Hip replacement is one of the most successful operations in orthopaedic surgery. Periprosthetic hip fractures (PPHF) have very serious consequences for the patient, and they also entail a very important economic impact on healthcare systems. The aim of the study was to provide the first detailed cost analysis of PPHF in a traumatology and orthopaedics service in a third level hospital in Spain.
MethodsThe study included all patients admitted between 2009 and 2019 with a diagnosis of “PPHF”. We assessed hospital stay cost, total cost of the operating theatre, cost of the implants used, analyses, consultations with other specialists, rehabilitation sessions, radiological tests, microbiology, blood transfusions and other surgical operations during the same admission.
Results78 patients were included in the study, 49 women and 29 men, with a mean age of 78.74 years (R 45–92). 69 patients received surgical treatment, 75% had open reduction and internal fixation (ORIF), and 25% had revision surgery. The total cost was €1,139,650.17. The average cost was €14,610.90. Significantly higher costs were incurred for revision compared to ORIF treatments, admissions that lasted more than 30 days, and patients who required more than one operation during admission. The most costly factors were the hospital stay (46%), the cost of the surgery itself (35%), and the implants (24%).
ConclusionsRevision arthroplasty versus ORIF treatment, admissions lasting more than 30 days, and patients requiring more than one operation on admission incurred significantly higher costs. The average cost, from a hospital perspective, generated by a PPHF was €14,610.90. The most costly factors were, in descending order, the hospital stay, the cost of the surgery itself, and the implants. It is necessary to establish protocols and updated therapeutic algorithms in the perioperative management of PPHF in order to reduce both morbidity rates and associated costs.
La artroplastia de cadera es una de las operaciones con mejores resultados en cirugía ortopédica. Las fracturas periprotésicas de cadera (FPPC) tienen consecuencias muy graves para el paciente y además suponen un impacto económico muy importante para los sistemas sanitarios. El objetivo del estudio es realizar el primer análisis detallado de los costes de las FPPC en un Servicio de Cirugía Ortopédica y Traumatología en un hospital universitario de tercer nivel en España.
MétodosEl estudio incluyó a todos los pacientes ingresados entre 2009 y 2019 con el diagnóstico de «FPPC». Se evaluaron el coste de la estancia hospitalaria, el coste total del quirófano, el coste de los implantes utilizados, los análisis de sangre, las consultas con otros especialistas, las sesiones de rehabilitación, las pruebas radiológicas, la microbiología, las transfusiones de sangre y otras intervenciones quirúrgicas durante el mismo ingreso.
ResultadosSe incluyó a un total de 78 pacientes, 49 mujeres y 29 hombres, con una edad media de 78,74 años (R 45-92); 69 pacientes recibieron tratamiento quirúrgico, el 75% se sometió a reducción abierta y fijación interna (RAFI) y el 25% a revisión protésica. El coste total fue de 1.139.650,17 €. El coste medio fue de 14.610,90 €. Los costes fueron significativamente más elevados en la revisión protésica que en la RAFI, en los ingresos que duraron más de 30 días y en los pacientes que requirieron más de una intervención quirúrgica durante el ingreso. Los factores que más influyeron en el coste fueron la estancia hospitalaria (46%), el coste de la intervención quirúrgica (35%) y el de los implantes (24%).
ConclusionesLa cirugía de revisión protésica frente a RAFI, los ingresos de más de 30 días y los pacientes que requirieron más de una intervención quirúrgica durante el ingreso supusieron costes significativamente mayores. El coste medio, desde el punto de vista hospitalario, generado por una FPPC fue de 14.610,90 €. Los factores que más influyeron en el coste, en orden decreciente, fueron la estancia hospitalaria, el coste de la intervención quirúrgica y el de los implantes. Es necesario establecer protocolos y algoritmos terapéuticos actualizados en el manejo perioperatorio de la FPPC para reducir tanto las tasas de morbilidad como los costes asociados.
Hip arthroplasty is one of the most successful operations in orthopaedic surgery, and the number of both hip replacement and revision arthroplasties continues to increase year after year.1,2 Due to the ageing population and the increasing functional demands of lifestyle, this trend is expected to continue rising.3 In general, few complications are associated with this procedure; however, periprosthetic hip fractures (PPHF) have serious consequences for the patient and entail a very important economic impact on national health care systems.2,4–6 There is no previous published study showing the economic impact generated by these patients in Spain.
Treating them is complex owing to the technical difficulty and because they tend to affect elderly patients who often have poor bone quality and accompanying comorbidities, which is why the prognosis is often bleak.7 The actual incidence of PPHF is disputed, although it is estimated to be between 0.1 and 2.1% for primary replacements, increasing to 2.8–4% for surgical revisions.8,9
In this study we reviewed all PPHF that were treated in our centre, a tertiary level university hospital in Spain. We present a breakdown of all the costs involved in the hospitalisation of patients with this diagnosis, analysing the distribution according to the concepts of the expenditure generated. The aim of the study was to provide a detailed cost analysis of PPHF in a traumatology and orthopaedics service in a third level hospital.
Material and methodsInstitutional review board approval was obtained before the initiation of this study. A retrospective observational study was conducted, including all patients operated on between 2009 and 2019 who had a diagnosis of PPHF.
The preoperative X-rays of all the patients were reviewed to check that the Vancouver Classification was correctly applied10 on admission. For that, intraoperative documentation of the stability of the prosthesis was used to confirm whether it was really a stable/unstable stem. The inclusion criterion was PPHF admitted between 2009 and 2019. Patients who did not require admission were excluded.
The treatment adopted was that proposed by the authors of the Vancouver classification10 except for those patients with fractures around loosened implants with good bone stock (type B2). In a presurgical session conducted in conjunction with the orthogeriatric service, each patient V-B2 was individually and comprehensively assessed. The therapeutic approach in V-B2 is explained in more detail in a recently published article by the same authors.11 The decision on whether to perform ORIF or stem revision was made on the basis of the fracture type according to the Vancouver classification, previous mobility of the patient, fracture pattern (anatomical reconstruction possible), anaesthetic risk, previous pain in the hip and the experience of the senior orthopaedic surgeons. A weighting of the different parameters was not carried out. The main factor to take into account was previous mobility and anaesthetic risk12 (ASA≥3 and Anaesthesia/Orthogeriatric assessment). In elderly and multi-pathological patients, ORIF was preferred, while in young patients with high functional demand, stem revision was preferred. Regarding the fracture pattern, we chose osteosynthesis if the stem was fixed to a large fragment and whose anatomical reconstruction was possible. In some patients, the indication for osteosynthesis was forced due to low functional demand and high surgical risk.
In collaboration with the centre's Invoicing and Treasury Department, all invoices generated by the patient's admission were reviewed. The billed cost for each day of admission, screw, plate, cerclage, revision stem, analytical tests, X-rays, rehabilitation sessions, etc. was collected. The itemised concepts were: hospital stay (includes cost of the bed and an average of the costs of healthcare personnel doctor, nurse, healthcare assistant, etc.), total cost of the operating theatre, cost of the implants used, analyses, consultations with other specialists, hospital rehabilitation sessions, radiological tests, microbiology, blood transfusions, other surgical operations during the same admission, assessment in the emergency department and stays in intensive care. The costs are expressed in terms of the value of the euro in 2020.
The cost study carried out is from a hospital perspective, so we have not taken into account outpatient rehabilitation sessions, intermediate care centres, nor the cost generated once a patient has been discharged from hospital after the main operation. We do include the place where the patient went after discharge (intermediate care centres, a nursing home or at home) and, in patients with loosened stems, it was determined whether they had been able to walk during the first year.
Statistical analysisProportional comparisons were made using chi-square or Fisher's exact tests, as appropriate. Group comparisons of quantitative and ordinal variables were made using Student t-tests, Mann–Whitney tests, or ANOVA, as appropriate. A logistical regression analysis was performed for the categorical dependent variables. Probability values of less than 0.05 were considered significant. Data analyses were performed using the SPSS statistical package (IBM Corp. Released 2017. IBM SPSS Statistics for Windows, Version 25.0 Armonk, NY).
ResultsBetween 2009 and 2019, 78 patients were recruited. The mean follow-up time was 1131 days [3.1 years] (R 21–3168; SD 851). The sample characteristics can be seen in (Table 1). According to the Vancouver classification, 2 patients were type A (5.1%) and 72 were type B, of which 8 were B1 (10.2%), 56 were B2 (71.8%), and 8 were B3 (10.2%). Lastly, 4 fractures were classified as type C (5.1%). 9 patients were treated conservatively, while 69 were treated surgically (Table 2).
Patient demographics.
| Periprosthetic hip fractures | |
|---|---|
| Age | 78.74 years (R 45–92; SD 9.434) |
| Sex | Men 29 (37.2%)Women 49 (62.8%) |
| Side | Left 35 (44.9%)Right 43 (55.1%) |
| Mechanism of injury | Low energy 77 (98.7%)High energy 1 (1.3%) |
| Type of implant | Hemiarthroplasty 9 (11.5%)Hip replacement 65 (83.3%)Revision 4 (5.1%) |
| Implant indication | Osteoarthritis 62 (79.5%)Intracapsular fracture 11 (14.1%)Loosening 3 (3.8%)Avascular necrosis 2 (2.6%) |
| Cemented | No 55 (70.5%)Yes 23 (29.5%) |
| Follow-up time (days) | 1168 [3.2 years](R 10–3168; SD 825) |
Implanted material.
| Implanted material | N | % |
|---|---|---|
| Conservative | 9 | 11.5 |
| Cerclage | 6 | 7.7 |
| Plate+/−cerclage-7 Cable-ready plate (Zimmer)-28 NCB plate (Zimmer)-2 Dall-Miles plate (Stryker)-9 LCP plate (Synthes) | 46 | 59 |
| Revision arthroplasty-2 Revitan (Zimmer) | 2 | 2.6 |
| Revision arthroplasty+/−plate+/−cerclage-15 Revitan (Zimmer) | 15 | 19.2 |
The two type A fractures were treated conservatively, all the B1 and C fractures were treated using the ORIF technique, the B3 fractures were all treated by revision arthroplasty, with the exception of one bedridden patient who had a very displaced fracture that was fixed to prevent bleeding and skin trauma. Of the patients diagnosed with B2 fractures, 7 patients presented a very precarious baseline situation, both medically and functionally, for which reason they were treated conservatively; the remainder, 39 were treated with ORIF and 10 were given stem revision. For the statistical analysis, we unified all fractures with loosened stems (B2 and B3) in order to obtain a larger control group in terms of stays and costs, since no structural bone graft was used in any patient and the surgical technique and rehabilitation protocol if revision arthroplasty was carried out was the same regardless of whether it was B2 or B3.
The total average stay (Fig. 1) was 25.67 days (R 1–143; SD 21.37), preoperative stay was 8 days (R 1–20; SD 5.2) and postoperative stay was 20.13 days (R 5–134; SD 17.9). When we analysed the stay according to the Vancouver classification, B2/B3 patients had the longest average total stay, at 35.24 days. We found that those patients with stem loosening who underwent ORIF stayed in hospital for less time (26.03 days) compared to those who were given a stem revision (35.24 days), mainly due to the postoperative stay (17.1 days vs. 27.9 days).
Medical complications (wound infection -superficial/deep-, pulmonary thromboembolism, deep vein thrombosis, death in the first year, etc.) were presented by 17/78 patients (21.8%), and implant complications (plaque rupture, re-fracture, stem migration, prosthetic dislocation, etc.) were suffered by 8/69 patients (11.6%). A total of 24/78 patients (30.76%) experienced some type of complication and 9/69 (13.04%) patients required surgical reintervention: 4 patients had infections (deep to the fascia lata), requiring lavage and debridement; 2 had loosened stems that were converted to revision arthroplasty; 2 suffered dislocation (one required a constricted acetabulum replacement and another needed open reduction); and 1 experienced a refracture after revision and required a longer stem. The mortality rate in the first year was 14% (11/78), with no significant differences between the sexes (p=0.782). We also found no significant differences between the ORIF and revision arthroplasty groups: medical complications (p=0.679); implant complications (p=0.369); and need for reintervention (p=0.227). Of all the patients, 17 (21.8%) required readmission for treatment of complications, mainly medical. Nor were there any significant differences in B2 and B3, between ORIF and revision arthroplasty, with regard to the proportion of patients who were able to walk within the first year after surgery or readmission rate. After discharge 9 patients went to intermediate care centres, 12 patients went to a nursing home and 57 patients returned home.
The total cost of the 78 patients included in our study was €1,139,650.17, with an average cost of €14,610.90 (median €13,486.19). We did, however, find a great deal of cost variability between the patients: €689.19 to €52,908.21. The least costly patient suffered an avulsion of the trochanter and was discharged after having been admitted for just 1 day, while the patient who incurred the highest cost was a Vancouver B2 fracture patient, who suffered medical complications necessitating 3 days in the ICU, and a total of 143 days in hospital.
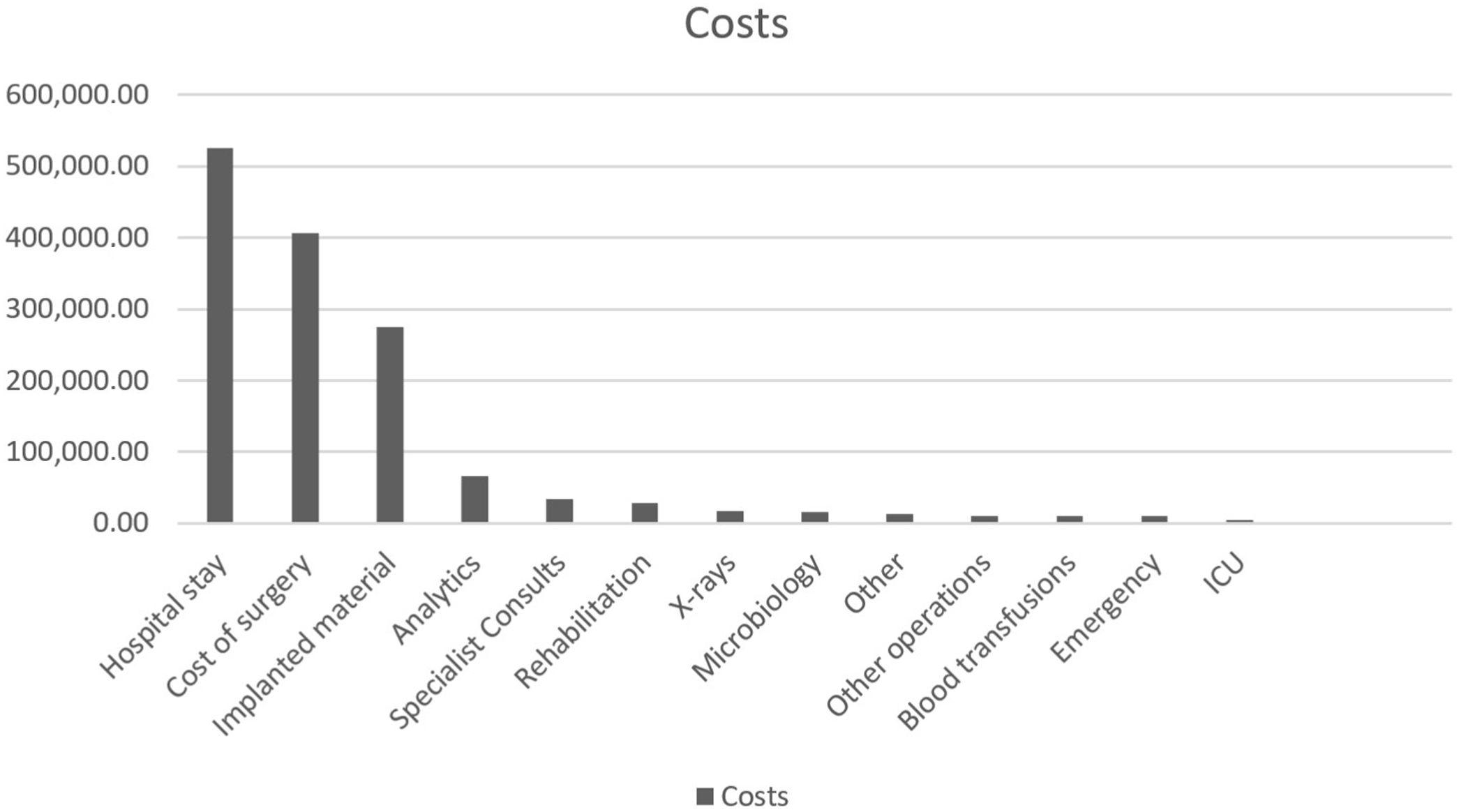
The majority of the costs are attributable to the hospital stay (46%). The overall cost of the operating theatre was 35% of the total cost and the implants (plates, screws, revision arthroplasties, etc.) accounted for 24% of the total. The remaining costs (analytics, microbiology, rehabilitation, etc.) have also been broken down (Table 3) (Fig. 2).
Breakdown of costs by concept.
| Costse (€; 2020) | Type A (N=2) | Type B1 (N=8) | Type B2/B3 ORIF (N=40) | Type B2/B3 revision (N=17) | Type B2/B3 conservative (N=7) | Type C (N=4) | % | Total (N=78) |
|---|---|---|---|---|---|---|---|---|
| Hospital stay | 766.39 | 5820.28 | 6547.66 | 9570.61 | 4740.33 | 4749.89 | 46 | 524,883.45 |
| Total cost of surgery | 0 | 5556.65 | 5014.63 | 8203.34 | 0 | 5409.07 | 35 | 406,131.37 |
| Implanted materiala | 0 | 3809.61 | 3167.80 | 6049.52 | 0 | 3546.77 | 24 | 274,217.83 |
| Analytics | 232.32 | 504.36 | 906.30 | 1206.24 | 429,781 | 392.08 | 5.7 | 65,834.43 |
| Specialist consults | 96.33 | 298.41 | 454.24 | 537.76 | 398,118 | 190.87 | 3 | 33,441.77 |
| Rehabilitation | 0 | 212.26 | 335.23 | 595.90 | 326,240 | 146.39 | 2.4 | 28,106.83 |
| Othersb | 0 | 568.85 | 133.49 | 142.41 | 63,459 | 110.13 | 1.6 | 13,195.92 |
| Radiologyc | 248.24 | 161.87 | 281.13 | 200.83 | 117,853 | 171.42 | 1.4 | 17,961.34 |
| Microbiology | 32.67 | 138.65 | 200.90 | 305.98 | 81,685 | 91.58 | 1.3 | 15,350.12 |
| Other operationsd | 0 | 215.34 | 107.90 | 150.57 | 0 | 436.76 | 0.9 | 10,345.48 |
| Blood transfusions | 0 | 93.75 | 131.25 | 202.94 | 64,286 | 75.00 | 0.9 | 10,200.00 |
| Emergency | 126.35 | 126.35 | 126.35 | 126.35 | 126.35 | 126.35 | 0.8 | 9855.08 |
| ICU | 0 | 0 | 0 | 255.55 | 0 | 0 | 0.4 | 4,344.37 |
| Average | 1502.31 | 13,696.80 | 14,239.07 | 21,498.449 | 6348.098 | 11,899.524 | 14,610.90 | |
| Total | 1,139,650.17 |
There were statistically significant differences in the operating room cost according to the subtype of the Vancouver classification (p=0.019), although we found no differences in the total cost of admission by Vancouver type (p=0.097). We did find significant differences between patients who had hospital stays exceeding 30 days (p<0.001), those who required more than one operation (p<0.001), and patients who underwent revision surgery instead of ORIF (p<0.001) (Table 4).
Average cost per treatment group.
| Average cost and hospital stay for each group | ||||
|---|---|---|---|---|
| Treatment type | N | Average age (years) | Average stay (days) | Average cost per patient (€) |
| All | 78 | 78.74 | 25.67 | 14,610.90 |
| Conservative | 9 | 83.67 | 12.89 | 5271.26 |
| Surgical | 69 | 78.10 | 27.33 | 15,829.11 |
| ORIF | 52 | 78.50 | 24.75 | 13,975.68 |
| Revision | 17 | 76.88 | 35.24 | 21,498.45 |
| Cerclage | 6 | 80.17 | 22.67 | 10,850.65 |
| Plate+/−cerclage | 46 | 78.34 | 27.60 | 15,202.97 |
| Revision | 2 | 68.00 | 20.00 | 15,953.85 |
| Replacement+/−plate+/−cerclage | 15 | 77.86 | 29.50 | 20,046.98 |
| Single operation | 60 | 78.61 | 22.29 | 13,235.26 |
| >1 operation during the same admission | 9 | 79.78 | 51.56 | 25,157.44 |
| Arthroplasty | 9 | 83.44 | 23.56 | 13,003.24 |
| Hemiarthroplasty | 65 | 78.74 | 26.55 | 15,040.82 |
| Revision arthroplasty | 4 | 68.25 | 16.00 | 11,241.92 |
| <30 days admission | 51 | 77.65 | 17.38 | 11,805.83 |
| >30 days admission | 18 | 83.00 | 49.70 | 22,745.60 |
Hospital stay is the factor that generates the greatest cost with regard to a patient with a PPHF.1,4 It has been described as representing up to 80% of the total cost4; however, in this study we found that it accounts for 46%. In the aforementioned study4 the average stay was 39.3 days whereas in this study it was 25.67 days. Other studies have described stays of between 5 and 13 days.6,13 Some authors report lower total hospital costs, but explain that these involve early discharge from rehabilitation and intermediate care centres.14 With these involving an average stay of 5 days, this fact underlines the important impact that the length of stay has on the total cost. The management of periprosthetic fractures, especially the new implants that allow more stable syntheses, has been a possible factor in the reduction of hospital stay in many studies.6,13
The cost averaged across all patients included in the study was €14,610. If we take into account those treated surgically, this rises to €15,829. Of these, the average cost for patients who received ORIF treatment was €13,975 compared to €21,498 for those who were given a revision surgery, which was found to be a significant difference (p<0001), a result in line with other studies.6,15 Other authors also state that revisions are more expensive, mentioning average figures of $34,078 compared to $18,706 for the ORIF group.14 However, it is again important to emphasise the role of the average stay in the total admission cost, as there are studies that show a significantly higher cost for implants in the revision group, but an earlier discharge, resulting in a higher total cost for ORIF group.16 The percentage of the total cost attributable to the surgery itself has been described as 20%,4 although in this study it accounts for 35%, with implants representing 68.5% of this (24% of the total).
Preoperative stay in our sample is very long (8 days) and we know that it is not representative of most hospitals. It depends on many factors, relating to both the patient (optimisation prior to surgery) and hospital logistics (availability of the operating theatre, availability of surgeons, other emergencies, etc.). It is widely accepted in the literature that delaying surgery for more than 2 days increases mortality.6 The utmost effort should be made to reduce this time and thereby optimise the results.
The distribution of fractures according to the Vancouver classification shows that most were type B2 (71.8%), as has already been described in the literature, although in other studies the percentage is lower, for example, a Swedish work reported 53%17 and an American study recorded 41%.13
The cost accounting methods differ substantially between almost all of the studies reviewed. Although, as stated, cost studies are an inexact science,18 with the help of the hospital's Invoicing Service, we used a systematic approach, analysing all the costs billed individually for each patient. Although the absolute costs are specific to our institution, the cost differences according to type of intervention can be applied to a wider population.
Some publications state that patients operated on using the ORIF technique have shorter stays than those who receive revision surgery,4,5 while others have found differences, although these are not significant.19 Although in this study, patients who underwent ORIF were admitted for an average of 24.75 days while revision surgery patients stayed in hospital for 35.24 days, this difference was not significant.
It is accepted that revision arthroplasty is more expensive than a hip replacement.5,13,14 Similarly, although it is true that implants are more expensive in a revision surgery than in an ORIF,20 it is known that the bulk of the cost for patients with PPHF is not incurred by the surgery itself, but rather by the entire perioperative management.16 To the extent that, in conjunction with other specialties, we can shorten the hospital stay by taking a comprehensive approach to the patient, the cost of implants becomes relatively more important, and this is a matter for the orthopaedic surgeon. For this reason, we must strive to optimise the time spent in hospital. Costs associated with readmissions due to complications were not assessed in this study. Other studies have analysed these and shown that they involve a high additional economic impact on healthcare systems.1
PPHF pose a higher risk of medical complications,21,22 generating a longer stay and increased total cost.5 In this work we found that 21.8% (17/78) of patients had medical complications, and 11.6% (8/69) suffered implant complications. No differences were found between ORIF and revisions with regard to either medical or implant complications, or the need for reoperation. The hospital readmission rate was 21.8% (17/78), similar to other studies that mention figures of 25%1; however, we have not analysed the cost of these new episodes.
Globally, there are important differences in resources between countries and even between cities within the same country. In the case of PPHF, i.e., older, dependent patients requiring rehabilitation, this plays a very important role in the management and consumption of economic resources.18 It would be interesting to implement more intermediate care centres or nursing homes in order to reduce hospital stays6,13 and thus reduce the economic impact on health systems.
For many years it has been accepted that all fractures with loosened stems should be managed via revision stem.23 However, in the literature there is still an open debate about whether it is really necessary to perform such aggressive surgery on all patients and whether this involves a significant functional benefit.3,11,24,25 Stem revision remains the treatment of choice in Vancouver B2
fractures, but, in selected cases, internal fixation can be a viable alternative option. In older patients, with low functional demand, ASA≥3, if there is adequate bone stock and it is possible to anatomically reconstruct the fracture where it is sufficiently stable to allow consolidation, we propose using the ORIF technique11,26 with the aim of reducing the need for blood transfusions, decreasing surgery times, reserving bone for possible future revision surgeries and cutting the cost of implants.3 We are currently analysing the radiological and functional results of our sample with the aim of establishing an algorithm to comprehensively manage patients suffering a PPHF.
The limitations of this study include its retrospective nature. In its methods, cost accounting and management control have their own peculiarities in their applications to institutions, organisations and companies. But this does not invalidate any approach to the measurement of the relevant variables and their correlations in order to capture indicative signals of the “economic calculation” for decision-making and the “economic impact” derived from such decisions. On the other hand, preoperative stay in our sample is very long (8 days), which has increased the total cost. This was mainly due to logistical problems, as it is a public hospital with limited resources and high demand for care. Finally, despite the fact that the scope of any work that is done is limited by the data handled. Expanding the study with other local or national data would enrich the scope by comparing and contrasting this work in our environment.
The number of primary arthroplasties continues to increase with time, the population continues to age, and the expectation is that this trend will continue in the coming years.6 It is necessary to optimise the management of these patients in order to reduce both morbidity rates and the costs associated with PPHF.
ConclusionsRevision arthroplasty versus ORIF treatment, admissions lasting more than 30 days, and patients requiring more than one operation on admission incurred significantly higher costs. The average cost, from a hospital perspective, generated by a PPHF was €14,610.90. No differences were found between ORIF and revision arthroplasty with regard to either medical or implant complications, need for reoperation or the hospital readmission rate. The most costly factors were, in descending order, the hospital stay, the cost of the surgery itself, and the implants. It is necessary to establish protocols and updated therapeutic algorithms in the perioperative management of PPHF in order to reduce both morbidity rates and associated costs.
Level of evidenceLevel of evidence III.
Ethical review committee statementWe have the favourable certificate from the ethics committee of our local ethics committee with the code: CHUC_2020_31.
FundingThe authors received no funding.
Conflict of interestThe authors declared no conflicts of interest.
The main author would like to thank Miguel Ángel Martín Marrero, Silvia Mayato Guanche, Manuel González Hernández and María del Rosario Pérez Fleitas for their help in the development of this manuscript.