Arthrodiastasis consists of the mobilisation of the hip while distracted by a hinged distractor. The aim of our study is to show the results of the treatment of late-onset Perthes disease with this technique in our institution.
Material and methodsAmbispective review of all the cases that underwent this surgery in our Department of Paediatric Orthopaedics between 2010 and 2014 with the following inclusion criteria: patients over 8 years old, with minimal deformity, and poor prognosis. Mobility, pain, Trendelenburg sign, radiographic sphericity, and complications were assessed.
ResultsA total of 13 patients (9 male, 4 female) were included. The mean age was 11.93 years. Radiographic risk signs were present in 7 cases. The mean decrease in pain measured with a visual analogue scale (VAS) after the surgery was 3.83 points (P<.05). Cephalic sphericity was maintained in 11 cases during follow up (1.75 years). Complications were observed complications in 84.6% of the patients, with infection of the screw tract being the most frequent. All of them were easy to treat.
ConclusionsArthrodiastasis is a minimally invasive technique, useful in the treatment of late onset Perthes disease. It improves clinical results and maintains cephalic shape when applied in early stages. However, it is not free of complications, which can involve as many as 8 out of 10 patients treated with the technique.
La artrodiastasis consiste en la movilización de la cadera mediante la distracción por medio de un fijador externo articulado. El objetivo de nuestro estudio es mostrar los resultados obtenidos en nuestro centro en el tratamiento de la enfermedad de Perthes de inicio tardío o de mal pronóstico con esta técnica quirúrgica.
Material y métodosRevisión ambispectiva de todos los casos intervenidos en nuestro servicio de ortopedia infantil entre los años 2010 y 2014 con los siguientes criterios de inclusión: pacientes mayores de 8 años, con mínima deformidad y pronóstico desfavorable. Se evalúan movilidad, dolor, Trendelenburg, esfericidad radiológica y complicaciones.
ResultadosSe incluyeron 13 pacientes, 9 de ellos varones, con una edad media de 11,93 años. Siete casos presentaron signos radiológicos de riesgo. La disminución del dolor mediante EVA tras la cirugía fue cuantificada en 3,83 puntos (p<0,05). Once casos mantuvieron la esfericidad cefálica durante el seguimiento (1,75 años). Las complicaciones observadas ascendieron al 84,6% de los casos, siendo la más frecuente la infección del trayecto de los tornillos, si bien fueron todas de sencillo manejo.
ConclusionesLa artrodiastasis constituye una técnica mínimamente invasiva y útil en el tratamiento de Perthes de inicio tardío o de mal pronóstico, mejorando la clínica y manteniendo la esfericidad cefálica, siendo recomendable el tratamiento de estos pacientes al inicio de la enfermedad. Sin embargo, no está exenta de complicaciones, que pueden afectar a 8 de cada 10 pacientes tratados.
Hip arthrodiatasis (from the Greek arthro [joint], dia (through) and tasis (stretch))1 consists of mobilising the same under the distraction created by an external fixator. Arthrodiatasis was first described in the knee and elbow by Volkov2 in 1975, and it was used for the first time in the hip by Aldegheri in 1979.1 The term “arthrodiastasis” came into general use as a synonym after the work published by Cañadell et al. in 1993.3
There are studies which show that distraction at the level of the hip joint has positive effects on bone regeneration and the prevention of cartilage degeneration at a femoral as well as acetabular level.3–6 It also seems to prevent the collapse of necrotic bone, while some studies even suggest an increase in the vascularisation of the tissues around the joint.7
Arthrodiastasis seeks to use an external fixator to neutralise muscular forces and the transmission of loads which act at the level of the hips during walking. This makes it a therapeutic option in the treatment of hip diseases, in which the annulation of collapsing forces is the basis of the therapy. Joint movement is maintained in the sagittal plane by means of an articulated hinge that permits distraction without excessively restricting mobility.
The natural evolution of serious forms of Legge-Calvé-Perthes’ disease causes cephalic collapse, resulting in joint incongruence. This gives rise to areas in which the hip is subjected to greater stress, leading to premature degenerative changes.
Hip arthrodiastasis is used in those cases with a poor prognosis in which the usual treatment gives poor results, usually in children aged from 8 to 10 years old. At these ages varicose femoral osteotomy may increase joint incongruence due to ulterior lack of remodelling capacity.8 It also causes gluteal insufficiency, while valgus osteotomy may potentially improve the transmission of loads to the affected area of the femoral head at the cost of favouring subluxation, without leading to an improvement in the avascular process.9 Lastly, acetabular osteotomies10 to reposition or increase the size of the acetabulum may increase the support of the femoral head. However, they often fail to reduce pressure on the femoral head or modify its morphology. No treatment has been proven to be significantly effective in improving the results of Legge-Calvé-Perthes disease in children older than 8 years old. This may be due in part to difficulties in evaluating the effect of the treatment of a disease with a highly variable course, duration and results. It may also be due to the methodology of the studies, which lack a control group.11,12 The aim of arthrodiastasis is to prevent the gradual collapse of the bone and flattening of the head which occurs in the majority of cases of Legge-Calvé-Perthes disease above 8–10 years old. It also achieves the preservation of a certain degree of joint mobility in the anteroposterior plane, while it also permits walking, even with partial loading of the joint.
The aim of our study is to show the results obtained in surgical treatment using arthrodiastasis in patients diagnosed with late onset Legge-Calvé-Perthes disease or cases with a poor prognosis.
Material and methodsAn ambispective revision was undertaken of all the cases operated in our paediatric orthopaedic department in the years from 2010 to 2014, with the following inclusion criteria: patients older than 8 years old, with minimum deformity and an unfavourable prognosis. Demographic data together with preoperative and surgical evaluations were gathered retrospectively, while follow-up evaluation was performed prospectively.
Surgical techniqueWe use a monolateral external fixator with an articulated hinge that permits hip flexion-extension: the Small Blue Dynamic Axial Fixator (DAF)® while the hinge is the Small DAF Self-Aligning Articulated Body® (Orthofix, Verona, Italy). We also use hydroxyapatite-coated screws of the maximum possible diameter, keeping this to less than 1/3 of femoral diaphysis diameter (OsteoTite®, Orthofix, Verona, Italia).
The patient is operated under general anaesthesia and is placed in supine decubitus on a radiotransparent table, raising the ipsilateral hip by means of a surgical cloth. The sterile surgical field includes the whole operated limb up to the iliac crest, using stockinet on the leg.
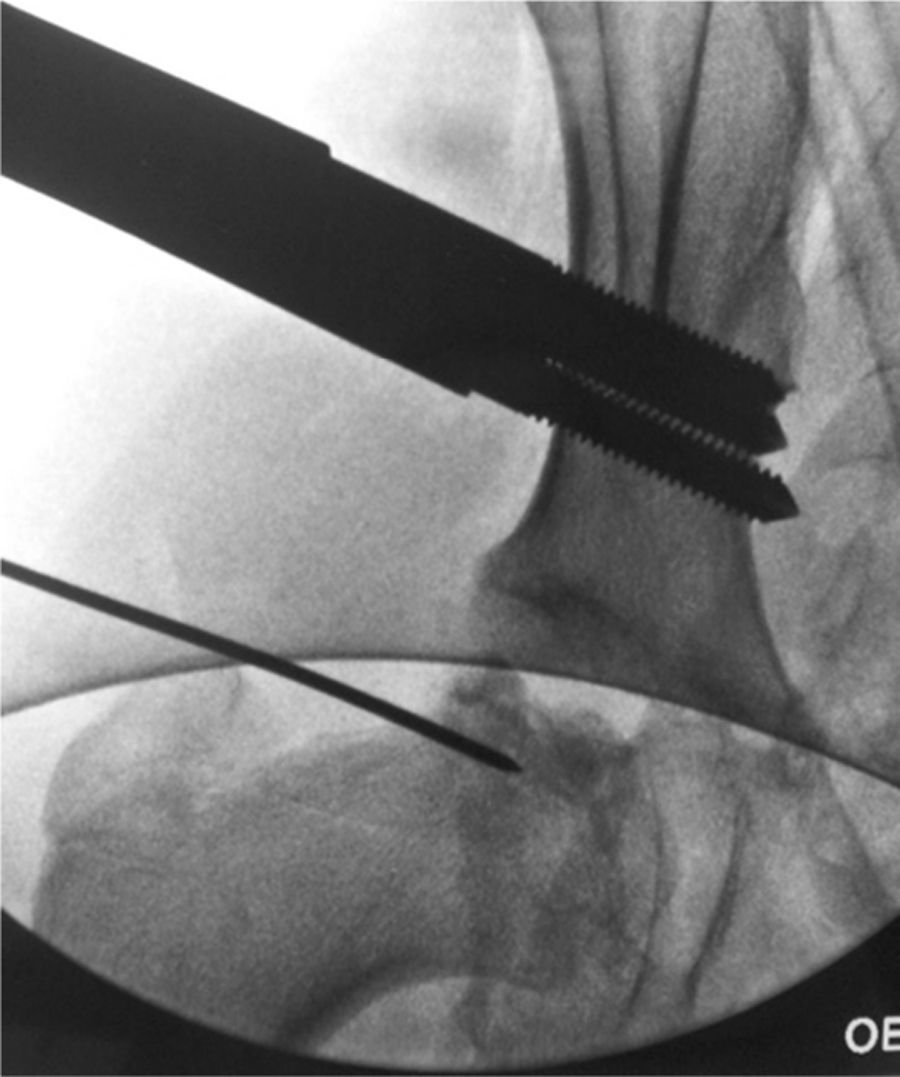
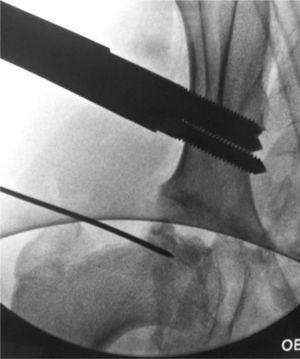
The centre of femoral head rotation is located under fluoroscopic control. The first step consists of inserting, perpendicular to the skin, a needle that is used as a guide in the centre of the femoral head. This will be our reference for positioning the hinge of the external fixator.
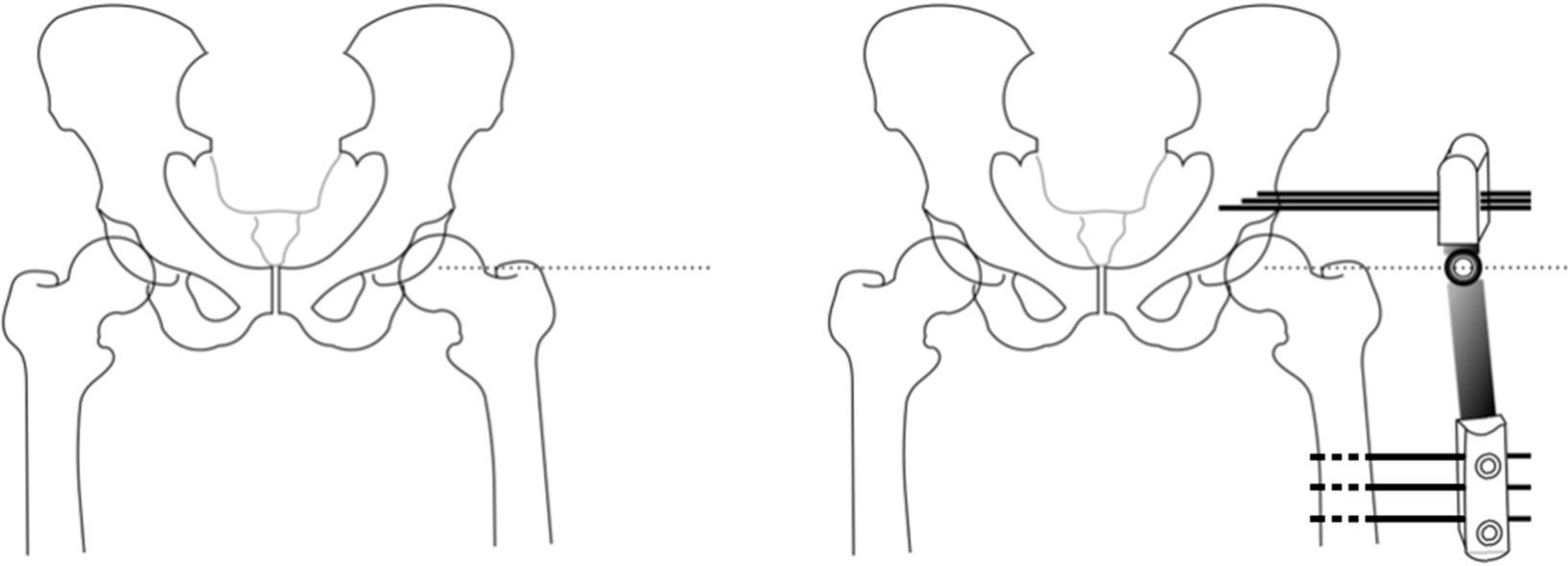
We insert 3 supraacetabular screws through the iliac wing in a transversal arrangement to the longest axis of the limb and parallel to each other, with the aid of a template in “T” (Small DAF T-Clamp template®, Orthofix, Verona, Italia) of the fixator and without surpassing the internal cortex to prevent intrapelvic injury. We have to take the fact that the inside of the iliac wing is “lined” with the iliac muscle. We use a fluoroscope projection at a shutter angle of 45∘. We use 3 more bicortical screws in the femoral diaphysis, arranged longitudinally along the same and parallel to each other, using the Small DAF Straight-Clamp Template® (Orthofix, Verona, Italy). The templates are then replaced by the definitive fixator (Small Blue DAF T Clamp®, Orthofix, Verona, Italy) (Figs. 1 and 2).
Surgical procedure of articulated arthrodiastasis. Firstly the centre of rotation of the femoral head is located by fluoroscopy and a Kirschner needle is inserted to serve as a reference. We then position 3 supraacetabular screws transversal to the longest axis of the femur, and 3 diaphyseal screws. The location of the external fixator hinge over the centre of rotation is especially important, so that we make this coincide with the guide needle. Before fixing the assembly, we perform a 15–20∘ abduction of the limb which allows the patient to sit.
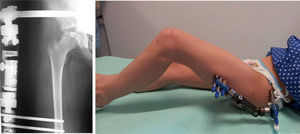
Hip abduction prior to fitting the external fixator structure is marked by the separation that is necessary to reach the sitting position, with the patella facing the zenith at approximately 15–20∘.11,13,14
We then withdraw the guide needle and check the range of movement under anaesthesia. We start to apply distraction in the operating theatre, to take advantage of the general anaesthesia (Fig. 3). The fixator opening is set to around 0.5–1cm3. Given the loss of distraction over time, it is checked and increased every 1 or 2 weeks until it is removed.
Partial loading by the patient is permitted from the first, using two crutches, and diastasis is maintained at approximately 4 months, after identification of the formation of the lateral column in the follow-up X-ray. We have to take into account that joint diastasis has to be achieved gradually, given that gradual elongation leads to neovascularisation of the tissues, while abrupt distraction causes pain and limitation of the range of movement.7
We remove the external fixator under general anaesthesia, with plasty of the scar edges to prevent adherences of the skin to deep tissues. We do not perform curettage of the trajectory of the screws if there are no signs indicating infection.
Study variablesJoint balance is studied before and after the operation, together with the presence of gluteal insufficiency (the Trendelenburg sign), limping and grading pain on the visual analogue scale (VAS). The presence of signs of a poor prognosis is evaluated radiographically, together with the joint distraction achieved and the sphericity obtained at the end of follow-up according to the criteria proposed by Stulberg. Nevertheless, this is not in itself a Stulberg classification as no all of the patients had attained skeletal maturity by the end of follow-up. The sphericity observed at the end of follow-up is compared with the degree of the same seen at the start of the treatment. The appearance of complications was also recorded. The pain present before and after the treatment is compared. The results obtained were analysed using the SPSS® computer program, version 22 for MacOS. Results were considered statistically significant when P<.05.
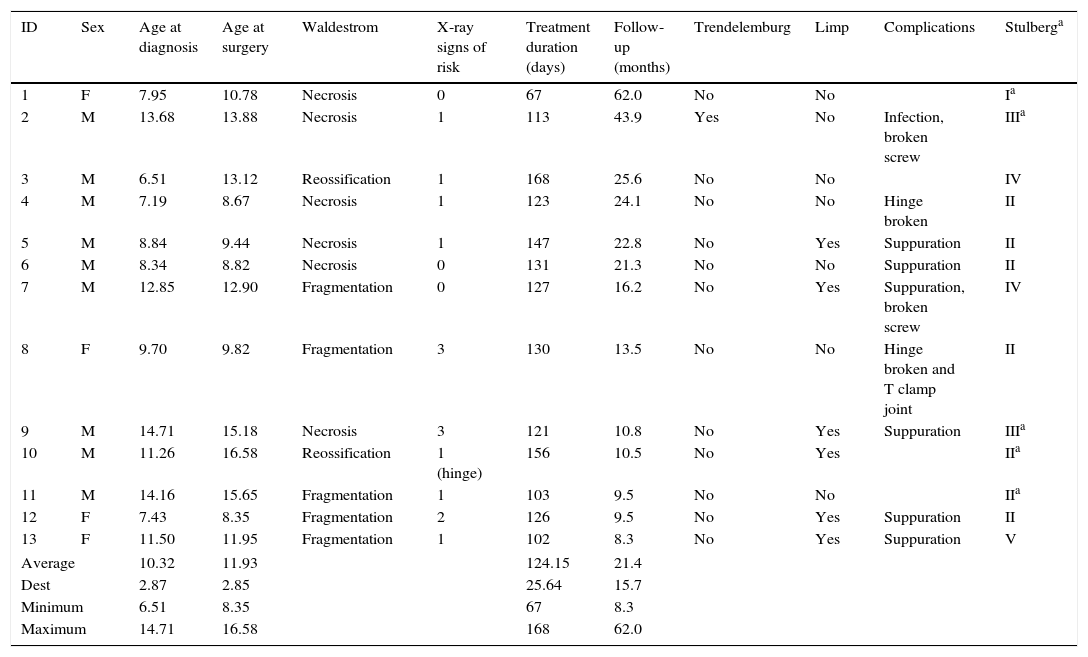
ResultsA total of 13 patients (Table 1) fulfilled the inclusion criteria (9 males and 4 females) with an average age at the time of surgery of 11.93 years old [range: 8.35–16.58; SD: 2.85]. The average time between diagnosis and the operation was 1.74 years [range: 17 days–6.6 years; SD: 2.13]. At the moment of surgery 2 patients were in the reossification phase, 6 in the necrosis phase and 5 in the fragmentation phase. In 8 cases (61.5%) there were radiological signs of risk, such as lateral calcification (1), metaphysis rarification (3), Gage's sign (6) or subluxation (1). One of the cases was already in an advanced phase of subluxation with hinge deformity.
Patient characteristics.
| ID | Sex | Age at diagnosis | Age at surgery | Waldestrom | X-ray signs of risk | Treatment duration (days) | Follow-up (months) | Trendelemburg | Limp | Complications | Stulberga |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | F | 7.95 | 10.78 | Necrosis | 0 | 67 | 62.0 | No | No | Ia | |
| 2 | M | 13.68 | 13.88 | Necrosis | 1 | 113 | 43.9 | Yes | No | Infection, broken screw | IIIa |
| 3 | M | 6.51 | 13.12 | Reossification | 1 | 168 | 25.6 | No | No | IV | |
| 4 | M | 7.19 | 8.67 | Necrosis | 1 | 123 | 24.1 | No | No | Hinge broken | II |
| 5 | M | 8.84 | 9.44 | Necrosis | 1 | 147 | 22.8 | No | Yes | Suppuration | II |
| 6 | M | 8.34 | 8.82 | Necrosis | 0 | 131 | 21.3 | No | No | Suppuration | II |
| 7 | M | 12.85 | 12.90 | Fragmentation | 0 | 127 | 16.2 | No | Yes | Suppuration, broken screw | IV |
| 8 | F | 9.70 | 9.82 | Fragmentation | 3 | 130 | 13.5 | No | No | Hinge broken and T clamp joint | II |
| 9 | M | 14.71 | 15.18 | Necrosis | 3 | 121 | 10.8 | No | Yes | Suppuration | IIIa |
| 10 | M | 11.26 | 16.58 | Reossification | 1 (hinge) | 156 | 10.5 | No | Yes | IIa | |
| 11 | M | 14.16 | 15.65 | Fragmentation | 1 | 103 | 9.5 | No | No | IIa | |
| 12 | F | 7.43 | 8.35 | Fragmentation | 2 | 126 | 9.5 | No | Yes | Suppuration | II |
| 13 | F | 11.50 | 11.95 | Fragmentation | 1 | 102 | 8.3 | No | Yes | Suppuration | V |
| Average | 10.32 | 11.93 | 124.15 | 21.4 | |||||||
| Dest | 2.87 | 2.85 | 25.64 | 15.7 | |||||||
| Minimum | 6.51 | 8.35 | 67 | 8.3 | |||||||
| Maximum | 14.71 | 16.58 | 168 | 62.0 | |||||||
The average passive joint balance before surgery was: flexion-abduction: 32.5∘ (SD: 12.7; range: 20–60∘), internal rotation: 6.67∘ (SD: 7.49; range: 0–20∘), external rotation: 30∘ (SD: 26.96, range: 0–80∘). 2 patients had Trendelenburg sign (16.6%) and 12 limp (92.3%).
An external fixator with 3 supraacetabular and 3 diaphysis screws was used in all of the cases except one in which only 2 diaphysis and 2 supraacetabular screws were used. The average time to extraction of the osteosynthesis material was 124.2 days (range; 67–168 days, SD: 25.64).
Patients evaluated pain intensity on the visual analogue scale (VAS), and the average VAS before surgery was 3.83 (range 0–8, SD: 2.82). During treatment with the fixator VAS was evaluated at an average of 4.83 (range 0–9, SD: 3.43), while after removal of the same it stood at 1 (range: 0–8, SD: 2.37). The reduction in pain according to the VAS from before surgery to afterwards was statistically significant (P<.05).
The average follow-up time was 1.75 years (248–1859 days) during which the average passive joint balance following the operation was: flexion-abduction 49.5∘ (range: 30–70∘; SD: 13.43), internal rotation: 19.55∘ (range: 5–45∘; SD: 13.43) and external rotation: 31.11∘ (range: 20–65∘; SD: 17.46). The average age at the end of the follow-up was 13.92 years old [range: 9.42–17.87 years old; SD: 3.08], and 5 patients had attained skeletal maturity. Final cephalic sphericity (calculated according to the adaptation of the parameters proposed by Stulberg for skeletally mature hips) was Stulberg I (one case, 7.7%), Stulberg II (7 cases, 53.8%), Stulberg III (2 cases, 15.4%), Stulberg IV (2 cases, 15.4%) and Stulberg V (one case, 7.7%). In those patients who attained skeletal maturity a true Stulberg was found of I (1 patient), II (2 patients) and III (2 patients). At the end of the follow-up, the shape of the femoral head at the start of arthrodiastasis had not changed in 11 of the 13 cases operated (84.6%), while in 2 cases (15.4%) the shape had become slightly less spherical in spite of the procedure. In the case in which hinge deformity existed prior to the operation, this did not change following the surgery.
The 11 [84.6%] complications observed included infection of the trajectory of the screws (7 cases, 53.8%) which was treated using oral antibiotics, except for one case that required admission for intravenous antibiotic treatment. At least one screw broke in 2 cases (15.4%) involving a supraacetabular screw in one case and a femoral screw in another that did not require intervention and, finally, on 2 occasions (15.4%) the external fixator disconnected due to failure of its hinge or proximal head. This required the manufacture by hand of a new system using a stainless steel ring (in one case the failure was exclusively of the hinge, while the other involved the hinge as well as the T-Clamp connection) (Fig. 4). In all cases at least one of the screws was observed to loosen, which in no case caused instability of the system.
DiscussionSome authors have used jointed distraction in hips with minimum collapse to maintain epiphysis height, and they have described results showing this together with the detention of epiphysis collapse.11 Our results show that over the short term cephalic deformation ceases with the treatment, preventing the progressive deformities that would arise in the natural course of the disease.
An improvement in active and passive joint balance has been detected over the short term, together with a reduction in pain. Supralateral subluxation has been found in the treatment of avascular necrosis15 and in Legge-Calvé-Perthes disease.13,16 These data can be extrapolated to those obtained in our series.
Some authors such as Segev17,18 and Kocaoglu4 accompany hip distraction with tenotomies and capsular liberation; in our case we ruled out the use of adductor and psoas tenotomies as they had been shown to be completely ineffective in previous studies. This is because the contracture is not only of the adductor longus muscle, but rather involves the whole complex of muscles around the hips. Moreover, the myotendinous section spontaneously cures in about 2–3 weeks.19
The long-term results described in the bibliography, such as those presented by Segev, with results after skeletal maturing and an average follow-up of 5.7 years, state that although their preliminary short-term descriptions had shown an improvement in femoral head sphericity, after skeletal maturity this morphology had become more similar to how it was before the start of treatment. However, the clinical results were described as satisfactory by the patients.18 In spite of this, no studies currently exist with a follow-up time long enough to show a reduction in the risk of requiring total hip arthroplasty.
Although this surgical technique is reproducible and relatively simple, it is not without complications. Although these are not important, as we found they affect practically all of the cases treated.
The most common complications are screw trajectory infections and breakage of the same. This is usually not serious and is treated routinely, without any after-effects. Some authors have associated screw trajectory infections with an increased risk of infection of the hip arthroplasty that these patients may require in the future.20,21 The frequency of this infection varies from 75% to 95% depending on the series in question, and in approximately 5%–10% of cases the magnitude of the infection makes it necessary to remove the material.
Loosening of the screws is a frequent complication in those cases when a system with only 2 screws at the ends is used. To prevent this complication we recommend the use of 3 screws at supraacetabular level and 3 others in the femoral diaphysis, so that if one of the screws does become loose, the others still ensure good fixation. The use of hydroxyapatite-coated threaded surfaces is now recommended, as this aids integration of the screw and reduces the surrounding osteolysis.
Screw breakage is not always associated with previous trauma. Some authors have associated this event with risk factors such as rapid distraction and very heavy patients.22
Connector failure is a characteristic complication of articulated external unilateral fixators, and it may lead to a 15–20∘ loss of the abduction position. Many studies have shown that failure at the level of the fixator hinge is the most frequent location of mechanical failure, so that some authors favour glueing with PMMA at the time of surgery, or the use of metal cerclage. It has to be pointed out that in 2014 the manufacturer of the product changed the instructions for the component frequently used as the hinge (the self-aligning articulated body for DAF) in which this part is not recommended for use in paediatric hip arthrodiastasis. This may be associated with the failure of the same that was observed in our revision.
There are few serious complications, and they can be prevented by correct surgical technique. The hinge must be located at the centre of rotation of the hip. If this is not so then movement will be painful, restricted and with an increased tendency for the screws to loosen.3
Physeal distraction is a rare complication, and a single case is described in the bibliography,21 and it was not possible to identify the cause. It consisted of a 1.6cm chondrodiastasis that arose with no painful symptoms. The sole after-effect in an 8-year follow-up was hip rigidity. As a theory the authors suggested an increase in intra-joint adherences that favoured distraction of the epiphysis.
In spite of using screws with a diameter less than 1/3 of the diameter of the femoral diaphysis, the weakness caused by the holes may lead to the appearance of fractures due to low energy trauma. In this case a prolongation of the external fixator may be used as treatment.13
Other surgical techniques have not been shown to be suitable for late-onset Legge-Calvé-Perthes disease, leading to more serious complications. In the results presented by Noonan et al.8 of a series of 18 hips subjected to varicose osteotomies, in one case the osteosynthesis material failed so that arthrodesis was required. There was one case of infection, 7 cases with residual limping and 10 cases with a discrepancy in the length of the lower limbs. In the systematic revision undertaken by Hsu et al.10 Shelf-type osteotomies were not shown to improve functioning over the long-term or to affect the appearance of arthrosis. This procedure is also potentially the cause of complications such as absorption of the graft or proximal migration, even though these complications were not found in the works revised.
ConclusionsThe use of arthrodiastasis in late onset Legge-Calvé-Perthes disease or cases with a poor prognosis is a minimally invasive technique that has beneficial effects. It improves joint balance and reduces pain, with the advantage of not compromising surgery in the future if necessary. These results show that although there is no improvement in morphology following the use of an external fixator, its use in the initial phases of necrosis keeps cephalic sphericity. This is why it is important to operate these patients at the start of the disease, when the head is still minimally spherical.
Level of evidenceLevel IV.
Ethical responsibilitiesProtection of persons and animalsThe authors declare that no experiments took place with human beings or animals for this research.
Data confidentialityThe authors declare that they followed the protocols of their centre of work on the publication of patient data.
Right to privacy and informed consentThe authors declare that this paper contains no patient data.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Aguado-Maestro I, Abril JC, Bañuelos Diaz A, García Alonso M. Artrodiastasis de cadera en la enfermedad de Legg-Calvé-Perthes. Rev Esp Cir Ortop Traumatol. 2016;60:243–250.