the body, with a rate of 6–8 cases per 100,000 inhabitants.3 Out of these cases, 18%–45% would be terrible triads.1
Among the damaged elements, there are several points of interest. On the one hand, the lateral collateral ligament complex (LCL) and the medial collateral ligament complex.4 On the other, the coronoids, since over 30° of flexion would be restricted by posterior instability.5,6 Their fractures have been classified according to Regan and Morrey7 or O´Driscoll et al.8 Up to 50% of the coronoids are needed to preserve humeral and ulnar stability.
Finally, fractures of the radial head, classified according toMason,9 but modified by Johnston,10 occur with a frequency of 33%-75%11 in elbow fractures although this radial head would support 40% of remaining stability in the proximal radius ulnar joint. Treatment of triads with radial head prostheses have had favourable results between 76% and 94% of cases with long term follow-up, despite capitellar wear and osteoarthritis (74% long term6).
Surgical treatment of this injury has improved mobility of the patients12 and achieved good clinical results,13 on clinical scales, such as the Mayo Elbow Performance Score (MEPS).14 However, treatment of this type of injury is not free from complications, including instability 16 in up to 22%,15 radial ulnar synostosis and osteoarthritis. A review of this pathology would therefore be useful to analyse the results obtained from our experience and assess possible differences in results, depending on the type of prosthesis used.
Our main objective were therefore to compare results according to the type of prosthesis used in the context of the triad. Our working hypothesis was that the cases treated with monopolar prostheses presented with less time in surgery and a lower rate of complications than the cases treated with bipolar prostheses.
Material and methodsProcedureThe procedure used was the development of an observational, descriptive and retrospective study, with a sample size of 47 patients. The level of evidence was type iv. Follow-up time was a median of 25.5 months, with minimum of 2 years and a maximum of 10 years.
Inclusion criteriaPatients aged between 18 and 65 years, who after trauma presented with dislocation of the elbow, with radial head and coronoid fractures, within the context of the terrible triad of the elbow. All cases had to have been treated with radial head arthroplasty, as the radial head was not able to be reconstructed. Radiographic and CAT scan studies were performed prior to surgery on all patients.
Exclusion criteriaPatients in a similar age range of between 18 and 65 years, with terrible triads of the elbow, where the radial head was synthsizable with pins. Patients with elbow dislocation, radial head fracture and coronoid compromise, with extension of the latter to the olecranon, to fracturing it (suspicion of transolecranon dislocation).
Protocol of terrible triad of the elbow managementOur protocol of action for this injury was to perform a previous radiographic study, reduction under general anaesthesia and posterior preoperative planning using a three-dimensional reconstruction CAT scan. With regards to surgical treatment, we follow that proposed by Mathew et al.,17 based on Hotchkiss and Weiland.2 Our approach to the lesion is posterior, from where we access the lateral region of the elbow. If the radial head is not synthesizable, we have to perform an osteotomy, giving us access to treat the coronoids and then continue with repair from inside to out, replacing the radial head with a prosthesis and finally repairing the lateral collateral ligament complex. In this case, if the elbow was not stable, we would be required to review the medial collateral ligament as well and if instability persisted, apply external fixation. If the radial head could be repaired with osteosynthesis, we would have to assess whether the coronoids were accessible from the lateral approach. If not, we would proceed with a medial approach, to repair the coronoids, and to repair the medial ligaments, to later treat the radial head and finally repair the lateral ligaments. If after this the elbow continued to be unstable, it would require external fixation. Our postoperative treatment protocol would be immobilisation for 3 weeks, with a plaster and then from week three onwards begin physiotherapy.
PatientsIn the 47 patient sample analysed, mean age was 43.5±8.9 years, with all affected cases being males. Direct trauma occurred in all cases. 72.7% of the patients belonged to groups of professions which required major strength for undertaking their jobs (mechanics, installation assemblers, etc.) compared with 27.3% of professionals with lower requirements for strength (administrative staff, couriers, etc.) Injury distribution was 48.9% right and 51.1% left elbows.
The frequency of radial head injuries according to the classification by Mason9 and Johnston10 was 100% for type IV. The distribution of coronoid apophysis according to the classification by Regan y Morrey7 was: type III fractures: 20 cases (42.6%), type II fractures: 25 cases (53.2%) and type III fractures: 2 cases (4.2%).
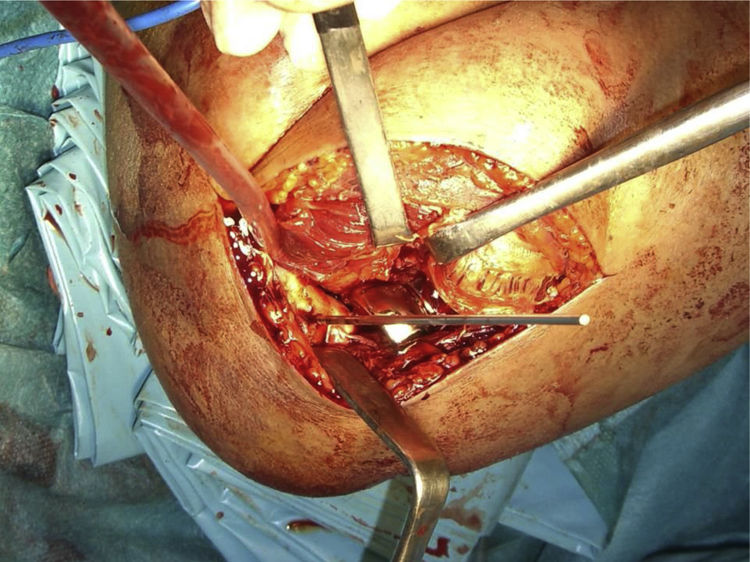
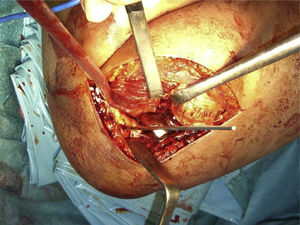
Surgical procedureWith regard to surgical procedure, waiting time was less than one week in 44.7% of cases, from 1 to 4 weeks in 48.9% of cases and more than 4 weeks in 6.4% of cases. Time in surgery was 112.3±59.1min. Mean hospital stay was 2.8±1.3 days. The lateral collateral ligament complex (LCL)was reattached in 55.3%. Repair was made with transosseous suture (27.3%), attachments, such as OBL (Smith-Nephew Dyonics®) (Fig. 1), or FastIn (DePuy-Mitek®) in 28%. In 44.7% it was possible to proceed to end-to-end ligament suture. External fixation was used in 3 cases (6.4%).
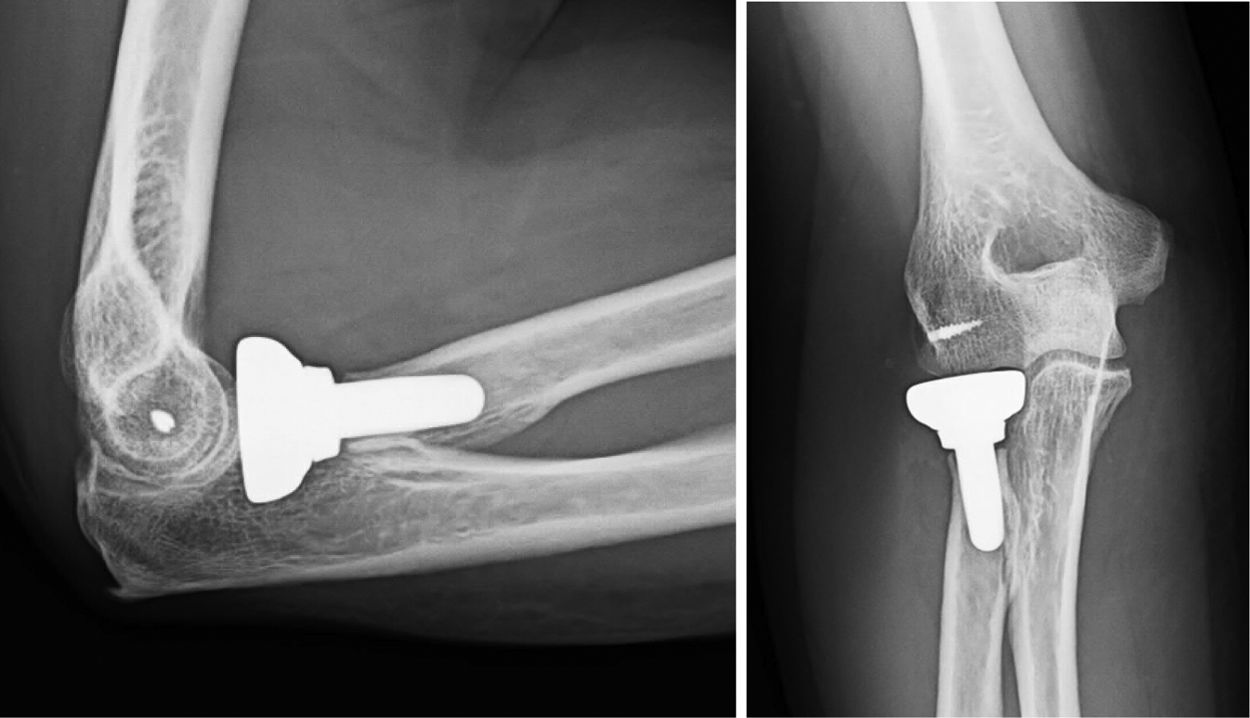
Two types of prosthesis were used, the Tornier® bipolar(45.7%, 22 cases) (Fig. 2) and the Acumed® monopolar (54.3%, 25 cases) (Fig. 3). They were cemented in 30.4% of cases and cementless in 69.6%. The short stem was used in 82.6% and the long stem in 17.4%.
Regarding coronoid fracture treatment this was: orthopaedic (4.3%), reduction and osteosynthesis with Kirschner needles (53.2%), transosseous fixation (8.5%), graft and osteosynthesis with pins (2.1%), epicondyl graft and needles (2.1%) and removal of minimum, comminuted and loose coronoid fragments (29.8%) (Fig. 4).
Study variablesThe analysed variables were: affiliation data, Mason classification, surgical aspects (moment of surgery, time in surgery, type of prosthesis, cementation, reinterventions); rehabilitation time, causes of prosthetic failure, complications, radiographic findings (according to van Riet et al.18), loosening areas (Popovic et al.19), MEPS20,21 and Cassebaum22,23scales.
Statistical analysisWe conducted an intergroup study between 2 types of prosthesis: monopolar and bipolar, to establish findings, according to the cases treated with one prosthesis or the other.
Regarding the statistical study, a global descriptive study was first conducted, with details of means, medians, standard deviations, minimums and maximums for numerical variables and the study using frequency tables for the categorical variables.
After this, different statistical tests were used to determine statistically significant differences. The comparison was made depending on the type of prosthesis used, the time in surgery, cementation or degree of coronoid compromise.
For the numerical variables, prior analysis was initially performed using the test of normality and specifically the Shapiro-Wilko test. The non normal numerical nature of distribution was determined in the majority of the analysed variables, except for the time in surgery, rehabilitation time, flexion and MEPS, variables which did demonstrate normal distribution.
For the hypothesis contrasts, in the case of presenting variables to analyse a non normal distribution the non parametric test was used. In the case of presenting the variables to be analysed for a normal distribution, parametric tests were used.
In the first supposition: analysis of quantitative numerical variables, of non normal distribution, with regard to other qualitative variables, the contrast between 2 independent samples were analysed (hospital stay time depending on the cemented or cementless type or prosthesis and hospital stay, extension, pronation and supination depending on the mono or bipolar type prosthesis) for which the Mann-Whitney U test was used, on being dichotomous qualitative variables in both cases: either cementation or non cementation, or either mono compared to bipolar. For the case of analysis of 3 independent samples, being qualitative non dichotomous variables (study of time in hospital, depending on the delay in surgical procedure, or length of hospital stay, depending on type of coronoid fracture), the Kruskall-Wallis test was used.
In the second supposition: analysis of quantitative numerical variables, with normal distribution, compared with other qualitative variable, 2dependent variables were analysed, for which the Student’s t-test was used (time in surgery, rehabilitation time, result of the MEPS scale depending on cementation or non cementation, or time in surgery, months of rehabilitation, flexion or MEPS depending on the type of mono or bipolar prosthesis). In this case, the qualitative variables were dichotomous (cementation compared with non cementation and mono compared with bipolar prosthesis). When the quantitative variables were of normal distribution they were analysed compared with non dichotomous quantitative variables and the ANOVA test was applied. This was therefore used to assess statistical differences regarding time in surgery and rehabilitation, or MEPS scale when the result were compared regarding moment of surgery or type of coronoid fracture.
For categorical variables contingency tables were used, specifically the Chi square test and the exact Fisher test. These tests were used to see if there were any differences between mono or bipolar prostheses, with regard to the variables: need for external fixation, cementation, reintervention, stiffness, prosthetic mobilization, heterotopic ossification, prosthetic loosening, results according to Cassebaum, MEPS groups and employment prognosis.
In the analyse confidence intervals of 95% were sought. The level of alpha statistical significance was .05.
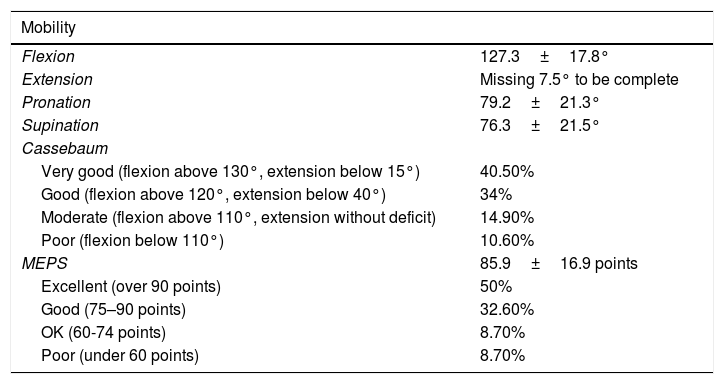
ResultsGood results were reached regarding mobility, Cassebaum22,23or MEPS (Table 1).
Overall results regarding mobilise, Cassebaum and MEPS. Observe the predominance of excellent and good results.
| Mobility | |
|---|---|
| Flexion | 127.3±17.8° |
| Extension | Missing 7.5° to be complete |
| Pronation | 79.2±21.3° |
| Supination | 76.3±21.5° |
| Cassebaum | |
| Very good (flexion above 130°, extension below 15°) | 40.50% |
| Good (flexion above 120°, extension below 40°) | 34% |
| Moderate (flexion above 110°, extension without deficit) | 14.90% |
| Poor (flexion below 110°) | 10.60% |
| MEPS | 85.9±16.9 points |
| Excellent (over 90 points) | 50% |
| Good (75–90 points) | 32.60% |
| OK (60-74 points) | 8.70% |
| Poor (under 60 points) | 8.70% |
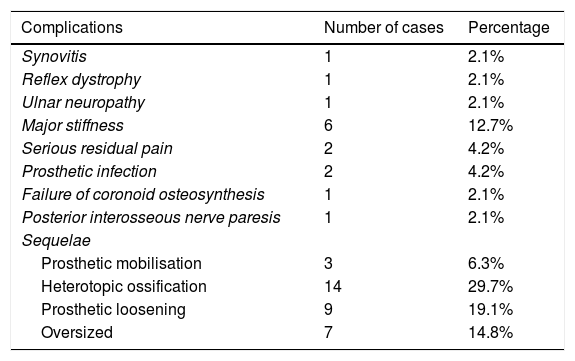
Rehabilitation time was 4.7±2.5 months. Follow-up time was a median of 25.5 months, with a minimum of 2 years and a maximum of 10 years. In 76.6% of cases the patient went back to work. There were complications in 36.2% of the series. The complications and sequelae are contained in Table 2. Among the sequelae found, heterotopic ossification affected mainly the anterior capsule (62.5%). It also affected the loosening areas which were distributed according to Popover et al.’s classification19 in the following way: area 7 (14.3%), from area 1 to area 6 (7.1%), areas 1 and 7 (50%), from area 1–7, the whole stem area (14.3%), and in areas 2, 3, 4, 5 and 6 (14.3%).
Main complications and sequelae. Observe the high frequency (29.8%) of heterotopic ossifications.
| Complications | Number of cases | Percentage |
|---|---|---|
| Synovitis | 1 | 2.1% |
| Reflex dystrophy | 1 | 2.1% |
| Ulnar neuropathy | 1 | 2.1% |
| Major stiffness | 6 | 12.7% |
| Serious residual pain | 2 | 4.2% |
| Prosthetic infection | 2 | 4.2% |
| Failure of coronoid osteosynthesis | 1 | 2.1% |
| Posterior interosseous nerve paresis | 1 | 2.1% |
| Sequelae | ||
| Prosthetic mobilisation | 3 | 6.3% |
| Heterotopic ossification | 14 | 29.7% |
| Prosthetic loosening | 9 | 19.1% |
| Oversized | 7 | 14.8% |
There were also reinterventions in 26.1% of cases (12 cases). The most outstanding were the removal of the prosthesis in 2 cases (4%-3%), open arthrolysis in 2 cases (4.3%), arthroscopy in 4 cases (8.5%), the removal of the AK in coronoids in 4 cases (8.5%).
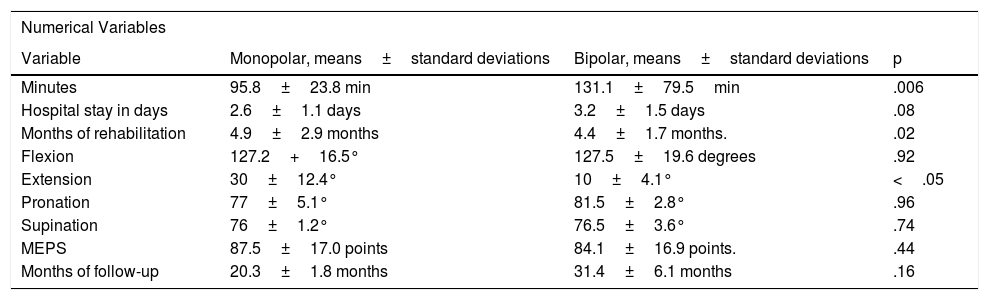
Contrast of hypothesisThis was a contrast of hypotheses study to deduce whether there were statistically significant differences, or not, in the light of different aspects. The most important data relating to the intergroup comparative study between patients treated with monopolar prostheses and bipolar prostheses are contained in Table 3. Note that the time in surgery was higher in bipolar surgery and there was a higher rate of reinterventions, and complications in cases of bipolar arthroplasties.
Contrast of hypothesis between bipolar and monopolar prostheses comparing numerical type variables. Observe that intervention time was higher in the bipolar operations. Contrast of hypothesis of categorical type variables. Observe that there was a greater rate of reinterventions, more stiffness, prosthetic mobilisation, ossification and prosthetic loosening in the cases of bipolar arthroplasties.
| Numerical Variables | |||
|---|---|---|---|
| Variable | Monopolar, means±standard deviations | Bipolar, means±standard deviations | p |
| Minutes | 95.8±23.8 min | 131.1±79.5min | .006 |
| Hospital stay in days | 2.6±1.1 days | 3.2±1.5 days | .08 |
| Months of rehabilitation | 4.9±2.9 months | 4.4±1.7 months. | .02 |
| Flexion | 127.2+16.5° | 127.5±19.6 degrees | .92 |
| Extension | 30±12.4° | 10±4.1° | <.05 |
| Pronation | 77±5.1° | 81.5±2.8° | .96 |
| Supination | 76±1.2° | 76.5±3.6° | .74 |
| MEPS | 87.5±17.0 points | 84.1±16.9 points. | .44 |
| Months of follow-up | 20.3±1.8 months | 31.4±6.1 months | .16 |
| Categorical Variables | |||
|---|---|---|---|
| Variables | Monopolar. number of cases (%) | Bipolar, number of cases (%) | p |
| Suture of the LCL | 16 (64) | 10 (45.4) | .2 |
| Need for external fixator | 0 (0) | 3 (13.6) | .05 |
| Need for cement | 0 (0) | 14 (63.6) | <.05 |
| Stems | 24 short/1 long | 14 short/7 long | <.05 |
| Reintervention | 5 (20) | 10 (45.4) | .05 |
| Removal of prosthesis | 0 (0) | 2 (9) | .19 |
| stiffness | 3 (12) | 8 (36.3) | .04 |
| Prosthetic mobilisation | 0 (0) | 3 (13.6) | .05 |
| Heterotopìcossification | 3 (12) | 11 (50) | .004 |
| Loosening of prosthesis | 1 (4) | 8 (36.3) | .005 |
| Oversized | 2 (8) | 5 (22.7) | .17 |
Other aspects were that there we no differences with regard to delay in surgical procedures, either in : time in surgery time, p=.49; days in hospital, p=.36, months of rehabilitation, p=.65, or result of the MEPS scale, p=.80.
Regarding type of prosthesis, if they were cemented or cementless, this had no impact on rehabilitation time or on MEPS scale, with p values =.42 or p=.37, respectively. However, there were differences regarding time in surgery, p=.04, on cementing or not cementing a prosthesis, with this being higher in the cemented prosthesis.
Finally, regarding type of coronoid apophysis fracture, no differences were found regarding length of hospital stay in days (p=.39), but there were differences for time in surgery (p=.05), with this being greater in higher grade coronoid fractures. However, there were no differences regarding rehabilitation time (p=.42) or MEPS (p=.89).
DiscussionTreatment of Hotchkiss’ terrible triad1,2 has conventionally been surgical,24 although some authors25 have reported orthopaedic treatments, the main referrals of which are for stable elbows, without blockages and with minimal fracture of the coronoid process <2mm (Regan and Morrey I-II).
In this study we focused on reviewing cases which were treated surgically and with a radial head prosthesis, given the non-reconstitutable nature of the head.
The summary of main results obtained in this study led us to believe that the type of prosthesis did impact the treatment of terrible triads of the elbow. Indeed, time in surgery for the implantation of monopolar prostheses was lower than that of bipolar. We also found that with bipolar prostheses more external fixation was required, more patients required re-surgery and the number of complications was higher. However, this did not affect the MEPS or Cassebaum validated clinical tests.
In this study a sample size of 47 cases was obtained. The relationship of this series with others in the literature has led to a highly varied analysis, from the 11 cases reported by Fitzgibbons et al.12 or the 137 reported by Rodriguez-Martin et al.26 The interesting point of this study was to assess only cases with arthroplasty and compare them according to the type of materials used.
In our series, the result of the MEPS scale was 85.9±16.9 points. If we analyse the clinical results obtained from previous series we observe difference aspects. Thus, surgical treatment has demonstrated that it may restore elbow stability, with favourable results in mobility, and up to 19.7 points on the Disabilities of Arm, Shoulder and Hand (DASH) scale or 85–96 points on the MEPS12scale. This treatment determined the good result in cases of instability27 and for Zhou et al.,28 especially with the lateral route. In our series we did not resect the radial head, because we believe that the resection of the radial head in type IV cases did not offer favourable results, due to the risk of associated instability. However, Nestorson et al.29 did indicate this in their series of 18 cases and Lópiz et al.,30 in their Mason III fractures, when comparing resection to arthroplasty, obtaining 13.5 points for resections compared with 24.8 points for arthroplasty, with the DASH scale.
In the surgical treatment of these injuries, time of surgery has an impact.31 In our experience, there were no differences regarding delayed surgical procedure, in: time of intervention, days of hospital stay, months of rehabilitation or result on the MEPS scale. Planning of surgery and its development by a team of qualified surgeons is of interest. For several authors,32,33 early treatment led to results on the Broberg and Morrey34 score of 88 points. For other authors,35, if treatment was delayed over 2 weeks, reintervention rates were up to 15%-20%, due to instability, removal of material or stiffness. Lindenhovius et al.36 observed a better flexion and extension arc (113° vs. 93°, p <.05), and supination (p <.05), in patients who had been operated on earlier. The Broberg and Morrey34 scale was similar (90 compared with 87 points). For Rodriguez-Martin et al.26, in their study on 137 terrible triads of the elbow, an arc of 111,4° was obtained, from flexion and extension, with MEPS of 85.6 points, when treatment took place during the first 2 weeks.
With regards to the type of treatment, in this series only cases of terrible triads have been described, with radial head arthroplasty. However, there are other authors who advocate osteosynthesis treatment. Leigh and Ball37 developed a comparative study between 13 cases with radial head osteosynthesis and 11 cases treated with arthroplasty, with higher values on the DASH scale reached with the arthroplasty. Watters et al.38 published a series of 39 cases, where all the patients with a prosthesis had a stable elbow, compared with 3 or the 9 cases treated with osteosynthesis who were unstable (p=.009). There was no difference in the rate of reinterventions or the DASH scale points. Marsh et al.,39 in their study on 55 patients, reported good results after modular prosthetic replacement with a 5-year follow-up, with MEPS of 91±13 points. Also Chanlalit et al.40,41studied 8 elbow specimens. The point of force for elbow dislocation was similar between the monopolar prostheses and the native radial heads, although it was very different regarding the bipolar prostheses (non anatomical)(p=.0006). Levy et al.,42 in their series of 15 patients, collected MEPS of 85 points, with maximum supination and pronation arcs around 80°. In their series of 44 patients, Martín-Fuentes et al.43 also obtained 82% of satisfactory results with monopolar prostheses.
In our experience, we used monopolar prostheses (25) and bipolar prostheses (22). We found there were differences, depending on the type of prosthesis, regarding time in surgery (being higher in the bipolar); rate of reintervention and complications (being higher in the bipolar). We are currently changing our referral for monopolar system prostheses, such as that of Acumed®, since the comparative studies between both prostheses in cadaver report better results in primary stability for the monopolar prostheses and poorer ones for the bipolar ones with different rates of dislocation or clinical instability.44 Therefore, regarding the results reached for the main objective of the study (comparing the 2 types of prostheses for terrible triads) compared with previous studies we may state the following: for Hartzler et al.45 this point arouses controversy. Thus, when the LCL is intact, there would be no differences between both prostheses in valgus stress p=1.0). Neither would there be differences in latitude in external rotation with regard to the valgus stress (p=1.0). For Giannicola et al.,46 monopolar prostheses however, would not reproduce all the anatomical variants of the proximal radius and would require meticulous surgical technique, since any technical error could lead to major joint incongruence. Bipolar prostheses enable adaptation to the anatomy of each patient and would theoretically be easier to implant. The disadvantage would be the possible lower joint stability and the tribological changes from wear and tear of the polyethylene. Another theoretical advantage would be reduction of septic loosening and wear and tear at ulnar and humeral levels. For Chen et al.,47 bipolar prostheses are associated with more heterotopìcal ossifications and radiolucencies. For Heijink et al.,48 in their review of 727 patients, however, no major differences we found in review rates when one or the other prosthesis was used. For several authors,49,50 bipolar prostheses would afford good functional results, such as for van Hoecke et al.,51 with MEPS of 86.6 points, although radiolucencies were suggested. Finally, authors such as Sánchez-Sotelo and Morrey52 have stated that although bipolar prostheses could be used in the treatment of terrible triads, the bipolar implants have a higher tendency to prosthetic subluxation and to polyethylene wear and tear, and they therefore prefer to use monopolar prostheses.
With regard to the action on coronoid apophysis, we observed that time in surgery is higher the more complex the coronoid fracture. With regard to the previous series, Papatheodorou et al.53 reviewed 14 cases with a final result on the Broberg and Morrey34 scale of 90–100 points. Garrigues et al.54 achieved flexion and extension arcs of 115° in 40 patients with coronoid fixation with needles. In our series, treatment with Kirschner needles accounted for up to 55.3% of cases.
Treatment of this type of injury is not free from complication. In our series in 36.2% and up to 22% for Jones y Jordan115 the following were described: instability;16 radial ulnar synothosis; infection; osteoarthritis (39%-67%); heterotopic ossification36 (11%); stiffness55 (59%) and compromise of the ulnar nerve, requiring neurolysis55 (21%), or periimplant fractures.56 For Laflamme et al.57, the implants of porous stems have a greater tendency towards osteolysis (p=.01) and oversize (p=.21), which is avoidable by measuring the proximal variance.58 For Sullivan et al.,59 there is also a wearing inside the medullary canal (“dilatory remodelling”) in 34.9% of their series, without the need for bipolar replacment60 or removal,61 unless it is painful.62
Finally, in this series 76.6% of the patients who underwent surgery were included, which would be in keeping with that recorded in other series, such as that of Dunn et al.,63 with a return to normal life of 75% of the sample.
LimitationsMedian follow-up time was 25.5 months, with a minimum of 2 years and a maximum of 10 years. We believe this follow-up time could be short and that many of the complications which occurred with the radial head arthroplasties, such as loosening, mobilization, etc. would probably increase if follow-up had been longer.
ConclusionsIn our experience, within the context of the “terrible triad” of the elbow, the type of prosthesis does have an impact, since the time in surgery for the implantation of a monopolar prosthesis was lower. Furthermore, with bipolar prostheses greater external fixation is required, which also leads to a higher rate of reinterventions and complications but no differences between the two prostheses exist in clinical results.
FinancingThe authors did not receive any type of financing for this study.
Conflict of interestsThe authors have no conflict of interests to declare.
We wish to thank Mr. José Villanueva and Ms. Lucía Buzón, members of the theatre staff in our hospital for taking intraoperative photographs for this study. We would also like to thank the theatre supervisor, Miss. Mercedes Naranjo, for collecting the cases, and subsequently creating out database.
Please cite this article as: Jiménez-Martín A, Contreras-Joya M, Navarro-Martínez S, Najarro-Cid FJ, Santos-Yubero FJ, Pérez-Hidalgo S. Resultados clínicos de la artroplastia radial en la tríada terrible de Hotchkiss, a propósito de 47 casos. Rev Esp Cir Ortop Traumatol. 2020;64:83–91.