Screw tip augmentation with bone cement for fixation of osteoporotic proximal humerus fractures seems to improve stability and to decrease the rate of complications related to implant failure. However, the optimal augmentation combinations are unknown. The aim of this study was to assess the relative stability of two augmentations combinations under axial compression load in a simulated proximal humerus fractures fixed with locking plate.
Material and methodsA surgical neck osteotomy was created in five pairs of embalmed humeri with a mean age of 74 years (range 46–93 years), secured with a stainless-steel locking-compression plate. In each pair of humeri, on the right humerus were cemented the screws A and E, and in the contralateral side were cemented screws B and D of the locking plate. The specimens were first tested cyclically in axial compression for 6000 cycles to evaluate interfragmentary motion (dynamic study). At the end of the cycling test, the specimens were loaded in compression force simulating varus bending with increasing load magnitude until failure of the construct (static study).
ResultsThere were no significant differences in interfragmentary motion between the two configurations of cemented screws in the dynamic study (p=0.463). When tested to failure, the configuration of cemented screws in lines B and D demonstrated higher compression load to failure (2218N vs. 2105, p=0.901) and higher stiffness (125N/mm vs. 106N/mm, p=0.672). However, no statistically significant differences were reported in any of these variables.
ConclusionsIn simulated proximal humerus fractures, the configuration of the cemented screws does not influence the implant stability when a low-energy cyclical load is applied. Cementing the screws in rows B and D provides similar strength to the previously proposed cemented screws configuration and could avoid complications observed in clinical studies.
La utilización de tornillos cementados en la fijación interna de fracturas de húmero proximal con placas bloqueadas parece mejorar la estabilidad del implante y disminuir las complicaciones asociadas al fracaso de síntesis. Sin embargo, la combinación óptima de tornillos cementados se desconoce. El objetivo de este estudio fue analizar la estabilidad relativa de 2 configuraciones de tornillos cementados sometidos a una fuerza de compresión axial en una fractura simulada de húmero proximal.
Material y métodosSe realizó una osteotomía del cuello quirúrgico en 5 pares de húmeros embalsamados con una edad media de 74 años (rango: 46-93), fijados con una placa de acero inoxidable con tornillos bloqueados. En cada par de húmeros, en el húmero derecho se cementaron los tornillos A y E, y en el lado contralateral se cementaron los tornillos B y D. Cada espécimen fue testado inicialmente mediante una carga cíclica de compresión axial durante 6.000 ciclos para evaluar el movimiento interfragmentario (estudio dinámico). Al final de la prueba, los especímenes se sometieron a una carga de compresión axial progresiva para medir la rigidez de la construcción (estudio estático).
ResultadosNo se encontraron diferencias estadísticamente significativas en la movilidad interfragmentaria entre las 2 configuraciones de tornillos cementados en el estudio dinámico (p=0,463). Cuando se sometieron a rotura, los especímenes con tornillos cementados en las hileras B y D presentaron una carga de rotura mayor (2218N vs. 2105; p=0,901) y una mayor rigidez (125 vs. 106N/mm; p=0,672); sin embargo, ninguna de estas diferencias fue estadísticamente significativa.
ConclusionesLa configuración de los tornillos cementados utilizadas en este estudio no influyen en la estabilidad del implante cuando se aplica una carga cíclica de baja energía. La cementación de los tornillos de las hileras B y D proporciona una resistencia similar a la cementación de los tornillos A y E.
The main complication of open reduction and internal fixation (ORIF) with locked plates in fractures of the proximal humerus (PHF) is failure of synthesis and intra-articular penetration of the screws,1 especially in patients with osteoporotic bone. This is mainly due to shear forces occurring at the bone-implant interface, leading to loss of reduction and fracture collapse.
In order to improve implant stability, different strategies have been developed, such as allograft supplementation or cementation of the screws with polymethylmethacrylate (PMMA). Both biomechanical studies2–5 and clinical studies6,7 with this technique have shown that PMMA cementation of screws in PHF improves stability and decreases complications associated with synthesis failure; however, the optimal configuration of cemented screws is unknown.
The surgical technique8 proposes cementing the two most proximal screws and the two calcar screws to ensure a homogeneous distribution of cement in the humeral head. Despite this, the calcar screws are often located close to the fracture site and clinical studies have described up to 11.5% cement extravasation in these screws.6 Furthermore, in clinical studies the cementation of more proximal screws has been associated with 4–8% partial necrosis.6,7 To avoid these two types of complications, we propose the cementation of central humeral head screws.
The hypothesis of this study is that the cementation of the central row screws achieves biomechanically comparable results to those obtained with the cementation of the screws proposed by the original technique and could avoid the complications observed in clinical studies.
The aim of this study was to analyse the relative stability of two cemented screw configurations subjected to axial compression force in a simulated proximal humerus fracture fixed with plate and locked screws: proximal and distal row cementation (A and E) versus central humeral head screw cementation (B and D).
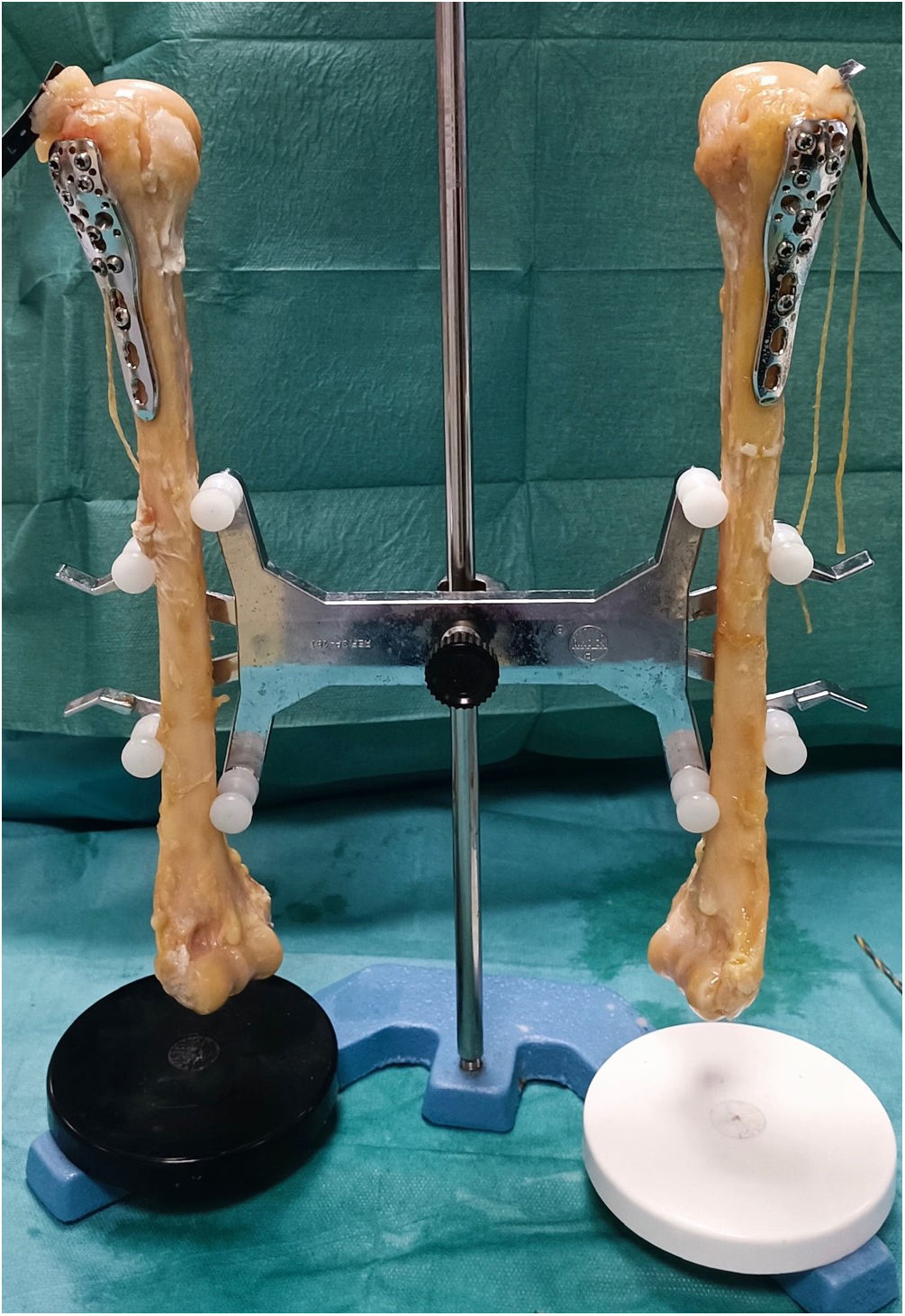
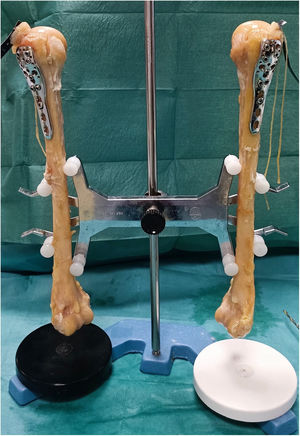
Material and methodsPreparation of specimensTen human humerus specimens were extracted from five cadavers from the cadaver bank of the Universidad Autónoma de Madrid (three males and two females) with a mean age of 74 years (range, 46–93).
A preformed stainless steel proximal humerus plate with locked screws (PHILOS; DePuy Synthes, Zuchwil, Switzerland) was placed in each humerus (Fig. 1). The position of the plate was determined 1cm inferior to the articular surface and 1cm posterior to the bicipital slide. The plate was initially fixed with a cortex screw in the diaphysis, followed by fixation of the humeral head with locked screws to the plate, and final fixation of the diaphysis also with locked screws.
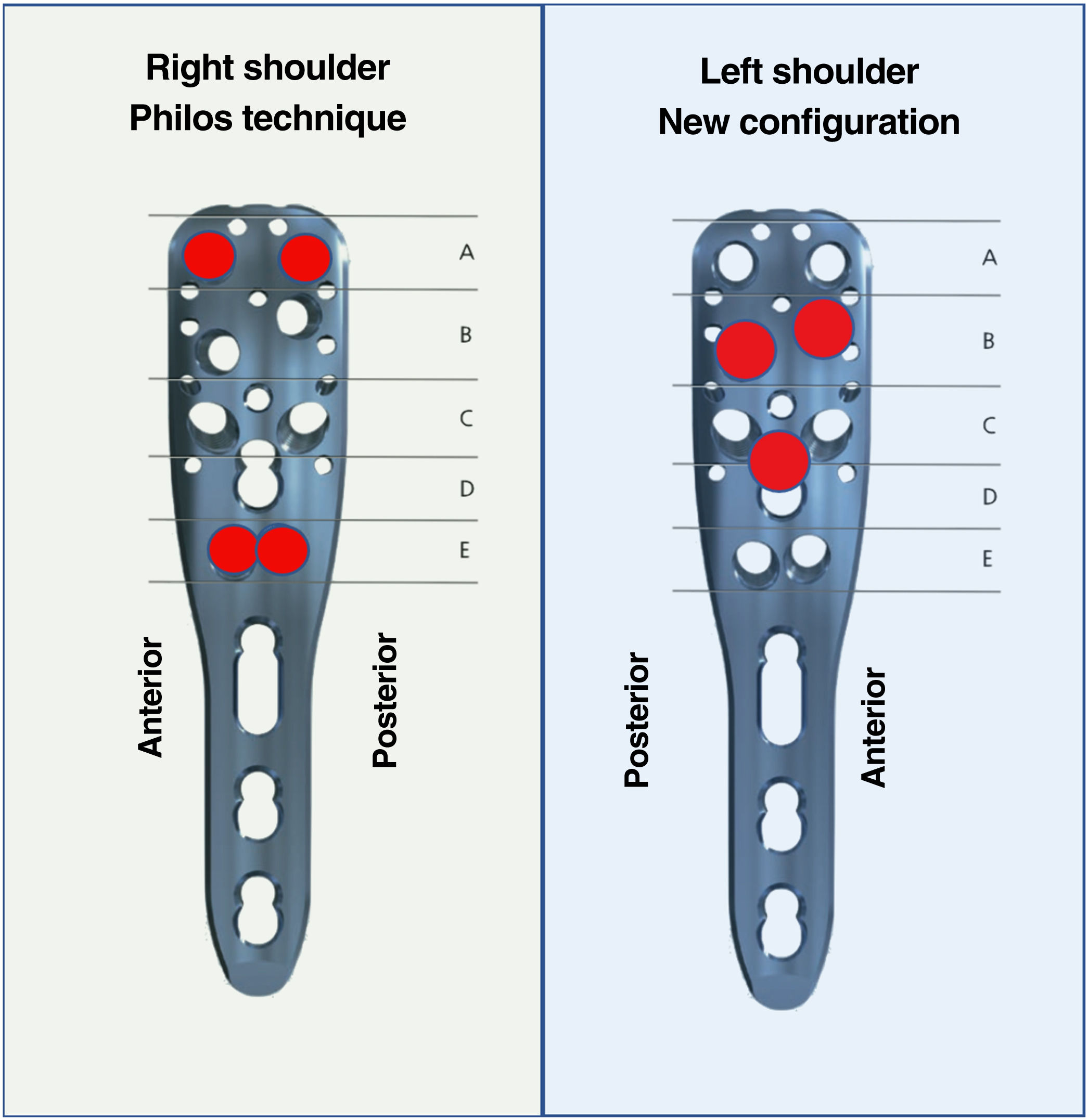
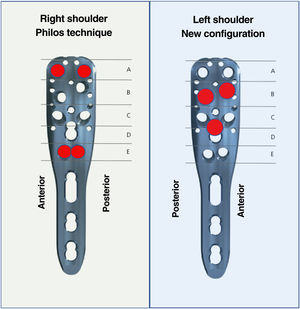
Four mm was subtracted from the measurement obtained with conventional screws using a short screw configuration to avoid intra-articular penetration of the screws in case of fracture collapse. When cannulated screws were used, 6mm was subtracted from the measurement obtained instead of 4mm to avoid the cement being too close to the articular surface and to achieve interdigitation of the cement with the humeral head. To minimise interspecimen variability, in each pair of humeri from the same cadaver, cannulated screws were used on the right side for subsequent cementation following the classical cementation technique (rows A and E), while on the left side cannulated screws were used in the central rows according to the proposed new configuration of cemented screws (rows B and D) (Fig. 2).
To minimise interspecimen variability, in each pair of humeri from the same cadaver, cannulated screws were used on the right side for subsequent cementation following the classical cementation technique (rows A and E), while on the left side cannulated screws were used in the central rows according to the proposed new configuration of cemented screws (rows B and D) (Fig. 2).
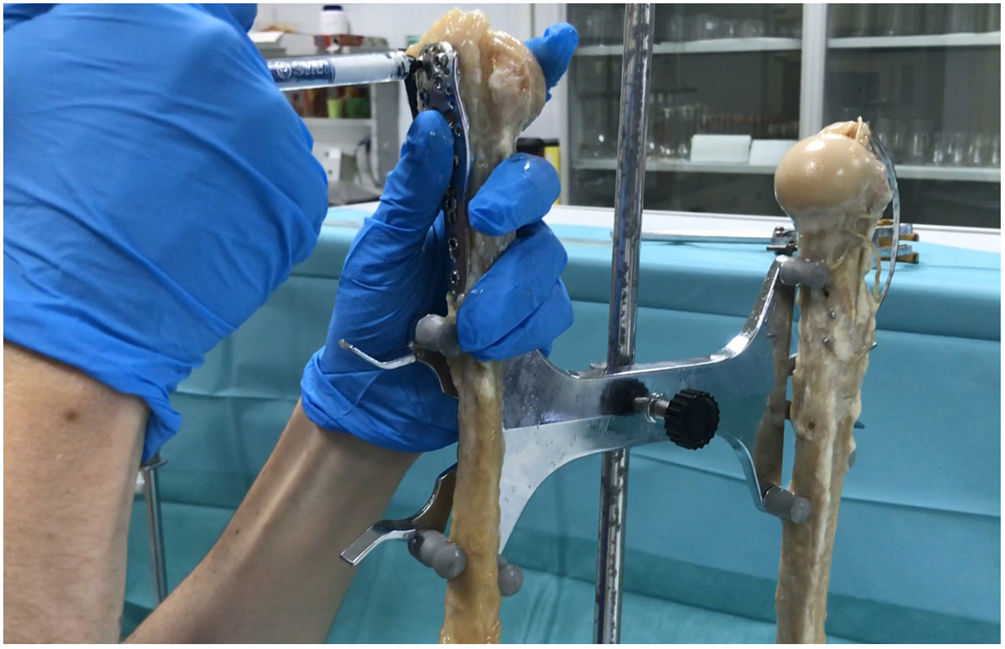
All humeri were X-rayed to verify that the plates were correctly positioned and the screws were of adequate length. The screws were then cemented with 5ml of cement in each cannulated screw (Trauma Cem Vþ; DePuy Synthes) (Fig. 3) and all humeri were radiographed once cementing was complete.
In each specimen, a wedge osteotomy was performed with a saw, simulating an unstable fracture of the surgical neck. The osteotomy was established 1cm from the lower edge of the articular cartilage with a thickness of .5cm. Performing the osteotomy after implant placement avoids variations due to fragment mobilisation. Subsequently, an X-ray was taken of all the humeri after completion of the osteotomies (Fig. 4).
ImplantsAll the implants used were made of stainless steel. All plates had the same length (90mm) and the same number of holes (three distal and nine proximal). All screws were placed except for those in row C, as the tips of these screws are usually at the same height as the tips of the screws in row A.
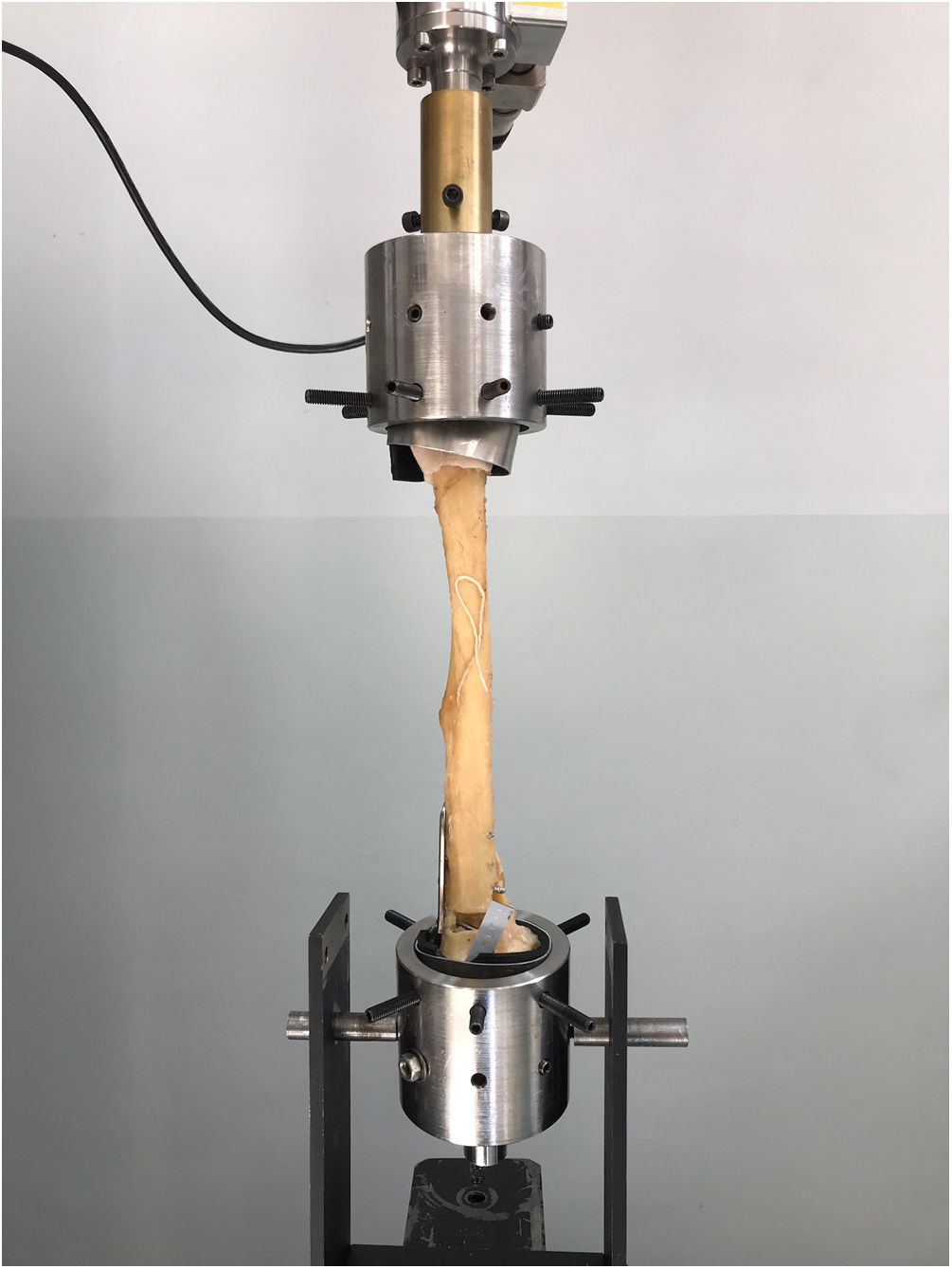
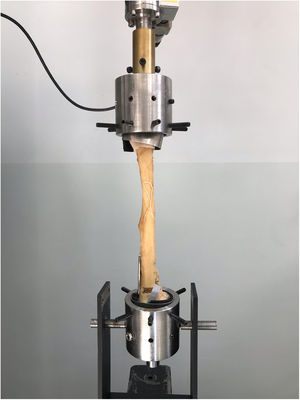
Biomechanical studyEach specimen was initially tested by cyclic axial compressive loading with a servo-hydraulic machine (Schenk_Trebel) to evaluate interfragmentary movement (dynamic study). A cosine load was applied to the specimens in a range between 15N and 50N at a frequency of .25Hz up to 6000 cycles (Fig. 5). For this study, implant failure was defined as a displacement between fragments greater than 5mm with respect to the initial situation.
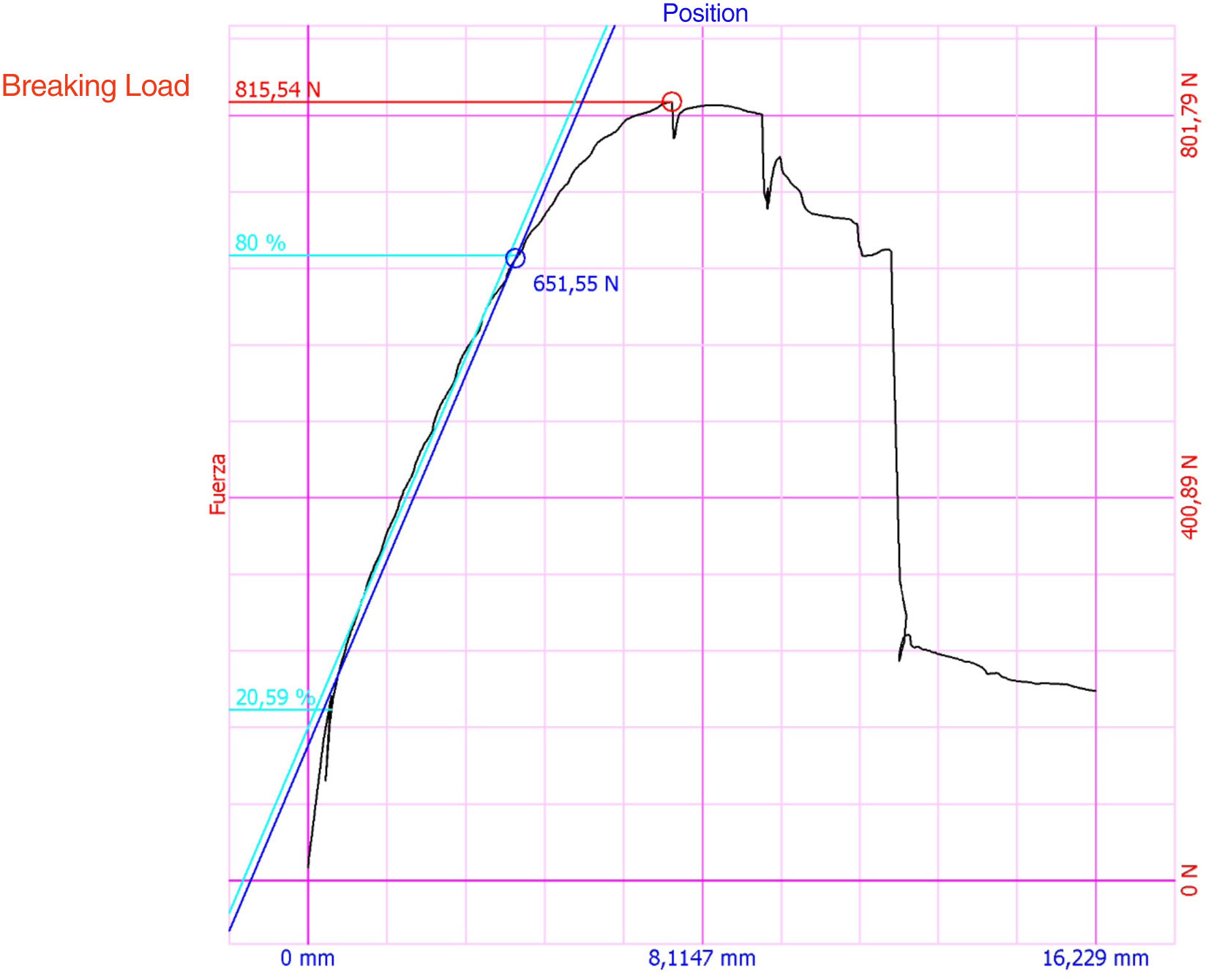
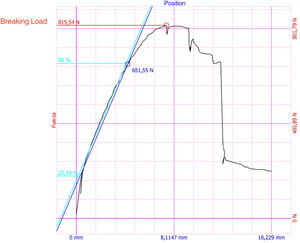
At the end of the test, the specimens were subjected to a compressive load at break to measure the stiffness of the construction (static study). For this purpose, an increasing compressive load was applied at a rate of 20mm/min until failure, defined as dissociation between the bone and the implant, the appearance of a fracture line or implant breakage. The load was recorded as a function of displacement and the energy absorbed as the area under the curve.
Statistical analysisStatistical analysis was performed using SPSS software (SPSS Inc., Chicago, IL, USA), Comparisons between pairs of specimens were performed with the Wilcoxon signed-rank test. A p value<.05 was considered statistically significant.
ResultsDynamic studyDuring the dynamic axial compression study, no statistically significant differences in interfragmentary mobility were found between specimens with screws cemented in rows A and E and specimens with screws cemented in rows B and D (p=.463). After 6000 cycles, the maximum interfragment mobility was .29mm (range .08–.53) and .32mm (range .22–.53, respectively. None of the specimens failed during the dynamic study.
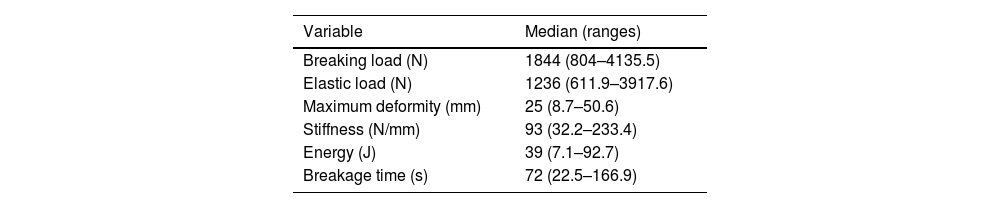
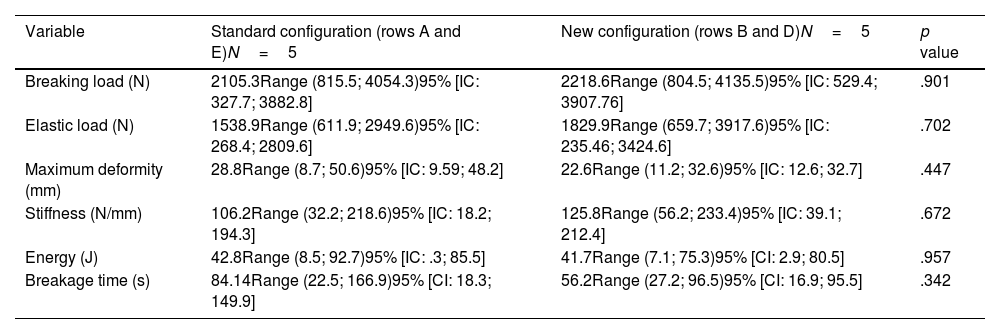
Static studyWhen subjected to rupture (Fig. 6), the median failure load was 1.844N, and the mean failure time was 72s (Table 1). When comparing the two cemented screw configurations, specimens with screws cemented in rows B and D presented a higher ultimate load (2.218N vs. 2.105, p=0.901) and higher stiffness (125N/mm vs. 106N/mm, p=0.672). Specimens with cemented screws in rows A and E tolerated 6mm more deformity before failure (p=.447) and the time to failure was longer (84s vs. 56s, p=.342); however, neither of these differences was statistically significant (Table 2).
Comparison between specimens with the classic cemented screw configuration and the specimens with the new configuration in the fracture test.
| Variable | Standard configuration (rows A and E)N=5 | New configuration (rows B and D)N=5 | p value |
|---|---|---|---|
| Breaking load (N) | 2105.3Range (815.5; 4054.3)95% [IC: 327.7; 3882.8] | 2218.6Range (804.5; 4135.5)95% [IC: 529.4; 3907.76] | .901 |
| Elastic load (N) | 1538.9Range (611.9; 2949.6)95% [IC: 268.4; 2809.6] | 1829.9Range (659.7; 3917.6)95% [IC: 235.46; 3424.6] | .702 |
| Maximum deformity (mm) | 28.8Range (8.7; 50.6)95% [IC: 9.59; 48.2] | 22.6Range (11.2; 32.6)95% [IC: 12.6; 32.7] | .447 |
| Stiffness (N/mm) | 106.2Range (32.2; 218.6)95% [IC: 18.2; 194.3] | 125.8Range (56.2; 233.4)95% [IC: 39.1; 212.4] | .672 |
| Energy (J) | 42.8Range (8.5; 92.7)95% [IC: .3; 85.5] | 41.7Range (7.1; 75.3)95% [CI: 2.9; 80.5] | .957 |
| Breakage time (s) | 84.14Range (22.5; 166.9)95% [CI: 18.3; 149.9] | 56.2Range (27.2; 96.5)95% [CI: 16.9; 95.5] | .342 |
All specimens failed in the diaphysis by a fracture line that included at least one of the holes used for plate fixation.
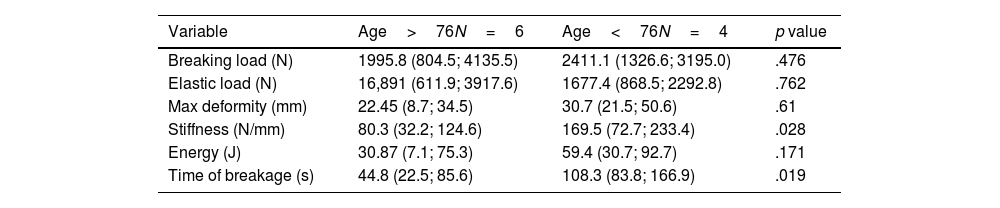
A comparative analysis was performed between those specimens with an age older than 76 years (n=6) and those younger than 76 years (n=4) and it was observed that those specimens younger than 76 years tolerated greater deformity before failure (30.7mm vs. 22.4mm, p=.61), higher ultimate load (2411N vs. 1995N, p=.476) and absorbed greater energy (59J vs. 30J, p=.171), without these differences being statistically significant. Significant differences were only observed in stiffness and breakage time (Table 3).
Comparison between the specimens in the trial at breakage according to age.
| Variable | Age>76N=6 | Age<76N=4 | p value |
|---|---|---|---|
| Breaking load (N) | 1995.8 (804.5; 4135.5) | 2411.1 (1326.6; 3195.0) | .476 |
| Elastic load (N) | 16,891 (611.9; 3917.6) | 1677.4 (868.5; 2292.8) | .762 |
| Max deformity (mm) | 22.45 (8.7; 34.5) | 30.7 (21.5; 50.6) | .61 |
| Stiffness (N/mm) | 80.3 (32.2; 124.6) | 169.5 (72.7; 233.4) | .028 |
| Energy (J) | 30.87 (7.1; 75.3) | 59.4 (30.7; 92.7) | .171 |
| Time of breakage (s) | 44.8 (22.5; 85.6) | 108.3 (83.8; 166.9) | .019 |
The results of this study suggest that, in proximal humerus fractures, the configuration of the cemented screws does not influence implant stability when low energy cyclic loading is applied. However, when subjected to progressive compressive loading, the cemented screws in the B and D rows exhibit greater stiffness and appear to withstand greater loading before failure occurs, although these differences are not statistically significant. These results have clinical relevance, as the cemented screw configuration proposed in this study appears to contribute similarly to implant stability and may reduce the complications observed in clinical studies related to intra-articular cement leakage or partial necrosis.
Most biomechanical studies with this technique cement the four proximal screws3–5 or those in the anteromedial region of the humeral head.2 The rationale for choosing to cement the two screws in the anterior direction is based on the results of a previous study in which bone quality was assessed along the first six screws of the Philos plate.9 According to these data, the screws in positions 4 and 5 for a right proximal humerus specimen, and the corresponding positions 3 and 6 for a left proximal humerus, represent the anteromedial region of the humeral head and have been identified as having a lower bone mineral density.
Roderer et al.2 found that the breaking load was higher in those specimens with cemented screws directed towards the anterior region of the humeral head compared to those with uncemented screws (291N vs. 211N, p=.01). The studies by Unger et al.4 and Kathrein et al.3 support these results. In contrast to them, Schliemann et al.5 performed a biomechanical study of six pairs of humeri with a simulated three-part fracture fixed with polyetheretheretherketone (PEEK)-reinforced carbon fibre plate and anterior screw cementing and observed no statistically significant differences in stiffness (453N/mm vs. 461N/mm, p=.594) or in ultimate load (706N vs. 669N, p=.646) between specimens with cemented and uncemented screws. This may be because the mean age of the humeri in this study was 54 years, in contrast to previous studies where the mean age was 70–78 years.2–4 What was observed in this study was that there was less mobility at the bone-implant interface in the cemented-screwed humeri when subjected to varus force. This means that, although cementation of the screws contributes to improved implant stability, the benefit is greater in patients with osteoporotic bone than in younger patients with good bone quality.
Furthermore, it is striking that the breaking load observed in our study (1844N) is much higher than that obtained in previous studies with or without the use of cemented screws.2–4 In our opinion, this is mainly due to the placement of a greater number of screws in the humeral head and especially the calcar screws, since in previous biomechanical studies with this technique only the four most proximal screws were placed. The placement of an oblique locking screw within the inferomedial quadrant of the proximal humeral head fragment (calcar screw) has previously been shown to be important in preventing fixation failure.10,11 On the other hand, the number of screws cemented in our study is higher than in previous studies. Varga et al.,12 in a finite element study, analysed 64 different configurations of cemented screws to fix a three-part PHF and observed that both the number and configuration of cemented screws strongly influence implant stability, the greater the number of cemented screws, the greater the stability. In contrast to previous biomechanical studies, Varga et al.12 observed that the greatest benefits were achieved with the cementation of calcar screws and those directed towards the posterior region, while bone mineral density did not seem to influence the results, although the latter study does not include the cementation of the central screw in row D. We have not observed statistically significant differences between the two configurations of cemented screws, but we believe that calcar screws should always try to be placed, even if they are not cemented, because they contribute significantly to fracture stability.
This study has several limitations. On the one hand, it involves a small number of specimens, so its statistical power may not be sufficient. In addition, data obtained from a single osteotomy model may not be applicable to complex multifragmentary fracture patterns. Finally, data obtained from a cadaver study do not take into account the progressive fracture healing that occurs in vivo.
ConclusionsWe can conclude that, in simulated fractures of the proximal humerus, the cemented screw configurations used do not influence implant stability when low-energy cyclic loading is applied. Cementation of the B- and D-row screws provides similar strength to the previously proposed cemented screw configuration and could avoid the complications observed in clinical studies regarding intra-articular cement leakage or partial necrosis.
Level of evidenceLevel of evidence iv.
FundingNatalia Martínez Catalán received a grant from the Sociedad Española de Cirugía Ortopédica y Traumatología (SECOT) for this research project.
Conflict of interestsAntonio M. Foruria, MD PhD, received financial compensation for participating as a speaker or presenter in educational activities organised by DePuy Syntes in Spain and other European countries, in which the implants included in this article were discussed.
The other authors, their immediate families, and any research foundation with which they are affiliated have not received financial payments or other benefits from any commercial entity related to the subject of this article.