The purpose of this paper is to present our experience in the treatment of the fractures of the hamate and to make a review of the literature on this topic.
Material and methodWe retrospectively reviewed 10 patients treated in our clinic between 2005 and 2012 suffering from fractures of the hamate. Six cases were fractures of the body and four were fractures of the hamate. Five cases were of associated injuries. Diagnostic delay ranged from 30 days to 2 years. Patient follow-up ranged from 1 to 10 years. Patient satisfaction was evaluated using the DASH questionnaire. Five patients with a fracture of the body underwent surgery, and one was treated conservatively. Two patients with fracture of the hook of the hamate were treated with immobilisation, and two more patients had the fragment removed.
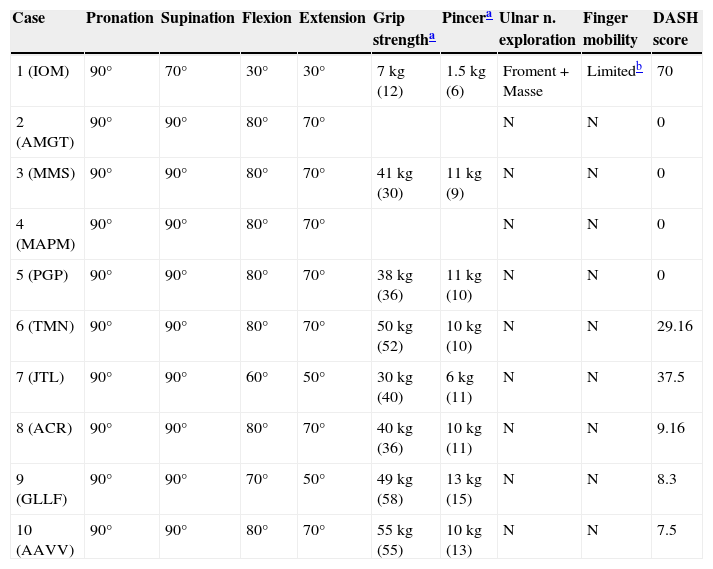
ResultsThe grip strength and the digital clip were reduced in 2 cases. Flexion and extension of the wrist was limited in 3 cases. The mobility of the fingers was normal in all the cases, except in one. The results obtained from the DASH questionnaire were normal in all the cases, except in one case of fracture of the hamate, and in two cases of fracture of the body.
ConclusionsThe surgical treatment should reduce the dislocation and stabilise the injuries with osteosynthesis. The fractures of the hamate are usually diagnosed late, and the most recommended treatment is removal of the fragment, although it cannot be deduced from this study.
El objeto de este trabajo es presentar nuestra experiencia en el tratamiento de las fracturas del ganchoso y hacer una revisión bibliográfica.
Material y métodoHemos revisado de forma retrospectiva 10 pacientes tratados en nuestro centro entre 2005–2012 que presentaban fractura del ganchoso. Seis casos eran fracturas del cuerpo y 4 fracturas del gancho. Cinco presentan otras lesiones asociadas. El retraso diagnóstico osciló entre los 30 días y los 2 años. El tiempo de seguimiento oscilaba entre 1 y 9 años. Se valoró la calidad de vida del paciente con el cuestionario DASH. Cinco pacientes con fractura del cuerpo fueron intervenidos y uno fue tratado conservadoramente. Dos pacientes con fractura del gancho fueron tratados con inmovilización y otros dos tratados con exéresis del fragmento.
ResultadosLa fuerza de prensión y de la pinza digital estaba disminuida en 2 casos. La flexoextensión de la muñeca estaba limitada en 3 casos. La movilidad de los dedos era normal en todos los casos excepto en uno. La puntuación obtenida en el DASH estaba en los límites de la normalidad en todos los casos excepto en un caso de fractura del gancho y en 2 casos de fractura del cuerpo.
ConclusionesEl tratamiento quirúrgico deberá reducir la luxación y estabilizar las lesiones con osteosíntesis. Las fracturas del gancho suelen diagnosticarse tardíamente y su tratamiento más aconsejable es la exéresis, aunque no es deducible de este estudio.
Isolated hamate (or unciform) bone fractures are infrequent lesions. According to some authors,1–6 they represent between 2% and 4% of carpal fractures, although others7 have reported a higher incidence (15%). Hamate fractures can occur in the body or the hook (or hamulus) of the bone, but are more frequent in the hook.8
Hamate fractures were classified by Milch9 and subsequently modified by Hirano and Inoue.10 Cain et al.11 and Ebraheim et al.12 classified hamate body fractures when associated to a carpometacarpal fracture-dislocation. This frequent association has been reported by several authors.11–15 It is also common to find hamate body fractures caused by high-energy trauma associated with: wrist fractures, other carpal bones and carpal dislocations which have been reported in the literature as exceptional,8,13,16–22 and accompanied by significant soft tissue lesions10 such as compartment syndrome,19 vascular, neural and tendinous lesions.
The diagnosis of hamate hook fractures is difficult. The anteroposterior and lateral radiographic projections are not normally sufficient to detect them,23 so computed tomography (CT) and magnetic resonance imaging (MRI) scans are required to complement the diagnosis. Hamate body fractures associated to a carpometacarpal fracture-dislocation are unstable lesions which in most cases require stabilisation through osteosynthesis (Kirschner wires, Herbert screws24 and miniscrews25), both of the hamate fracture and the carpometacarpal dislocation.
The objective of this work is to present our experience in the treatment of hamate fractures, and to conduct a literature review.
Materials and methodsWe conducted a retrospective study with 10 patients at our centre who suffered a hamate fracture between 2005 and 2012. There were 8 males and 2 females, with a mean age of 31.2 years (range: 20–53 years). Out of the 10 cases, 3 hook fractures and 5 body fractures affected the right hand, whilst 1 hook fracture and 1 body fracture affected the left hand. In all cases, the affected hand was the dominant.
The study included patients who fulfilled the following inclusion criteria: being of legal age and having a diagnosis of hamate fracture. We excluded from the study patients who presented a language barrier that prevented a correct understanding of the questionnaires and those who did not attend the review. Patients were evaluated by a traumatologist who was not aware of any prior pathology: mobility, sensitivity, grip and pincer strength measured with a Baseline® dynamometer (Hydraulic Pinch Gauge, Hydraulic Hand Dynamometer) and measured in kg. The Moberg sensitivity test (Discrim-A-Gon®), atrophy of the 1st commissure, Wartenberg sign, Masse sign and Froment sign to detect ulnar neurological involvement were also examined. We also assessed the actual wrist radiographs in anteroposterior, lateral and oblique projections and carpal tunnel projection. The quality of life of patients was evaluated using the DASH questionnaire. We obtained informed consent from every patient in order to carry out the study.
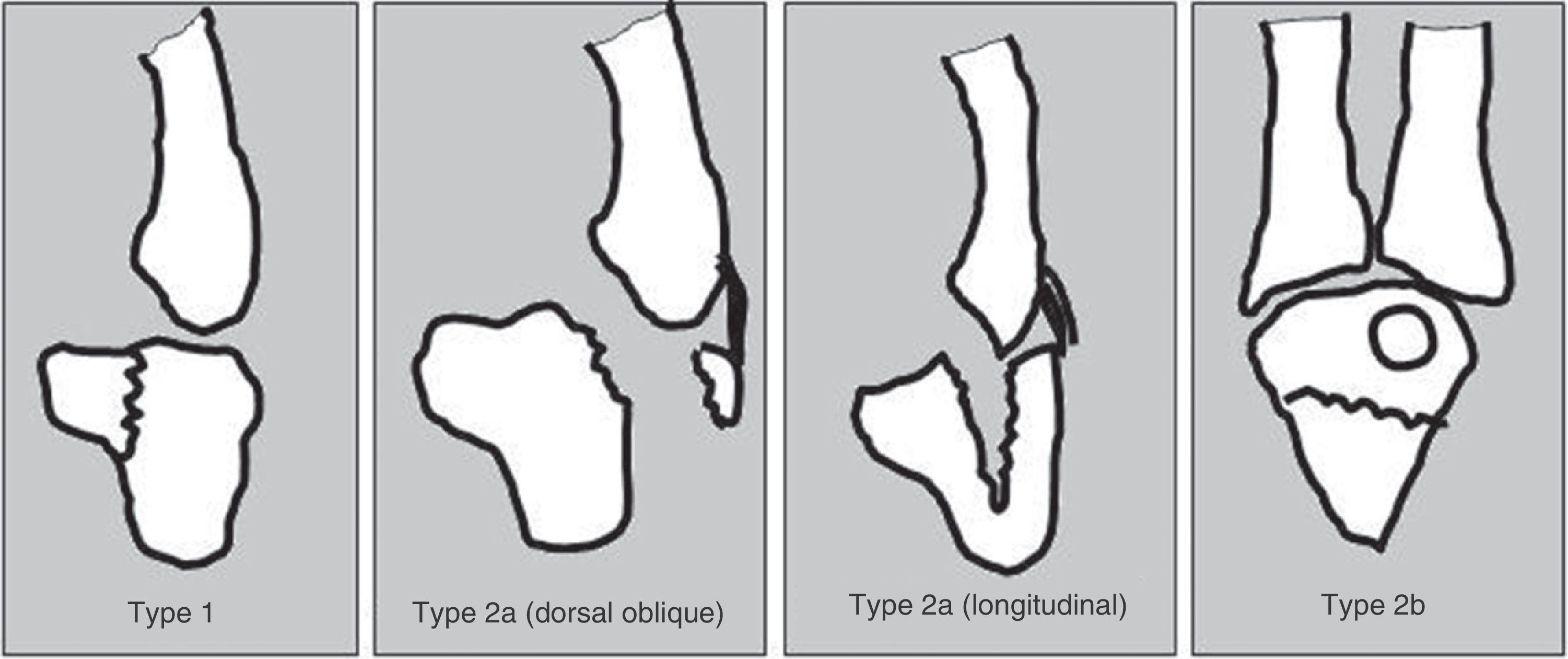
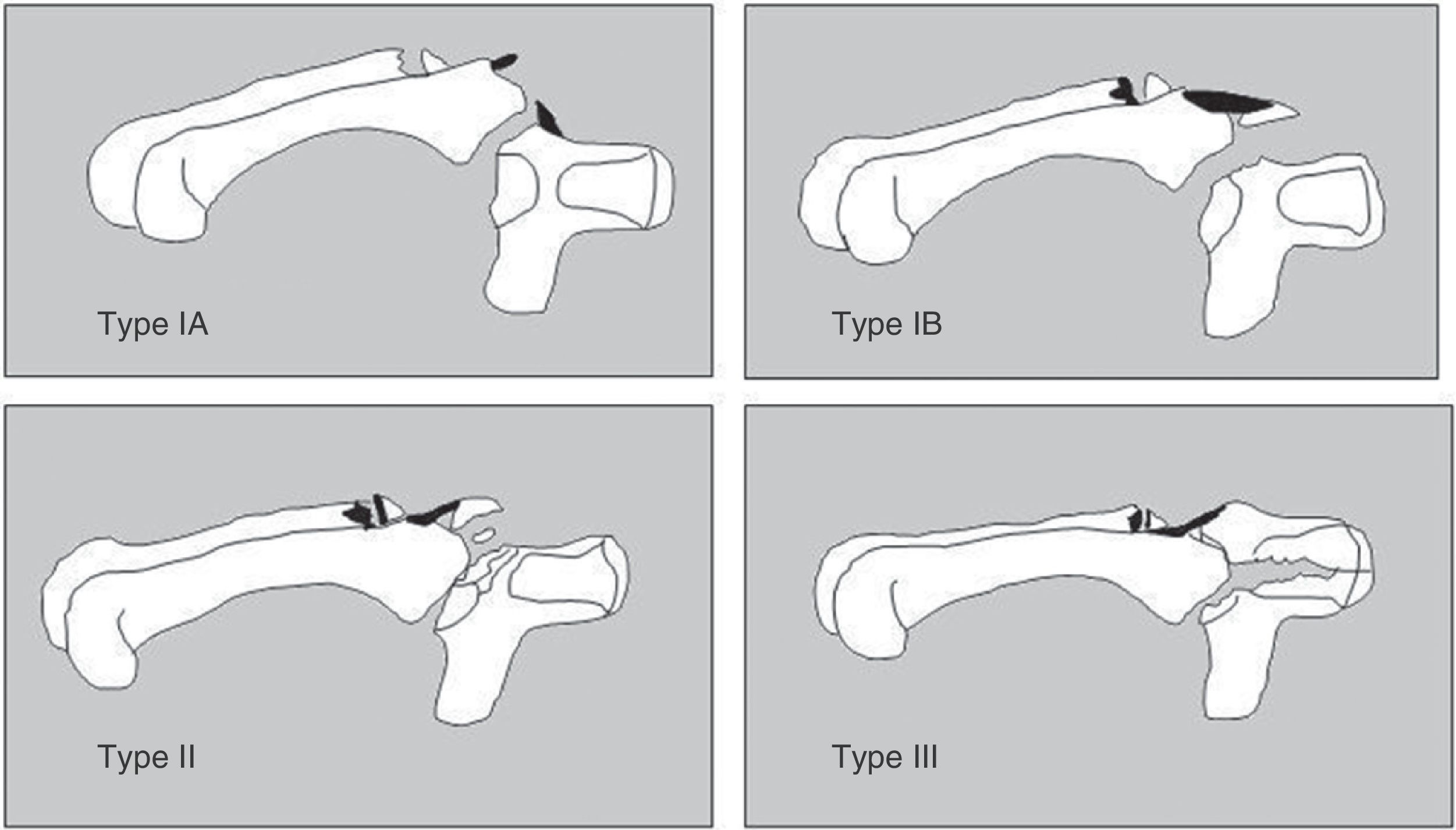
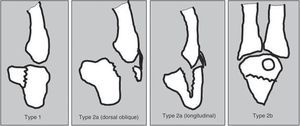
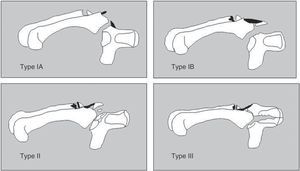
We followed the Milch classification9 as modified by Hirano and Inoue10 for isolated hamate fractures (Fig. 1) and the Cain classification11 when the hamate fracture was associated to a lesion of the carpometacarpal joint of the 4th and 5th metacarpals (Fig. 2).
Classification of hamate fractures. Type 1: hamate hook fracture. Type 2a: coronal hamate body fracture (subdivided into oblique dorsal fracture and longitudinal fracture. Type 2b: transverse hamate body fracture. Based on Hirano and Inoue.10
Classification of hamate body fractures when associated to carpometacarpal fracture-dislocation. Inclusion in this classification requires a fracture or dislocation of the base of the IV and V metacarpals. Type IA: subluxation of the base of the V metacarpal and tear of the dorsal carpometacarpal ligament. No radiographically apparent lesion of the hamate. Type IB: dorsal fracture of the hamate. Type II: dorsal comminuted fracture of the hamate. Type III: longitudinal coronal fracture of the hamate. Based on Cain et al.11.
Type 1 fracture (hook): 4 cases (1 of them associated to a scaphoid fracture).
Type 2a fractures (oblique dorsal): 4 cases: 1 with no associated lesions (case number 3), 1 with dislocation of the base of the 5th metacarpal (case number 8), 1 with fracture of the base of the 4th and dislocation of the 5th metacarpal (case number 9) and 1 with fracture-dislocation of the 4th metacarpal (case number 10).
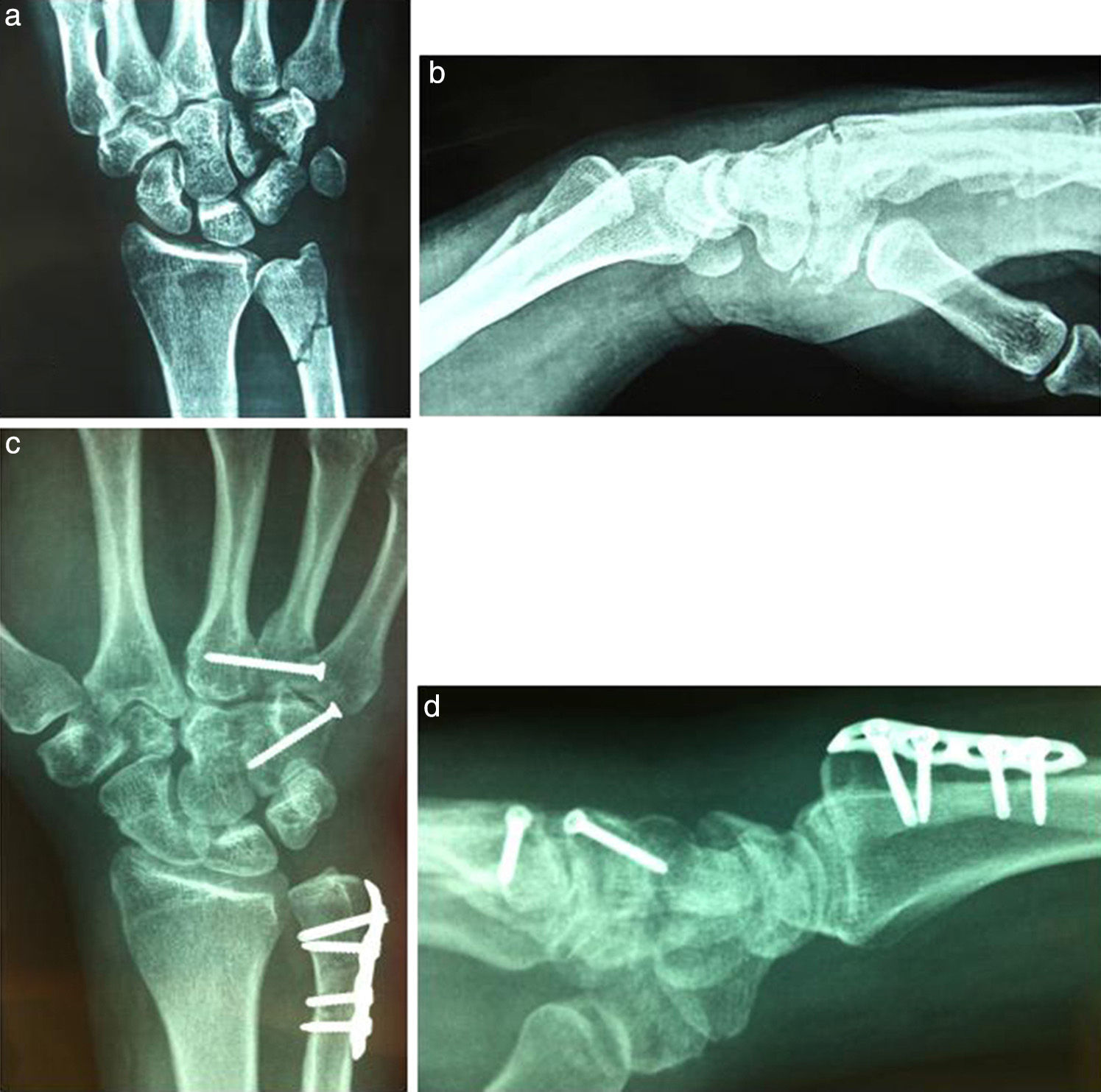
Type 2a fractures (longitudinal): 1 case with ulnar fracture and dislocation of the base of the 4th metacarpal (case number 1) (Fig. 3).
Longitudinal fracture of the hamate body, dislocation of the base of the 4th metacarpal and fracture of the ulna. (a) Anteroposterior projection. (b) Lateral projection. (c) Radiographic control after 1 year, with anteroposterior projection showing consolidation of the fractures of the ulna and hamate body and reduction of the base of the 4th metacarpal. (d) Lateral projection of case number 1.
Fractures type 2b (transverse): 1 case with dislocation of the base of the 5th metacarpal (case number 7).
According to the Cain classification we found:
Type IB: 3 cases, type II: 1 case and type III: 1 case.
The diagnostic delay for hamate hook fractures ranged between 30 days and 2 years (Table 1).
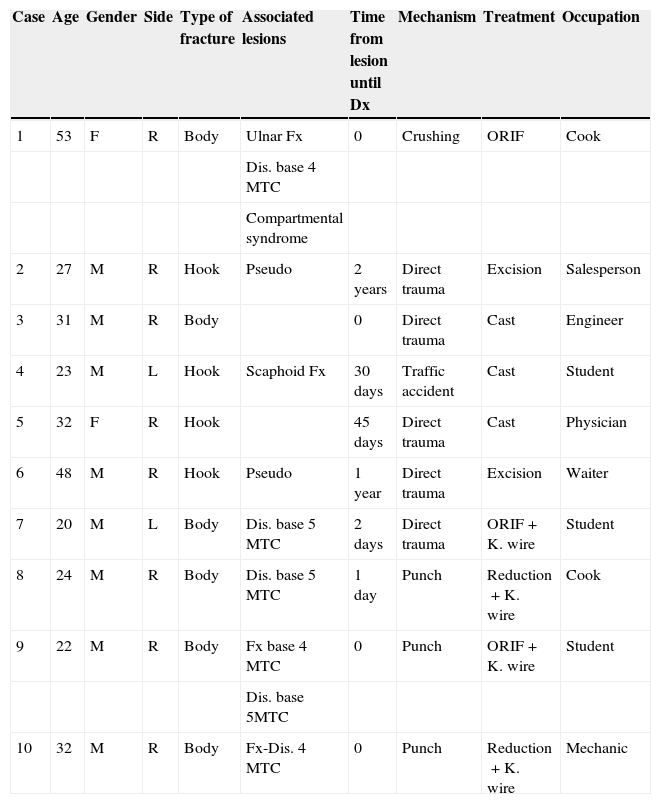
Data of the cases, epidemiology, mechanism, associated lesions, treatment and occupation.
| Case | Age | Gender | Side | Type of fracture | Associated lesions | Time from lesion until Dx | Mechanism | Treatment | Occupation |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 53 | F | R | Body | Ulnar Fx | 0 | Crushing | ORIF | Cook |
| Dis. base 4 MTC | |||||||||
| Compartmental syndrome | |||||||||
| 2 | 27 | M | R | Hook | Pseudo | 2 years | Direct trauma | Excision | Salesperson |
| 3 | 31 | M | R | Body | 0 | Direct trauma | Cast | Engineer | |
| 4 | 23 | M | L | Hook | Scaphoid Fx | 30 days | Traffic accident | Cast | Student |
| 5 | 32 | F | R | Hook | 45 days | Direct trauma | Cast | Physician | |
| 6 | 48 | M | R | Hook | Pseudo | 1 year | Direct trauma | Excision | Waiter |
| 7 | 20 | M | L | Body | Dis. base 5 MTC | 2 days | Direct trauma | ORIF+K. wire | Student |
| 8 | 24 | M | R | Body | Dis. base 5 MTC | 1 day | Punch | Reduction+K. wire | Cook |
| 9 | 22 | M | R | Body | Fx base 4 MTC | 0 | Punch | ORIF+K. wire | Student |
| Dis. base 5MTC | |||||||||
| 10 | 32 | M | R | Body | Fx-Dis. 4 MTC | 0 | Punch | Reduction+K. wire | Mechanic |
Dis.: dislocation; Dx: diagnosis; F: female; Fx: fracture; K. wire: Kirschner wire; L: left; M: male; MTC: metacarpal; ORIF: open reduction and internal fixation; R: right.
Two hamate hook fractures were treated conservatively and another 2 were treated through excision of the fragment (Fig. 4). Out of those treated conservatively, 1 affected the end of the hook, with a very small fragment, and the other was a non-displaced fracture of the base associated to a non-displaced fracture of the scaphoid. Both were treated by immobilisation with a plaster cast.
Fracture of the hamate hook. (a) Anteroposterior projection, (b) and lateral projection, with no visible fracture. CT axial projection, (c) and sagittal projection, (d) showing the fracture of the hamate hook. Current CT images after the excision, axial projection (e) and sagittal projection (f) of case number 2.
Five fractures of the hamate body were treated surgically; all of them were associated to a carpometacarpal dislocation that was reduced and stabilised with a Kirschner wire in 4 cases and with a screw in 1 case. One of the hamate body fractures was associated to a fracture of the 4th metacarpal, and was reduced and stabilised with a Hand Innovation® miniplate with 1.5mm screws. Another hamate body fracture was associated to an ulnar fracture treated by osteosynthesis with a plate (case number 1). The hamate body fracture was stabilised with a compression screw in 1 case and with a miniplate (case number 7) in 1 case. In 3 cases, the fragment of the hamate bone was so small that it precluded osteosynthesis, instead being treated by stabilisation of the carpometacarpal joint. One non-displaced fracture of the hamate body was treated by immobilisation.
ResultsWe explored the mobility of the affected wrist and found pronation with no kind of limitation, and full supination except in case number 1, where it was 22% compared to the healthy side. Flexion and extension were limited in cases 1-7-9. Radial and ulnar deviations were complete (Table 2).
Results obtained for mobility, grip strength and pincer, neurological exploration and DASH scale.
| Case | Pronation | Supination | Flexion | Extension | Grip strengtha | Pincera | Ulnar n. exploration | Finger mobility | DASH score |
|---|---|---|---|---|---|---|---|---|---|
| 1 (IOM) | 90° | 70° | 30° | 30° | 7kg (12) | 1.5kg (6) | Froment+Masse | Limitedb | 70 |
| 2 (AMGT) | 90° | 90° | 80° | 70° | N | N | 0 | ||
| 3 (MMS) | 90° | 90° | 80° | 70° | 41kg (30) | 11kg (9) | N | N | 0 |
| 4 (MAPM) | 90° | 90° | 80° | 70° | N | N | 0 | ||
| 5 (PGP) | 90° | 90° | 80° | 70° | 38kg (36) | 11kg (10) | N | N | 0 |
| 6 (TMN) | 90° | 90° | 80° | 70° | 50kg (52) | 10kg (10) | N | N | 29.16 |
| 7 (JTL) | 90° | 90° | 60° | 50° | 30kg (40) | 6kg (11) | N | N | 37.5 |
| 8 (ACR) | 90° | 90° | 80° | 70° | 40kg (36) | 10kg (11) | N | N | 9.16 |
| 9 (GLLF) | 90° | 90° | 70° | 50° | 49kg (58) | 13kg (15) | N | N | 8.3 |
| 10 (AAVV) | 90° | 90° | 80° | 70° | 55kg (55) | 10kg (13) | N | N | 7.5 |
DIP, distal interphalangeal joint; MCP, metacarpophalangeal joint; N, normal; PIP, proximal interphalangeal joint.
Grip and pincer strength were significantly decreased in the affected hand compared to the contralateral hand in cases 1 and 7. Exploration of the ulnar nerve found no differences between the affected hand and the contralateral except in case 1, which presented positive Masse and Froment signs.
Finger mobility in the affected hand was normal in all cases except for number 1, in whom the metacarpophalangeal, proximal interphalangeal and distal interphalangeal movements of all the fingers were limited due to compartmental syndrome.
The quality of life of patients in relation to the results of the treatment was measured using the DASH questionnaire. The score registered in hamate hook fractures was of 0 in 3 cases and 29 in 1 case. In hamate body fractures, the DASH score was under 10 in 4 cases. One case with a score of 37 and another case with a score of 70 corresponded to patients with high-energy trauma with extensive soft tissue involvement.
DiscussionThe mechanism of hamate hook lesions can be direct or indirect. The direct mechanism involves falls with the wrist in extension or impacts on the hypothenar eminence and, occasionally, repeated trauma caused by practicing certain sports (golf, baseball, tennis). The indirect mechanism involves strong contractions of the flexor carpi ulnaris with avulsion from the base of the hamate hook transmitted through the pisohamate ligament. The largest series of hamate hook fractures is that described by Stark et al.26
The mechanism in hamate body fractures is generally a trauma on the hand with a closed fist against a strong object. With a dorsal and proximal displacement, the base of the metacarpal (MTC) impacts against the dorsal and distal edge of the hamate and separates a dorsal fragment thereof.8,27,28 If the impact exceeds the capacity of the 4th and 5th MTC, there is a fracture or dislocation and the load transfer determines the degree and type of hamate lesion. Flexion during the impact results in a dorsal dislocation of the base of the 5th MTC, tear of the dorsal carpometacarpal ligament and, often, a fracture of the dorsal edge of the hamate. Axial loads through a minimally flexed 4th–5th MTC cause a type III hamate lesion11 and when the 4th–5th MTC are in extension they determine a rare palmar dislocation13,14 caused by the tension of the pisometacarpal ligament. It is the tension of the pisohamate ligament that causes the fracture of the hamate hook. This rare combination of hamate hook fracture and anterior dislocation of the base of the 5th MTC can be an indirect sign of a lesion of the flexor carpi ulnaris complex at a distal level, which led Garcia-Elias et al.13 to believe that excising the fragment of the hook is not advisable under such circumstances, although it can be done in other situations. In our series, all the fractures except for 1 were associated to a carpometacarpal lesion of the 4th and 5th metacarpals.
The mechanism that explains hamate lesions associated to other carpal bones12,18,21 seems to involve a traction force acting through the transverse ligament of the carpus, causing compression of the transverse arch of the carpus, which is transmitted through the accessory ligaments for the scaphoid,8,16 trapezium21… There have also been reports of associations of hamate fractures with wrist fractures17 as a consequence of high-energy lesions. In our series, case number 1 presented an associated ulnar fracture and case number 4 a scaphoid fracture. The prognosis of these high-energy lesions is worse than in the rest of the mechanisms,26 as evidenced by case number 1.
The diagnosis is difficult to obtain in hamate hook fractures with a vague pain located in the hypothenar eminence. In any dorsal dislocation of the base of the 4th and 5th MTC we must always consider a hamate fracture.12,27,28 It is difficult to establish a diagnosis based on the anteroposterior and lateral radiographic projections; instead projections in oblique pronation11,27 at 45° and 15° are required, which for other authors12,29 should be at 30°, whilst Stark et al.26 and Yamazaki et al.30 recommend a projection in 45° supination with the wrist in dorsiflexion. The carpal tunnel projection is useful in hamate hook fractures, but can be painful during acute phases.24,26 However, an MRI scan will provide sufficient bone and soft tissue details, thus surpassing other tests due to its high sensitivity and specificity. It can also be useful to obtain 3D-CT and high-density CT scans with the wrist in a “praying position” so as to compare both wrists and exclude congenital anomalies.4,6,26 This is a technique of choice for the diagnosis of hamate hook fractures.6,31
The literature reports a high rate of failures5,6,26 with conservative treatment based on immobilisation of hamate hook fractures. In cases with delayed diagnoses or acute and displaced fractures, the treatment of choice is excision, even if the patients are asymptomatic,4,10,23,32 due to the high risk of pseudoarthrosis6 and tear of the 4th and 5th finger flexors. For Hirano and Inoue10 and García Elias et al.,13 fixation with screws may be indicated in exceptional cases. It is a demanding technique, although some authors perform it percutaneously through a dorsal approach.5 Similar results have been published following excision and reduction and internal fixation, although the healing time was shorter with excision.6
In carpometacarpal fracture-dislocations, failure to achieve a reduction of the dislocation with the corresponding carpometacarpal joint congruence may lead to a reduction of grip strength.3 We prefer to apply a conservative treatment based on immobilisation in stable type IA and IB cases, whilst for unstable cases we carry out percutaneous fixation with Kirschner wires to the 3rd MTC,10,11,28,33 although this method cannot ensure a satisfactory reduction. In types II and III lesions, open reduction is indicated to reconstruct soft tissues and restore and fix the hamate bone fragment using a plate or screws to create joint congruence; optionally fixing with Kirschner wires if the stability of the carpometacarpal joint is in doubt.
Diagnostic delay3,4,7,23,26,34 is the norm in hamate hook fractures, and has been quantified by Stark et al.23 in 5.8 months. In our series, this ranged between 30 days and 2 years. Routine radiographs conducted in emergency services do not usually detect this lesion and only the suspected diagnosis will lead to requesting an MRI and/or CT scan which will confirm the hook fracture.
Osteonecrosis and non-union are possible complications described in hamate hook fractures.6 In addition, median35 and cubital nerve lesions caused by compression of the displaced hamate hook fragment have also been reported, particularly of the motor branch, as well as section of the ulnar nerve during the surgical approach.4,36 There have also been reports of tenosynovitis and tear of the 4th and 5th finger flexor tendons caused by constant erosion against the rough bone surface of the hamate hook fracture, more frequent in the 5th than in the 4th.23,26,29–32,34,37,38 A closed lesion of the 5th finger tendon should lead to suspicion of non-union of a hamate hook fracture.30 There have also been reports of compartmental syndrome19 resulting from high-energy trauma, as in case number 1 in our series.
We can conclude that hamate hook fractures are usually diagnosed belatedly and their most advisable treatment is excision. Hamate body fractures are frequently associated to a carpometacarpal fracture-dislocation. Surgical treatment should reduce the dislocation and stabilise the lesion through osteosynthesis.
Level of evidenceLevel of evidence IV.
Ethical responsibilitiesProtection of people and animalsThe authors declare that this investigation did not require experiments on humans or animals.
Confidentiality of dataThe authors declare that they have followed the protocols of their workplace on the publication of patient data.
Right to privacy and informed consentThe authors declare that this work does not reflect any patient data.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Condés JMS, Martínez LI, Carrasco MAS, Julia FJC, Martínez ELS. Fracturas del ganchoso. Rev Esp Cir Ortop Traumatol. 2015;59:299–306.