Developmental dysplasia of the hip (DDH) causes anatomical changes that cause early coxarthrosis. Although risk factors have been determined, the aetiology and physiopathology remains exactly unknown. Neonatal screening with physical examination and ultrasound have been established in order to diagnose this disease early in life. A diagnosis in the first months of life is essential as it enables a normal hip to form and prevent the appearance of early coxarthrosis. Treatment principles are to be able to reduce the hip without provoking avascular necrosis of the femoral head, and to normalise the acetabular development. Knowledge of the orthopaedic and surgical options is essential in order to achieve success in the treatment.
La displasia del desarrollo de la cadera provoca cambios anatómicos que dan lugar a una coxartrosis precoz. La etiología y la patofisiología de la displasia de cadera no se conocen con exactitud, aunque se han determinado factores de riesgo. Se han establecido programas de despitaje neonatal clínicos y ecográficos que lleven a un diagnóstico precoz de esta afección. Un diagnóstico en los primeros meses de vida es fundamental porque permite obtener una cadera normal y evitar la aparición de una coxartrosis precoz. El tratamiento debe conseguir reducir la cadera, evitando la aparición de una necrosis avascular de la cabeza femoral, y normalizar el desarrollo del acetábulo. Existen opciones ortopédicas y quirúrgicas que deben ser conocidas para lograr un éxito en el tratamiento.
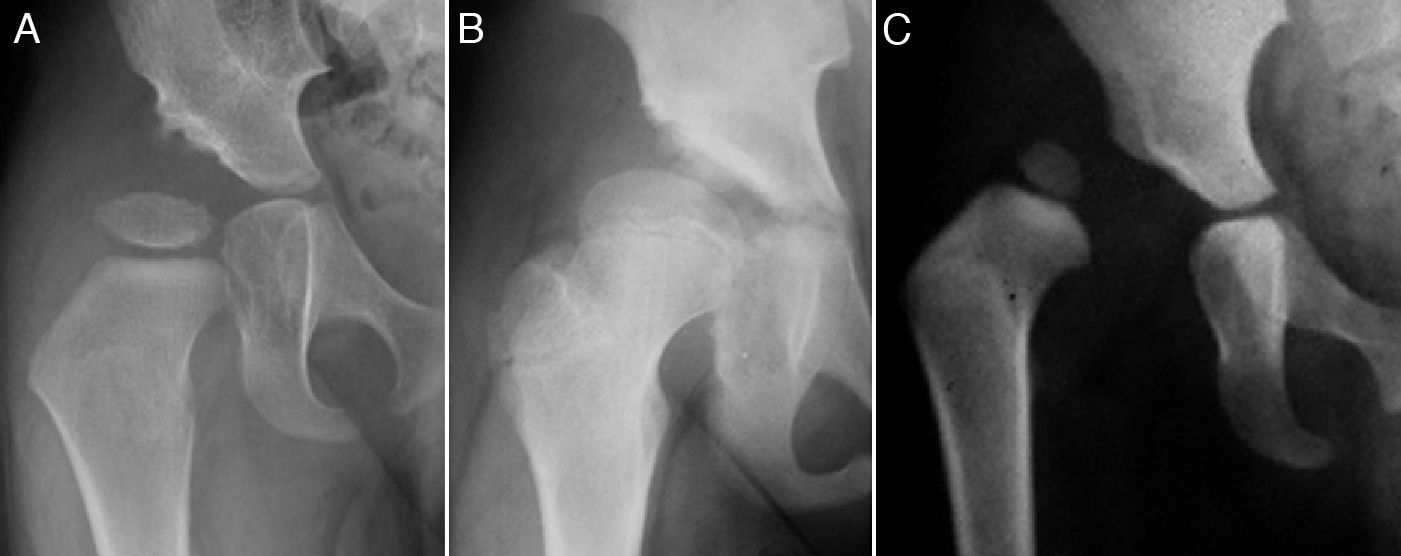
The term developmental dysplasia of the hip (DDH) includes a wide spectrum of abnormalities of the acetabulum and the proximal femur, including isolated dysplasia, subluxation and dislocation of the femoral head (Fig. 1).1–4 In dysplasia, there is an inadequate development of the acetabulum, the femoral head or both, although there is also a concentric relationship between the 2 articular surfaces. However, in subluxated hips, although there is contact between both articular surfaces, the femoral head is not centred on the acetabular cavity.5 In the case of dislocation the femoral head is completely out of the acetabulum.6
AnatomyNormal hipThe hip consists of the acetabulum, the femoral head and the soft tissues comprising the joint capsule, the labrum, the ligamentum teres or round ligament and pulvinar tissue. The acetabulum is a hemispherical cavity formed by the acetabular cartilage, triradiate cartilage, ischium and ilium. The acetabular cartilage continues medially as the triradiate cartilage and together they form the acetabular cartilage complex.7 Both separate the ilium, ischium and pubis. The acetabular cartilage forms the outer two-thirds, while the triradiate cartilage, ilium and ischium form the non-articular medial third. The triradiate cartilage is responsible for the growth of the acetabulum and the innominate bone, maintaining the relationship with the growth of the femoral head.8 Concavity of the acetabulum is developed by the presence of the convex femoral head.9
Within the acetabulum we find the pulvinar; fibrofatty tissue covering its non-articular part.7 The round ligament (ligamentum teres) joins the femoral head to the acetabular floor. On the periphery of the acetabulum is the labrum, a triangular and circumferential fibrocartilage which increases the depth of the acetabulum.2 The relative size of the labrum with respect to the femoral head is greater during childhood than in adult life, reflecting the importance of the labrum in hip stability during paediatric age.2 The labrum is located throughout the entire periphery of the acetabulum except for the lower region, where the transverse ligament is situated. The joint capsule is inserted into the outer side of the ilium bone, immediately adjacent to the labrum.
For its part, the proximal femur is formed only by cartilage at birth. A cartilaginous isthmus connects the femoral and trochanteric growth plates along the lateral edge of the femoral neck. The ossification centre of the femoral head appears at about 6 months of age, whilst the ossification centre of the greater trochanter does so at 5–6 years of age. There is a femoral anteversion at birth which decreases with growth. A mean femoral anteversion of 31° at 1 year of life has been described, which decreases to 15° at 16 years of age.10 The cervicodiaphyseal angle also decreases with age, going from a mean value of 136° at 1 year of life to a mean value of 127° at 18 years of age.4
Dysplastic hipA series of changes of variable magnitude take place in the acetabulum, proximal femur and soft parts of dysplastic hips. These changes occur over time due to age and load supported, and involve adaptive changes in the joint. There is a flattening of the acetabulum along with an increase of the thickness of its bony floor. Pulvinar fat, round ligament, labrum and joint capsule become hypertrophied and the transverse ligament becomes inverted.3 The abnormal pressure of a dislocated or subluxated femoral head on the labrum causes hypertrophy of the fibrocartilage and forms fibrous tissue. This voluminous labrum is called limbus and is often everted and adhered to the inner side of the joint capsule.3 The labrum may also be inverted in dislocated hips, thus preventing their reduction.
In some cases there is a crest, known as neolimbus, in the posterosuperior part of the articular cartilage, which is formed by a thickening of the acetabular hyaline cartilage.3 The neolimbus appears in response to excentric pressure by the femoral head and separates 2 cavities: the innermost part corresponds to the primary acetabulum, whilst the outer part is part of the secondary acetabulum. While the primary acetabulum is hypoplastic due to the absence of stimuli from the femoral head,9 the secondary acetabulum, formed by the posterosuperior quadrant of the acetabulum, the everted labrum and the joint capsule, holds the subluxated femoral head.3 The neolimbus does not represent an obstacle for reduction and disappears spontaneously once the hip has been reduced.
Regarding the proximal femur, there is a shortening of the femoral neck in hip dysplasia, as well as a deformity of the head and a delay in the appearance of the secondary ossification nucleus.11 Although the existence of coxa valga is widely accepted, some authors maintain that the opposite is true and that the proximal femur adopts an arrangement in varus rather than valgus.11 There is also some controversy about the presence or absence of an increased femoral anteversion.12
AetiologyIn order for an adequate development of the hip to take place, it is necessary for the femoral head to be correctly centred on the acetabulum and for a balance to exist between the growth of the acetabular and triradiate cartilages.8,9 Any change in this equilibrium, either during the intrauterine period or during postnatal development, will lead to an altered development of the hip.9 Given the low incidence of DDH among foetuses aborted before week 20,13 it is conceivable that these problems occur during the last months of pregnancy.
The aetiology of developmental dysplasia of the hip is multifactorial and has been related to hormonal, genetic and mechanical factors. The “hormonal theory” is based on the influence that sex hormones have on the connective tissue of the joint capsule. Oestrogen inhibits the synthesis of collagen and promotes the crosslinking of its fibres and the formation of elastin.14 Experiments have shown that oestrogen administration decreases the collagen content of the joint capsule of the hip, while progesterone increases it.14 Thus, we may conclude that oestrogen hinders hip dislocation, while progesterone facilitates it.15 There is a hormonal joint laxity in the latter part of pregnancy which makes this period into a fundamental step in endocrinology theory.15 However, it has not been possible to associate the presence of DDH with changes in urine oestrogen concentration, serum beta-estradiol concentration or relaxin concentration in serum or in umbilical cord blood.16
The “mechanical theory” maintains that persistently applied forces can cause a deformity which occurs more easily during periods of growth. Due to its elevated growth rate and its relative plasticity, the foetus is highly vulnerable to such deformities.13 The deforming forces can be caused by the abdominal or uterine musculature, by a maintained position, especially in hip flexion and knee extension, or by a decrease of the free space available to the foetus, either because the foetus is large or because the volume of amniotic fluid is decreased.3,13,14
Genetic factorsAlthough there have been no adequate studies regarding the genetic factors of DDH, the concentration of cases within families described in the literature suggests a genetic susceptibility. A relative risk of 12.1 for first-degree relatives and 1.74 for second-degree relatives has been described.17 Moreover, there is a concordance of 43% among monozygotic twins which decreases to 3% for dizygotic twins. In addition to familial concentration, the incidence of DDH among females doubles that among males,17 which could be partially explained by a genetic susceptibility, a favouring hormonal environment or a higher incidence of breech presentation. These data highlight the contribution of genetic factors to the aetiology of the disease.
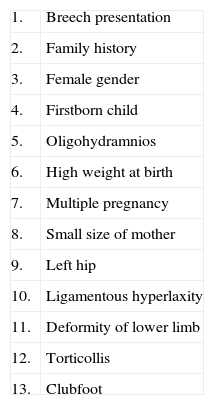
Although the exact aetiopathogenesis of DDH is unclear, some risk factors are known (Table 1). There are factors related to space problems for the foetus, including the presence of oligohydramnios and its various causes (arterial hypertension, Potter syndrome, etc.),13 multiple pregnancies or mothers with short stature. Other factors are related to an increase of the deforming forces: breech presentation due to maintaining a position with knee extension and hip flexion,18 being a firstborn child, since the relaxation of the uterus and the abdominal wall is less in the first pregnancy,13 the left hip, since the most frequent intrauterine position is with left leg adduction against the coxis13 and the presence of ligamentous hyperlaxity. Other risk factors include female gender, probably due to a favouring hormonal environment and an increased incidence of breech presentation17,18 and family history of hip dysplasia, as a result of genetic susceptibility.17,18
Risk factors for the development of hip dysplasia.
| 1. | Breech presentation |
| 2. | Family history |
| 3. | Female gender |
| 4. | Firstborn child |
| 5. | Oligohydramnios |
| 6. | High weight at birth |
| 7. | Multiple pregnancy |
| 8. | Small size of mother |
| 9. | Left hip |
| 10. | Ligamentous hyperlaxity |
| 11. | Deformity of lower limb |
| 12. | Torticollis |
| 13. | Clubfoot |
Although the association of DDH with the presence of torticollis seems clear,13 there is currently some controversy regarding the association of DDH with the presence of deformities such as clubfoot or adduct metatarsal.19 The association of DDH with an increased weight at birth has also been discussed.18
The most important risk factors associated with the presence of abnormalities on ultrasound scans at birth are breech presentation, a family history of DDH and female gender.20
However, most children with DDH21 and the majority requiring treatment20 do not present risk factors.
Natural historyThe term DDH encompasses a wide spectrum of disorders: instability of the hip, acetabular dysplasia and hip subluxation and dislocation.1 Hip dysplasia causes its instability in the first months of life, which is evidenced by the Barlow and Ortolani manoeuvres. A prevalence of neonatal hip instability of 1–1.5% has been described among living newborns,22 as well as an incidence of 5 cases per 1000 living male births and 13 per 1000 living female births.22
Most unstable hips in the neonatal period are resolved spontaneously during the first weeks of life.23 This spontaneous resolution seems to be the result of an increased muscle tone or a reduction in the amount of relaxin. In fact, only 1.2% of cases of neonatal hip instability require treatment.24 Moreover, it has been demonstrated that most ultrasound abnormalities observed during the first days of life, which are present in 6.6% of explored hips, become resolved spontaneously.20 Cases which are not resolved spontaneously are considered as persistent dysplasia. A rate of ultrasound evidence of persistent hip dysplasia (therefore, requiring treatment) of 3 cases per 1000 live births has been described at 6 weeks of life.20 Furthermore, a rate of radiological evidence of persistent hip dysplasia of 1.5 cases per 1000 live births at 5 months of life has also been reported.25
Untreated persistent developmental dysplasia of the hip leads to a series of anatomical changes which alter joint biomechanics, increasing tension on a smaller contact area.6 Elevated articular pressures maintained for long periods of time cause degeneration of the articular cartilage and lead to early coxarthrosis. DDH is the cause of 2.6–9.1% of all total hip prostheses implanted at any age,26,27 and the most common cause among young patients (21–29%).22,27 The presence of subluxation has proven to be the most relevant factor, since it almost invariably leads to the development of coxarthrosis.28 The natural history of acetabular dysplasia in the absence of subluxation is difficult to predict because its true incidence is unknown. Nevertheless, there is a clear association of acetabular dysplasia with coxarthrosis.22 In cases of complete dislocation, the presence of a secondary acetabulum is the key factor for the development of coxarthrosis.28 Most patients who do not present a secondary acetabulum maintain an acceptable range of motion with little functional disability. The reason why some complete dislocations develop a secondary acetabulum and some do not is currently unknown. Neonatal hip instability is associated with a 2.6 times higher risk of requiring a hip prosthesis during young adulthood, compared with stable hips at the time of birth.22 The results of hip assessment scales are good until degenerative changes appear in the joint.28
In addition to the onset of coxarthrosis, patients suffering complete unilateral dislocation develop a length discrepancy in the lower limbs, unsteady gait, postural scoliosis, hip deformity in flexion and adduction and valgus deformity of the ipsilateral knee which may cause pain and lead to the development of gonarthrosis.28 Patients suffering bilateral dislocations develop lumbar hyperlordosis and altered gait. There is also a limitation of hip abduction. The functional outcomes of patients with unilateral or bilateral dislocations are similar.28 There is no association between the level of dislocation and the result of hip assessment scales, development of a secondary acetabulum, back pain or ipsilateral knee problems.28
DiagnosisSuccess in the treatment of hip dysplasia involves an anatomical reduction of the joint and the restoration of growth and normal development of the acetabulum.5 As children develop, reduction becomes more difficult and the potential of the acetabulum to recover its growth decreases, thereby reducing the chances of success.29 Treatment in the first months of life is simple and has a very good prognosis, thus making early diagnosis a fundamental element in the treatment of DDH.
Hip instability in the neonatal phaseEarly diagnosis is based on the demonstration of an unstable hip through the Barlow and Ortolani manoeuvres.23,30 The Barlow manoeuvre, consistent in abducting the hip and pushing in the posterior direction attempting to dislocate the hip towards posterior, shows the presence of a reduced but dislocatable hip,23 whereas the Ortolani manoeuvre consists in abducting the hip and pushing the greater trochanter area in the anterior direction and indicates the presence of a subluxated or dislocated but reducible hip.30 The Ortolani manoeuvre is the most useful procedure to detect instability.30–33 Universal screening for hip dysplasia has been established using clinical examination as a part of the physical examination protocol for newborns. The accuracy of clinical examination increases with practice, so that while very reliable in expert hands, it may be less so in the hands of a novice or inexperienced person. Although an incidence of neonatal hip instability of 5 cases per 1000 living male births and 13 cases per 1000 living female births has been described,22 this incidence decreases to 1 in 2000 living births when children are explored by an experienced paediatric orthopaedist.20 In addition, the isolated finding of “clicking” in the hip of newborns is not considered pathological.34 Therefore, at present the recommendation is to refer all patients with clinical suspicion or significant risk factors (breech presentation or family history) to paediatric orthopaedic consultation.
Clinically, a difficulty in hip abduction can also be observed. We must bear in mind that dislocated but irreducible hips (such as teratological dislocations, for example) will not show hip instability, but rather difficulty in abduction, upon physical examination. Therefore, in addition to the Barlow and Ortolani manoeuvres, hip abduction must always be examined.
Godward and Dezateux35 studied children under 5 years who underwent surgery for DDH and described how clinical screening was not able to detect dysplasia during the first 3 months of life in 70% of cases. Furthermore, it has been reported that 92% of patients who underwent hip prosthesis implantation as a result of dysplasia showed no hip instability during neonatal exploration.22 Therefore, it could either be concluded that neonatal clinical screening does not achieve the desired results or that there is a type of hip dysplasia with late onset which is not present in the neonatal period, at least clinically. Universal ultrasound testing has been proposed as a means to improve neonatal screening and reduce the incidence of delayed diagnoses which currently exists with clinical examination. However, randomised clinical trials have shown that ultrasound testing does not reduce the incidence of late diagnosis.36 The current consensus is to perform an ultrasound test only in those cases where doubt remains after physical examination or in patients with significant risk factors.37
Physical exploration after the neonatal phaseThe prevalence of hip instability upon physical examination decreases after the first week of life as a result of increased muscle tone.23 However, the incidence of asymmetry in hip abduction increases as the child grows.25 Although physical examination for DDH in the neonatal period is based on the observation of an unstable hip through the Barlow and Ortolani manoeuvres, a limitation of abduction is the most important clinical sign in children aged 2–3 months, especially when it is unilateral.38 Another sign that can be observed by physical examination is a discrepancy in leg length, which is manifested through the Galeazzi sign. Thigh fold asymmetry is not a very reliable sign, as it is present in 30% of children with normal hips, and yet it is not present in all children suffering DDH.1 Once children have started to walk they may present a limp or hyperlordosis of the lumbar spine.
Imaging diagnosisUltrasoundRegarding imaging diagnosis, the most commonly used methods are ultrasound and radiography. Ultrasound is useful in the first months of life. Graf39 described an evaluation method based on the morphology of the hip which requires 2 angles to be calculated: the alpha angle, formed by the ilium and a line going from the promontory to the point in the acetabulum without an acoustic shadow, corresponding to the triradiate cartilage; and the beta angle, formed by a line going from the promontory to the tip of the labrum.39 This author classified hips into 4 groups according to the findings. On the other hand, Terjesen et al.25 proposed a dynamic evaluation method which emphasised the importance of instability and the percentage of head coverage. It has been reported that dynamic assessment of hip stability is the only ultrasound technique showing a significant relationship with the outcome.
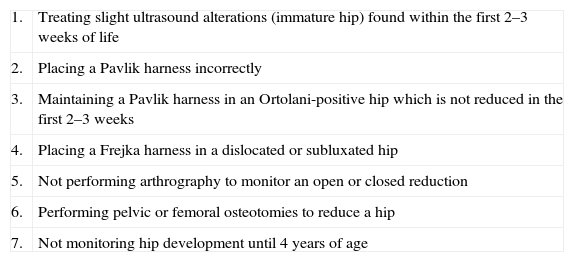
There is, as yet, no clear position on the natural history of ultrasound findings or whether patients with pathological findings should be treated. We must bear in mind that 96% of cases showing abnormalities on ultrasound tests performed during the first week of life become spontaneously resolved within 6 weeks.20 For this reason, we recommend conducting ultrasound screening between the third and sixth weeks of life (Table 2).
Frequent errors in treatment.
| 1. | Treating slight ultrasound alterations (immature hip) found within the first 2–3 weeks of life |
| 2. | Placing a Pavlik harness incorrectly |
| 3. | Maintaining a Pavlik harness in an Ortolani-positive hip which is not reduced in the first 2–3 weeks |
| 4. | Placing a Frejka harness in a dislocated or subluxated hip |
| 5. | Not performing arthrography to monitor an open or closed reduction |
| 6. | Performing pelvic or femoral osteotomies to reduce a hip |
| 7. | Not monitoring hip development until 4 years of age |
When the ossification centre is present, it appears as an acoustic shadow which darkens the medial structures and hinders the ultrasonographic evaluation of the hip. For this reason, plain radiography is considered the imaging test of choice in DDH after 4 months of life.34 A series of radiographic measures have been described to assess the anatomical configuration of the acetabulum: acetabular index, acetabular Sharp angle, ACM angle and acetabular floor width.40
The acetabular index and acetabular Sharp angle reflect the inclination of the acetabular roof, while the ACM angle is useful in assessing acetabular depth.40 These angles show higher values than normal in patients suffering dysplasia, reflecting a flattening of the acetabulum.29 In addition, DDH also causes an increase in the thickness of the acetabular floor.
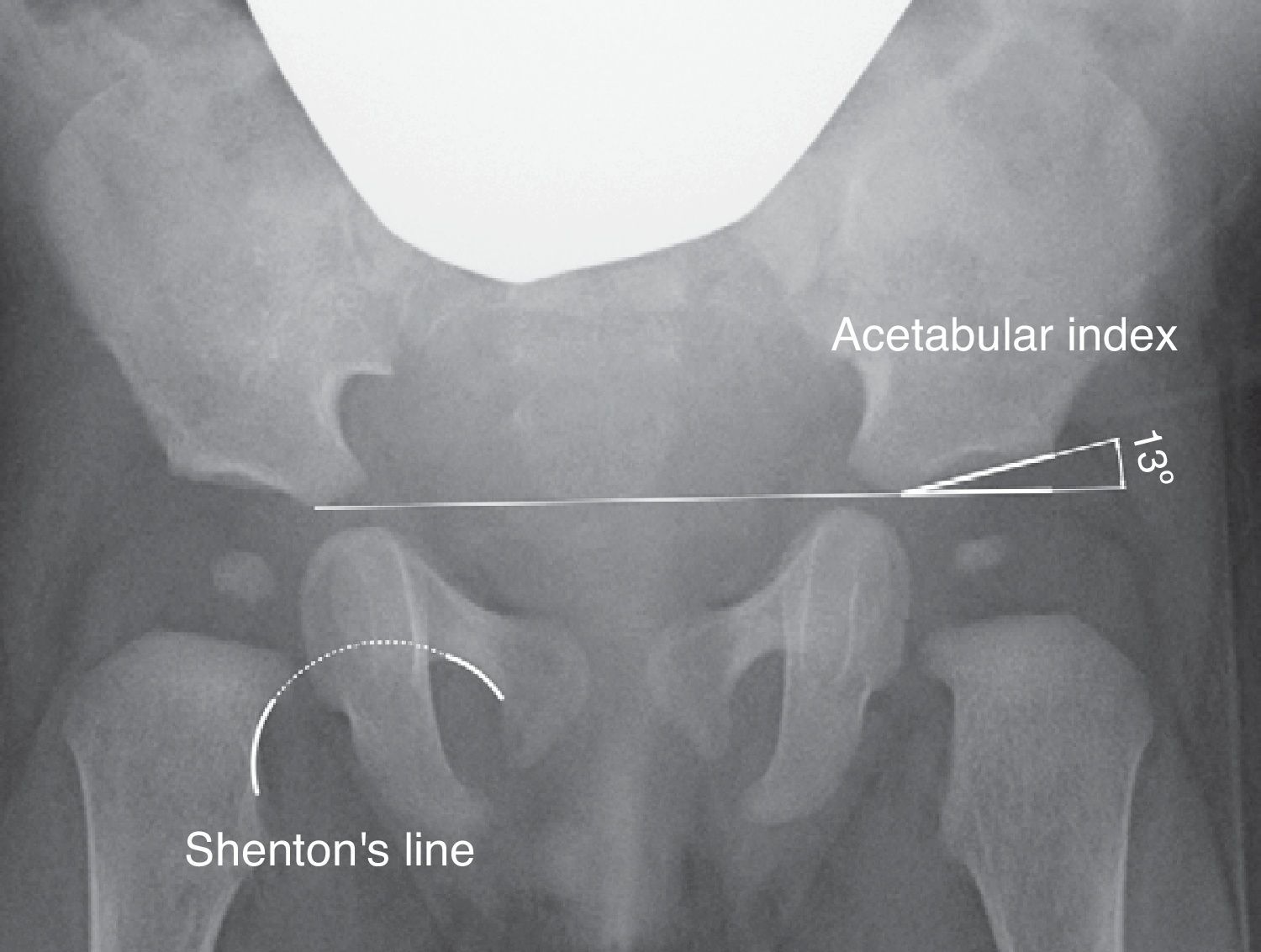
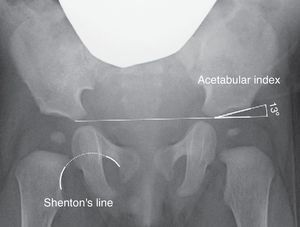
The acetabular index measures the inclination of the acetabular roof and is the most commonly used measure in the assessment of acetabular morphology, although its value can be altered by the position of the pelvis (Fig. 2).40 The acetabular index presents a range of values considered normal. In general, the upper limits considered as normal are 30° in children under 1 year, 25° in children aged between 1 and 3 years, and 20° after 3 years of age.29 Some authors consider all values exceeding 30° to be pathological.41 However, the confidence interval of intraobserver variation is ±6°, whereas the confidence interval of interobserver variation is ±5.5°.42 For this reason, the progression of values in a series of radiographs is considered to be more relevant than the absolute value of an isolated measurement.42,43
The acetabular Sharp angle is also useful in assessing the inclination of the acetabular roof.40 It is used in older patients, when the triradiate cartilage becomes ossified and the acetabular index cannot be calculated.
Moreover, there are other radiographic measurements which assess the relationship of the proximal femur and acetabulum, such as Shenton's line, the Wiberg centre-edge angle and the acetabular coverage. Shenton's line is the arch formed by the lower edge of the femoral neck and the upper edge of the obturator foramen when the hip is anatomically reduced (Fig. 2). Shenton's line is the most widely used measurement to assess the relationship between the proximal femur and acetabulum, especially after 2 years of life.40 The Wiberg centre-edge angle reflects the coverage of the femoral head. Values greater than 25° are considered normal in adults, while values below 20° are considered pathological. However, between the ages of 3 and 17 years, values less than 15° are considered pathological.44 The Wiberg centre-edge angle presents great variability in the first 3 years of life due to the difficulty in locating the centre of the femoral head.44 In hip subluxation it is possible to observe an interrupted Shenton's line and a decreased centre-edge angle.6 By contrast, Shenton's line remains intact in acetabular dysplasia, although the centre-edge angle is still decreased. In hip dislocation, Shenton's line is interrupted due to the posterosuperior dislocation of the femoral head, whilst it is not possible to calculate the centre-edge angle.
The Severin classification evaluates acetabular dysplasia, femoral head deformity and subluxation in the radiographs of hips which have reached skeletal maturity.45 This classification presents a good correlation with long-term radiological, clinical and functional hip results.
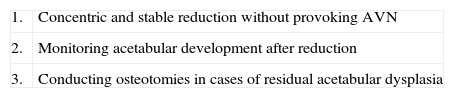
TreatmentSuccessful treatment involves achieving and maintaining an anatomical reduction of the joint and recovering a normal development of the acetabulum. Treatment of DDH could be summarised as follows (Table 3):
- (1)
First, we must obtain a stable and concentric reduction of the hip, avoiding complications such as avascular necrosis of the femoral head.
- (2)
Second, we must monitor acetabular development occurring after hip reduction through serial radiographs. The stimulus of anatomical and stable reduction of the femoral head may normalise the acetabulum.46 It has been reported that evolution of the acetabular index is the most reliable parameter to predict the presence or absence of residual acetabular dysplasia at the end of growth.
- (3)
Third, it is necessary to perform pelvic and/or femoral osteotomies in cases with residual hip dysplasia. It is generally considered that the potential for acetabular growth decreases significantly after 4 years of age and, along with it, so does the possibility that a simple hip reduction may achieve normalisation of the acetabulum.29 Pelvic osteotomies are performed from 3 to 4 years of age with the aim of improving the configuration of the acetabulum. Performing a pelvic or femoral osteotomy with the intention of reducing or stabilising a hip is a relatively frequent error.
During the first months of life, hip reduction is relatively simple. Moreover, during this period the stimulus of maintaining a reduced hip achieves normalisation of the acetabulum by itself in most cases. Pavlik47 showed that hip and knee flexion caused a spontaneous and atraumatic reduction and abduction of the hip, maintaining its active mobility and preventing avascular necrosis of the femoral head. In contrast to other treatment options, Pavlik considered active mobility as the most relevant therapeutic factor. The Pavlik harness allows active hip mobility in the safety zone, whose limits are a minimal abduction under which redislocation occurs (approximately 30°) and a maximum abduction above which the risk of avascular necrosis of the femoral head increases (approximately 60°). The success rate of the Pavlik harness reached 95% in cases of acetabular dysplasia or hip subluxation and 80% in cases of dislocation.48 The Pavlik harness is the most commonly used method in the treatment of DDH in children from the time of birth until approximately 6–10 months of age, depending on various authors (Fig. 3).47–49 After these ages, a brace which maintains a fixed position is indicated.
Figure A shows a 5-month-old girl with a Pavlik harness. The anterior strap flexes the hip 90°, causing hip abduction. This hip abduction is determined by the flexion of the hip and knee, rather than by the posterior strap, which is designed simply to prevent the thigh from falling into adduction. The harness allows hip mobility within a safe range. Figure B shows a newborn with a misplaced harness. Hip abduction is excessive and is determined by the posterior strap rather than by the joint flexion of the knee and hip. This excessive hip abduction increases the risk of avascular necrosis of the femoral head.
A rate of hip reduction between 63% and 92% of cases has been described with the Pavlik harness in cases of dislocation.48,50 Use of the harness should be discontinued if hip reduction has not occurred spontaneously within the first 2–4 weeks of treatment, as it increases the incidence of complications.51 Ultrasound testing is useful to confirm spontaneous reduction, although clinical examination has proven sufficient. A number of factors have been linked to failure by the Pavlik harness to achieve reduction: dislocated hips which are not reducible with the Ortolani manoeuvre, greater displacement of the femoral head, the presence of an inverted labrum, a high beta angle, a decreased percentage of femoral coverage, an acetabular index greater than 36°, presentation after the seventh week of life and bilateral dislocation.52
Complications associated with the Pavlik harness are minimal, provided it is used correctly.47 The incidence of avascular necrosis, the most feared complication, is almost inexistent.47,50 However, the incidence of avascular necrosis of the femoral head increases considerably if the harness is placed with excessive abduction (Fig. 3).49 Placement of the harness with excessive flexion may cause an inferior dislocation or transient paralysis of the femoral nerve.49 Other complications associated with the use of the Pavlik harness, such as worsening of acetabular dysplasia and the appearance of brachial palsy, have also been described.
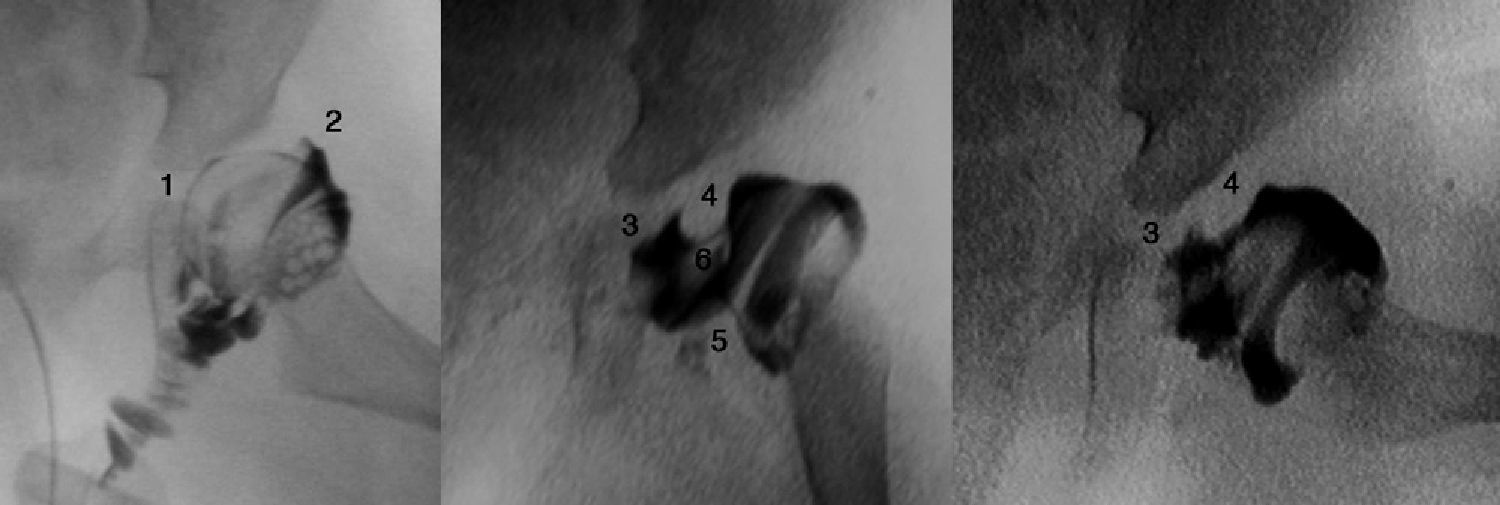
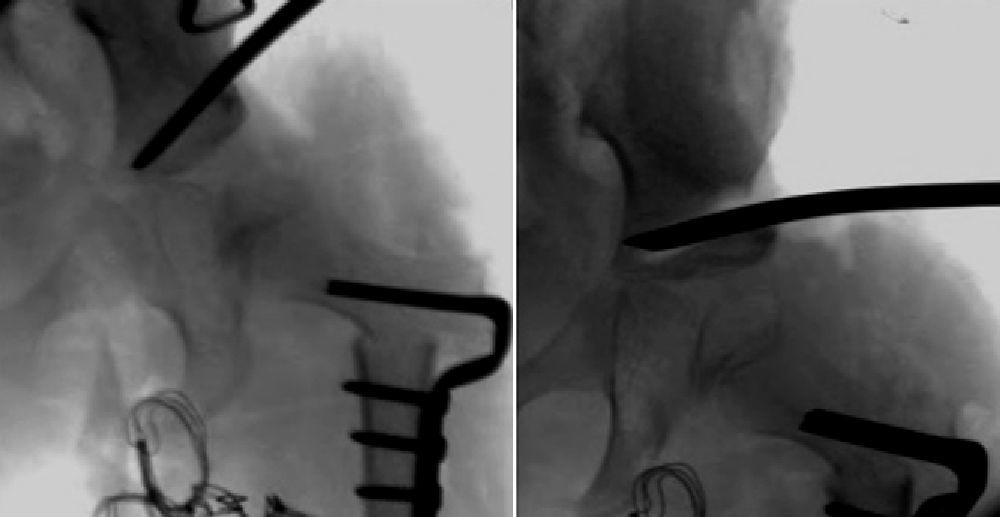
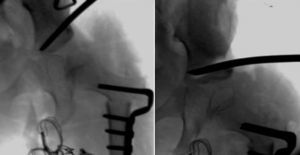
Difficulty to achieve reduction increases with age, in turn decreasing the efficiency of the Pavlik harness. Arthrography accurately assesses the quality of the reduction, as it reveals the soft parts of the joint, as well as the shape and size of the cartilaginous part of the acetabulum and the femoral head (Fig. 4).53 The reduction should be concentric and stable in a functional position. In cases where arthrography does not reveal an anatomical reduction, an open reduction must be performed, releasing intraarticular and extraarticular obstacles which prevent reduction: pulvinar, labrum, hypertrophied round ligament, transverse ligament, psoas tendon and anteromedial capsule.3 When attempting a closed reduction in the presence of obstacles, interposed structures will increase pressure on the femoral head, thus increasing the risk of occlusion of the venous drainage or cartilaginous channels and causing avascular necrosis of the femoral head. It is very important to remember that treatment with closed reduction in the presence of interposed structures will lead to poor long-term results and will increase the risk of avascular necrosis.53 Therefore, it is imperative to obtain an arthrography in subluxated or dislocated hips, in order to assess the need for a closed or open reduction.
A hip arthrogram. Case A illustrates a correct reduction of the hip without medial contrast accumulation (1) and with a “rose thorn” sign (2), which corresponds to the contrast between the capsule and labrum. The arthrography of Case B shows a medial accumulation of contrast (3), which indicates an incorrect hip reduction due to the existence of obstacles: the labrum (4), the psoas tendon (5) and the round ligament (6). A closed reduction of the hip is contraindicated in Case B, requiring instead an open reduction to eliminate the anatomical barriers.
The probability of requiring an open reduction increases with age. Although reduction is difficult, the growth potential of the acetabulum will still be high, so that the stimulus of concentric hip reduction will achieve normalisation of the dysplastic acetabulum. Once an open or closed reduction has been achieved, this will be maintained with a cast for 3 months to achieve hip stabilisation. This reduction protocol under general anaesthesia followed by immobilisation with a spica cast is applied at the beginning of childhood in children presenting dislocations which are non-reducible using the Pavlik harness.
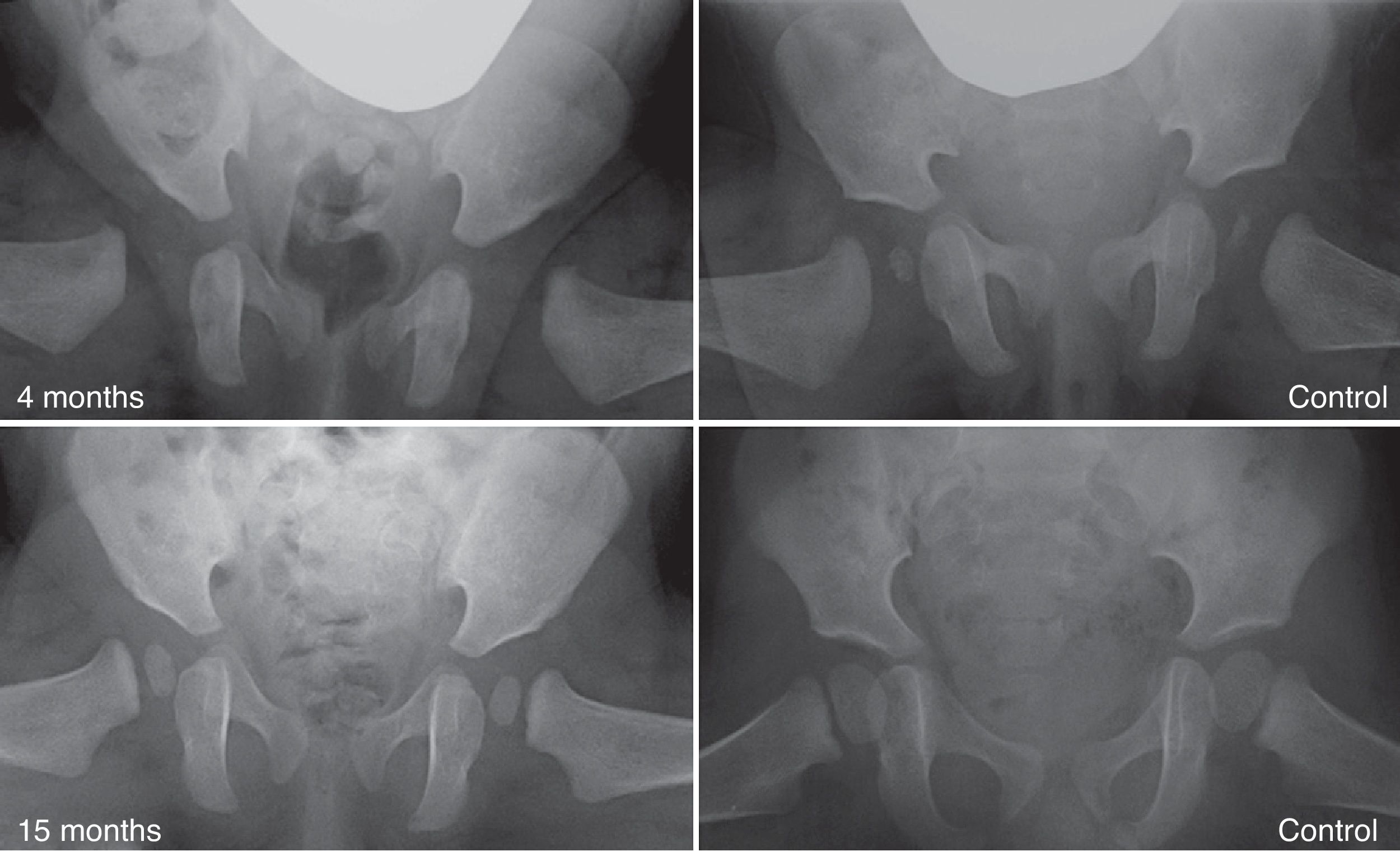
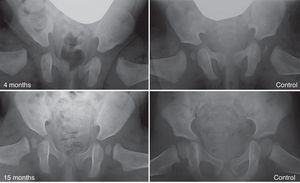
With advancing age it becomes less likely that reduction alone can normalise a dysplastic acetabulum.29 The prevalence of “residual dysplasia” increases along with the age when the hip is reduced, regardless of the type of reduction (Fig. 5).54 The age limit at which the stimulus that causes hip reduction is sufficient to normalise the acetabulum is currently unknown. Moreover, regardless of age at the time of reduction, the stimulus is not always sufficient and residual dysplasia can occur even when the treatment is performed in the first months of life. Despite the considerable success of the Pavlik harness in the short- and medium-term, long-term residual dysplasia has been described in 17–19% of patients treated with this method.55 In addition, residual dysplasia has been described in 22–33% of hips treated through open or closed reductions.54,56,57 Acetabular and/or femoral osteotomies become necessary when the acetabulum does not become normalised (persistent residual dysplasia) or is not expected to due to age. These procedures will prevent the onset of coxarthrosis in adulthood. The correct time to indicate these procedures is currently under debate, with age and evolution of the acetabular index as indicator of acetabular remodelling being the most reliable parameters to predict the probability of residual dysplasia upon skeletal maturity.29,54
Residual dysplasia following treatment with a Pavlik harness. The image in the upper left quadrant shows an anteroposterior pelvic radiograph of a 4-month-old patient at the start of treatment with the harness. The image in the lower left quadrant is an anteroposterior pelvic radiograph of the same patient at 15 months of age, showing residual acetabular dysplasia despite treatment with the Pavlik harness. The images on the right correspond to anteroposterior radiographs of a normal pelvis: at 4 months of age in the case of the upper right quadrant and at 15 months of age in the case of the lower right quadrant.
“Femoral osteotomies”, consisting in varisating and derotatory osteotomies, are performed to stabilise hip reduction and to stimulate the development of the acetabulum.58 Their use is based on the presumed existence of increased femoral anteversion and coxa valga, which is at issue.11,12 Increased femoral anteversion is the most frequent cause of recurrence of subluxation and, therefore, derotatory femoral osteotomy is necessary in some cases to achieve a stable reduction of the hip. Additionally, some authors have shown that concentric hip reduction followed by derotatory osteotomy can stimulate the development of the acetabular roof without the need to varisate the proximal femur or perform an acetabuloplasty.58 However, other authors believe that acetabular dysplasia cannot always be solved by actions conducted exclusively on the proximal femur.59
The “acetabular osteotomies” described in the literature may be divided into 2 groups: osteotomies which maintain the articular cartilage as a contact surface between the acetabulum and the femoral head, and so-called salvage osteotomies, which do not. In turn, the former are divided into osteotomies which alter the orientation (Salter osteotomy, Steel triple osteotomy or periacetabular osteotomy) and osteotomies which alter the shape (Pemberton osteotomy, San Diego or Dega osteotomy).
“Reorientation osteotomies” only improve the direction of the acetabulum. These osteotomies include Salter osteotomy, periacetabular osteotomy or Steel triple osteotomy. These osteotomies mobilise the acetabulum so that lateral and anterior coverage increases, while at the same time decreasing the posterior and inferior coverage. Among the “osteotomies which alter the shape” we can find the Dega osteotomy and the Pemberton osteotomy. Dega osteotomy is performed through the lateral cortex of the ilium and is directed towards the triradiate cartilage, leaving an intact medial cortex and enabling mobilisation of the acetabular roof, using the triradiate cartilage as a hinge (Fig. 6). Pemberton osteotomy begins at the anteroinferior iliac spine, curves towards the ilioischial line of the triradiate cartilage and also uses the triradiate cartilage as a hinge. Osteotomies which alter the shape achieve a greater degree of correction of acetabular dysplasia and a greater coverage of the femoral head than the Salter osteotomy.60 We must bear in mind that physiological osteotomies are not performed to reduce or stabilise dislocated or subluxated hips, but only in reduced and stable hips in order to improve acetabular configuration.
Regarding irreducible hips, salvage osteotomies (Chiari osteotomy and shelf osteotomy) can be conducted in order to increase coverage of the femoral head, giving stability to the joint and increasing the load area of the acetabulum. However, these osteotomies do not maintain the articular cartilage as a contact surface between the acetabulum and femoral head. It has been demonstrated that the joint capsule interposed between the femoral head and the surface of the ilium mobilised in the Chiari osteotomy or between the femoral head and the bone graft used for the shelf osteotomy undergoes metaplasia and acquires a structure which resembles the articular cartilage.61
Neither acetabular nor femoral osteotomies achieve normalisation of the acetabulum and prevention of the development of coxarthrosis in all cases. Thomas et al.62 studied the long-term results of the Salter osteotomy and described implantation of a hip prosthesis in 31% of patients who survived more than 40 years after surgery. In addition, 17% presented definitive radiographic signs of osteoarthritis (grades 3 or 4 in the Kellgren and Lawrence scale) although they had not undergone prosthesis implantation. Similarly, Steppacher et al.63 described the implantation of a total hip replacement in 38% of patients undergoing periacetabular osteotomy, 20 years after the procedure. Gibson and Benson64 described the long-term results of patients who were treated in early childhood through an open or closed hip reduction and derotatory osteotomy of the proximal femur. These authors noted the presence of osteoarthritic signs in 44% of cases at 21 (range: 16–31) years of age.
Level of evidenceLevel of evidence v.
Ethical responsibilitiesProtection of people and animalsThe authors declare that this investigation did not require experiments on humans or animals.
Confidentiality of dataThe authors declare that this work does not reflect any patient data.
Right to privacy and informed consentThe authors declare having obtained written informed consent from patients and/or subjects referred to in the work. This document is held by the corresponding author.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Moraleda L, et al. Displasia del desarrollo de la cadera. Rev Esp Cir Ortop Traumatol. 2013;57:67–77.