The use of hip arthroscopy as a treatment for femoroacetabular impingement (FAI) has increased exponentially in recent years without robust evidence or consensus about the patients who benefit from it.
ObjectiveTo develop explicit criteria for the appropriate indication of hip arthroscopy in FAI.
MethodA panel of experts was formed with 11 traumatologists following the RAND/UCLA method to identify the appropriateness criteria for hip arthroscopy in patients with FAI. The panel made independent evaluations of each indication using a nine-point adequacy scale, then met face-to-face to vote using an iterative discussion process. The influence of the variables on the final score was studied using multinomial logistic regression models. The Classification and Regression Tree (CART) analysis was used to summarise the results in the form of decision trees.
ResultsTwenty-three point four percent of the 192 scenarios evaluated in the face-to-face meeting was considered appropriate (40% agreement), 26.6% uncertain and 50% inappropriate (75% agreement). The most influential variables in considering the use of arthroscopy appropriate were: joint symptoms compatible with shock test, duration of symptoms, functionality, age and Hip Outcome Score (HOS) scale.
ConclusionsWe developed an explicit set of criteria for the appropriate use of hip arthroscopy in FAI using the RAND/UCLA method, providing a tool that would identify patients who are potential candidates for surgical treatment using arthroscopic hip surgery.
El uso de la artroscopia de cadera como tratamiento del choque femoroacetabular (CFA) ha aumentado exponencialmente en los últimos años sin que exista evidencia robusta o consenso sobre los pacientes que se benefician de ella.
ObjetivoElaborar criterios explícitos para la indicación adecuada de la artroscopia de cadera en CFA.
MétodoSe realizó un panel de expertos con 11 traumatólogos siguiendo el método RAND/UCLA para identificar los criterios de uso adecuado de la artroscopia de cadera en pacientes con CFA. El panel realizó evaluaciones independientes de cada indicación usando una escala de adecuación de nueve puntos, posteriormente se reunió presencialmente para votar usando un proceso iterativo de discusión. Se estudió la influencia de las variables en la puntuación final, utilizando modelos de regresión logística multinomial. Se utilizó el análisis Classification and Regression Tree (CART) para resumir los resultados en forma de árboles de decisión.
ResultadosDe los 192 escenarios evaluados en la reunión presencial, el 23,4% fue considerado adecuado (acuerdo del 40%), el 26,6% dudoso y el 50% inadecuado (acuerdo del 75%). Las variables más influyentes para considerar adecuado el uso de la artroscopia fueron: clínica articular compatible con test de choque, duración de los síntomas, funcionalidad, edad y escala Hip Outcome Score (HOS).
ConclusionesHemos desarrollado un conjunto explícito de criterios de uso adecuado de la artroscopia de cadera en CFA mediante el método RAND/UCLA, proporcionando una herramienta que permitiría identificar pacientes potencialmente candidatos a tratamiento quirúrgico mediante cirugía artroscópica de cadera.
Femoroacetabular impingement is one of the conditions responsible for hip pain and arthrosis of the hip in the young adult.1 It is caused by the presence of changes to the femoral head and neck (cam type) or the acetabulum (pincer type) or both, which lead to lesions in the labrum and joint cartilage.2,3 These deformities are even relevant in people with no joint problems and some authors have stated that the prevalence in an asymptomatic population of the cam type deformity is 37%, whilst the pincer type is 67%.4
Treatment with minimally invasive techniques may be given, among which are arthroscopic approaches.5 At present, it is unknown how many arthroscopic hip procedures are performed in Spain, although the perception is that it is increasing. Data published in the Basque Country from 2008 to 2013 show an increase in hip arthroscopy within the total of arthroscopic procedures performed of 2.77–27.5%.6
A systematic review of the available scientific literature on hip arthroscopy showed a single randomised clinical trial. 7,8 This situation has not changed in the most recent systematic revisions.9,10
Studies which identify appropriate use combine the available scientific evidence and the opinion of expert professionals in the use of technology. Their aim is to determine the indications for which the expected health benefits (e.g. increase life expectancy, pain relief, etc.) would overcome the expected negative consequences (e.g. mortality, anxiety, pain and lost working hours) by a sufficiently wide margin.11
One of the methods which allows for appropriate use of a technology is the RAND/UCLA method.12 This method has several phases: critical review of the references regarding the study theme; creation of mutually exclusive and manageable understandable settings based on the main variables implemented in the decision making and manageable for assessment during a reasonable period of time; selection of national experts who will form part of the panel, and scoring of the settings in two rounds, one individual and the other face to face.
Lack of evidence and uncertainty underlying arthroscopic treatment indications for femoroacetabular13 impingement justify conducting this study to identify which patients are candidates for an arthroscopic procedure for treatment of the femoroacetabular impingement using the RAND/UCLA methodology.
Material and methodsA review of the literature on the efficacy, effectiveness and safety of hip arthroscopy in patients with femoroacetabular impingement was carried out. A single systematic review was found to meet with this criteria7 and was distributed to the members of the subsequently formed expert group.
The group of experts was formed as a national and multicentric panel, with eleven professionals. They were all specialists in trauma and orthopaedic surgery, with different levels of experience in the use of the arthroscopic technique within the framework of the public health service. The main criteria for selection of the experts were: recognised leadership, geographical diversity and absence of a conflict of interests.14 The suggestions made by the study's clinical consultants were also considered, together with the proposals made by the Spanish Network of Health Service Technologies on request by the Agency for Healthcare Technology Assessment of Andalusia (AETSA). The panel members appear in Appendix I.
Clinical settings assessedThe experts reported the appropriateness of arthroscopy in a series of clinical settings. Scores were given on a scale of 1 to 9. When the score fell within the interval of 1 to 3, the use of the arthroscopy was considered as “inappropriate”; when it fell within the interval of 4 to6, it was “undetermined” and if it fell between 7 and 9 it was “appropriate”. The panellists gave independent, anonymous scores which were not made public.
The settings aimed to represent the clinical characteristics where a hip arthroscopy could be considered. They were defined by consultants, in an iterative process, based on their experience and the information from review of the literature. To ensure that the panellists interpreted in a similar way, a list of definitions of the terms used in these settings was given to them (Appendix II).
Setting classificationThe experts gave a score to the settings on two occasions or “rounds”, in accordance with the RAND/UCLA14 method. During the first round the panellists received the following documentation by electronic mail: the clinical settings, together with instructions for completing them, variable definitions and the review of the literature. Once scoring had been completed, the document was returned to the researchers with the scores.
Scores from the first round were statistically processed, by calculating the median of the scores for each setting. Furthermore the level of agreement in each setting was assessed, as described below.
These results were presented to the experts in the second round, which took place at a face-to-face meeting, which lasted a day. There were two moderators, who managed the meeting, but they did not score or intervene like the experts. In this second round each panellist had a document which contained their own scores from the first round, together with the completely anonymous distribution of scores from the other experts.
During the second round the panellists discussed the scores given and the settings, mostly focusing on the areas where agreement failed. They were also able to modify the structure of several settings to better reflect several clinical aspects.
Analysis of scoresFrom the scores given by the experts in the second round, the use of arthroscopy in each setting was classified as “appropriate”, “uncertain” or “inappropriate”. The classification was made in keeping with the median score and the level of agreement among them. In one setting it was considered that there was “agreement” if, as a maximum, three experts scored outside the interval of 3 points of the scale which contained the median. There was “disagreement” if four or more of the experts scored on the interval under the scale (1–3) and at least another four in the upper limit (7–9), and “undetermined” if none of the previous criteria were met.
A setting was considered to be “appropriate” when the median was ≥7 and there was no disagreement, “inappropriate” when the median was ≤3 and there was no disagreement and “uncertain” when the median was >3 and <7 or there was disagreement.
Statistical analysisThe panellists’ scores were listed in the frequency tables for each setting.
The link between the degree of appropriateness and the level of agreement was studied with contingency tables and by calculating the chi-square test.
To estimate the importance of each variable in the explanation of appropriate usage of arthroscopic intervention in femoroacetabular impingement, an ordinal logistical regression model was created in which the dependent variable was the appropriate use (appropriate, uncertain, inappropriate), and the independent variable were selected from those used to define the settings. The −2 log L coefficient was calculated as a criteria for the measurement of the validity of model match.
The Classification and Regression Tree (CART)15 analysis was applied. This tree formation technique for decision-making provides a summary of the results of large data bases with multiple categories. The main purpose of this type of non-parametric analysis is to summarise results so that they may be practical and interpretable.
Statistical analysis including the CART, was performed with the SPSS programme version 23.16
ResultsThe initial result obtained came from the analysis of the first round of scores. In this round agreement from the panellists was 17.3%.
After an extended debate at the face-to-face meeting of the second round (at which nine of the eleven panellists attended and two by teleconference),the panellists were able to modify the structure of the list of indications, reducing the number of clinical settings to assess from 768 to 192.
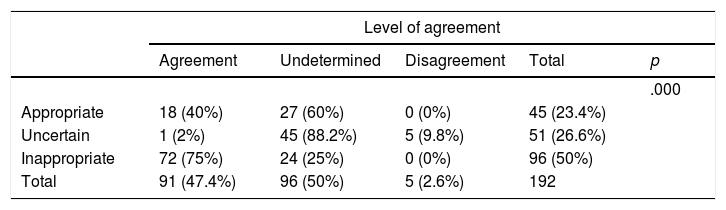
These 192 settings were again individually and anonymously given a score, obtaining an agreement between panellists of 47.4%. Disagreement obtained in this second round was very low (2.6%). It was also observed that 45 indications (23.4%) were considered appropriate, 51 (26.6%) uncertain and 96 (50%) inappropriate (Table 1).
Distribution of settings according to the classification of appropriate usage and level of agreement.
| Level of agreement | |||||
|---|---|---|---|---|---|
| Agreement | Undetermined | Disagreement | Total | p | |
| .000 | |||||
| Appropriate | 18 (40%) | 27 (60%) | 0 (0%) | 45 (23.4%) | |
| Uncertain | 1 (2%) | 45 (88.2%) | 5 (9.8%) | 51 (26.6%) | |
| Inappropriate | 72 (75%) | 24 (25%) | 0 (0%) | 96 (50%) | |
| Total | 91 (47.4%) | 96 (50%) | 5 (2.6%) | 192 | |
The percentages in brackets are calculated in rows, with the exception of those that appear in the “total” column which are calculated in accordance with the column.
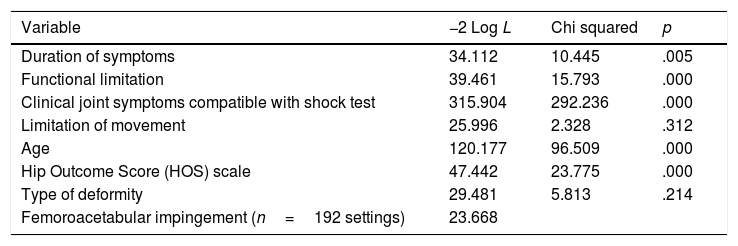
A logistic regression model was adjusted with each of the variables included in the settings of the second round, taking into consideration the degree of appropriateness (Table 2). The regression model used showed that the variables with the highest influence, in statistical order of relevance, in the determination of appropriate indication for hip arthroscopy in femoroacetabular impingement were joint symptoms compatible with shock test, age, hip outcome score (HOS) scale, functional limitation and symptom duration. As a whole, the variables included explained the 98.1% of variability of the level of appropriateness of the use of arthroscopy in femoroacetabular impingement.
Contribution of the setting variables for appropriateness of the hip arthroscopy in femoroacetabular impingement.
| Variable | −2 Log L | Chi squared | p |
|---|---|---|---|
| Duration of symptoms | 34.112 | 10.445 | .005 |
| Functional limitation | 39.461 | 15.793 | .000 |
| Clinical joint symptoms compatible with shock test | 315.904 | 292.236 | .000 |
| Limitation of movement | 25.996 | 2.328 | .312 |
| Age | 120.177 | 96.509 | .000 |
| Hip Outcome Score (HOS) scale | 47.442 | 23.775 | .000 |
| Type of deformity | 29.481 | 5.813 | .214 |
| Femoroacetabular impingement (n=192 settings) | 23.668 |
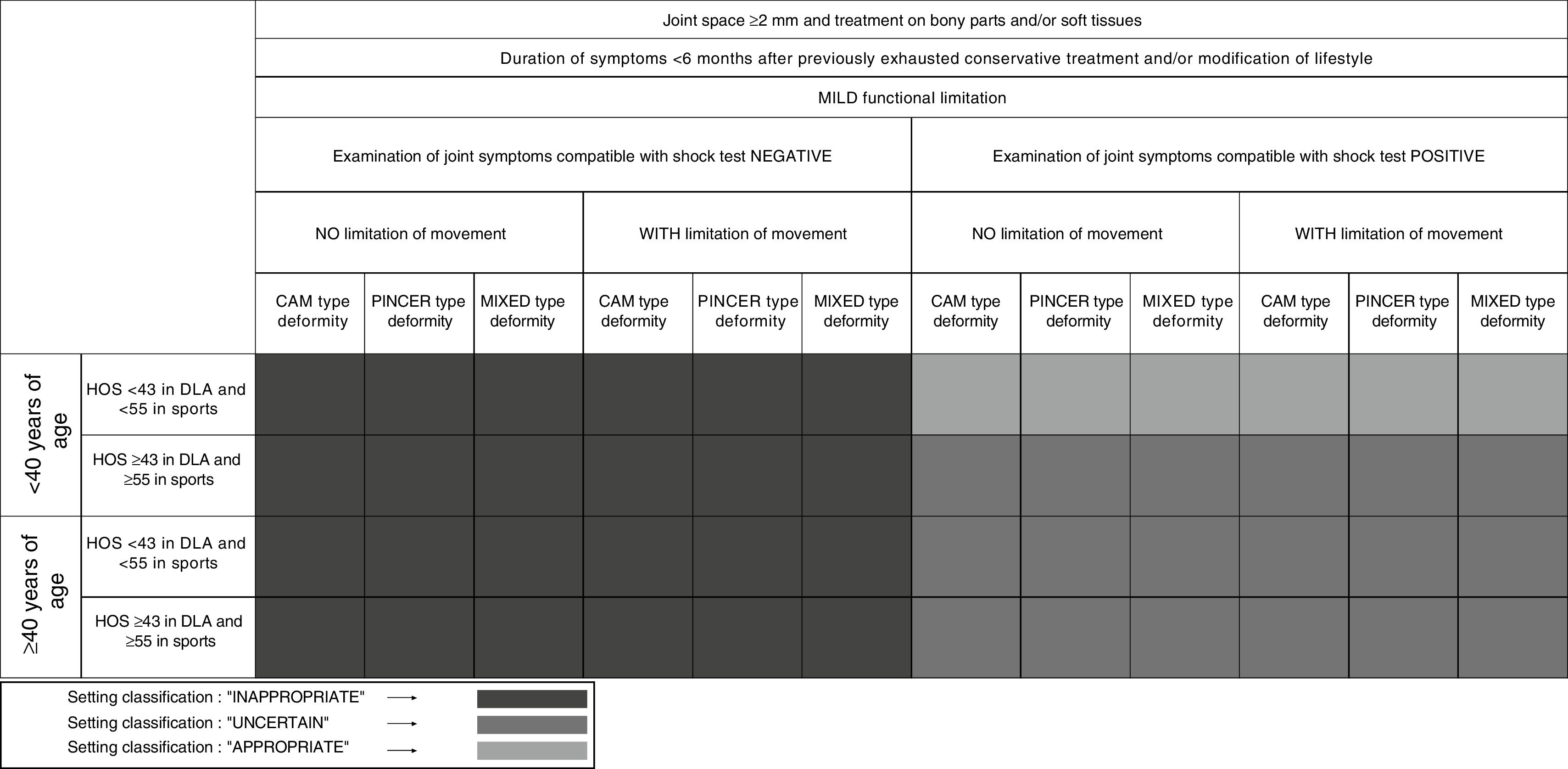
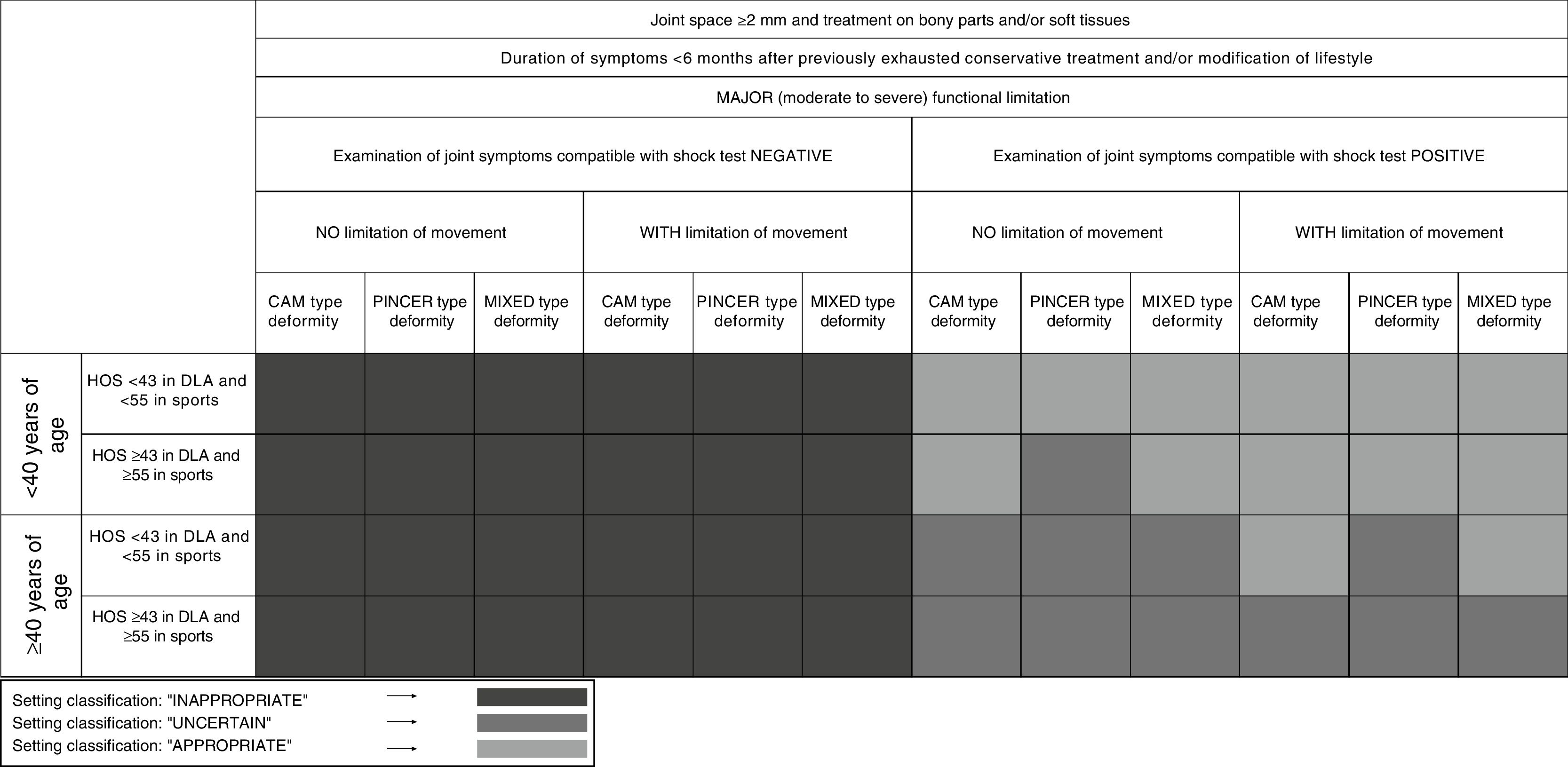
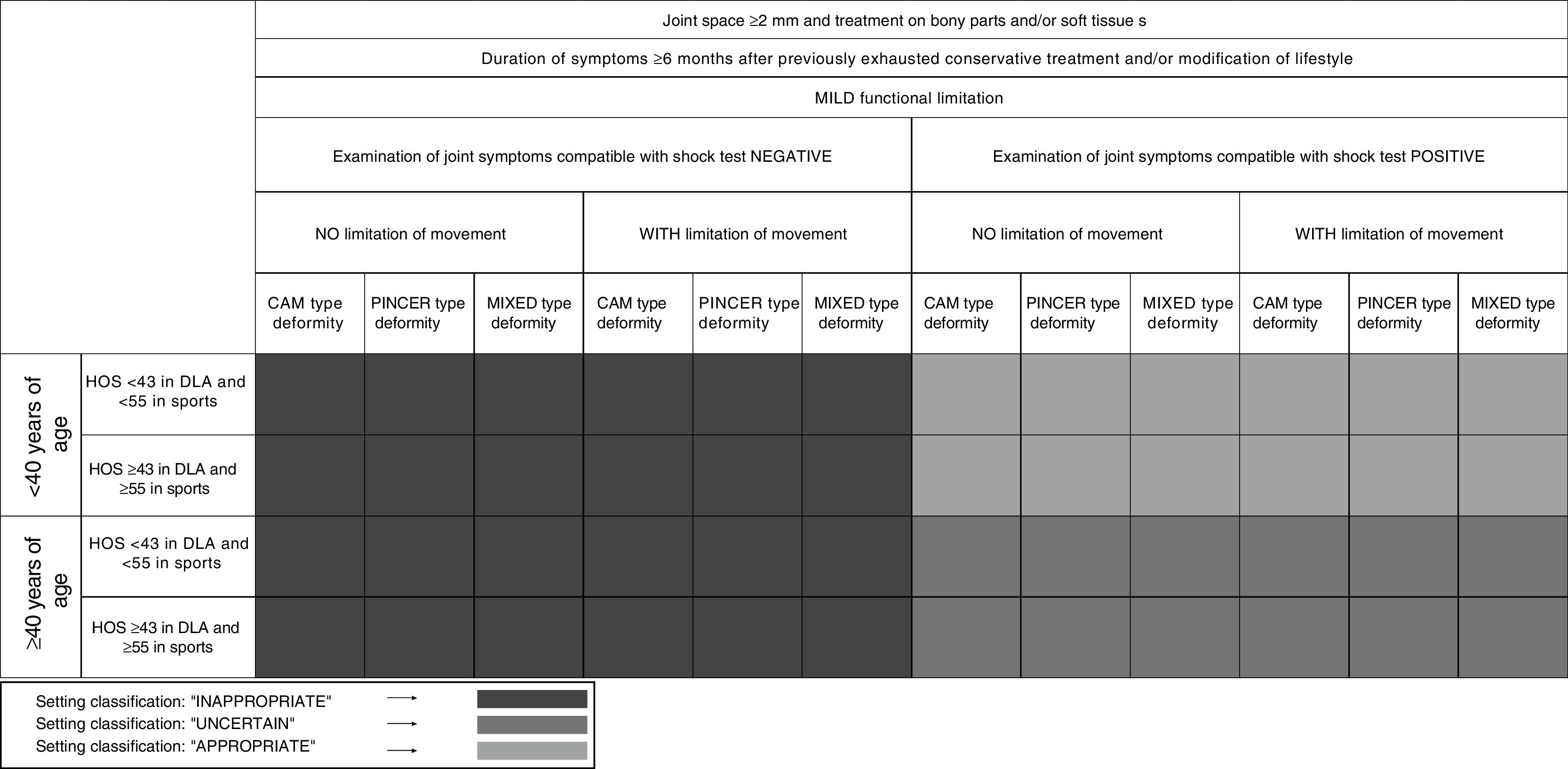
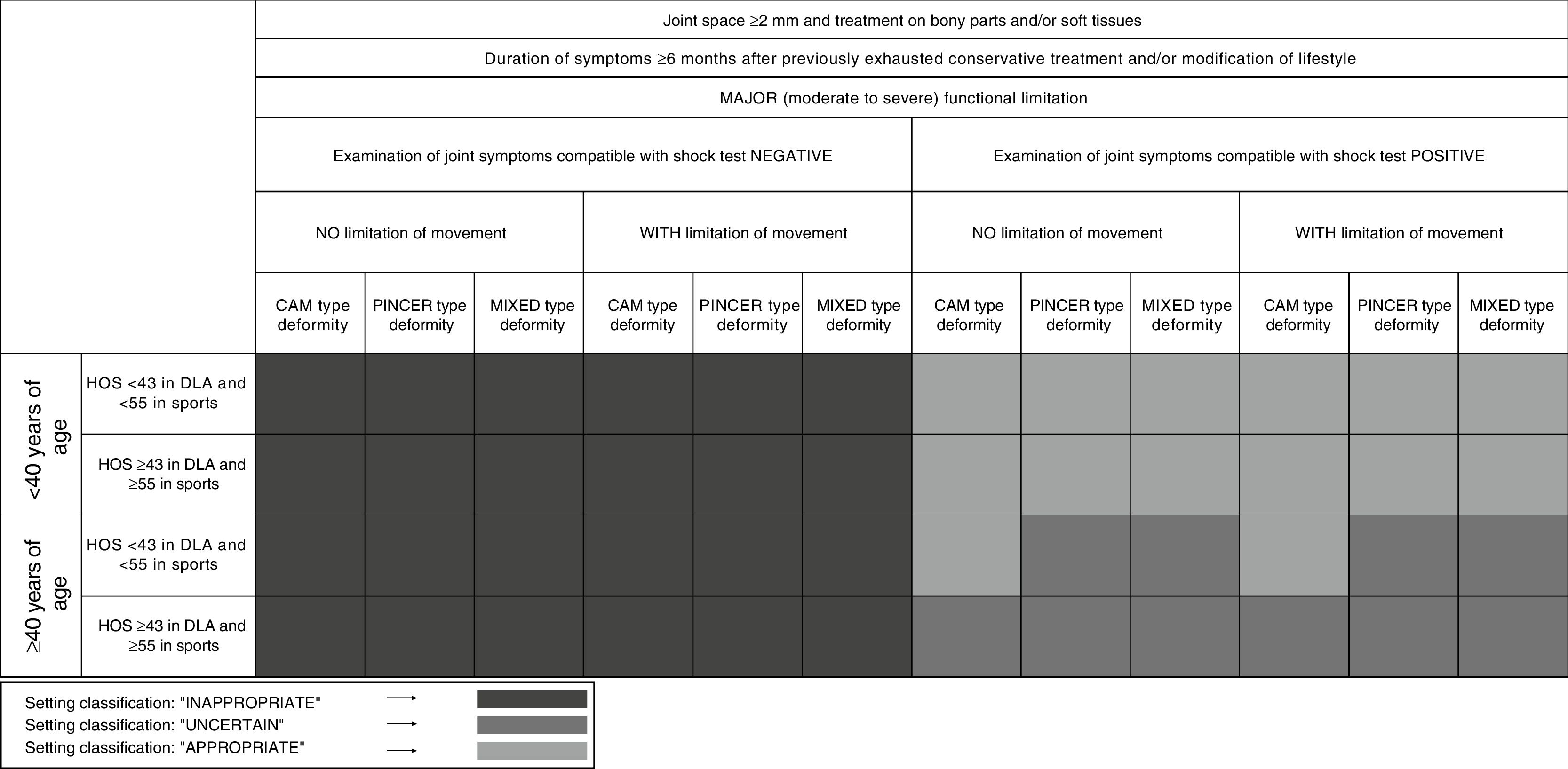
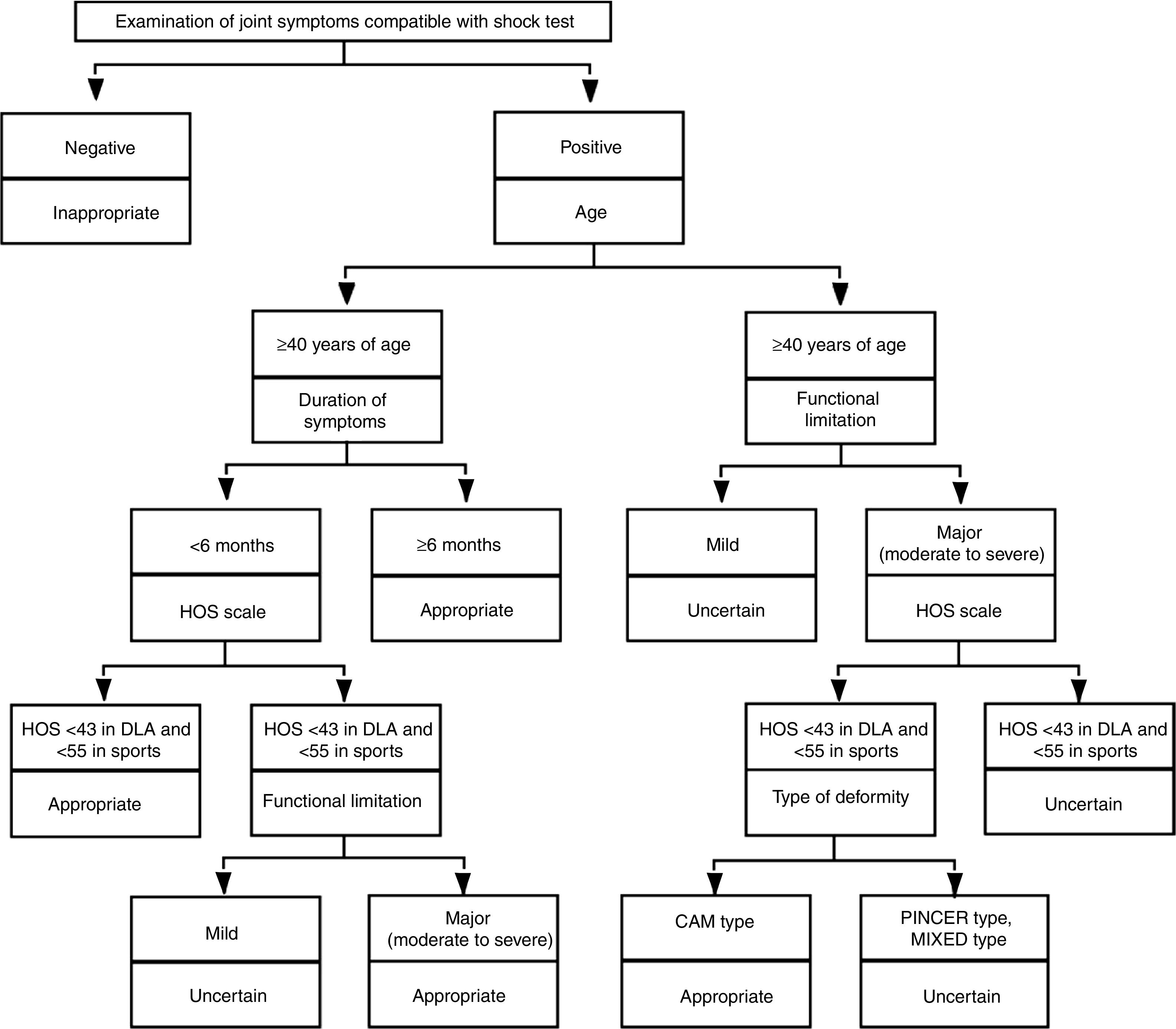
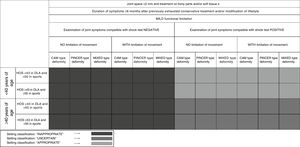
Figs. 1–4 contain the results of the development of the appropriate usage criteria for hip arthroscopy in femoroacetabular impingement. The criteria were presented in the form of a decision table.
As an example, the following may be observed in Figure 1: a patient with a joint space ≥2mm and treatment on the bony parts and/or soft tissue, with a duration of symptoms <6months, after previously exhausted conservative treatment and/or modification of life style, with mild functional limitation, joint symptoms compatible with negative shock test, with no movement limitations, a cam type deformity, <40 years of age and a score on the HOS scale <43 DLA and <55 in sports activities was considered inappropriate.
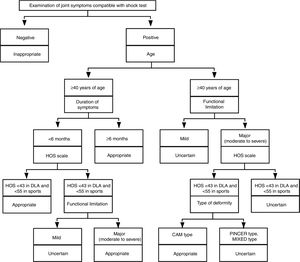
The criteria put forward in the panel of experts during the second round were summarised in the classification trees (Fig. 5). The overall classification error of the decision tree was 1.6%.
The decision tree on hip arthroscopy in the pathology of femoroacetabular impingement shows that when the joint symptoms compatible with shock test were negative, the indication for arthroscopy was considered inappropriate in all cases whereas when the joint symptoms compatible with shock test were positive, arthroscopy was considered appropriate or uncertain depending on the other variables.
DiscussionAt present, the number of hip arthroscopies has grown exponentially.6,17 This rapid increase in interventions has not been accompanied with consensus among professionals regarding indications. 18,19 In fact, one of the few publications located on this issue is that designed by the 2016 Warwick Agreement. This document was a major milestone, because it covered diagnostic criteria and the diverse therapeutic focal points of femoroacetabular impingement from a conceptual perspective.20
However, localised scientific evidence reported major inconsistencies with respect to specific surgical criteria as well as parameters and specific values. This impeded the identification of patient characteristics of those who were referred for hip arthroscopy as treatment for femoroacetabular impingement.21 This same information was conveyed by the consultants in meetings before the protocol design of our study. Although the benefits of the arthroscopic technique were pointed out so too was the pertinence and relevance of the availability of surgical criteria to help guide the referral of this technique.
As a result, the results of this study could lead to appropriate explicit criteria for the treatment of femoroacetabular impingement through arthroscopic surgery. For this, in this study we used the RAND/UCLA method which is able to combine whatever scientific evidence is available with the collective judgement of clinical experts. Its purpose is to establish the appropriate usage criteria for a medical or surgical procedure, depending on symptoms, medical history and results of specific tests for each patient.
One of the main strong points of the current study is precisely the use of the RAND/UCLA methodology as an established, validated and reliable tool for determining appropriateness.22 This methodology was validated on many occasions and indifferent procedures (arthroplasties, interventionist cardiology, vascular surgery, cataract surgery, …), either prospectively in studies with patients or using statistical procedures such as classification and regression tree models (CART).23–26 The use of original results from the panel, i.e. the application of 192 clinical settings may result in a somewhat tedious task in clinical practice. However, we validated the CART analysis techniques so as to be able to summarise the results in classification trees which would allow us to follow the branches and nodes they comprise, in a specific clinical situation, and thus classify this situation in as an appropriate, inappropriate or uncertain arthroscopic intervention similarly to how it would be performed when following a decision tree.
One major benefit of the RAND/UCLA method is the inclusion of a large number of settings, with consideration of many clinical variables on determination of appropriateness. This would allow for the generalisation of results to the majority of possible patients with femoroacetabular impingement who would potentially be suitable for surgical treatment using arthroscopic hip surgery.
The settings were selected to represent a wide range of possible indications of hip arthroscopy, although contemplating additional settings could have increased this range and adding further detail could have made the panel of experts less viable for the members and increased the difficulty in achieving relevant consensus.
This study also shows the areas of uncertainty where lines of future investigation may be developed, mostly where the panel has determined that performing arthroscopy is uncertain. This could help to identify questions where there is no available response. Furthermore, the panel of experts underlined the significance and potential usefulness of promoting a record of patients treated by arthroscopy and the identification of benchmarks for analysis of the results obtained and the application of the proposed criteria in this consensus.
During the face-to-face meeting, the panel of experts stated the need to use an appropriate evaluation scale in femoroacetabular impingement, which would be validated and viable in clinical practice. The panellists identified the HOS20,27 scale in its components of evaluation of everyday activities and sport (with a cut-off point of <43 and <55, respectively). It was also of note that the document used as a reference in nuances, modifications of settings and definitions in the face-to-face meeting was the consensual document, the 2016 Warwick Agreement,20 which on consideration by the experts as such, could serve as a starting point for future projects.
To sum up, we believe that these criteria for hip arthroscopy in patients with femoroacetabular impingement could assist in decision making within a surgical context, in appropriately selected patients.
ConclusionsHip arthroscopy was considered appropriate as surgical treatment for femoroacetabular impingement depending on the presence of the following criteria: joint symptoms, duration of symptoms, functional limitations, age of patient and HOS scale.
Level of evidenceLevel of evidence V.
Ethical disclosuresProtection of people and animalsThe authors declare that no experiments have been used on humans or animals for this research.
Data confidentialityThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article
FundingThis article is based on the results obtained in a project entitled: “Hip arthroscopy. Indications for appropriate usage” (available in: http://www.aetsa.org/download/publicaciones/01_AETSA_Artroscopia_cadera_DEF_NIPO.pdf). This project was financed by the Ministry of Health, Social Services and Equality, within the framework of the annual work plan of the Spanish Network of Agencies for the Evaluation of Technologies and Health Benefits of the National Health System.
Conflicts of interestThe authors declare no conflicts of interest.
| Name | Association |
|---|---|
| Dra. Ana Castel Oñate | Hospital Príncipe de Asturias (Alcalá de Henares, Madrid) |
| Dr. Eduardo García Cimbrelo | Hospital la Paz (Madrid) |
| Dr. Jorge Guadilla Arsuaga | HU Araba (Vitoria) |
| Dr. Miguel Hermida Sánchez | Estructura Organizativa de Xestión Integrada de Santiago de Compostela (Santiago de Compostela) |
| Dr. Óliver Marín Peña | Hospital Infanta Leonor (Madrid) |
| Dr. Carlos Martín Hernández | HU Miguel Servet (Zaragoza) |
| Dr. José Luis Pais Brito | HU de Canarias (San Cristóbal de La Laguna, Santa Cruz de Tenerife) |
| Dr. Francesc Pallisó Folch | HU de Santa María (Lleida) |
| Dr. José Sueiro Fernández | HU de Puerto Real (Cádiz) |
| Dr. Juan Tercedor Sánchez | HU Virgen de las Nieves (Granada) |
| Dr. Marc Tey Pons | Hospital del Mar (Barcelona) |
The panel of experts considered it a vital condition that the patients had a joint space ≥2mm and required treatment on the bony part and/or soft tissue.
• Duration of symptoms
The time which elapsed between the presentation of the symptoms and the moment of considering the possibility to use arthroscopy (once conservative treatment was exhausted, including changes in lifestyle). The following categories were suggested:
- –
< 6 months.
- –
≥ 6 months.
• Functional limitation
Restriction of movement of the joint to be assessed.
- –
Mild functional limitation: restriction in carrying out demanding movements.
- –
Major functional limitation (moderate-severe): restriction in carrying out everyday tasks.
• Clinical joint examination
This test was carried out with the patient lying down on their back. The hip was turned inward whilst simultaneously applying passive flexion up to approximately 90°, and was then adduced. The flexion and adduction enabled approach of the femoral neck and the acetabular ridge and two variables were recorded:
- –
Examination of joint symptoms compatible with shock test positive.
- –
Examination of joint symptoms compatible with shock test negative.
• Range of movement
In this variable, used in the examination for diagnosis, there were two categories:
- –
WITHOUT limitation of movement of the hip.
- –
WITH limitation of movement of the hip.
• Age
Complete years lived by the patient.
The following categories were considered:
- –
< 40 years.
- –
≥ 40 years.
• Hip Outcome Score (HOS)scale
Martin, Kelly and Philippon (2006) designed this assessment questionnaire of the hip with the sections for everyday life activities (HOS-DLA) and for practising sport (HOS-SSS). Two categories were estimated in this variable:
- –
HOS <43 in everyday life activities (DLA) and <55 for the sports subscale.
- –
HOS ≥43 in everyday life activities (DLA) and ≥55 for the sports subscale.
Original reference: Martin RL, Kelly BT, Philippon MJ. Evidence of validity for the hip outcome score. Arthroscopy 2006, 22(12):1304-11.
Reference of validation into Spanish: Seijas R, Sallent A, Ruiz-Ibán MA, Ares O, Marín-Peña O, Cuéllar R, Muriel A. Validation of the Spanish version of the Hip Outcome Score: A multicenter study. Health Qual Life Outcomes. 2014;12:70.
• Type of deformity
Three types of femoroacetabular impingement were identified:
- –
Cam type, which occurs due to the blocking of the aspherical appendage of the femoral head within the acetabular cavity.
- –
Pincer type, characterised by the lineal impact of the acetabular ridge against the head-neck union within the context of an overlap of the acetabulum which may be local (for example, in cases of acetabular retroversion) or global (in cases of coxa profunda or acetabular profusion).
- –
Mixed type, this type of impingement includes characteristics of the two above-mentioned lesions.
The presence of deformities would be considered using radiographic diagnosis, although when other tests are available, such as arthro magnetic resonance, they could also be indicated.28
Members of the panel of experts of hip arthroscopy can be found in the Appendix I.
Please cite this article as: Molina-Linde JM, Carlos-Gil AM, Benot-López S, Lacalle-Remigio JR, García-Benítez B, Delgado-Martínez A, et al. Desarrollo de criterios de uso adecuado para la artroscopia de cadera en pacientes con choque femoroacetabular. Rev Esp Cir Ortop Traumatol. 2018;62:328–336.