Total hip arthroplasty in young patients has evolved in recent decades, and the use of short stems in young adult patients has been gaining popularity. The restitution of the biomechanics of the hip is a primary requirement to determine the future success of total hip replacement, and even more so in young adults who present the particularity of having a high functional demand and a long life expectancy.
ObjectiveThe aim of this prospective study was to evaluate the learning curve and initial clinical-radiological outcomes of the Alteon Neck Preserving Stem (ANPS) (Exactech, Gainesville, FL, USA) with a minimum of 2 years follow up.
Material and methodsWe conducted a multicenter prospective study that analyzed 90 consecutive total hip replacements during 2014. We performed a clinical-radiological analysis measuring Harris Hip Score (HHS), subjective Rodes and Maudsley satisfaction evaluation, radiolucencies, components position, limb length discrepancy, heterotopic ossification, medical and surgical complications and learning curve.
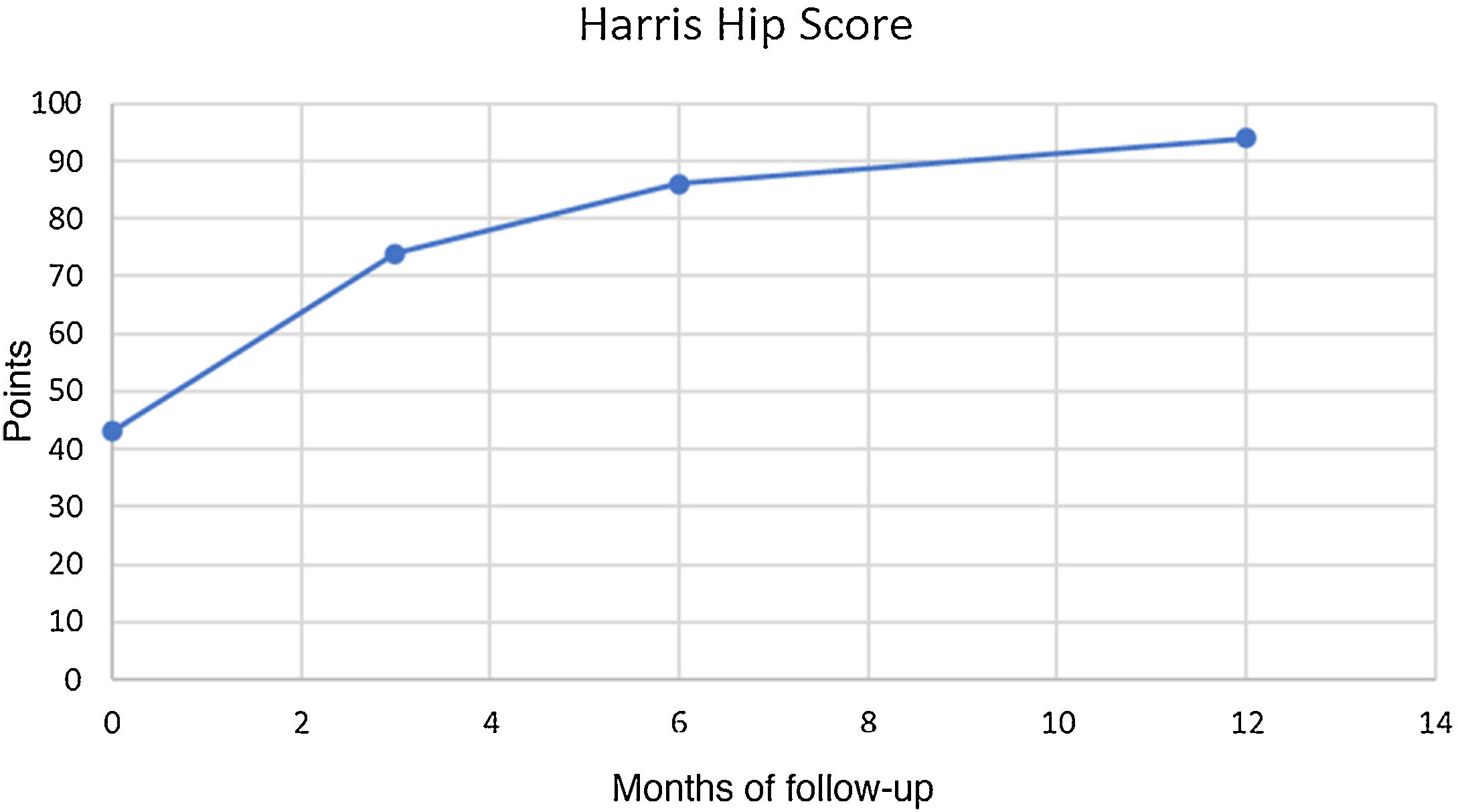
ResultsDuring the first 30 cases, the intraoperative complication rate was 16%, while in the next 60 cases no intraoperative complications were reported. Thigh Pain was reported in 3 cases (3.3%), being 2 moderates, and 1 severe. In 2 cases subsidences of 3 mm were detected in the first scheduled X-ray, both related to intraoperative fractures with no progression after 3 months. Mean HHS improved from 42.9 points (range 37–54 points) preoperatively to 93.2 on average (range, 87–96) at the end of the follow up (p < .01). Subjective evaluation was excellent in 75 (83,3%) cases and good in 15 patients (16,6%).
ConclusionsThis short stem has good clinical radiological results in a short and medium term follow-up and in the hands of surgeons specializing in arthroplasty the learning curve is estimated to be less than 30 surgeries.
La artroplastia total de cadera en pacientes jóvenes ha ido evolucionando en las últimas décadas y la utilización de tallos cortos en pacientes adultos jóvenes ha ido ganando popularidad. La restitución de la biomecánica de la cadera es requisito primordial para determinar el éxito a futuro del reemplazo total de cadera, y aun mas en los adultos jóvenes quienes presentan la particularidad de tener una alta demanda funcional y una esperanza de vida prolongada.
ObjetivoEl objetivo de este estudio prospectivo fue evaluar la curva de aprendizaje y los resultados clínico-radiológicos iniciales del Alteon Neck Preserving Stem (ANPS) (Exactech, Gainesville, FL, EE.UU.) con un mínimo de 2 años de seguimiento.
Material y métodosSe realizó un estudio prospectivo multicéntrico que analizó 90 reemplazos totales consecutivos de cadera durante 2014. Realizamos un análisis clínico-radiológico utilizando Harris Hip Score (HHS), evaluación de satisfacción subjetiva de Rodes y Maudsley, radiolucencias, posición de los componentes, discrepancia en la longitud de las extremidades, osificación heterotópica, complicaciones médicas y quirúrgicas y un análisis de la curva de aprendizaje.
ResultadosDurante los primeros 30 casos, la tasa de complicaciones intraoperatorias fue del 16% mientras que en los siguientes 60 casos no se reportó ninguna complicación intraquirurgica. El dolor de muslo se notificó en 3 casos (3,3%), siendo 2 moderados y 1 grave. En 2 casos se detectaron hundimientos de 3 mm en la primera radiografía programada, ambas relacionadas con fracturas intraoperatorias sin progresión después de 3 meses. La media de HHS mejoró de 42,9 puntos (rango 37 a 54 puntos) preoperatoriamente a 93,2 en promedio (rango, 87–96) al final del seguimiento (p < 0,01). La evaluación subjetiva fue excelente en 75 casos (83,3%) y buena en 15 casos (16,6%).
ConclusionesEste tallo corto tiene buenos resultados radiológicos clínicos en un seguimiento a corto y medio plazo y presenta una curva de aprendizaje aceptable definida en nuestro caso de menos 30 cirugías.
Implant designs and their materials have evolved over the years with the use of short stems in total hip arthroplasty (THA) in Young adult patients gaining in popularity. During the 1990s two short stems appeared and in the last decade they have gained a significant number of followers with the consequent increase in the number of products on the market with their individual differences.1–4 Although a large number of designs exist, Kheir et al. suggested they be grouped into type 1 of the unified classification of cementless stems and sub-classified into four subtypes according to their different attachment philosophy.5
Currently, subtype 1B stems are the ones most implanted and similar outcomes are reported to standard sized cemented or cementless stems in the medium term. The literature suggests advantages such as bone preservation; anatomical reproduction; theoretical ease of rescue surgery with a standard stem or the versatility to adapt the stem in Dorr A cortical bones.6 However, implant technique is different to that of the conventional size and repetition of technique is required for easy management.7–9
Recovery of hip biomechanics is the essential requisite to determine the future success of the THA and it should be even more in young adults with a particularly high functional demand and longer life expectancy.10 Their implants should be reviewed probably at least once in the patient’s life.11 This is because the positioning of the implant; the ability to restore femoral offset; the discrepancy of lower limbs and the complications during implantation could potentially alter the survival of the implant and all designs available on the market should be studied in both the long term and the short term follow-up.
As a result, the aim of this study was to analyse the learning curve and initial clinical and functional outcomes with the use of the short cervicometaphyseal fixation stem.
Material and methodsAfter obtaining approval from the hospital evaluation committee and informed consent from patients the study was initiated prospectively.
Inclusion criteria: aged from 21 to 65 years; THA as a consequence of osteoarthritis, avascular osteoarthritis necrosis, and grade 1 and 2 hip dysplasia according to the Crowe classification.12
Exclusion criteria: THA caused by femoral neck fracture; grades 3 and 4 hip dysplasia according to the Crowe classification; tumoral or metastatic diseases; previous hip infection in hip to be operated on.
In all cases an Alteon Neck Preserving Stem™ (ANPS) combined with a Novation Crowncup™ with high cross-linked polyethylene insert GXL with raised rear wall of 10° and metallic 32 or 36 mm head were used.
The stem in this study is a stem which partially preserves the femoral neck and has metaphyseal fixation, of a titanium alloy coated with plasma spray, with seven sizes and options of standard or extended neck with a 12/14 type cone that allows for the use of heads of different sizes and materials.
Procedures were performed by a specialist in hip arthroplasties with over ten years of experience in centres with more than 800 annual hip replacements.
Surgical techniqueHypotensive anaesthesia, lateral decubitus. Posterolateral approach with short rotator cuff release with preservation of the piriformis muscle and muscle and capsular reinsertion according to the technique described by Pellic.13 No radioscopic control was used during the preparation of placement of the definitive implants. Patients received antibiotic prophylaxis 30 min prior to surgery and for 24 h post surgery with cefazolin 1 g every eight hours and thromboprophylaxis for 21 days with rivaroxaban one tablet daily.
Duration of surgery and blood loss were recorded, based on the blood reservoir connected to suction.
Clinical assessment was carried out with scheduled check-ups, before surgery and with three-week, three-month, six-month and one-year follow-up visits. The Harris Hip Score (HHS) scores were collected before surgery and one year after surgery14 and subjective assessment was made of outcomes with the Roles and Maudsley score (subjective four-point scale with assessment of pain and limitations, with one being excellent with no pain or limitations after treatment; two significant improvement following treatment; three a relative improvement following treatment, and four poor with similar or worse symptoms following treatment).15
The rehabilitation protocol included early mobility from the first day after surgery and ambulation with a walker and full weight bearing in all cases save in the single case of fracture of lateral cortex fracture in which cerclage was performed and weight bearing was restricted for two weeks progressing to partial and then to full weight bearing. It should be noted that the calcar fractures did not extend to the greater trochanter at any time and although cerclage was performed, full weight bearing was not restricted but partial weight bearing was practised for two weeks. The patients were then encouraged to progressively return to their normal activities, as tolerated, with the use of a cane for one month, depending on their clinical and radiographic progress.
For radiographic assessment anteroposterior and lateral X-rays of the hips were taken in the scheduled three-week, three-month, six-month and one-year follow-up visits. After this they were taken annually.
The Gruen classification was used to assess the topography of the osteolysis or radiolucent lines.16 Subsidence was determined using the method described by Loudon and Charnley.17 Loosening was defined as subsidence greater than 5 mm or progression of radiolucent lines or stem demarcation. The presence of radio-opaque images at the periphery of the femoral stem were also assessed as a sign of osseointegration.18
The Ackland method was used for acetabular assessment for anteversion19 and for acetabular tilt the line passing through the apexes of the acetabular component and posterior edge of the tear-drop image was marked, considered in accordance with the area described by Lewinnek 40 ± 10 of tilt.18
The three areas described by DeLee et al.20 were used to locate radiolucent lines if they appeared. Acetabular loosening was defined by progression of radiolucent lines on three consecutive control X-rays, acetabular cup migration >5° or screw breakage.
Limb discrepancy was measured by measuring a fixed point on the pelvis at the lower edge of the tear-drop image and the proximal edge of the lesser trochanter.21
The Brooker classification was used for the presence of heterotopic calcifications.22
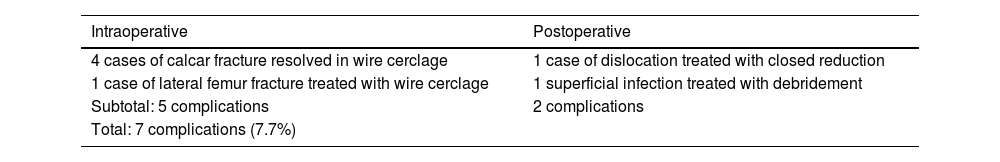
Detected complications were classified as intraoperative (incomplete fractures of the calcar without extension to the greater trochanter and fractures of the lateral cortex of the femur) and postoperative (one episode of dislocation and one episode of superficial infection). Revisions and reoperations were also recorded.
Statistical analysis: continuous variables were expressed as medians and interquartile ranges (IQR). Categorical variables were reported as frequencies and percentages. Continuous variables were compared using the independent sample t-test when date was distributed normally and the Mann–Whitney U test when they were not. Categorical variables were compared using the X2 test and Fisher exact test. Odds ratios (OR) with their 95% confidence interval (CI) were reported. Statistical significance was defined by a p value <.05. All analyses used Stata 13™ (Stata Corp., College Station, Texas) statistical software.
ResultsA total of 90 hips were operated on during 2014, meeting the inclusion criteria and with a minimum follow-up of two years; 49 patients were women and 31 men (54%:46%) with seven patients in the group of women and three in the group of men who were operated on both hips with a three-month interval. No patient received bilateral implant at the same time. Average age was 52.3 years with a range between 21and 65 years, a body mass index in all cases below 30; 84 hips (93%) of the series received spinal anaesthesia and the remainder general anaesthesia.
Mean duration of surgery was 61 min with a range of 49−85 min and blood loss of 400 mL (range of 240−630 mL).
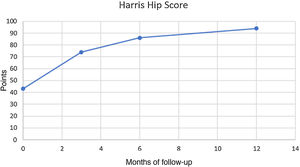
In clinical evolution the Harris score improved from 42.9 preoperative points (range 37–54) to 93.2 points (range 87–96) at one year follow-up (p < .01) (Fig. 1). The Harris score evolution during the follow-ups is contained in Fig. 1. The subjective evaluation was excellent in 75 cases (84%) and good in 15 cases (16%), with no cases of fair or poor results.
Thigh pain presented in three patients (3.3%), and was moderate in two and severe in one. It was located on the anterior side of the thigh in two and laterally in one case. The frequency of presentation was sporadic in two of them during high-demand activities (prolonged jogging, weight bearing at the gymn). In all three cases the discomfort subsided before the first year follow-up and none of them had to be revised for this reason. No patients had Trendelenburg gait.
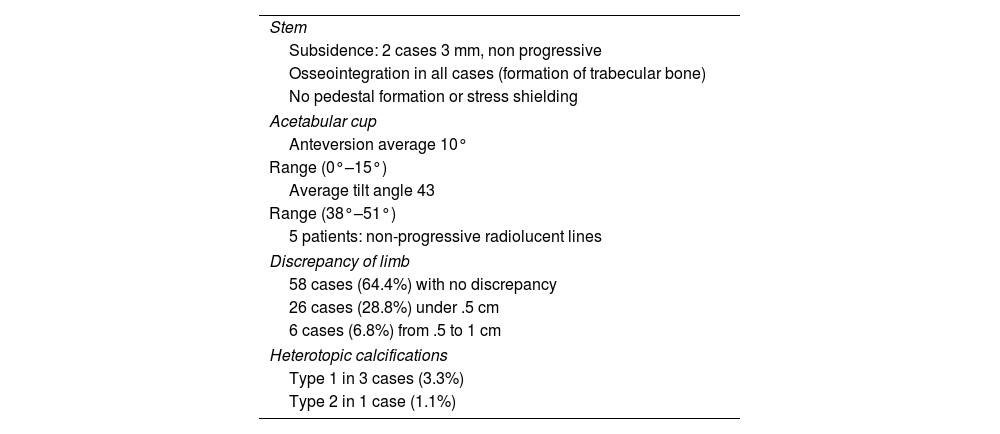
In two cases there was 3 mm subsidence discovered during the radiographic controls in the first quarter, but with no progression. In these cases incomplete calcar fractures were detected during surgery. Osseointegration was detected with appearance of trabecular bone converging towards the stem, with no signs of pedestal formation or resorption due to disuse of the proximal bone.
Acetabular anteversion averaged 10° (IQR 0°–15°), with no extroverted acetabular components observed. The average tilt angle was 43° (IQR 38°–51°). In five (5.5%) patients radiolucent lines with not progression or clinical significance were detected (Table 1).
Radiographic evaluation.
| Stem |
| Subsidence: 2 cases 3 mm, non progressive |
| Osseointegration in all cases (formation of trabecular bone) |
| No pedestal formation or stress shielding |
| Acetabular cup |
| Anteversion average 10° |
| Range (0°–15°) |
| Average tilt angle 43 |
| Range (38°–51°) |
| 5 patients: non-progressive radiolucent lines |
| Discrepancy of limb |
| 58 cases (64.4%) with no discrepancy |
| 26 cases (28.8%) under .5 cm |
| 6 cases (6.8%) from .5 to 1 cm |
| Heterotopic calcifications |
| Type 1 in 3 cases (3.3%) |
| Type 2 in 1 case (1.1%) |
In 58 patients (64.4% of the series), postoperative measurement of limb length found no discrepancy between the operated limb and the contralateral one. In 26 cases (28.8%) there was hypermetry below .5 cm, and the remaining six patients (6.6%) had a hypermetry between .5–1 cm. In cases of two-time bilateral replacement measurement was made after secondary surgery. In no case did the patients disagree with the outcome.
Type 1 and 2 heterotopic calcifications of the Brooker classification were detected in four cases, with no clinical relevance. Table 2 contains a summary of the radiographic analysis.
Complications.
| Intraoperative | Postoperative |
|---|---|
| 4 cases of calcar fracture resolved in wire cerclage | 1 case of dislocation treated with closed reduction |
| 1 case of lateral femur fracture treated with wire cerclage | 1 superficial infection treated with debridement |
| Subtotal: 5 complications | 2 complications |
| Total: 7 complications (7.7%) |
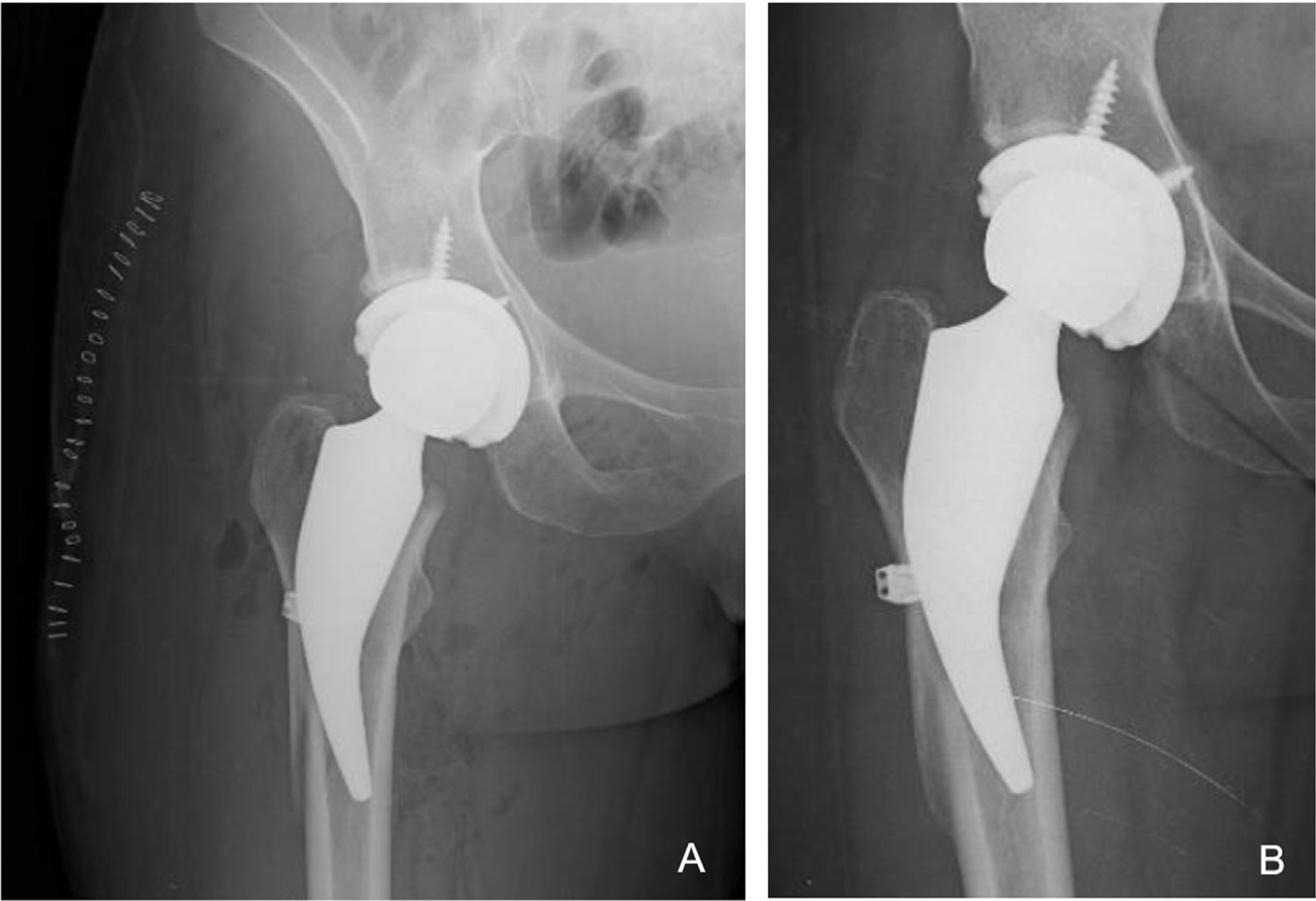
Complications and revisions: five cases of fracture were detected intraoperatively, four in the proximal calcar region (incomplete) which were treated with wire cerclage during the same primary surgery (one progressed to loosening and had to be revised two years after surgery [1.1% of the series]) and one case with fracture of the lateral cortex in a patient with pronounced coxa valga which was also treated with wire cerclage in the same surgical act as the primary replacement. Consolidation of the lateral cortex fracture was before three months and did not progress to loosening. Walking with a walker was only limited for the first 45 days (Fig.2) was allowed. All intraoperative fracture cases were within the first 30 cases performed with this implant. Postoperatively, there was one case of traumatic dislocation which was resolved with closed reduction, and one superficial surgical wound infection which resolved with medical and antibiotic treatment (Table 2).
The image shows a woman aged 32 years who underwent a THA for osteonecrosis of the right hip. A) Postoperative X-ray of the same patient with THR with cortical fracture of intraoperative lateral femoral cortex treated during surgery with monofilament twisted wire cerclage. B) AP X-ray showing a well-fixed stem with no subsidence and a consolidated lateral femoral cortex and good fixation at six months follow-up.
Clinical outcomes markedly improved in the HHS which did not alter during the follow-up period and is promising in the long term. Regarding subjective satisfaction, outcomes were excellent and good, and there were few cases of thigh pain (only detected in patients with very high functional demands were asked and this disappeared after one year). In our series improvement on the Harris scale was significant one year after follow-up with p < .01, of 42.9 points in preoperative stage (range 37–54) to 93.2 points (range, 87–96) postoperative. We found there were similarities with that reported by Lombardi et al. in their series of 93 hips with four years of follow-up where they reported that the scores on the Harris scale for the hip improved from 52.5 points prior to the operation to 84.7 at the last control.23 Other authors also reported evolutions on the functional scales, similar to our series.9,24 We believe that there could have been differences in the outcomes on the Harris scale from the first 30 cases, compared with the remainder, if we had measured this variable in all consultations. However, having assessed it at year one of follow-up we observed that after the complication the patients had good functional outcomes (HHS above 80) in all cases.
The surgical technique is demanding, since it seeks to adapt to the proximal anatomy of the femur to restore joint biomechanics. The implantation of the compacting rasps are with a specific technique which consists of taking the curve of the calcar to be able to give varus or valgus to the definitive stem, creating the opportunity to maintain the length of the limb and control the offset by positioning the stem. This determines entry and increases fracture risks, which are reported as 4%.8 In our series complications with intraoperative fractures occurred were during the first 30 cases, and were considered part of the learning curve in the vast majority of reports.25–28 In all five cases intraoperative complications were resolved with wire cerclage and delayed weight bearing during rehabilitation. Only one case progressed to loosening, and it was the only case in the entire series to be revised (1.1%).
Several authors advise against the use of short stems due to the high rate of failure or persistent pain in the thigh,8,28 mainly during the implantation technique learning period, rising to 12.1% in some stems, according to that published by Arnholdt et al. in 2017.29 In our series we found there were similar percentages of intraoperative complications amounting to 16% if we took the first 30 cases as a reference of 100%, a percentage that would be unacceptable for our surgical practice with any stem to be implanted. However, once past this learning curve of 30 patients we had no complications regarding stem implantation (0 intraoperative complications in 60 cases). The percentage of intraoperative complications dropped to 5.5% when 90 cases were reached and the trend is to continue dropping in upcoming replacements
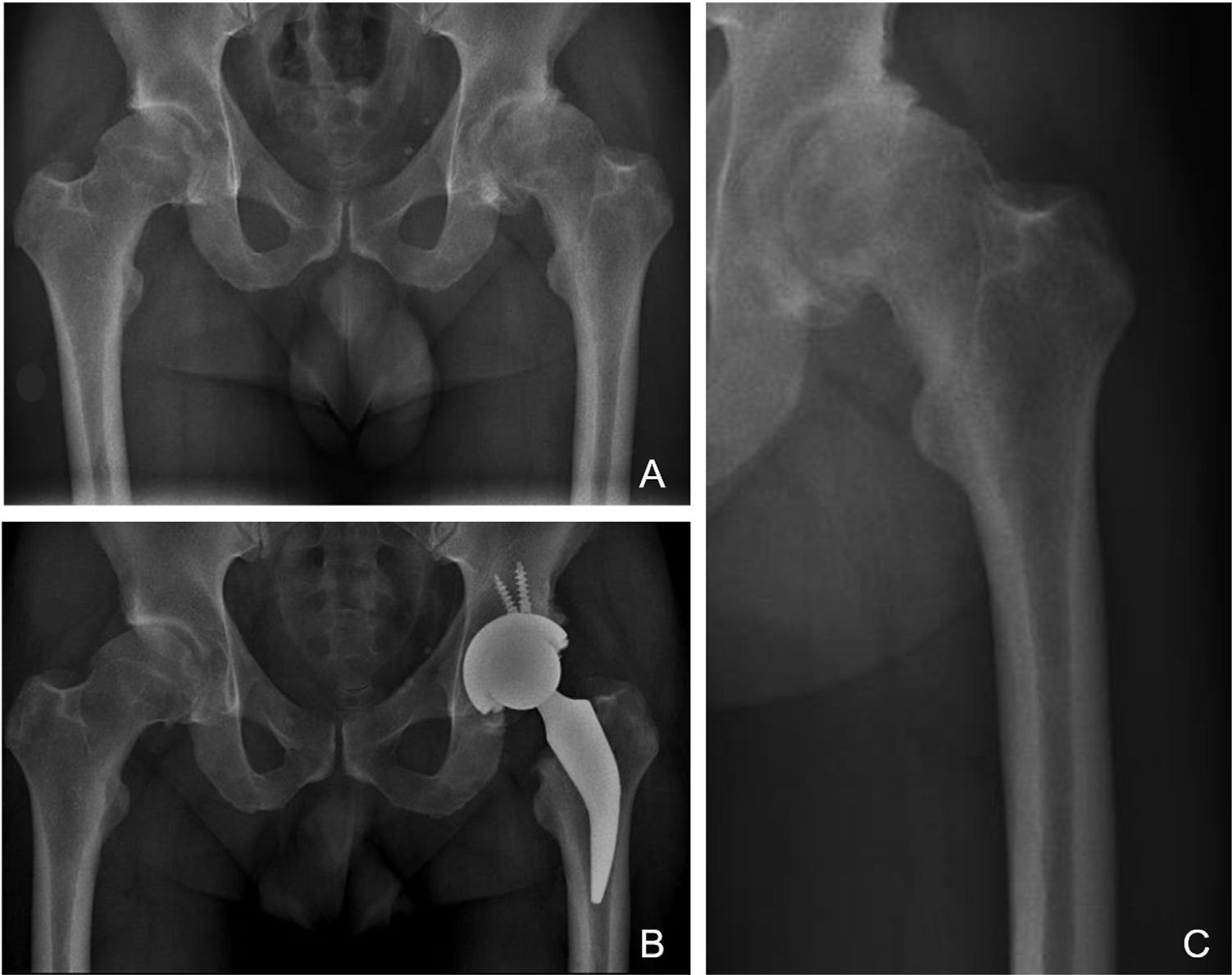
The philosophy of fixation of the stem researched classified as type 1B of the Kheir et al.,5 classification has a three-point fixation in the calcar area and proximal femoral cortex with metaphyseal fixation. The femoral neck and calcar resist the load and transfer it to the diaphysis. Preservation at the neck increases the rotational stability of the neck, which, together with metaphyseal fixation without diaphyseal invasion, avoids part of the incongruities seen in type A femurs of the Dorr classification which are more common in young adults.30 We believe this type of implant is a valid solution to potential femur-implant incompetence when placed in a Dorr A femur, since the short stem would not invade the canal at the diaphyseal level and would circumvent the conflict region, thus avoiding potential femoral fractures or problems in metaphyseal fixation of a standard, cementless stem when trying to insert it into a canal that is too thin. As can be seen in Fig. 3, where despite no preserving bone in the femoral neck, as suggested by the surgical technique and implant philosophy, the indication for implantation of a short stem would benefit from its potential revision with a metaphyseal–diaphyseal fixation stem, as it does not invade the diaphyseal region (Fig. 3).
X-rays of a 38-year-old male patient with diagnosis of advanced osteoarthritis of the left hip and who underwent THR. A) Preoperative AP X-ray where a lack of coverage of both hips is observed, with severe wear of his left hip and thick femoral cortices that could correspond to Dorr “A” classification. B) Immediate postoperative AP X-ray where a left THR is observed with restoration of his hip biomechanics; note the short stem does not invade the femoral canal at diaphyseal level, avoiding conflicts of femur-implant incompetence. C) X-ray focused on left preoperative hip where the potential conflict for implanting a cementless standard stem in a Dorr A femur is observed in greater detail.
Radiographic assessment showed trabecular bone formation patterns around the stem within the first three to six months. Using the systematic approach no progression was observed in the cases of initial migration and we coincided in correlation with clinical outcomes with those reported by Wittenberg et al. where they reported that these stems were secondarily stabilised.31 Jahnke et al. reported migrations of up to 1.5 mm in varus-valgus orientation with posterior stabilisation and no clinical relevance in patients assessed by Ein Bild Röntgen Analyse (EBRA-FCA).32 This upholds the theory which proposed that a short stem placed in varus or in valgus is not necessarily a badly positioned stem. On the contrary, we believe that the versatility of placing the preservation stem in greater or lesser valgus is a tool to try to restore the biomechanics of the patient’s native hip.
Our study has its limitations. Although the sample size is small and follow-up short we believe it is sufficient to assess the learning curve of a surgeon specialising in hips who has begun to use a new implantation technique of a stem they were not familiar with. The lack of a control group has made it impossible to compare results obtained with other implants already assessed in the long term and recognized worldwide, although this was not the main aim of this study. However, the series was fully documented, with consecutive patients and none lost to follow-up and it included the learning curve of a hip surgeon whilst using cervicometaphyseal fixation stems with a consistent and reproducible technique.
ConclusionThe clinical and radiographic outcomes of the metaphyseal fixation stem studied in this series are promising, with an acceptable learning curve, defined in our case as at least 30 patients. However, it is advisable to carry out long-term follow-up studies to confirm the success of this type of stem.
FinancingThis study did not receive any type of funding.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Godoy-Monzon D, Perez Torres J, Pascual Espinosa JM, Garcia-Mansilla A. Evaluación de la curva de aprendizaje y resultados iniciales con un vástago corto de fijación cervicometafisaria: Una serie de casos. Rev Esp Cir Ortop Traumatol. 2022;66:59–66.